Abstract
Background and Objective
The role of bariatric surgery in non-obese patients with type 2 diabetes (T2DM) remains unclear, and its use in clinical practice is controversial. We conducted a systemic review and meta-analysis to investigate the metabolic changes after surgical treatment in diabetic patients with body mass index (BMI) <30 kg/m2.
Methods
We conducted a comprehensive search in MEDLINE (PubMed), EMBASE and the Cochrane Library of published articles from January 2000 to April 2013 reporting the clinical outcome changes in various metabolic outcomes in diabetic patients with BMI <30 kg/m2.
Results
Ten prospective studies including 290 patients were included in the meta-analysis. Bariatric surgery led to an overall 2.79 kg/m2 [95%CI 2.05~3.53, P<0.00001] reduction in BMI, a 1.88%[95%CI 1.32~2.43, P<0.00001] reduction in glycosylated hemoglobin, a 3.70 mmol/L [95%CI, 1.93~5.47, P<0.00001] reduction in fasting blood glucose, a 6.69 mmol/L [95%CI, 2.29~11.08, P=0.003] reduction in postprandial glucose, anda 3.37 [95%CI 0.55~6.18, P=0.02] reduction in homeostasis model assessment of insulin resistance (HOMA-IR). After surgical treatment, 76.2% of the patients were insulin free, and 61.8% patients were off medication. In total, 90(42.4%), 10(37%) and 34(37.2%) patients had post-surgical HbA1c levels of <6%,<6.5% and<7%, respectively. No deaths were observed in the included studies, and the major complication rate was 6.2%.
Conclusions
Based on the currently available data, bariatric surgery might improve glycemic control and weight loss in a very limited range with a doubled surgical complication rate in drug-refractory T2DM patients with BMI <30 kg/m2. It remains too premature to suggest bariatric surgery for non-obese T2DM patients.
Introduction
Type 2 diabetes mellitus (T2DM) is a global public health issue. The global prevalence of diabetes among adults 20~79 years of age was 8.3% in 2011, with 366 million people affected, and was predicted to increase to 9.9% by 2030 [1]. Current treatments for T2DM focus on the prevention and management of complications, instead of on a radical cure, because T2DM is considered to be an irreversible, chronic, and progressive disease. In spite of the rapid progress in pharmacological and non-pharmacological approaches to diabetes in recent years, 92.7% of adult diabetic patients had poorly-controlled blood glucose levels and related co-morbidities [2].
Bariatric surgery in patients with a larger body-mass index (BMI) could lead to complete resolution of diabetes in more than 90% of patients, with a reduction in risk factors for cardiac disease including hypertension and lipid abnormalities [3,4]. The underlying mechanisms have been suggested to involve weight loss and caloric restriction. However, a large study including 608 patients with a follow-up period of 14 years suggested that the resolution of diabetes occurred long before significant weight loss, and the correction of T2DM continued even when the patients remained obese [5].
In recent years, surgical treatments have attracted growing interest as therapies for non-obese T2DM patients [6–9]. Surgery has been reported to possibly facilitate glycemic control with a reduction in the need for insulin [10]. However, a limited study population and short follow-up duration might introduce biases into the outcomes. There have been few published systematic reviews on the effect of metabolic surgery as a single treatment in non-obese T2DM patients.
In this study, we attempted to analyze the published surgical observational studies in non-obese T2DM patients (defined as patients with BMI <30 kg/m2) to discover the clinical evidence of metabolic surgery for the resolution of diabetes.
Materials and Methods
The meta-analysis was conducted following the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines [11]. We reported this study in accordance with the preferred reporting items for systematic reviews and the meta-analysis (PRISMA) checklist (S1 Table).
Literature Search
We conducted a comprehensive search in MEDLINE (PubMed), EMBASE and the Cochrane Library from January 2000 to April 2013 with a combination of the following keywords: “bariatric surgery OR metabolic surgery OR obesity surgery OR Roux en Y OR gastric banding OR anastomosis OR biliopancreatic diversion OR gastric bypass OR jejunoileal bypass” AND “diabetes OR diabetes mellitus OR type 2 diabetes OR T2DM” AND “overweight OR low BMI OR body mass index <30 kg m2 OR normal weight”. In addition, we reviewed the references of the included studies for additional potentially eligible studies. We checked the studies for duplicate publications. Articles on identical participants were considered to use an overlapping population, under which circumstances, the data were extracted only from the highest quality study. Articles that only provided abstracts were included if sufficient data were reported; unpublished reports were not considered.
Inclusion and Exclusion Criteria
The following criteria were used for inclusion of the study into the analysis:1) T2DM patients with baseline BMIs lower than 30 kg/m2; 2) gastrointestinal (GI) abnormalities, such as peptic ulcer diseases (PUDs), gynecological abnormalities and gastric carcinoma, were not associated at baseline; 3) at least two of the outcomes of interest were reported clearly; and 4) English was the language of publication regardless of the research methods.
Literature reviews were excluded as were articles with data from overlapping populations, animal or in vitro studies, studies involving children or adolescents, and studies of type 1 diabetes or gestational diabetes.
Data extraction and quality assessment
All the data were extracted independently by two authors (AB, SL) using a predefined standardized data extraction form. Discrepancies were resolved by consulting a third investigator (GL). Corresponding or first authors were contacted through E-mail in cases in which the data regarding our outcome of interest were likely to have been analyzed, although they were not clearly reported. The following data were extracted from the included articles: the first author, publication year, country, study design, sample size, intervention type, sex, age, follow-up duration, diabetes duration and comparable outcomes. The following outcomes were analyzed to assess the metabolic status before and after various bariatric surgeries: the BMI, glycated hemoglobin A1c (HbA1c), fasting blood glucose (FBG), postprandial blood glucose (PP), C-peptide, homeostatic model of insulin resistance (HOMA-IR), total cholesterol (TC), triglyceride (TG) levels and body weight.
The quality of the included studies was assessed by the Newcastle-Ottawa scale for the selection of the participants, adjustments of the confounders, description of the outcomes and duration of the follow-up [12].
Data analysis
The following data were collected to indicate diabetes-related clinical outcomes: the remission rate (the percentage of patients who had reached various target points) in each study and the medicine-free rate (the percentage of patients who discontinued medicine after surgery). The overall remission rates were calculated as the percentage of the patients having achieved an HbA1c level <6%, <6.5%, and <7%, respectively, if reported in the studies. The status of the patients receiving insulin and post-surgical amelioration of medication treatment were assessed if provided in the studies.
The status of co-morbidities and complications before surgery and the improvement rates after surgery were described based on the information provided in each study and were calculated in percentages when the relevant data were available.
The safety of the surgical methods was evaluated in percentages by the surgery-related complications and mortality rate in each included study.
Statistical analysis
The statistical analysis was performed using Review manager 5.1 software (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration). A P value <0.05 was considered to be statistically significant. The mean difference (MD) and 95% CI were used to describe the continuous data for each study. We assessed the heterogeneity among the studies initially by graphically examining the forest plots and subsequently by a statistical evaluation using a Chi-square test of homogeneity and evaluation of the inconsistency index (I2) statistic. A P-value <0.1 or I2>50% indicates significant statistical heterogeneity among the studies. We pooled the studies using a random-effect model in the presence of statistical or other heterogeneity and fixed-effect models otherwise.To explore the sources of between study heterogeneity in the pooled analysis, subgroup analyses were performed based on the geographic area, intervention type, duration of diabetes, and follow-up period.
Results
Search results
The flow diagram of the article selection is shown in Fig 1. In total, 662 articles and abstracts were identified by the initial searches, of which 560 articles were excluded by screening the titles. An additional 62 papers were excluded after reading the abstracts, leaving 64 articles for the full publication review. After a full-text examination, 16 potentially appropriate papers were finally retrieved. We found population overlapping between two studies. Of two studies conducted by Depaula et al., only one reported our outcomes of interest, and it was included. Three studies had data with a BMI >30 kg/m2, and one study had inadequate data of interest. Ten articles were included in the final analysis [7–10,13–18]. Table 1 shows the baseline characteristics of the final studies that were included for the meta-analysis. The quality assessments of the included studies are shown in S2 Table.
Fig 1. Flow chart of article selection.
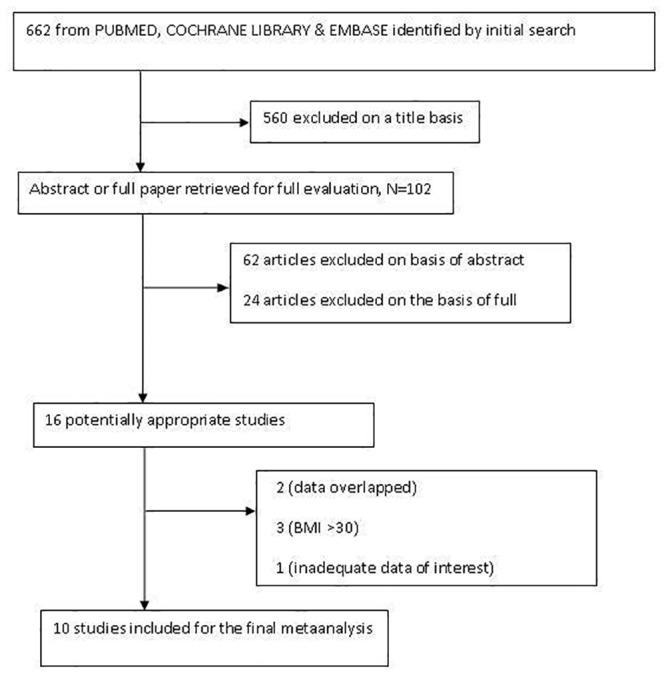
Table 1. Baseline characteristics of the included studies.
| Included study | Study design | Sample size (M/F) | Type of surgery | Country | Mean age(yrs) | Follow-up period(months) | Duration of diabetes (yrs) | Studied outcomes |
|---|---|---|---|---|---|---|---|---|
| Ramos et al [7] | Prospective | 20 (11/9) | DJB | Brazil | 43yrs | 6 | 5.3, range: (2–8) | BMI, FBG, HbA1c, C-peptide |
| Depaula et al [13] | Prospective | 69 (47/22) | LII+DSG | Brazil | 51±5.6 | 21.7 | 11±4 | FBG, HbA1c, BMI, lipids, C-peptide, HOMA-IR, co-morbidities |
| Geloneze et al [10] | Prospective | 12 (9/3) | DJB | Brazil | 50±5.3 | 6 | 9±2 | FBG, HbA1c, C-peptide, BMI, C-peptide |
| Lee et al [18] | Prospective | 6 (6/0) | DJB | Korea | 50.2 | 6 | 5.5, range: (2–10) | FBG, HbA1c, body weight |
| Kim et al [8] | Prospective | 10 (2/8) | LMGB | Korea | 49.6 | 6 | 6.6 | BMI. HbA1c, FBG, PP |
| Scopinaro et al [17] | Prospective | 15 (13/2) | BPD | Italy | 57.8±6.7 | 24 | 11.1±6.1 | Body weight, BMI, HbA1c, HOMA-IR, lipids, FBG |
| Navarrete et al [9] | Prospective | 10 (5/5) | LSG+DJB | Venezuela | 46.5 | 12 | <10 | HbA1c, body weight, FBG, BMI |
| M.García et al [16] | Prospective | 13 (10/3) | BAGUA | Spain | 63.84±8.25 | 6 | 16.9±8.75 | FBG, PP, HbA1c, C-peptide, BMI, co-morbidities. |
| J.B.Dixon et al [37] | Prospective | 103 (41/62) | LMGB+RYGB | Korea+Taiwan | 47.5±9.6 | 12 | 8.2±5.0 | BMI, HbA1c |
| C.Shrestha et al [15] | Prospective | 33 (24/9) | RYGB | China | 49.51±1.33 | 3 | <10 | BMI, HbA1c, FBG, PP |
BAGUA = one anastomosis gastric bypass;BMI = body mass index; BPD = biliopancreatic diversion; FBG: fasting blood glucose; DJB = duodenojejunalbypass; HOMA-IR: homeostatic model of insulin resistance; M/F = male/female; LII-DSG = laparoscopic sleeve gastrectomy; LMGB = laparoscopic mini gastric bypass;PP = postprandial blood glucose; RYGB = roux-en-Y gastric bypass; TC = total cholesterol; TG = triglyceride
Systematic review
The ten eligible studies were prospective studies involving a total of 290 T2DM patients, with a mean age of 51.4 years, and with 58% of the pooled participants being male. The studies were conducted in populations from Brazil (3), Korea (2), Italy (1), Venezuela (1), China (1), Spain (1) and both Taiwan & Korea (1). The mean BMI was 26.62±2.19 kg/m2. The follow-up interval ranged from three months to two years. The mean duration of diabetes prior to surgery in each included study ranged from 2 to 20 years. The participants involved underwent bariatric surgery for the purpose of glycemic control.
Various surgical procedures were investigated, with the performance of duodenal—jejunal bypass surgery (DJB) in three studies, sleeve gastrectomy (LII-DSG) in two, biliopancreatic diversion (BPD) in one, Roux-En Y in one, laparoscopic mini-gastric bypass (LMGB) in one, and anastomosis gastric bypass (BAGUA) in one study. One study population was composed of 79% patients undergoing LMGB and 21% Roux-En Y gastric bypass. All of the patients were under treatment for diabetes, specifically by therapy with insulin, oral anti-hyperglycemic agents or both. Insulin users accounted for 42.8% of the pooled population.
Resolution and remission of T2DM was defined and reported differently in each study. In the overall population, the rates of achievement of HbA1c levels of 6%, 6.5%, and 7% were 42.4% (N = 90/212),37% (N = 10/27), and 37.2% (N = 34/94), respectively. Although the remission rate was low,the reliance on anti-diabetic medications was reduced with statistical significance after surgery. Throughout the follow-up period after surgery, 76.2% of the patients were insulin free, and 61.8% were medication free for blood glucose control. The prevalence of the co-existence of hypertension and dyslipidemia was 21.7% and 41.7% in the overall population before surgery, respectively. After surgery, blood pressure was controlled in 88.9% of the patients without antihypertensive medications, and serum TC and TG improved in 45.8% and 38% of the overall patients, respectively [13,17].
The overall major surgical complication rate was 6.2%, including intestinal obstruction, intestinal perforation, and intra-abdominal bleeding (S3 Table). The rate of early surgical complications (<30 days) was 3.4%, including the presence of a fistula, gastrointestinal bleeding, urinary tract infection, pneumonia, and wound infection. In one of the included studies with a long follow-up period (21.7 months), 15.9% of the patients reported complications including prolonged diarrhea, gouty attacks, prolonged emesis, urinary tract infection, or fungal esophagitis during the follow-up [13]. Death was not reported in any of the included studies. More detailed data from each study are provided in S4 Table.
Meta-analyses
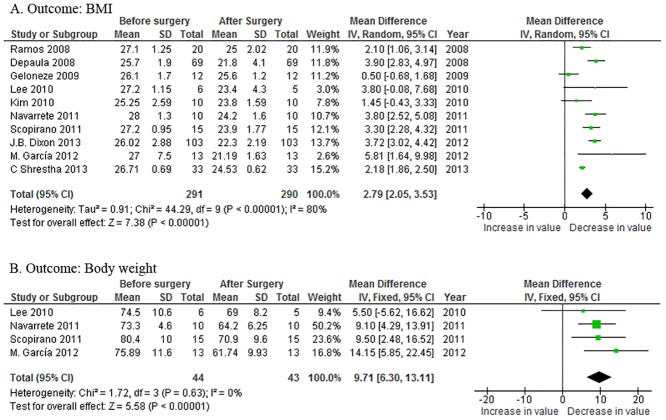
BMI and weight loss
All the articles reported mean changes in the BMI. Compared with the preoperative status, the BMI reduction was 2.79 kg/m2 [95%CI 2.05~3.53, P<0.00001] after surgery (Fig 2A), when a random-effect model was applied because the heterogeneity among the studies was obvious (P<0.0001). Body weight loss was reported in four papers, and the overall weight loss was 9.71 kg [95%CI 6.30~13.11, P<0.00001] (Fig 2B) in the fixed-effect model.
Fig 2. Forest plots of the effects of metabolic surgery on:(A) body mass index (BMI) and (B) body weight.
CI = confidence interval; IV = inverse variance; SD = standard deviation.
Glycemic control
Nine of the papers included in the meta-analysis reported changes in the HbA1c levels before and after surgery. The overall HbA1c level reduction was 1.88% [95%CI 1.32~2.43, P<0.00001] after surgery (Fig 3A). The overall reduction of the fasting blood glucose (FBG) level was 3.70mmol/L [95%CI 1.93~5.47, P<0.0001] in seven papers with available data (Fig 3B). The overall reduction of the postprandial blood glucose level was 6.69mmol/l [95%CI 2.29~11.08, P = 0.003] in three papers with available data (Fig 3C). The random—effect model was used in all three analyses because significant statistical heterogeneity among the studies was observed (P<0.00001 in all three analyses).
Fig 3. Forest plotsof the effects of metabolic surgery on: (A) HbA1c; (B) fasting blood glucose; and (C) postpradial blood glucose.
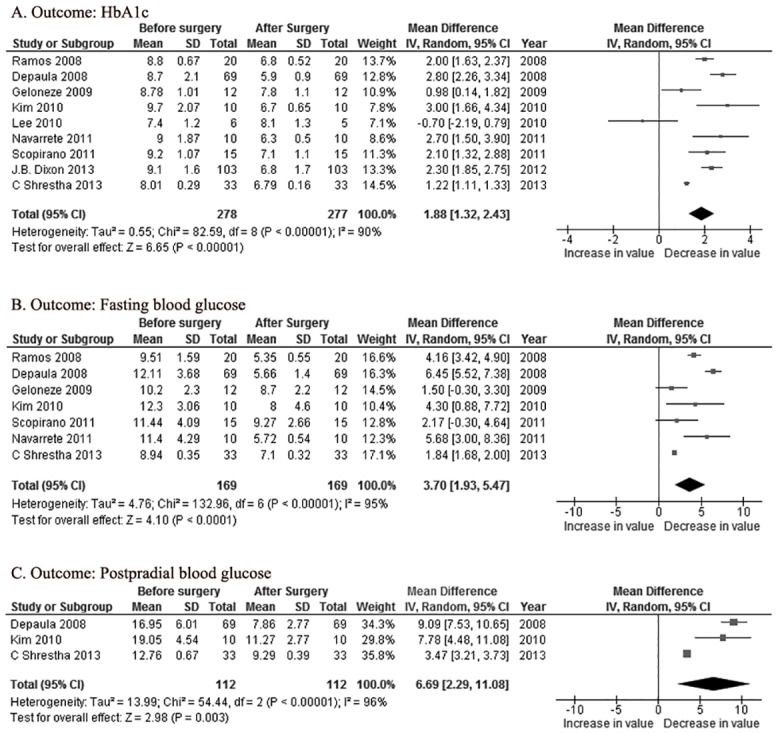
CI = confidence interval; IV = inverse variance; SD = standard deviation.
Lipid profiles
Four of ten articles reported the values of TC and TG before and after surgery and were included for the mean estimation. The overall reductions of TC and TG were 29.49 mg/dl [95%CI -5.23~64.21, P = 0.10] and 22.27mg/dl [95%CI -55.79~100.32, P = 0.58], respectively (Fig 4A and 4B). The random—effect model was applied for significant statistical heterogeneity (P<0.0001).
Fig 4. Forest plotsof the effects of metabolic surgery on: (A) total cholesterol and (B) triglyceride.
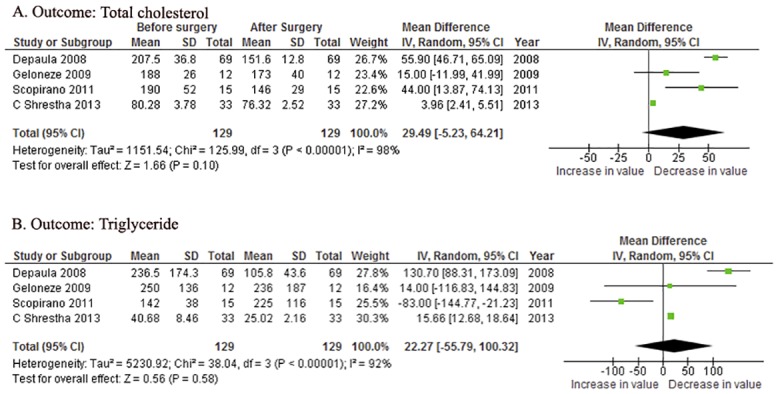
CI = confidence interval; IV = inverse variance; SD = standard deviation.
Insulin resistance and beta cell function
Three articles reported the HOMA-IR before and after surgery. The overall C-peptide decrement was 0.37ng/ml [95%CI -0.48~1.22, P = 0.40] in four papers with reported data (Fig 5A). The overall reduction of the HOMA-IR was 3.37 [95%CI 0.55~6.18, P = 0.02] (Fig 5B). The random—effect model was usedin both analyses for significant statistical heterogeneity (P<0.00001 in both analyses).
Fig 5. Forest plotsof the effects of metabolic surgery on: (A) C-peptide and (B) HOMA-IR.
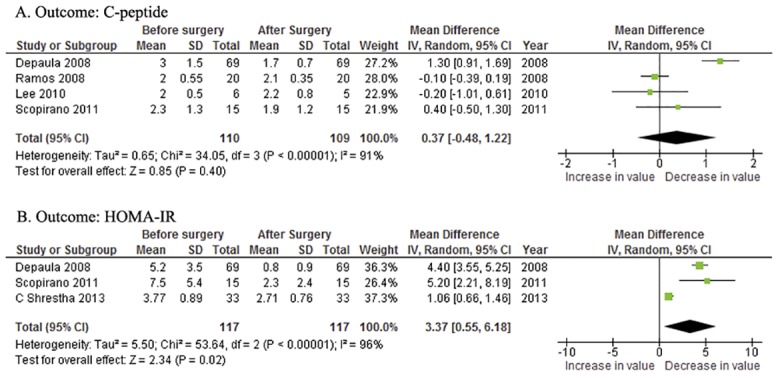
CI = confidence interval;HOMA-IR = homeostasis model assessment of insulin resistance; IV = inverse variance; SD = standard deviation.
Subgroup analyses
We introduced subgroup analyses to explore the source of heterogeneity and understand the effect factors of the results better. We explored all the studied outcomes, stratified by the follow-up period, type of surgery, duration of diabetes, and ethnicity. The results are shown in Table 2. In the subgroup with a follow-up period of longer than seven months, the pooled BMI, HbA1c, and FBG showed a significant reduction (pooled OR [95% CI]: BMI, 3.68 [3.20~4.15]; HbA1c, 2.46 [2.15~2.76]; FBG, 4.91 [2.32~7.51]), all of which were more significant reduced than those in the subgroup with a shorter follow-up period (pooled OR [95% CI]: BMI, 2.08 [1.79~2.37]; HbA1c, 1.28 [1.18~1.39]; FBG, 2.80 [1.16~4.45]). This finding indicated that the effect of bariatric surgery might be associated with the follow-up duration. In the subgroup with a duration of diabetes longer than eight years, the pooled BMI and HbA1c levels were reduced significantly (pooled OR [95% CI]: BMI, 3.41 [2.51~4.31]; HbA1c, 2.18 [1.38~2.98]), both of which were more significantly reduced than those in the subgroup with a shorter diabetic duration (pooled OR [95% CI]: BMI, 2.00 [1.32~2.68]; HbA1c, 1.78 [1.46~2.11]). This finding indicated that patients with a shorter duration of diabetes might gain greater benefit from bariatric surgery.
Table 2. Stratified analyses of the investigated outcomes.
| Variables | Stratification | Number of studies | Pooled mean differences (95%CI) | P value for heterogeneity | I 2 | P value for pooled mean differences |
|---|---|---|---|---|---|---|
| BMI | ||||||
| Follow-up period | ||||||
| >7 months | 4 | 3.68 [3.20–4.15] | p = 0.86 | 0% | p<0.0001 | |
| <7 months | 5 | 2.08 [1.79, 2.37] | p = 0.06 | 56% | p<0.0001 | |
| Type of surgery | ||||||
| DJB | 3 | 2.20 [1.29, 3.11] | p = 0.43 | 0% | p<0.0001 | |
| Duration of diabetes | ||||||
| >8 years | 6 | 3.41 [2.51,4.31] | p = 0.0001 | 83% | p<0.00001 | |
| <8 years | 4 | 2.00 [1.32, 2.68] | p = 0.93 | 0% | p<0.0001 | |
| Ethnics | ||||||
| Asia | 4 | 2.55 [1.58, 3.51] | p = 0.0009 | 82% | p<0.0001 | |
| South America | 4 | 3.08 [2.46, 3.70] | p = 0.04 | 65% | p<0.0001 | |
| HbA1c | ||||||
| Follow-up period | ||||||
| >7 months | 4 | 2.46 [2.15, 2.76] | p = 0.39 | 0% | p<0.00001 | |
| <7 months | 5 | 1.28 [1.18, 1.39] | p = 0.0005 | 86% | p<0.0001 | |
| Type of surgery | ||||||
| DJB | 3 | 1.71 [1.38, 2.04] | p = 0.00001 | 87% | P = 0.16 | |
| Duration of diabetes | ||||||
| >8years | 4 | 2.18 [1.38, 2.98] | p = 0.00001 | 93% | p<0.00001 | |
| <8years | 4 | 1.78 [1.46, 2.11] | p = 0.001 | 84% | p = 0.01 | |
| Ethnics | ||||||
| Asia | 3 | 1.55 [0.60, 2.50] | p = 0.00001 | 91% | 0 = 0.001 | |
| South America | 4 | 2.14 [1.86, 2.42] | p = 0.006 | 79% | p<0.0001 | |
| FBG | ||||||
| Follow-up period | ||||||
| >7 months | 3 | 4.91 [2.32, 7.51] | p<0.00001 | 80% | p<0.0002 | |
| <7 months | 4 | 2.80[1.16, 4.45] | p = 0.007 | 92% | p<0.0008 | |
| Type of surgery | ||||||
| DJB | 2 | 2.96 [0.37, 5.56] | p<0.00001 | 86% | p = 0.03 | |
| Duration of diabetes | ||||||
| >8 years | 4 | 4.02[0.97, 7.07] | p = 0.00001 | 97% | p = 0.010 | |
| <8 years | 3 | 3.27 [1.31, 5.22] | p = 0.03 | 72% | p = 0.001 | |
| Ethnics | ||||||
| Asia | 2 | 2.45 [0.37, 4.53] | p = 0.02 | 49% | p = 0.02 | |
| South America | 4 | 4.46 [2.53, 6.39] | p = 0.00001 | 89% | p<0.0001 | |
| PP | ||||||
| Follow-up period | ||||||
| >3 months | 2 | 5.30 [1.12, 9.47] | p = 0.01 | 0% | p<0.0001 | |
| C-peptide | ||||||
| Type of surgery | ||||||
| DJB | 2 | -0.11 [-0.38, 0.16] | p = 0.48 | 0% | p = 0.42 | |
| Duration of diabetes | ||||||
| <8 years | 2 | -0.11[-0.38, 0.16] | p = 0.48 | 0% | p = 0.42 | |
| Total cholesterol | ||||||
| Follow-up period | ||||||
| >7 months | 2 | 54.89[46.09,63.68] | p = 0.46 | 0% | p<0.00001 | |
| <7 months | 2 | 4.00 [2.45, 5.54] | p = 0.42 | 0% | p<0.00001 | |
| Triglyceride | ||||||
| Follow-up period | ||||||
| >7 months | 2 | 15.66[12.68,18.64] | p = 0.98 | 0% | p<0.00001 | |
| Ethnics | ||||||
| South America | 2 | 89.43[19.92,198.79] | p = 0.10 | 64% | p = 0.11 | |
| HOMA-IR | ||||||
| Follow-up period | ||||||
| >3 months | 2 | 4.46 [3.64, 5.28] | p = 0.61 | 0% | p<0.00001 |
BMI = body mass index; CI = confidence interval; FBG = fasting blood glucose; DJB = duodenojejunal bypass; HOMA-IR = homeostatic model of insulin resistance; PP = postprandial blood glucose
Discussion
T2DM is a chronic disease with a high prevalence and limited major treatments. Bariatric surgery is suggested be an alternative treatment for T2DM that has possibilities to induce remission of the disease. In 2011, the International Diabetes Federation (IDF) released a statement [19] suggesting that bariatric surgery could be used in obese patients with a BMI >40 kg/m2 and that it might bring benefit to obese T2DM patients with a relatively low BMI (BMI 30~35 kg/m2), who do not respond to standard medical therapies. However, the effects of bariatric surgery for non-obese T2DM patients have not been established. Although previously published studies predominantly focused on the role of bariatric surgery in patients with BMI<35kg/m2, patients with BMI<30kg/m2 were occasionally included in most studies [20–22]. The global cutoff points of the BMI for overweight and obesity are set at 25.0 kg/m2 and 30.0 kg/m2, respectively, by the World Health Organization (WHO) [23]. However,epidemiological studies have suggested thatwhen the BMI exceeds 25kg/m2, every 5 kg/m2 elevation in the BMI is associated with an approximately 30% increase in mortality [24]. A systematic review of the co-morbidity incidences for overweight and obese populations in 89 studies showed that obese and overweight patients are associated with an increased risk of multiple co-morbidities [25]. Thus, overweight deserves attention equal to that of obesity in medical treatments, considering the incidence of morbidity and mortality. Additionally, several studies in overweight patients without obesity have suggested that surgery provided potential benefits in treating T2DM and its related co-morbidities [13,26] whereas some studies reported low remission and amelioration rates of only 15% and 30%, respectively [27]. Although our preliminary data suggested potential beneficial effects of surgery in non-obese T2DM patients, it is too early to suggest the clinical application of bariatric surgery for non-obese T2DM patients.
In this study, we pooled the data from 290 non-obese T2DM patients, who received bariatric surgery after the failure of glycemic control via the available pharmacological treatments. Statistically significant improvements in the HbA1c, FBG, PP and HOMA-IR levels aftersurgery were observed in the pooled analysis. Compared with the studies in patients with higher BMI levels, the trend was consistent; however, the level of improvement was lower. Our results suggested that various metabolic surgeries could lead to significant reduction in insulin administration, as well as the use of oral medication, regardless of the surgical procedure. Although no deaths were reported in the included studies, the overall major complication rate from surgery was 6.2%, and the reoperation rate was 1.7%, almost twice as much as the rates in patients with slightly higher BMI levels [20]. The ethical consideration should be drawn to seek approximately 40% remission rate of diabetes from surgery with a 6% major complication rate. Thus, the evidence remained far from adequate for supporting surgery in non-obese T2DM patients. Studies should report their data with prolonged follow-up periods to address the long-term effects and safety. The ethical considerations of newly conducted clinical trials should be analyzed carefully because the net benefit from surgical treatment in non-obese patients is difficult to address.
In our pooled results, a weight loss of 9.7 kg (ranging from 5.7% to 32%) and a remission rate of 42.4%(defined as the achievement of an HBA1c level < 6%) were observed after surgery. However, this finding was inconsistent with a meta-analysis conducted by Li et al., which involved 357 patients with a BMI <35 kg/m2 from thirteen studies, and reported a weight loss of 17.23kgwith an 80% remission rate(HBA1c<7%) and a 66.35%clinical resolution rate [20]. This inconsistency might suggest an association between the effect of bariatric surgery and the preoperative BMI. Patients with BMI 30~35 kg/m2 could increase the pooled effect size of surgery in the previous meta-analysis.
Our subgroup analysis indicated that patients with a longer follow-up duration might gain more benefit from the surgery, noting that the 95% CI was not overlapped, which indicated that a long-term reduction of the BMI and HbA1c levels derived by bariatric surgery in non-obese patients might be worth further investigation. The continuation of the follow-up of patients in existing studies is necessary to address the long-term effect and safety profiles. In the subgroup analysis, the patients with a longer duration of diabetes achieved a higher reduction of the BMI and HbA1c; however the 95% CI overlapped. This result is inconsistent with previous meta-analyses [16,28–34]. Traditionally, patients with a shorter diabetic duration were considered to have better beta-cell function. However, the patients with various durations of diabetes from our included studies had a similar pre-surgical C-peptide level, which is generally lower than that shown in most previous studies of bariatric surgery in patients with higher BMI levels [35,36]. In addition, our results indicated that the C-peptide level was not changed significantly after surgery, whereas only the HOMA-IR improved. The relatively poor beta-cell function in non-obese patients, regardless of the diabetic duration, might partially explain this inconsistency, as well as the poor efficacy of bariatric surgery in such patients. Only a few included articles reported the association of diabetes with its co-morbidities, adding difficulty in the accurate assessment of the metabolic status after surgery. With the available studies pooled, our overall results showed that TC and TG were not changed significantly after surgery. There remains no evidence for introducing bariatric surgery aiming to treat any co-morbidity in non-obese patients.
This meta-analysis has several limitations. First, our meta-analysis included a very limited number of non-RCT studies, which had small sample sizes and incomplete data, which potentially affected the accuracy of the analysis. Second, we used the BMI to define obesity and overweight, as suggested by the WHO, which could only partially reflect the fitness of diabetic patients. Third, significant heterogeneity was observed in the overall analysis, which might result in the pooled results being less convincing, although we applied random-effect models and conducted the subgroup analysis accordingly. Fourth, reporting bias could be introduced because positive results are more likely to be published. Fifth, only articles published in English were included, which might lead to publication bias. Finally, the follow-up durations of the included studies were short, which caused the long-term effect and safety data for non-obese patients to be unclear.
Conclusion
Based on the currently available data, bariatric surgery might improve glycemic control and weight loss in a very limited range, with doubled surgical complications in drug-refractory T2DM patients with BMI <30 kg/m2. It is too early to suggest bariatric surgery for non-obese T2DM patients. Persistent follow-up of non-obese patients in existing studies is necessary to further address the long-term efficacy and safety of surgical treatment in this patient population.
Supporting Information
(DOCX)
(DOCX)
BAGUA = one anastomosis gastric bypass; BPD = biliopancreatic diversion; DJB = duodenojejunal bypass; LII-DSG = laparoscopic sleeve gastrectomy; LMGB = laparoscopic mini gastric bypass; RYGB = roux-en-Y gastric bypass.
(DOCX)
LDL = low-density lipoprotein; NA = not available.
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–21. Epub 2011/11/15. 10.1016/j.diabres.2011.10.029 . [DOI] [PubMed] [Google Scholar]
- 2. Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291(3):335–42. Epub 2004/01/22. 10.1001/jama.291.3.335 . [DOI] [PubMed] [Google Scholar]
- 3. Monteforte MJ, Turkelson CM. Bariatric surgery for morbid obesity. Obes Surg. 2000;10(5):391–401. Epub 2000/10/29. 10.1381/096089200321594246 . [DOI] [PubMed] [Google Scholar]
- 4. Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37. Epub 2004/10/14. 10.1001/jama.292.14.1724 . [DOI] [PubMed] [Google Scholar]
- 5. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222(3):339–50; discussion 50–2. Epub 1995/09/01. ; PubMed Central PMCID: PMCPmc1234815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Geloneze B, Geloneze SR, Chaim E, Hirsch FF, Felici AC, Lambert G, et al. Metabolic surgery for non-obese type 2 diabetes: incretins, adipocytokines, and insulin secretion/resistance changes in a 1-year interventional clinical controlled study. Ann Surg. 2012;256(1):72–8. Epub 2012/06/06. . [DOI] [PubMed] [Google Scholar]
- 7. Ramos AC, Galvao Neto MP, de Souza YM, Galvao M, Murakami AH, Silva AC, et al. Laparoscopic duodenal-jejunal exclusion in the treatment of type 2 diabetes mellitus in patients with BMI<30 kg/m2 (LBMI). Obes Surg. 2009;19(3):307–12. Epub 2008/11/07. 10.1007/s11695-008-9759-5 . [DOI] [PubMed] [Google Scholar]
- 8. Kim Z, Hur KY. Laparoscopic mini-gastric bypass for type 2 diabetes: the preliminary report. World J Surg. 2011;35(3):631–6. Epub 2010/12/18. 10.1007/s00268-010-0909-2 . [DOI] [PubMed] [Google Scholar]
- 9. Navarrete SA, Leyba JL, Llopis SN. Laparoscopic sleeve gastrectomy with duodenojejunal bypass for the treatment of type 2 diabetes in non-obese patients: technique and preliminary results. Obes Surg. 2011;21(5):663–7. Epub 2011/02/22. 10.1007/s11695-011-0371-8 . [DOI] [PubMed] [Google Scholar]
- 10. Geloneze B, Geloneze SR, Fiori C, Stabe C, Tambascia MA, Chaim EA, et al. Surgery for nonobese type 2 diabetic patients: an interventional study with duodenal-jejunal exclusion. Obes Surg. 2009;19(8):1077–83. Epub 2009/05/29. 10.1007/s11695-009-9844-4 . [DOI] [PubMed] [Google Scholar]
- 11. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. Epub 2000/05/02. . [DOI] [PubMed] [Google Scholar]
- 12.Wells G SB, O’Connell D, Peterson J, Welch V. The NewcastleOttawa Scale (NOS) for assessing the quality of nonrandomised studies in metaanalyses.: In.: Ottawa Hospital Research Institute.
- 13. DePaula AL, Macedo AL, Mota BR, Schraibman V. Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21–29. Surg Endosc. 2009;23(6):1313–20. Epub 2008/10/03. 10.1007/s00464-008-0156-x . [DOI] [PubMed] [Google Scholar]
- 14. Dixon JB, Hur KY, Lee WJ, Kim MJ, Chong K, Chen SC, et al. Gastric bypass in Type 2 diabetes with BMI < 30: weight and weight loss have a major influence on outcomes. Diabet Med. 2013;30(4):e127–34. Epub 2013/01/03. 10.1111/dme.12107 . [DOI] [PubMed] [Google Scholar]
- 15. Shrestha C, He H, Liu Y, Zhu S, Xiong J, Mo Z. Changes in Adipokines following Laparoscopic Roux-en-Y Gastric Bypass Surgery in Chinese Individuals with Type 2 Diabetes Mellitus and BMI of 22–30 kg.m(-2.). Int J Endocrinol. 2013;2013:240971 Epub 2013/05/22. 10.1155/2013/240971 ; PubMed Central PMCID: PMCPmc3652206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garcia-Caballero M, Valle M, Martinez-Moreno JM, Miralles F, Toval JA, Mata JM, et al. Resolution of diabetes mellitus and metabolic syndrome in normal weight 24–29 BMI patients with One Anastomosis Gastric Bypass. Nutr Hosp. 2012;27(2):623–31. Epub 2012/06/27. 10.1590/s0212-16112012000200041 . [DOI] [PubMed] [Google Scholar]
- 17. Scopinaro N, Adami GF, Papadia FS, Camerini G, Carlini F, Briatore L, et al. The effects of biliopancreatic diversion on type 2 diabetes mellitus in patients with mild obesity (BMI 30–35 kg/m2) and simple overweight (BMI 25–30 kg/m2): a prospective controlled study. Obes Surg. 2011;21(7):880–8. Epub 2011/05/05. 10.1007/s11695-011-0407-0 . [DOI] [PubMed] [Google Scholar]
- 18. Lee HC, Kim MK, Kwon HS, Kim E, Song KH. Early changes in incretin secretion after laparoscopic duodenal-jejunal bypass surgery in type 2 diabetic patients. Obes Surg. 2010;20(11):1530–5. Epub 2010/08/31. 10.1007/s11695-010-0248-2 . [DOI] [PubMed] [Google Scholar]
- 19. Dixon JB, Zimmet P, Alberti KG, Rubino F. Bariatric surgery: an IDF statement for obese Type 2 diabetes. Diabet Med. 2011;28(6):628–42. Epub 2011/04/13. 10.1111/j.1464-5491.2011.03306.x ; PubMed Central PMCID: PMCPmc3123702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li Q, Chen L, Yang Z, Ye Z, Huang Y, He M, et al. Metabolic effects of bariatric surgery in type 2 diabetic patients with body mass index < 35 kg/m2. Diabetes Obes Metab. 2012;14(3):262–70. Epub 2011/11/05. 10.1111/j.1463-1326.2011.01524.x . [DOI] [PubMed] [Google Scholar]
- 21. Shimizu H, Timratana P, Schauer PR, Rogula T. Review of Metabolic Surgery for Type 2 Diabetes in Patients with a BMI < 35 kg/m(2). J Obes. 2012;2012:147256 Epub 2012/06/22. 10.1155/2012/147256 ; PubMed Central PMCID: PMCPmc3375149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Reis CE, Alvarez-Leite JI, Bressan J, Alfenas RC. Role of bariatric-metabolic surgery in the treatment of obese type 2 diabetes with body mass index <35 kg/m2: a literature review. Diabetes Technol Ther. 2012;14(4):365–72. Epub 2011/12/20. 10.1089/dia.2011.0127 . [DOI] [PubMed] [Google Scholar]
- 23. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. Epub 2004/01/17. 10.1016/s0140-6736(03)15268-3 . [DOI] [PubMed] [Google Scholar]
- 24. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. Epub 2009/03/21. 10.1016/s0140-6736(09)60318-4 ; PubMed Central PMCID: PMCPmc2662372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88 Epub 2009/03/27. 10.1186/1471-2458-9-88 ; PubMed Central PMCID: PMCPmc2667420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim WS, Kim JW, Ahn CW, Choi SH. Resolution of type 2 diabetes after gastrectomy for gastric cancer with long limb Roux-en Y reconstruction: a prospective pilot study. J Korean Surg Soc. 2013;84(2):88–93. Epub 2013/02/12. 10.4174/jkss.2013.84.2.88 ; PubMed Central PMCID: PMCPmc3566474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim JW, Cheong JH, Hyung WJ, Choi SH, Noh SH. Outcome after gastrectomy in gastric cancer patients with type 2 diabetes. World J Gastroenterol. 2012;18(1):49–54. Epub 2012/01/10. 10.3748/wjg.v18.i1.49 ; PubMed Central PMCID: PMCPmc3251805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang GF, Yan YX, Xu N, Yin D, Hui Y, Zhang JP, et al. Predictive factors of type 2 diabetes mellitus remission following bariatric surgery: a meta-analysis. Obes Surg. 2015;25(2):199–208. Epub 2014/08/12. 10.1007/s11695-014-1391-y ; PubMed Central PMCID: PMCPmc4297287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yu J, Zhou X, Li L, Li S, Tan J, Li Y, et al. The long-term effects of bariatric surgery for type 2 diabetes: systematic review and meta-analysis of randomized and non-randomized evidence. Obes Surg. 2015;25(1):143–58. Epub 2014/10/31. 10.1007/s11695-014-1460-2 . [DOI] [PubMed] [Google Scholar]
- 30. Lee WJ, Chong K, Ser KH, Chen JC, Lee YC, Chen SC, et al. C-peptide predicts the remission of type 2 diabetes after bariatric surgery. Obes Surg. 2012;22(2):293–8. Epub 2011/12/06. 10.1007/s11695-011-0565-0 . [DOI] [PubMed] [Google Scholar]
- 31. Cohen RV, Schiavon CA, Pinheiro JS, Correa JL, Rubino F. Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22–34 kg/m2: a report of 2 cases. Surg Obes Relat Dis. 2007;3(2):195–7. Epub 2007/03/28. 10.1016/j.soard.2007.01.009 . [DOI] [PubMed] [Google Scholar]
- 32. Lakdawala M, Shaikh S, Bandukwala S, Remedios C, Shah M, Bhasker AG. Roux-en-Y gastric bypass stands the test of time: 5-year results in low body mass index (30–35 kg/m(2)) Indian patients with type 2 diabetes mellitus. Surg Obes Relat Dis. 2013;9(3):370–8. Epub 2012/10/17. 10.1016/j.soard.2012.07.017 . [DOI] [PubMed] [Google Scholar]
- 33. Robert M, Ferrand-Gaillard C, Disse E, Espalieu P, Simon C, Laville M, et al. Predictive factors of type 2 diabetes remission 1 year after bariatric surgery: impact of surgical techniques. Obes Surg. 2013;23(6):770–5. Epub 2013/01/29. 10.1007/s11695-013-0868-4 . [DOI] [PubMed] [Google Scholar]
- 34. Casella G, Abbatini F, Cali B, Capoccia D, Leonetti F, Basso N. Ten-year duration of type 2 diabetes as prognostic factor for remission after sleeve gastrectomy. Surg Obes Relat Dis. 2011;7(6):697–702. Epub 2011/10/18. 10.1016/j.soard.2011.08.014 . [DOI] [PubMed] [Google Scholar]
- 35. Hayes MT, Hunt LA, Foo J, Tychinskaya Y, Stubbs RS. A model for predicting the resolution of type 2 diabetes in severely obese subjects following Roux-en Y gastric bypass surgery. Obes Surg. 2011;21(7):910–6. Epub 2011/02/22. 10.1007/s11695-011-0370-9 . [DOI] [PubMed] [Google Scholar]
- 36. Kim S, Richards WO. Long-term follow-up of the metabolic profiles in obese patients with type 2 diabetes mellitus after Roux-en-Y gastric bypass. Ann Surg. 2010;251(6):1049–55. Epub 2010/05/21. 10.1097/SLA.0b013e3181d9769b . [DOI] [PubMed] [Google Scholar]
- 37. Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337–72. Epub 2013/03/27. 10.4158/ep12437.gl ; PubMed Central PMCID: PMCPmc4140628. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
BAGUA = one anastomosis gastric bypass; BPD = biliopancreatic diversion; DJB = duodenojejunal bypass; LII-DSG = laparoscopic sleeve gastrectomy; LMGB = laparoscopic mini gastric bypass; RYGB = roux-en-Y gastric bypass.
(DOCX)
LDL = low-density lipoprotein; NA = not available.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.