Abstract
Introduction:
Onychomycosis is a fungal infection of the nail unit. Anatomical and physiological characteristics of the nail apparatus impose the need for long-term treatment to achieve complete cure.
Goal:
The main goal of this project is to study the effectiveness of several treatment protocols for onychomycosis based on Scoring Clinical Index for Onychomycosis (SCIO).
Material and methods:
The study included 133 patients with onychomycosis, diagnosed by KOH microscopy and culture. Based on disease severity, patients were grouped into groups with SCIO values: 6-9, and 12-16. These groups were randomly subdivided to 5 subgroups according to the given treatment protocols: fluconazole 150 mg 1x weekly, itraconazole continual therapy, itraconazole pulse therapy, terbinafine 250 mg/d, and terbinafine + ciclopirox 8% lacquer, respectively. The cure rate was evaluated at the end of 48 week.
Results:
The obtained cure rates according to the above mentioned protocols were: 92.30%, 81.81%, 83.33%, 90.90%, and 100%, respectively for groups of patients with SCIO values 6 – 9. Within patients with SCIO values 12-16, were achieved cure rates as follows: 78.57%, 78.57%, 75%, 80%, and 86.66%.
Conclusions:
There was no statistically significant difference in cure rate between five treatment protocols applied in this study. In patients with high SCIO values is expected a decrease in cure rate.
Keywords: onychomycosis, SCIO, treatment protocols
1. INTRODUCTION
Onychomycosis is a chronic fungal infection of the nail unit, which gradually destroys the nail plate (1). At the beginning, fungal nail infections are asymptomatic, and the only complaints of the affected persons are cosmetic. Later, with the disease progression, the nail plates become deformed, which may be followed by difficulties during prolonged standing and walk (if the disease is localized on toenails), obstacles during writing and typing (when fingernails are affected), pain, paresthesia, discomfort and loss of dexterity (2). Treatment of onychomycosis is mainly based on systemic therapy, excluding superficial form of onychomycosis, or the mildest cases when only the distal margin of the nail plate is affected. Therefore, treatment modality can be determined according to clinical form of onychomycosis, or SCIO values. SCIO is a mathematical tool that enables evaluation of the disease severity (3). It is based on key factors which affect development of onychomycosis and treatment success. Antimycotics used earlier (griseofulvine and ketoconazole) had their limitations because of side effects such as nausea, headache, skin rash, hypersensitivity, fotosensitivity, drug interaction, hepatotoxicity, the need for long use and frequent relapse after the cessation therapy. Nowadays, allylamines and azoles are the mainstay therapy for onychomycosis (1). In use are terbinafine, itraconazole and fluconazole. Extensive research on the use of these drugs show low level risk for the appearance of side effects. Fluconazole has not been approved by the FDA, however is used in other countries for onychomycosis treatment (4). The aim of this study is to evaluate the effectiveness of several treatment protocols for onychomycosis based on SCIO.
2. MATERIAL AND METHODS
The study included 133 patients with OM. They were subject of clinical nail examination and sampled for direct microscopy and culture. The sample collection was taken separately from each nail, provided that the patient didn’t receive systemic antifungal therapy or applied topical antifungals for at least 2 weeks. The material was collected from the most proximal part of the affected nail. Direct microscopy was repeated in cases with negative or suspicious results. For fungal culture was used Sabourod peptone-glucose agar. The evaluation of the disease severity was based on SCIO onycho-index and calculated by electronic calculator in the link: http://www.onychoindex.com. The disease severity was the main criterion according to which the sample stratification was done, and groups with SCIO values: 6–9, and 12-16 were formed. These groups were randomly subdivided to 5 subgroups according to the given treatment protocols: fluconazole (FLU) 150 mg 1x weekly, itraconazole continual therapy, 200mg/d (ITRc), itraconazole pulse therapy, 1 week per month (ITRp), terbinafine (TB) 250 mg/d and, TB + ciclopirox (CPX) 8% lacquer, topicaly 1/d, respectively. The patients underwent regular controls by a dermatologist every month. At each control was measured the length of the new proximal portion of the nail plate. Measurements of liver enzymes levels were performed in regular basis, too. SCIO values were calculated at the 12th and 48th week. In order to assess eradication of the fungal infection, KOH microscopy was performed at the end of the 48th week. The cure rate was evaluated at the end of the 48th week. Statistical processing of obtained data is done by ANOVA and Z–electronic calculator.
3. RESULTS
Table 1 shows patients with initial SCIO values 6–9 grouped according to the treatment protocols. ANOVA confirmed that there was no significant difference between the groups at the significance level p>0.05 (F = 1.036 and p=0.397), consequently the groups were comparable. At the week 12, in patients treated with combined therapy (TB+CPX) was achieved a significant improvement compared to other groups treated with monotherapy (Figure 1). However, by comparing the results of clinical evaluation between the groups, at the end of the 48th week (SCIO 48), no significant difference resulted (F=0.602, p=0.663) at the significance level p>0.5 The obtained results at the 48th week, which represent mycological cure, are expressed in percentage values. Z Test Calculator for 2 population proportions is used to compare the results of the each protocol with each one. It was concluded no significant difference in the treatment efficiency between these 5 treatment protocols at the significance level 0.05.
Table 1.
Performance of treatment with different protocols within the group of patients with initial SCIO values 6–9
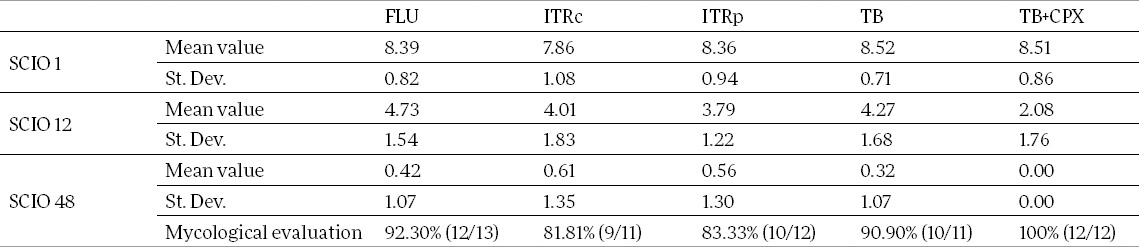
Figure 1.
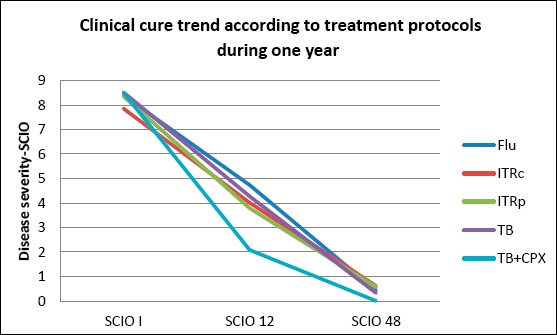
Clinical cure trend according to different treatment protocols in patients with SCIO 6–9.
There were 74 patients with initial SCIO values 12-16 divided randomly into 5 subgroups according to the treatment protocols (Table 2). By ANOVA testing is confirmed that there was no significant difference between those groups at the significance level 0.05, given that F = 1.593 and p=0.186, and consequently the groups were comparable.
Table 2.
Performance of treatment with different protocols among the patients with initial SCIO values 12–16

Based on SCIO treatment guideline, for patients with onychomycosis with SCIO values 12-16, was used the scheme of extended duration: itraconazole 200mg per day for 16 weeks continually; itraconazole pulse therapy – 4 pulses and terbinafine 16 weeks continually. During the follow up of the clinical cure, it was evident a slightly greater improvement in patients treated with terbinafine (Figure 2). However, by comparing SCIO values obtained at the end of the 48th week, resulted no significant difference between the groups (F=0.348, p=0.845) at the significance level p > 0.05.
Figure 2.
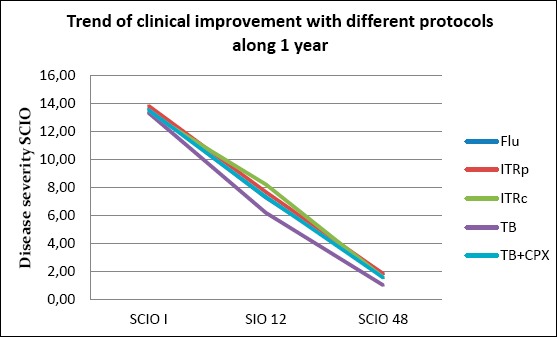
Trend of clinical improvement under different protocols in patients with SCIO 12-16.
By comparing the results of mycological cure obtained with different treatment protocols, expressed in percentage values, no significant difference among the groups of patients with initial SCIO value 12-16 was achieved at the significance level 0.05.
4. DISCUSSION
Treatment of onychomycosis is still challenging. In order to evaluate the superiority of one antifungal agent over the other, a lot of comparative studies have been done. Fluconasole wasn’t included in these studies.
In a study (5) with 53 patients with toenail onychomycosis caused by dermatophytes, 27 patients were treated with itraconazole 200 mg/daily, while other 26 of them were treated with terbinafine 250 mg/daily for 3 months. The achieved clinical and mycologic cure rate for group treated with itraconazole was 60.9% and 64.7% for terbinafine group, while remained other patients had improvement. In another study (6), 60 patients divided into 3 groups, were treated with 250mg/d terbinafine, 500 mg/d terbinafine for a week per month, and 400mg/d itraconazole for a week per month, respectively. In the all 3 groups the response to the treatment was similar, about 80% cure rate, and without significant difference. Honeyman et al. (7) have treated 85 patients with itraconazole 200mg/d, and other 82 patients with terbinafine 250mg/d for 4 months. At the end of the month 12, clinical cure rate for terbinafine group was 57.8%, and 62.6% for itraconazole group. The mycologic cure rate for terbinafine was 95.3% and 84.3% for itraconazole.
By analyzing the results of these studies concluded that largely doesn’t exist significant difference in treatment efficacy between itraconazole and terbinafine. However, in researches with larger number of patients, terbinafine treatment efficacy resulted to be greater than that of itraconazole, and this difference was significant (8, 9). In a study with 151 patients with dermatophyte caused toenail onychomycosis, was compared treatment efficacy between terbinafine 250mg/d and intermittent therapy with itraconazole (10). The continuous therapy with terbinafine showed superiority and the relapse rate was very low in comparison with intermittent therapy (10). Brautigam et al. (11), included 86 patients in the study, divided into 2 groups. To the first group was administered 250 mg/d terbinafine, and to the second one, 200 mg/d itraconazole. The achieved mycologic cure rates were 81% for terbinafine group, and 63% for itraconazole group. In a study by De Backer et al. (12), 186 patients with toenail onychomycosis were treated with 250 mg/d terbinafine, and other 186 patients with itraconazole 200 mg/d during 12 weeks. The difference in the treatment efficacy resulted significant, given that the clinical and mycological cure rates for terbinafine were 73% and 76%, while the obtained cure rates for itraconazole were 48% and 50% respectively. According to Roberts and his collaborators (1), terbinafine is superior in comparison with itraconazole in vitro as well as in vivo against dermatophyte caused onychomycosis, and should be considered as first line medication, while itraconazole should be considered as the best alternative of terbinafine. Cohen (13), reports that clinical experiments have documented the superiority of terbinafine over other antifungal agents for onychomycosis treatment.
Studies on the efficacy of fluconazole in treating onychomycosis, revealed high cure rates, but also the necessity for long term treatment. According to Welch and his collaborators (14), investigations have resulted with cure rate in the range 80-90% after administration of 150 mg fluconazole once-weekly for an average of 6-9 months. In a study (15) with 362 patients with toenail onychomycosis, 3 treatment protocols with fluconazole once weekly were administered in doses: 150mg, 300 mg, and 450mg. At the sixth month, achieved mycological cure rates were: 53%, 59%, and 61%, respectively. In another study, 349 patients with thumbnail onychomycosis, treated with fluconazole 150mg 1 x per week, achieved clinical cure rate 76% after six months (16).
For itraconazole is characteristic that its concentration in nail unit remains high even after the cessation of therapy (17). Therefore, itraconazole may be administered in pulse therapy regimens (intermittent dosing), every 4 week. Several studies have documented efficacy of itraconazole administered as continuous therapy 200 mg per day, or twice daily for 1 week per month (2 or 3 pulses) (18, 19, 20).
Combination of topical therapy with the newer oral antifungal agents may increase the efficacy in onychomycosis treatment (21) and shorten the duration of therapy. Therefore, the objective of several studies was the investigation of efficacy of combined therapy in onychomycosis treatment. Avner et al. (22) in 2005 compared treatment efficacy of terbinafine 250mg/d for 16 weeks as monotherapy with the combination therapy: terbinafine 250mg/d for 16 weeks + ciclopirox olamine 8% lacquer solution for 9 months. Mycological cure rate was 64.7% for monotherapy and 88.2% for the combination therapy. Other authors (23, 24) in their publications have reported the superiority of combination therapy over monotherapy based on the lower treatment cost as well, also.
In our study, different protocols were applied for onychomycosis treatment: fluconazole 150mg weekly, itraconazole 200mg/daily, itraconazole 400mg/daily, every 4 week of the month, terbinafine 250mg/daily, and terbinafine 250mg/daily in combination with 8% ciclopirox lacquer 1/daily. Patients were categorized into two groups based on the disease severity which was assessed by SCIO. Differences in the treatment outcomes proved to be not statistically significant as in studies with a small number of patients of the other authors.
5. CONCLUSION
Despite the fact that the combination therapy achieved better results compared to monotherapy, there was no significant difference in cure rate between five treatment protocols applied in this study. In patients with high SCIO values a decrease in cure rate is recorded. Standardized evaluation of onychomycosis severity helps in determining the appropriate therapy, objective assessment of the treatment progress, and enables comparison of similar conditions, which is important in scientific research.
Footnotes
CONFLICTS OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Roberts D, Taylor WD, Boyle DJ. Guidelines for treatment of onychomycosis. British Journal of Dermatology. 2003;148:402–410. doi: 10.1046/j.1365-2133.2003.05242.x. [DOI] [PubMed] [Google Scholar]
- 2.Pariser D. The Rationale for Renewed Attention to Onychomycosis. Seminars in Cutaneous Medicine and Surgery. 2013 Jun;32(2, Suppl 1):S9–S12. doi: 10.12788/j.sder.0013. [DOI] [PubMed] [Google Scholar]
- 3.Sergeev AY, Gupta AK, Sergeev YV. The Scoring Clinical Index for Onychomycosis (SCIO index) Skin therapy Lett. 2002;7(Suppl1):6–7. [PubMed] [Google Scholar]
- 4.Elewski B, Pariser D, Rich Ph, Scher RK. Current and Emerging Options in the Treatment of Onychomycosis. Semin Cutan Med Surg. 2013;32(2, Suppl 1):S9–S12. doi: 10.12788/j.sder.0016. [DOI] [PubMed] [Google Scholar]
- 5.Arenas R, Dominguez-Cherit J, Fernandez L M. Open randomized comparison of itraconazole versus terbinafine in onychomycosis. Int J Dermatol. 1995;34:138–143. doi: 10.1111/j.1365-4362.1995.tb03600.x. [DOI] [PubMed] [Google Scholar]
- 6.Tosti A, Piraccini B M, Stinchi C, Venturo N, Bardazzi F, Colombo MD. Treatment of dermatophyte nail infections: an open randomized study comparing intermittent terbinafine therapy with continuous terbinafine treatment and intermittent itraconazole therapy. J Am Acad Dermatol. 1996;34:595–600. doi: 10.1016/s0190-9622(96)80057-0. [DOI] [PubMed] [Google Scholar]
- 7.Honeyman JF, Talarico F S, Arruda LHF, et al. Itraconazole versus terbinafine (LAMISIL®): which is better for the treatment of onychomycosis? J Eur Acad Dermatol Venereol. 1997;9:215–221. [Google Scholar]
- 8.Sigurgeirsson B, Olaffson JH, Steinssen JB, et al. Long-termeffectiveness of treatment with terbinafine vs itraconazole in onychomycosis: a 5-year blinded prospective follow-up study. Arch Dermatol. 2002;138:353–357. doi: 10.1001/archderm.138.3.353. [DOI] [PubMed] [Google Scholar]
- 9.Evans EGV, Sigurgeirsson B, Billstein S. European multicentre study of continous terbinafine vs intermittent itraconazole in the treatment of toenail onychomycosis. Br Med J. 1999;318:1031–1035. doi: 10.1136/bmj.318.7190.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Doncker P, Degreef H, André J, Piérard G. The challenge of the future! Orlando, Florida, USA: Fifty-sixth Annual American Academy of Dermatology Meeting; 1998. Why are some patients with onychomycosis still not responding to the newer antifungal agents? Poster # 187. February 27-March 4. [Google Scholar]
- 11.Brautigam M, Nolting S, Schoff RE, Weidinger G. for the Seventh Lamisil German Onychomycosis Study Group. Randomized double blind comparison of terbinafine and itraconazole for treatment of toenail tinea infection. Br Med J. 1995;311:919–922. doi: 10.1136/bmj.311.7010.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Backer PP, De Keyser C, De Vroey, Lesaffre E. A 12-week treatment for dermatophyte toe onychomycosis: terbinafine 250 mg/day vs. itraconazole 200 mg/day - a double-blind comparative trial. Br J Dermatol. 1996;134(Suppl. 46):16–17. doi: 10.1111/j.1365-2133.1996.tb15653.x. [DOI] [PubMed] [Google Scholar]
- 13.Cohen AD, Medvesovsky E, Shalev R, et al. An independent comparison of terbinafine and itraconazole in the treatment of toenail onychomycosis. J Dermatolog Treat. 2003 Dec 14;(4):237–242. doi: 10.1080/09546630310017834. [DOI] [PubMed] [Google Scholar]
- 14.Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Mycology. 2010;28(2):151–159. doi: 10.1016/j.clindermatol.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Scher RK, Breneman D, Rich P, et al. A placebo-controlled, randomized, double-blind trial of once-weekly fluconazole (150 mg, 300 mg, or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol. 1998;38:S77–86. doi: 10.1016/s0190-9622(98)70490-6. [DOI] [PubMed] [Google Scholar]
- 16.Drake L, Babel D, Stewart M, et al. A placebo-controlled, randomized, double-blind trial of once-weekly fluconazole (150, 300, or 450 mg) in the treatment of distal subungual onychomycosis of the fingernail. J Am Acad Dermatol. doi: 10.1016/s0190-9622(98)70491-8. in press. [DOI] [PubMed] [Google Scholar]
- 17.De Doncker P. Pharmacokinetics of oral antifungal agents. Dermatol Ther. 1997;3:46–57. [Google Scholar]
- 18.De Doncker P, Decroix J, Pierard G E, et al. Antifungal pulse therapy for onychomycosis: a pharmacokinetic and pharmacodynamic investigation of monthly cycles of 1-week pulse therapy with itraconazole. Arch Dermatol. 1996;132:34–41. doi: 10.1001/archderm.132.1.34. [DOI] [PubMed] [Google Scholar]
- 19.Havu V, Brandt H, Heikkilä H, Hollne A, Oksman R, Rantanen T, Saari S, Stubb S, Turjanmaa K, Piepponen T. A double-blind, randomized study comparing itraconazole pulse therapy with continuous dosing for the treatment of toe-nail onychomycosis. Br J Dermatol. 1997;136:230–234. [PubMed] [Google Scholar]
- 20.Odom R, Daniel C R, III, Aly R. A double-blind, randomized comparison of itraconazole capsules and placebo in the treatment of onychomycosis of the toenail. J Am Acad Dermatol. 1996;35:110–111. doi: 10.1016/S0190-9622(96)90519-8. [DOI] [PubMed] [Google Scholar]
- 21.Tosti A. Onychomycosis - emedicine.medscape.com/article/1105828-overview [Google Scholar]
- 22.Avner S, Nir N, Henri T. Combination of oral terbinafine and topical ciclopirox compared to oral terbinafine for the treatment of onychomycosis. J Dermatol Treatment. 2005;16:327–330. doi: 10.1080/09546630500420183. [DOI] [PubMed] [Google Scholar]
- 23.Baran R, Kaoukhov A. Topical antifungal drugs for the treatment of onychomycosis: an overview of current srategies for monotherapy and combination therapy. JEADV. 2005;19:21–29. doi: 10.1111/j.1468-3083.2004.00988.x. [DOI] [PubMed] [Google Scholar]
- 24.Frankum LE, Nightengale B, Russo CL, Sarnes M. Pharmacoeconomic analysis of sequential treatment path-ways in the treatment of onychomycosis. Managed care interface. 2005;18:55–63. [PubMed] [Google Scholar]


