Abstract
Antenatal mental disorders compromise maternal and child health, and women who have experienced childhood trauma may be at increased risk for such disorders. One hypothesis is that early trauma leads to the development and use of maladaptive coping strategies as an adult, which in turn could predict mental health difficulties during stressful transitions such as pregnancy. To test this hypothesis, this study examined the relationship between childhood trauma and mental health (depression, PTSD) in a sample of 84 pregnant women seeking antenatal care in Cape Town, South Africa, and explored whether maladaptive coping mediated this relationship. The majority of women (62%) met established criteria for antenatal depression and 30% for antenatal PTSD; in addition, 40% reported a history of childhood trauma. Childhood trauma, especially childhood sexual abuse and emotional abuse, was significantly associated with depression and PTSD. The relationships between childhood trauma and depression and PTSD were significantly mediated by maladaptive coping, even when adjusted for the woman’s age, gestational age, and HIV status. Findings highlight the need for coping-based interventions to prevent and treat antenatal mental disorders among women with childhood trauma, particularly in high-trauma settings such as South Africa.
Keywords: South Africa, pregnancy, trauma, depression, PTSD, coping
BACKGROUND
Maternal mental health during pregnancy impacts the wellbeing of both mother and child. Antenatal mental disorders such as depression and PTSD are linked to obstetric risks such as pre-term delivery (Grigoriadis et al., 2013; Straub, Adams, Kim, & Silver, 2012), pre-eclampsia (Kurki, Hiilesmaa, Raitasalo, Mattila, & Ylikorkala, 2000), and negative child outcomes including poor neonatal health (Misri et al., 2004), stunted infant growth (Grote et al., 2010; Stewart, 2007), and compromised development (Deave, Heron, Evans, & Emond, 2008). Moreover, antenatal mental disorders have been observed to be prevalent in low- and middle-income countries (Fisher et al., 2012), and contribute to a heavy burden of child and maternal consequences in these settings (Patel, DeSouza, & Rodrigues, 2003; Rahman, Bunn, Lovel, & Creed, 2007). South Africa is one such setting where mental disorders, particularly depression, have been detected at high levels among pregnant women (Hartley et al., 2011; Rochat, Tomlinson, Barnighausen, Newell, & Stein, 2011; Vythilingum, Roos, Faure, Geerts, & Stein, 2012). Less is known about the prevalence and predictors of antenatal PTSD among South African women, as well as behavioral opportunities for addressing either of these psychological morbidities during the pregnancy period.
One key factor that likely contributes to antenatal depression and PTSD in the South African setting is trauma history. South Africa is known to have high rates of interpersonal trauma (Gass, Stein, Williams, & Seedat, 2011; Jewkes & Abrahams, 2002; Jewkes, Penn-Kekana, Levin, Ratsaka, & Schrieber, 2001). In other settings, a history of interpersonal trauma has been associated with higher risk of mental disorders, both in general (Kaplow & Widom, 2007) and during the perinatal period (Howard, Oram, Galley, Trevillion, & Feder, 2013). Consistent with this, a recent South African study (Hartley et al., 2011) found that a strong predictor of antenatal depression was exposure to intimate partner violence (IPV). Not previously investigated in this setting, though, is the role of earlier life adversities such as childhood trauma in predicting antenatal mental health. Unfortunately, childhood trauma occurs at high rates in South Africa – with over a third of South African women reporting a history of childhood sexual abuse (Seedat, Van Niekerk, Jewkes, Suffla, & Ratele, 2009) – and has been linked to poor health and psychological outcomes (Troeman et al., 2011). Evidence suggests that childhood trauma may independently influence perinatal mental health regardless of recent victimization (Huth-Bocks, Krause, Ahlfs-Dunn, Gallagher, & Scott, 2013; Malta, McDonald, Hegadoren, Weller, & Tough, 2012) and must be examined for its specific impact during pregnancy. For example, a history of childhood trauma may raise stressful memories or cognitions during the transition to parenthood, which in turn could increase vulnerability for depression or PTSD especially in a context already fraught with stressors such as poverty, violence, and HIV (Shisana et al., 2014; Shisana, Rice, Zungu, & Zuma, 2010).
Given this constellation of stressors, one question that remains is how South African women cope during pregnancy, and whether this influences their mental health status. Coping strategies can be defined as cognitive and behavioral efforts to manage stressful demands (Folkman & Lazarus, 1986), and coping styles reflect the tendency to select certain strategies in the face of such demands (Carver, Scheier, & Weintraub, 1989). Coping strategies have been categorized broadly in different ways – active or passive, approach or avoidant, problem-focused or emotion-focused, as well as adaptive or maladaptive (Endler & Parker, 1994; Roth & Cohen, 1986; Zeidner & Saklofske, 1996). Trauma survivors tend to use maladaptive coping strategies, such as avoidance, self-blame and substance use, to cope with distressing memories of their traumatic experiences (Street, Gibson, & Holohan, 2005). While these strategies may reduce immediate distress, they can worsen long-term mental health symptoms (Briere & Elliott, 1994; Simoni & Ng, 2000). A tendency to use maladaptive coping strategies is thus expected to negatively influence mental health among pregnant women who report trauma histories. Yet limited literature exists on how women in low-income settings cope during pregnancy (Dunkel Schetter, 2011) and especially how maladaptive coping affects mental health in a high-trauma setting such as South Africa.
Research is needed to specifically examine the impact of childhood trauma and coping on perinatal mental health among South African women. In a sample of 84 pregnant South African women, this study aimed to (1) examine childhood trauma as a predictor of depression and PTSD symptoms during pregnancy; and (2) explore whether the impact of childhood trauma on these symptoms was mediated by maladaptive coping style. Findings from this study may help guide interventions to treat and prevent antenatal mental disorders in this high-risk population, thereby optimizing maternal and child outcomes.
METHODS
Setting
The study was conducted in Cape Town, South Africa. Participants were recruited from an antenatal clinic in a peri-urban area where HIV prevalence among pregnant women is estimated around 20% (National Department of Health, 2013). The clinic serves a primarily low-income, Black community, and was selected based on existing partnerships, available resources, and proximity to central Cape Town. Access to the clinic was granted by the hospital administration.
Design
Pregnant women were approached in the clinic by research staff while waiting for a routine antenatal care (ANC) visit. Eligibility criteria for this study included: (1) current pregnancy, (2) known HIV status, (3) Xhosa, Afrikaans, or English fluency, and (4) no cognitive impairment. Participants with an obstetric emergency were excluded from the study. Due to an initial interest in HIV status as a study variable, HIV-positive women were intentionally oversampled. All eligible women approached agreed to participate and provided informed consent. The study coordinator orally administered the questionnaires in participants’ preferred language (Xhosa, Afrikaans, English) in a private room at the clinic. On average, the survey took 45–60 minutes and did not interrupt participants from receiving their ANC care in a timely fashion. Participants received 50 South African Rands (approximately 5 USD) for their participation. All procedures were approved by the institutional review boards at [BLINDED FOR SUBMISSION].
Measures
Demographic information
Participants were asked to report their age, gestational age (in weeks), relationship status, education level, current employment, and HIV status.
Childhood trauma history
Childhood trauma was measured using the Childhood Trauma Questionnaire Short Form (CTQ-SF), a 28-item retrospective self-report questionnaire (Bernstein et al., 2003). The CTQ-SF yields five separate subscales that measure experiences of childhood physical abuse, sexual abuse, emotional abuse, emotional neglect, and physical neglect, each consisting of five items. An overall trauma score is created by summing the five subscales, with possible scores ranging from 25–125. For this study, the continuous overall trauma score was used as the main childhood trauma variable. A dichotomous variable reflecting the presence/absence of overall childhood trauma was created for descriptive purposes, with participants categorized in the “no trauma” group if they had a score of 25–40, and in the “trauma” group if they had a score of 41 or higher. Dichotomous variables for each subtype of childhood trauma were also created, using the following cut-off scores: physical abuse ≥ 8, sexual abuse ≥ 6, emotional abuse ≥ 9, physical neglect ≥ 8, and emotional neglect ≥ 10 (Bernstein & Fink, 1998).
Antenatal depression
Antenatal depression was assessed using the Edinburgh Postnatal Depression Scale (EPDS), a 10-item screening tool for depression during pregnancy and through the first postpartum year. The EPDS has previously been used in South Africa for detecting antenatal depression (Hartley et al., 2011; Vythilingum et al., 2013). Items are scored on a four-point scale ranging from 0 to 3, with reverse-scoring on select items. Item scores are then summed to create a total score ranging from 0 to 30, with higher scores indicative of greater depressive symptomology. Based on previous research in this setting (Hung et al., 2014; Rochat, Tomlinson, Newell, & Stein, 2013), an EPDS score of ≥13 was used as the descriptive cut-off for antenatal depression.
PTSD symptoms
The severity and frequency of PTSD symptoms occurring in the past week were measured using the Davidson Trauma Scale, a 17-item self-report scale (Davidson et al., 1997). A total PTSD score is created by summing all items on the scale, with possible scores ranging from 0 to 136. A cut-off of 40 or more is used as a cut-off for likely PTSD diagnosis (Davidson et al., 1997), and was used to create a dichotomous variable for descriptive purposes.
Maladaptive coping style
Coping styles were measured using the Brief COPE (Carver, 1997), which consists of 28 items. To create the maladaptive coping subscale, we summed 12 relevant items from six subscales (Self-Distraction, Denial, Substance Use, Behavioral Disengagement, Venting, and Self-Blame) to form a composite score, as done in some previous research (Kasi et al., 2012; Moore, Biegel, & McMahon, 2011). Internal consistency was high in this sample, with a Cronbach’s alpha of .80 for the 12 items. Possible scores on this subscale ranged from 12 to 48, with higher scores reflecting greater tendency to use these maladaptive coping strategies. Given the absence of established cut-offs for this subscale, the continuous variable was used for descriptive purposes.
Analysis
All analyses were conducted using SPSS (SPSS IBM v. 21.0, Armonk, NY). We first extracted descriptive statistics for demographic, mental health, and childhood trauma variables. Then we explored correlations between antenatal mental health scores and relevant predictors and covariates.
To assess mediation in a regression framework, we followed the steps outlined by Baron and Kenny (1986) for each mental health outcome, and used a bootstrapping method to statistically test the significance of observed indirect effects. We first estimated the overall effect of childhood trauma on the outcome, antenatal depression (c effect). Second, we tested the unique relationship between childhood trauma and the proposed mediator, maladaptive coping (a effect). Third, we tested the unique relationship between maladaptive coping and antenatal depression (b effect). Finally, we re-estimated the overall effect of childhood trauma on antenatal depression adjusting for the effect of maladaptive coping (c’ effect). If mediation is present, the first three estimated effects (a, b, c) should be statistically significant and the adjusted c’ effect is expected to be smaller than the original c effect. If the c’ effect is reduced but still significant, then partial mediation is suggested; if non-significant and zero, then complete mediation is suggested (Baron & Kenny, 1986). After examining the reduction of the c’ effect relative to the c effect, we computed the mediated effect (ab) using unstandardized coefficients, and tested the significance of this effect with 95% bias-corrected bootstrap confidence intervals, using the INDIRECT Macro for SPSS (Preacher & Hayes, 2004). Then, we applied the formula ab/c to estimate the proportion of the relationship between childhood trauma and antenatal depression that was mediated by maladaptive coping. Finally, we reran the INDIRECT Macro to test the direct and indirect effects adjusted for covariates of theoretical relevance, i.e., woman’s age, gestational age, and HIV status (Kapetanovic, Dass-Brailsford, Nora, & Talisman, 2014; Lee et al., 2007; Rich-Edwards et al., 2006). This entire sequence of mediation analyses was repeated using PTSD as the outcome.
RESULTS
Description of the Sample
Among the 84 participants (Table 1), most reported being in a relationship; among these, the majority indicated they were unmarried. Only 8% of the sample had education beyond the high school level. Most participants were currently unemployed and had a monthly income below 5000 South African Rands (approximately 477 USD). On average, reported gestational age was 26 weeks (SD=6, range=6–36). Since HIV-infected women were initially oversampled, many (60%) reported being HIV-positive.
Table 1.
Sample characteristics
| Variable | N (%) |
|---|---|
| Age | |
| <18 | 3 (3) |
| 18–25 | 46 (52) |
| 26–35 | 35 (40) |
| 36+ | 4 (5) |
| HIV-positive | 52 (60) |
| Relationship status | |
| Single | 5 (6) |
| Married | 15 (17) |
| In a relationship | 67 (77) |
| Education | |
| Primary school | 13 (15) |
| High school | 68 (77) |
| Tertiary education | 7 (8) |
| Unemployed | 63 (72) |
| Monthly income below 5000 rand | 73 (83) |
| Gestational age; mean (SD) | 26 (6) |
| EPDS score ≥13 | 52 (62) |
| DTS score ≥ 40 | 26 (31) |
Forty percent reported overall childhood trauma, as determined with a cutoff score of 41 or higher on the CTQ (Table 2). The mean CTQ score for the sample was 40 (SD=11.1), and scores ranged from 25–80. Notably, 56% of the sample reported physical neglect and almost half of all participants reported emotional abuse (44%) and emotional neglect (48%) during childhood. About one in four participants reported childhood physical (30%) and sexual (26%) abuse. Psychological distress was also common among participants, with 62% meeting the cut-off for antenatal depression and 30% meeting the cut-off for PTSD. Almost one in four (23%) participants met criteria for both disorders and could be classified as having comorbid depression and PTSD.
Table 2.
Proportion of sample having experienced childhood trauma
| CTQ1 Scale | N (%) |
|---|---|
| Physical abuse | 26 (29.5) |
| Sexual abuse | 23 (26.1) |
| Emotional abuse | 39 (44.3) |
| Physical neglect | 49 (55.7) |
| Emotional neglect | 42 (47.7) |
| Overall trauma | 35 (39.8) |
| Overall trauma score | Mean: 40.3 ± 11.1, Range: 25 – 80 |
CTQ= Childhood Trauma Questionnaire
Variables Associated with Antenatal Depression and PTSD
Antenatal depression was significantly correlated with earlier gestational age, overall childhood trauma score, and maladaptive coping style (Table 3). Among trauma subtypes, antenatal depression was associated specifically with childhood sexual and emotional abuse. Antenatal PTSD symptoms were significantly correlated with overall childhood trauma and maladaptive coping (Table 3). Among trauma subtypes, antenatal PTSD was associated with childhood sexual and emotional abuse, as well as physical abuse.
Table 3.
Correlations between antenatal mental health and study variables
| Depression | PTSD | |||
|---|---|---|---|---|
| Coefficient | p-value | Coefficient | p-value | |
| HIV status | −.01 | .92 | .02 | .83 |
| Age | .05 | .65 | .08 | .50 |
| Gestational age | −.25 | .02* | .00 | .98 |
| Overall CTQ score | .23 | .03* | .40 | .00** |
| Child physical abuse | .21 | .06 | .29 | .01** |
| Child sexual abuse | .25 | .02* | .36 | .00** |
| Child emotional abuse | .33 | .00** | .41 | .00** |
| Child emotional neglect | −.00 | .96 | .18 | .11 |
| Child physical neglect | −.01 | .93 | .21 | .06 |
| Maladaptive coping style | .35 | .00** | .49 | .00** |
Statistically significant at p<.05
Maladaptive Coping as a Mediator between Childhood Trauma and Antenatal Mental Health
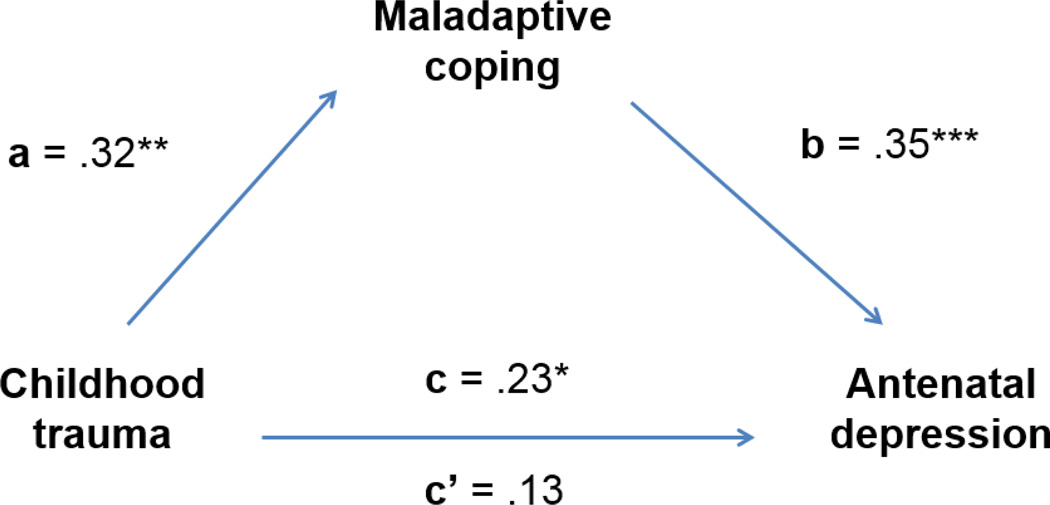
Considering antenatal depression as the outcome, all estimated effects in the mediation model (Figure 1) were found to be significant. Childhood trauma predicted maladaptive coping (a effect = .22, p = .005), and in turn maladaptive coping predicted antenatal depression (b effect = .22, p = .001). Overall, childhood trauma predicted antenatal depression (c effect = .11, p = .04), but its effect on antenatal depression was reduced by almost half and became non-significant when adjusted for the effect of maladaptive coping (c’ effect = .06, p = n.s.), suggesting substantial mediation. This was supported by the indirect effects test and the 95% bias-corrected bootstrap confidence intervals, ab = .05, 95% CI [.01, .10]. According to calculations (ab/c), 45% of the effect of childhood trauma on antenatal depression was mediated by maladaptive coping. The direct and indirect effects remained significant when adjusted for covariates, with gestational age emerging also as a significant predictor of depression, B = −.17, p = .03, such that women with more advanced pregnancies had significantly lower depression scores.
Figure 1.
Mediation model for antenatal depression outcome
Note: Standardized regression coefficients shown.
* p < .05, **p < .01, ***p ≤ .001
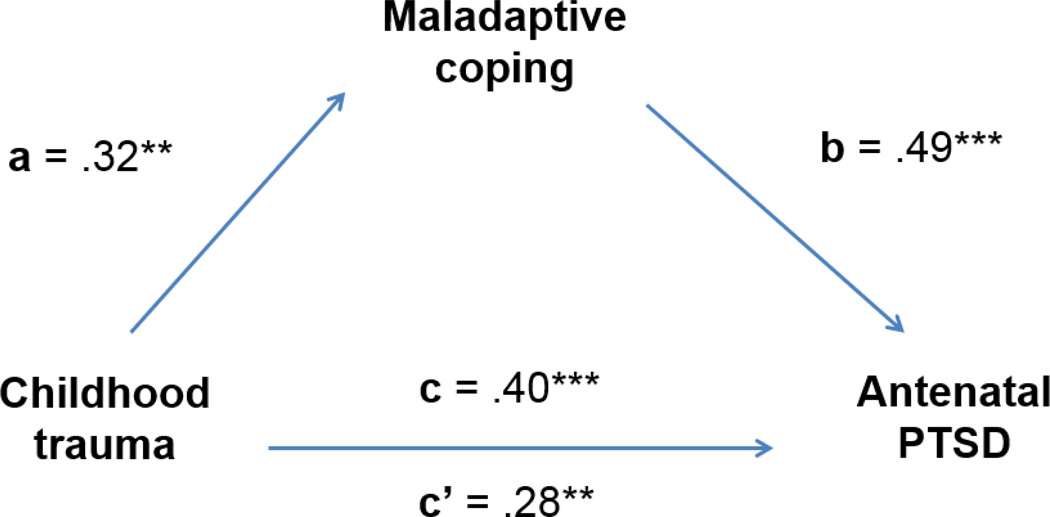
Considering antenatal PTSD as the outcome, all estimated effects in the mediation model (Figure 2) were found to be significant. As before, childhood trauma predicted maladaptive coping (a effect = .22, p = .005), and maladaptive coping also strongly predicted antenatal PTSD (b effect = 1.73, p < .001). The overall effect of childhood trauma on antenatal PTSD was significant (c effect = .99, p < .001) and was slightly reduced, though remained significant, when maladaptive coping was included in the model (c’ effect = .67, p = .008), suggesting partial mediation. This was supported by the indirect effects test and the 95% bias-corrected bootstrap confidence intervals, ab = .38, 95% CI [.11, .64]. According to calculations (ab/c), 38% of the effect of childhood trauma on antenatal PTSD was mediated by maladaptive coping. In addition, the direct and indirect effects remained significant when adjusted for covariates, with none of the covariates emerging as predictors of PTSD.
Figure 2.
Mediation model for antenatal PTSD outcome
Note: Standardized regression coefficients shown.
* p < .05, **p < .01, ***p ≤ .001
DISCUSSION
This study examined the relationship between childhood trauma, maladaptive coping, and mental health in a sample of South African women seeking antenatal care. Pregnant participants were characterized not only by sociodemographic risk in terms of poverty and low education, but also by high levels of childhood trauma and psychological distress in the forms of PTSD (30%) and depression (62%), occurring both independently and comorbidly.
We found that childhood trauma history was predictive of both depression and PTSD symptoms during pregnancy. In particular, childhood sexual abuse and emotional abuse were associated with both depression and PTSD, while childhood physical abuse was associated only with PTSD. These associations during pregnancy, novel to the South African context, expand the research base from developed settings in which early maltreatment has been found to be a risk factor for mental disorders in the perinatal period (Benedict, Paine, Paine, Brandt, & Stallings, 1999; Huth-Bocks et al., 2013; Kulkarni, Graham-Bermann, Rauch, & Seng, 2011; Meltzer-Brody et al., 2013). A history of childhood trauma may predict antenatal mental health in various ways. For example, though we were unable to test this hypothesis in the current study, women who have experienced childhood trauma may be more likely to be victimized as adults (Desai, Arias, Thompson, & Basile, 2002), which can then more proximally predict mental health during pregnancy.
Results from this study suggested that another pathway by which another childhood trauma may affect antenatal mental health is via coping behavior. In general, women with a history of childhood trauma are more likely to use maladaptive coping strategies (Street et al., 2005), a tendency which was confirmed in our pregnant sample. Childhood trauma could lead to the development and utilization of maladaptive coping strategies as an adult, which may then be both a behavioral mechanism and exacerbating factor for antenatal mental health problems. In mediation analyses, maladaptive coping emerged as a significant mediator of the relationship between childhood trauma and both mental health outcomes, especially depression. For depression, accounting for maladaptive coping rendered the effect of childhood trauma insignificant, while for PTSD, the effect of childhood trauma remained significant. Among South African women who have experienced childhood trauma, maladaptive coping seems to be a key target for preventing and/or treating antenatal depression. On the other hand, given that maladaptive coping did not nullify the relationship between childhood trauma and PTSD, this finding suggests that intervening on maladaptive coping alone is helpful but not necessarily sufficient for addressing PTSD among pregnant women who have experienced childhood trauma.
In this study, we chose to examine antenatal depression and PTSD as separate mental health outcomes, despite some overlap in their occurrence and symptom construct (Gros, Price, Magruder, & Frueh, 2012). Our findings characterized PTSD and depression as sufficiently distinct psychological outcomes. For example, we found that depression and PTSD were differentially related to maladaptive coping as a mediator, as discussed previously, with a stronger mechanism of coping for depression. In addition, depression was predicted by the woman’s gestational age, while PTSD was not. Women who were more advanced in their pregnancy tended to have lower levels of depression. Recent research in this setting has revealed that pregnancy recognition can be a stressful and often undesirable experience (Choi et al., 2014; Watt et al., 2014), so it is possible that women who are further along in their pregnancy may have more time to reconcile with their pregnancy status and adjust to the stressors brought on by pregnancy. Notably, however, one in four women in the sample did present with comorbid antenatal depression and PTSD. Comorbid depression and PTSD during pregnancy can be especially harmful for perinatal health, as one recent study found that a combined diagnosis of depression and PTSD quadrupled the risk of preterm delivery (Yonkers et al., 2014). Future work must explore this co-occurrence and how to treat both conditions simultaneously in South Africa (Abler et al., 2014).
This study had several limitations to note. First of all, the modest sample size precluded the use of formal structural modeling to test mediation. Second, we were unable to test other potential mediators (e.g., recent partner violence), which were not measured but have been previously associated with negative perinatal outcomes in South Africa (Koen et al., 2014). Third, we oversampled HIV-positive women, which raises questions about population representativeness – though we found that HIV status was not related to antenatal mental health. While surprising based on the overall literature (Kapetanovic et al., 2014; Spies et al., 2012), our findings were consistent with a recent South African study (Rochat et al., 2011) that found both HIV-infected and non-infected women to be similarly at risk for antenatal depression, suggesting there may be other factors that override the psychological impact of HIV status in this setting.
Despite the limitations, this study had several important strengths. To our knowledge, it is one of the first to look at predictors of antenatal PTSD symptoms in South Africa, particularly childhood trauma, despite the high prevalence of interpersonal and community trauma in South Africa (Gass et al., 2011; Jewkes & Abrahams, 2002; Jewkes et al., 2001). It used a gold-standard instrument to measure childhood trauma, and drew on validated screening instruments to assess mental health outcomes. In addition, it explored the role of coping in mental health during pregnancy, which has important implications for developing and tailoring behavioral interventions but has not received sufficient attention to date, especially in low-resource populations (Dunkel Schetter, 2011).
In terms of intervention implications, this study highlighted maladaptive coping style as a useful target among these women. Reducing maladaptive coping among pregnant women with trauma histories and/or promoting positive alternative coping strategies may make a difference for mental health, especially depression. Interventions should also address women’s trauma histories and symptoms for PTSD. Future areas of research include evaluating the effectiveness of coping-based interventions for pregnant women who have experienced childhood trauma. Research studies are also needed to examine whether specific forms of maladaptive coping (e.g., substance use, denial, etc.) are more common among pregnant women with trauma histories. Ecological momentary assessment (EMA) studies (Shiffman, Stone, & Hufford, 2008) may be useful in this population to track women’s coping behaviors in relation to various stressors and symptoms. In addition, qualitative research may illuminate the motivations underlying the selection of certain coping strategies, thereby pointing to further intervention avenues.
Conclusion
High rates of childhood trauma, antenatal depression and PTSD exist among South African women receiving antenatal care. This study suggests that childhood trauma may lead to the development of maladaptive coping styles as an adult, which can then lead to and/or exacerbate mental health difficulties during pregnancy, a stressful time for many women in this setting. Findings raise the importance of addressing maladaptive coping among trauma-exposed mothers in order to improve antenatal mental health and its related outcomes.
Acknowledgements
We are grateful to the women who participated in this study. In addition, we acknowledge the Duke Center for AIDS Research (NIAID grant P30-AI064518) and a grant (R34 MH102001) from the National Institute of Mental Health (NIMH), for support in the preparation of this manuscript.
References
- Abler LA, Sikkema KJ, Watt MH, Eaton LA, Choi KW, Kalichman SC, Skinner D, Pieterse D. Longitudinal cohort study of depression, post-traumatic stress, and alcohol use in South African women who attend alcohol serving venues. BMC Psychiatry. 2014;14(1):224. doi: 10.1186/s12888-014-0224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benedict MI, Paine LL, Paine LA, Brandt D, Stallings R. The association of childhood sexual abuse with depressive symptoms during pregnancy, and selected pregnancy outcomes. Child Abuse and Neglect. 1999;23(7):659–670. doi: 10.1016/s0145-2134(99)00040-x. [DOI] [PubMed] [Google Scholar]
- Bernstein D, Fink L. Manual for the childhood trauma questionnaire. New York: The Psychological Corporation; 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Briere JN, Elliott DM. Immediate and long-term impacts of child sexual abuse. The future of children. 1994:54–69. [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Choi KW, Abler LA, Watt MH, Eaton LA, Kalichman SC, Skinner D, Pieterse D, Sikkema KJ. Drinking before and after pregnancy recognition among South African women: the moderating role of traumatic experiences. BMC Pregnancy and Childbirth. 2014;14:97. doi: 10.1186/1471-2393-14-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JR, Book S, Colket J, Tupler L, Roth S, David D, Hertzberg M, Mellman T, Beckham J, Smith R. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine. 1997;27(01):153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- Deave T, Heron J, Evans J, Emond A. The impact of maternal depression in pregnancy on early child development. BJOG: An International Journal of Obstetrics and Gynaecology. 2008;115(8):1043–1051. doi: 10.1111/j.1471-0528.2008.01752.x. [DOI] [PubMed] [Google Scholar]
- Desai S, Arias I, Thompson MP, Basile KC. Childhood victimization and subsequent adult revictimization assessed in a nationally representative sample of women and men. Violence and Victims. 2002;17(6):639–653. doi: 10.1891/vivi.17.6.639.33725. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Endler NS, Parker JD. Assessment of multidimensional coping: Task, emotion, and avoidance strategies. Psychological Assessment. 1994;6(1):50. [Google Scholar]
- Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization. 2012;90(2):139G–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Stress-processes and depressive symptomatology. Journal of Abnormal Psychology. 1986;95(2):107–113. doi: 10.1037//0021-843x.95.2.107. [DOI] [PubMed] [Google Scholar]
- Gass JD, Stein DJ, Williams DR, Seedat S. Gender differences in risk for intimate partner violence among South African adults. J Interpers Violence. 2011;26(14):2764–2789. doi: 10.1177/0886260510390960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, Steiner M, Mousmanis P, Cheung A, Radford K, Martinovic J, Ross LE. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. Journal of Clinical Psychiatry. 2013;74(4):e321–e341. doi: 10.4088/JCP.12r07968. [DOI] [PubMed] [Google Scholar]
- Gros DF, Price M, Magruder KM, Frueh BC. Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Research. 2012;196(2–3):267–270. doi: 10.1016/j.psychres.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, le Roux I, Mbewu N, Rotheram-Borus MJ. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health. 2011;8:9. doi: 10.1186/1742-4755-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard LM, Oram S, Galley H, Trevillion K, Feder G. Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Medicine. 2013;10(5):e1001452. doi: 10.1371/journal.pmed.1001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung KJ, Tomlinson M, le Roux IM, Dewing S, Chopra M, Tsai AC. Community-based prenatal screening for postpartum depression in a South African township. International Journal of Gynecology & Obstetrics. 2014 doi: 10.1016/j.ijgo.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huth-Bocks AC, Krause K, Ahlfs-Dunn S, Gallagher E, Scott S. Relational trauma and posttraumatic stress symptoms among pregnant women. Psychodyn Psychiatry. 2013;41(2):277–301. doi: 10.1521/pdps.2013.41.2.277. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Abrahams N. The epidemiology of rape and sexual coercion in South Africa: an overview. Social Science and Medicine. 2002;55(7):1231–1244. doi: 10.1016/s0277-9536(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Penn-Kekana L, Levin J, Ratsaka M, Schrieber M. Prevalence of emotional, physical and sexual abuse of women in three South African provinces. South African Medical Journal. 2001;91(5):421–428. [PubMed] [Google Scholar]
- Kapetanovic S, Dass-Brailsford P, Nora D, Talisman N. Mental Health of HIV-Seropositive Women During Pregnancy and Postpartum Period: A Comprehensive Literature Review. AIDS and Behavior. 2014;18(6):1152–1173. doi: 10.1007/s10461-014-0728-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116(1):176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- Kasi PM, Naqvi HA, Afghan AK, Khawar T, Khan FH, Khan UZ, Khuwaja UB, Kiani J, Khan HM. Coping Styles in Patients with Anxiety and Depression. ISRN psychiatry. 2012;2012 doi: 10.5402/2012/128672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koen N, Wyatt GE, Williams JK, Zhang M, Myer L, Zar HJ, Stein DJ. Intimate partner violence: associations with low infant birthweight in a South African birth cohort. Metabolic Brain Disease. 2014;29(2):281–299. doi: 10.1007/s11011-014-9525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni MR, Graham-Bermann S, Rauch SA, Seng J. Witnessing versus experiencing direct violence in childhood as correlates of adulthood PTSD. Journal of interpersonal violence. 2011;26(6):1264–1281. doi: 10.1177/0886260510368159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstetrics and Gynecology. 2000;95(4):487–490. doi: 10.1016/s0029-7844(99)00602-x. [DOI] [PubMed] [Google Scholar]
- Lee AM, Lam SK, Lau SMSM, Chong CSY, Chui HW, Fong DYT. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstetrics and Gynecology. 2007;110(5):1102–1112. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]
- Malta LA, McDonald SW, Hegadoren KM, Weller CA, Tough SC. Influence of interpersonal violence on maternal anxiety, depression, stress and parenting morale in the early postpartum: a community based pregnancy cohort study. BMC Pregnancy and Childbirth. 2012;12:153. doi: 10.1186/1471-2393-12-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer-Brody S, Bledsoe-Mansori SE, Johnson N, Killian C, Hamer RM, Jackson C, Wessel J, Thorp J. A prospective study of perinatal depression and trauma history in pregnant minority adolescents. American Journal of Obstetrics and Gynecology. 2013;208(3):211. e211–211. e217. doi: 10.1016/j.ajog.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misri S, Oberlander TF, Fairbrother N, Carter D, Ryan D, Kuan AJ, Reebye P. Relation between prenatal maternal mood and anxiety and neonatal health. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 2004;49(10):684–689. doi: 10.1177/070674370404901006. [DOI] [PubMed] [Google Scholar]
- Moore BC, Biegel DE, McMahon TJ. Maladaptive coping as a mediator of family stress. Journal of social work practice in the addictions. 2011;11(1):17–39. doi: 10.1080/1533256X.2011.544600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Department of Health. The 2012 National Antenatal Sentinel HIV and Herpes Simplex type-2 prevalence Survey, South Africa. Pretoria: 2013. [Google Scholar]
- Patel V, DeSouza N, Rodrigues M. Postnatal depression and infant growth and development in low income countries: a cohort study from Goa, India. Archives of Disease in Childhood. 2003;88(1):34–37. doi: 10.1136/adc.88.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Rahman A, Bunn J, Lovel H, Creed F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatrica Scandinavica. 2007;115(6):481–486. doi: 10.1111/j.1600-0447.2006.00950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, Gillman MW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health. 2006;60(3):221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochat TJ, Tomlinson M, Barnighausen T, Newell ML, Stein A. The prevalence and clinical presentation of antenatal depression in rural South Africa. Journal of Affective Disorders. 2011;135(1–3):362–373. doi: 10.1016/j.jad.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochat TJ, Tomlinson M, Newell M-L, Stein A. Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS) Archives of women's mental health. 2013;16(5):401–410. doi: 10.1007/s00737-013-0353-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth S, Cohen LJ. Approach, avoidance, and coping with stress. American Psychologist. 1986;41(7):813. doi: 10.1037//0003-066x.41.7.813. [DOI] [PubMed] [Google Scholar]
- Seedat M, Van Niekerk A, Jewkes R, Suffla S, Ratele K. Violence and injuries in South Africa: prioritising an agenda for prevention. Lancet. 2009;374(9694):1011–1022. doi: 10.1016/S0140-6736(09)60948-X. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi L, Zuma K, Jooste S, Zungu N, Labadarios D, Onoya D, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press; 2014. [DOI] [PubMed] [Google Scholar]
- Shisana O, Rice K, Zungu N, Zuma K. Gender and poverty in South Africa in the era of HIV/AIDS: a quantitative study. J Womens Health (Larchmt) 2010;19(1):39–46. doi: 10.1089/jwh.2008.1200. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Ng M. Trauma, coping, and depression among women with HIV/AIDS in New York City. AIDS Care. 2000;12(5):567–580. doi: 10.1080/095401200750003752. [DOI] [PubMed] [Google Scholar]
- Spies G, Afifi TO, Archibald SL, Fennema-Notestine C, Sareen J, Seedat S. Mental health outcomes in HIV and childhood maltreatment: a systematic review. Syst Rev. 2012;1:30. doi: 10.1186/2046-4053-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart RC. Maternal depression and infant growth: a review of recent evidence. Matern Child Nutr. 2007;3(2):94–107. doi: 10.1111/j.1740-8709.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straub H, Adams M, Kim JJ, Silver RK. Antenatal depressive symptoms increase the likelihood of preterm birth. American Journal of Obstetrics and Gynecology. 2012;207(4):329 e321–329 e324. doi: 10.1016/j.ajog.2012.06.033. [DOI] [PubMed] [Google Scholar]
- Street AE, Gibson LE, Holohan DR. Impact of childhood traumatic events, trauma-related guilt, and avoidant coping strategies on PTSD symptoms in female survivors of domestic violence. Journal of Traumatic Stress. 2005;18(3):245–252. doi: 10.1002/jts.20026. [DOI] [PubMed] [Google Scholar]
- Troeman ZC, Spies G, Cherner M, Archibald SL, Fennema-Notestine C, Theilmann RJ, Spottiswoode B, Stein DJ, Seedat S. Impact of childhood trauma on functionality and quality of life in HIV-infected women. Health Qual Life Outcomes. 2011;9:84. doi: 10.1186/1477-7525-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vythilingum B, Field S, Kafaar Z, Baron E, Stein D, Sanders L, Honikman S. Screening and pathways to maternal mental health care in a South African antenatal setting. Archives of women's mental health. 2013;16(5):371–379. doi: 10.1007/s00737-013-0343-1. [DOI] [PubMed] [Google Scholar]
- Vythilingum B, Roos A, Faure SC, Geerts L, Stein DJ. Risk factors for substance use in pregnant women in South Africa. South African Medical Journal. 2012;102(11 Pt 1):851–854. doi: 10.7196/samj.5019. [DOI] [PubMed] [Google Scholar]
- Watt MH, Eaton LA, Choi KW, Velloza J, Kalichman SC, Skinner D, Sikkema KJ. "It's better for me to drink, at least the stress is going away": Perspectives on alcohol use during pregnancy among South African women attending drinking establishments. Social Science and Medicine. 2014;116:119–125. doi: 10.1016/j.socscimed.2014.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, Belanger K. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014;71(8):897–904. doi: 10.1001/jamapsychiatry.2014.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidner M, Saklofske D. Adaptive and maladaptive coping. In: Zeidner M, Endler N, editors. Handbook of coping: Theory, research, applications. New York: Wiley; 1996. [Google Scholar]