Abstract
Traumatic brain injury is a major economic burden to hospitals in terms of emergency department visits, hospitalizations, and utilization of intensive care units. Current guidelines for the management of severe traumatic brain injuries are primarily supportive, with an emphasis on surveillance (i.e. intracranial pressure) and preventive measures to reduce morbidity and mortality. There are no direct effective therapies available. Over the last fifteen years, pre-clinical studies in regenerative medicine utilizing cell-based therapy have generated enthusiasm as a possible treatment option for traumatic brain injury. In these studies, stem cells and progenitor cells were shown to migrate into the injured brain and proliferate, exerting protective effects through possible cell replacement, gene and protein transfer, and release of anti-inflammatory and growth factors. In this work, we reviewed the pathophysiological mechanisms of traumatic brain injury, the biological rationale for using stem cells and progenitor cells, and the results of clinical trials using cell-based therapy for traumatic brain injury. Although the benefits of cell-based therapy have been clearly demonstrated in pre-clinical studies, some questions remain regarding the biological mechanisms of repair and safety, dose, route and timing of cell delivery, which ultimately will determine its optimal clinical use.
Keywords: cell-based therapy, stem cells, traumatic brain injury
Editor's key points.
The authors review the mechanisms of traumatic brain injury and the potential place for the use of cell-based therapies.
They conclude that there is a clear potential for benefit, but substantial work remains in optimising cell-based therapy.
In the United States between 2001 and 2010, severe traumatic brain injury (TBI) was responsible for up to 2 200 000 emergency department visits, 300 000 hospitalizations and 55 000 deaths each year. Traumatic brain injuries contributed to 30% of all injury-related deaths in the USA. Their economic burden, including direct medical and indirect costs, was estimated in 2010 to be approximately $76 billion dollars.1 In 2007, the Brain Trauma Foundation and the American Association of Neurological Surgeons published the third edition of evidence-based guidelines for the management of severe TBI.2
However, because of the severe morbidity and mortality associated with TBI, innovative therapies are needed. Based on promising pre-clinical studies and a few completed clinical trials, cell-based therapy may be such a new, innovative, therapeutic approach. In this review, we describe the pathophysiology of TBI and give a comprehensive overview of the pre-clinical studies on the use of cell-based therapy for TBI. We present the different cell types used for treatment, their main biological basis of action, the various animal models utilized, and outline the main results. We also discuss the few published and ongoing clinical trials. This review was created by searching PubMed for relevant studies, considering the following MeSH terms: stem cell, cell-based therapy, and traumatic brain injury, from the first published studies on this topic in 2000 until 2014, and examining the clinicaltrial.gov database and major published reviews. Of 896 articles initially selected, we eliminated articles not directly focused on brain trauma or cell-based therapy and finally reviewed 89 articles, among which, 68 were pre-clinical studies.
Pathophysiology of traumatic brain injury
Time dependent injury, neuronal loss and the inflammatory micro-environment
TBI can result from direct impact or from extreme acceleration-deceleration and rotational forces. The injury evolves over two phases. The primary phase corresponds to immediate damage to the central nervous system with massive depolarization of brain cellular components, resulting in a major release of inflammatory neurotransmitters, inducing monocyte/macrophage-mediated phagocytosis and complement-mediated cytolysis, and diffuse neuronal dysfunction.3 Initial forces can also disrupt the blood brain barrier, further aggravated by early expression of high concentrations of glucose transporter-1 and synthesis and release of nitric oxide.4 Consequently, the resulting cerebral haemorrhage and oedema can increase intracranial pressure and lead to cerebral ischaemia. The secondary phase starts a few hours after the injury and can last several days. It is mostly characterized by an intracellular influx of calcium, free radical generation with lipid peroxidation, and mitochondrial dysfunction,4 leading to apoptosis and necrosis of neuronal cells.
The neuronal loss after TBI is both focal and diffuse as a consequence of the primary and secondary phases of the injury. The hippocampus is especially vulnerable to the neuronal loss, even in the absence of elevated intracranial pressure,5 explaining why many studies have been interested in this cerebral region. Apoptotic neurones have been observed in the hippocampus even up to 12 months after TBI, correlating with memory impairment both in animal models and humans.6 TBI is responsible for an acute inflammatory environment, with monocyte/macrophage-mediated phagocytosis and complement-mediated cytolysis, which can persist several weeks after the injury.7 Although TBI can up-regulate neuronal growth factor (NGF) and brain derived neurotrophic factor (BDNF) and down-regulate neurotrophin-3, this inflammatory environment may impede the function of endogenous stem cells in repair.8
Neurogenesis and angiogenesis
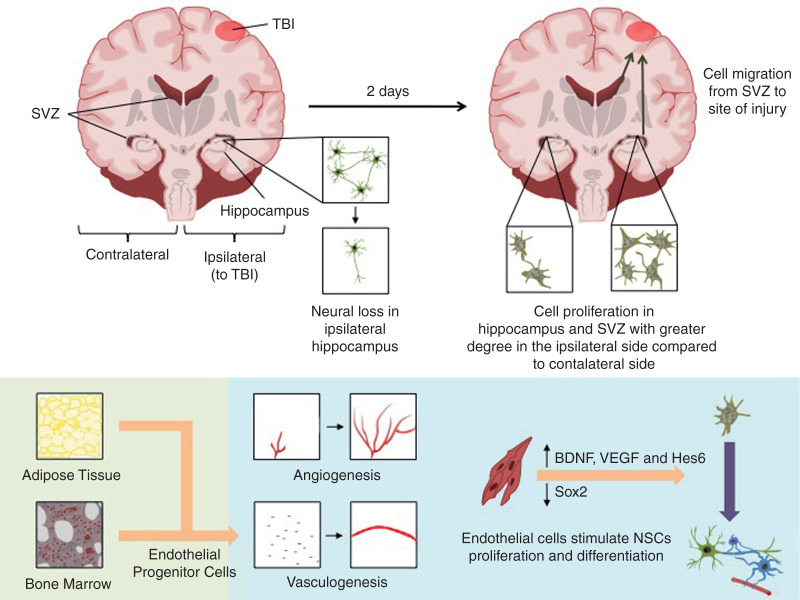
Neurogenesis and angiogenesis are stimulated after TBI. After a short proliferation phase, neural stem cells (NSC) migrate from the sub-ventricular zone (SVZ) to the site of injury and differentiate into neuronal and glial cells, stimulated by growth factors released by endothelial cells (Fig. 1). In animal models, the ipsilateral SVZ proliferation increases two to four-fold after TBI, while contralateral SVZ proliferation increases to a lesser extent.9 Also, active angiogenesis has been observed three days after an ischaemic insult. Nevertheless, even if neuroblasts have been shown to migrate to areas of injury, their ability to replace neuronal loss is uncertain.9 Furthermore, the reparative mechanisms are often overwhelmed by the resulting inflammatory neurotransmitters, cerebral haemorrhage and oedema after TBI. Multiple investigators have studied the effect of various stem and progenitor cells as therapy in this injury environment, to minimize the severity of TBI.
Fig 1.
Neurogenesis and Angiogenesis After Traumatic Brain Injury. Neurogenesis occurs throughout adult human life in two different zones of the brain: the subgranular zone of the hippocampus dentate gyrus, and the subventricular zone (SVZ) of the lateral ventricles - olfactory bulb pathway. The hippocampus and the SVZ generate neural stem cells (NSCs), which are self-renewing and multipotent. NSCs can generate neural progenitor cells (NPCs), which do not maintain the NSCs pool but rather generate neuronal and glial cells. After the initial neuronal loss in the hippocampus after traumatic brain injury (TBI): (a) Neurogenesis increase in the SVZ and in the hippocampus as early as two days, essentially in the ipsilateral side of the injured brain but also in the contralateral side to a lesser extent. Neurogenesis remains usually high for two weeks in the SVZ and one month in the hippocampus, and sometimes last up to one year. NSCs can therefore migrate directly from the SVZ to the site of injury and differentiate into neuronal and glial cells. New neurones can extend axonal projections to the cornu ammonis (CA)-3 region of the hippocampus two weeks after TBI, leading to cognitive improvement. (b) Angiogenesis from pre-existing vessels and vasculogenesis from bone-marrow and adipose-tissue derived endothelial cells are also stimulated after TBI. Increased angiogenesis has been shown three days after injury, with proliferation of endothelial cells by twelve hours. Endothelial cells also stimulate the proliferation and differentiation of NSCs and migration of neuroblasts, in part through the production of soluble growth factors such as the brain derived neurotrophic factor (BDNF) and vascular endothelial growth factor (VEGF). Endothelial cells also promote neuronal differentiation by up- and down- regulating Hes6 and Sox2 expression, respectively. Although effective after minor brain injury, these mechanisms may be insufficient after severe TBI. BDNF, brain derived neurotrophic factor; CA, cornu ammonis; Hes6 and Sox2, transcription factors; NPC, neural progenitor cells; NSC, neural stem cells; SVZ, subventricular zone; TBI, traumatic brain injury; VEGF, vascular endothelial growth factor.
Pre-clinical studies using stem and progenitor cells as treatment for traumatic brain injury
Reported mechanisms of action
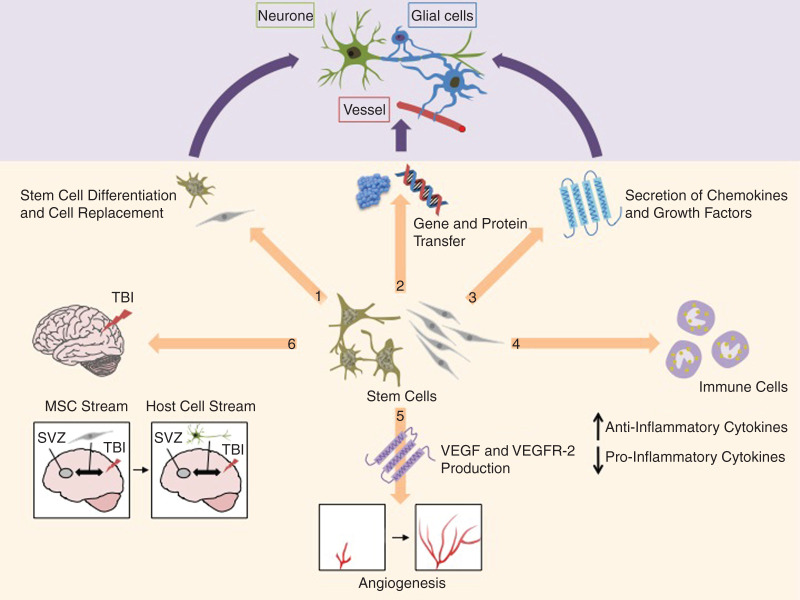
Various cell types have been used as potential therapy for TBI: mesenchymal stem cells (MSC), NSCs, neural progenitor cells (NPC), NTera2 (NT2) cells, embryonic stem cells, multipotent adult progenitor cells, and endothelial progenitor cells (Supplementary Table). Currently, several different mechanisms of action have been postulated to explain the therapeutic effects of transplanted stem and progenitor cells delivered after TBI (Fig. 2). The promotion of cell replacement by the differentiation of NSCs and MSCs was first hypothesized to be an essential mechanism of action of stem and progenitor cells after TBI.10,11 But our current knowledge suggests that improvements after TBI may essentially result from paracrine and systemic effects, via the secretion of chemokine and growth factors,12–14 decreasing oedema and inflammation caused by TBI, and enhancing endogenous neurogenesis, angiogenesis and vasculogenesis.15 Stem and progenitor cells may also stabilize damage cells via gene and protein transfer, by inter-cellular contact or fusion,16 and may develop pathways between the SVZ and the site of injury by a ‘biobridge,’ enhancing the migration of host neurogenic cells.17
Fig 2.
Potential Mechanisms of Action of Stem and Progenitor Cells in Traumatic Brain Injury. The therapeutic effect of stem and progenitor cells in traumatic brain injury (TBI) may be explained by the following mechanisms of action: 1) Differentiation of stem cells into loco-regional cell types and cell replacement although the long term engraftment rates are very low; 2) Stabilization of damage cells via gene and protein transfer by inter-cellular contact or fusion; 3) Increase of regional cell survival or proliferation via the secretion of chemokine and growth factors such as neurotrophic growth factor (NGF), brain derived neurotrophic factor (BDNF), vascular endothelial growth factor (VEGF), and fibroblast growth factor (FGF); 4) Reduction of oedema and inflammation caused by TBI, by enhancing, in the injured brain and the systemic circulation, the secretion of anti-inflammatory cytokines such as interleukin (IL)-10, and reducing the secretion of pro-inflammatory cytokines such as interferon-γ by immune cells; 5) Enhancement of angiogenesis and vasculogenesis in the ischaemic brain, by increasing VEGF secretion and the VEGF receptor (VEGFR)-2 expression; 6) And by development of pathways between the subventricular zone (SVZ) and the site of injury expressing high levels of extracellular matrix metalloproteinases and where transplanted stem cells implant initially. These transplanted stem cells act as pathways for the migration of host neurogenic cells. Once the ‘biobridge’ is formed, the grafted stem cells disappear and the host neurogenic cells persist, replacing the initial tasks of transplanted stem cells. BDNF, brain derived neurotrophic factor; FGF, fibroblast growth factor; IL, interleukin; NGF, neurotrophic growth factor; SVZ, subventricular zone; TBI, traumatic brain injury; VEGF, vascular endothelial growth factor; VEGFR-2, vascular endothelial growth factor receptor-2.
Mesenchymal stem cells
Cells origin, dose, and potency
MSCs were the most frequently used stem cells for therapy in experimental TBI (Supplementary Table). Previously, cell-based therapy with MSCs was shown to be safe clinically, when administered in patients with various acute organ injury such as myocardial infarction, acute kidney injury, stroke, etc.18 For preclinical studies in TBI, MSCs were mainly isolated from rat and human bone marrow,19,20 but were also isolated from human umbilical cord,21 rat and human adipose tissue,22,23 and human amniotic membrane.24 No study compared the effects of MSCs on TBI according to their site of isolation (i.e. bone marrow, adipose tissue, placenta). The primary mechanism of action proposed initially was the ability of MSCs to differentiate into neural cells, but there is little evidence that these cells can transform into functional neurones.25,26 Most mechanistic studies now deal with the ability of MSC to secrete paracrine soluble factors, which stabilize the endothelium preventing excessive permeability and suppress cells of the innate and adaptive immune system.
The administration dose of MSCs used in experimental TBI models in rodents varied from 1.5×105 27 to 2×107 28 cells per kg body weight, with the average dose being mostly between 106 and 107. Lower doses were reserved for stereotactic injection,14,17,21,24,27 or internal carotid artery,29 or lateral ventricle30,31 delivery. In studies with i.v. administration, higher cell dose was associated with higher cell survival rate, but without better functional improvement.32,33
Transplanted MSCs were cultured without growth factors in the large majority of pre-clinical studies. However, some groups cultured MSCs with NGF and BDNF23,34,35 or epidermal growth factor (EGF) and fibroblast growth factor (FGF)-2.21,24 NGF and BDNF increased the survival rate and the microtubule-associated protein-2 expression of transplanted MSCs,34,35 whereas EGF and FGF-2 did not change the expression of these neurone specific genes.21,24 Nevertheless, by delivering FGF-2 with bone marrow derived MSCs by stereotactic injection, Bhang and colleagues28 found increased expression of neuronal and astrocytic markers and improvement in animal motor function. Liu and colleagues36 directly injected FGF-2 into the lateral ventricle and showed a higher survival rate in transplanted bone marrow derived MSCs and increased differentiation into neuronal and glial cells, but no functional recovery.
In other studies, MSCs were transduced or transfected to enhance their survival in hypothermia, increase insulin production or endothelial and neuronal growth.27,37–39 MSCs, transduced with the temperature sensitive antigen tsA58 SV40LT, displayed higher survival rates and proliferation in the context of hypothermia.38 Enhanced concentrations of BDNF were found in cerebrospinal fluid after animal treatment with bone marrow derived MSCs transfected with the BDNF gene.37 Hippocampal cell loss was reduced with bone marrow derived MSCs, transfected with glucagon like peptide-1.27 And the use of MSCs, transfected with anti-tissue inhibitor of matrix metalloproteinase-3, restored adherent junctions in the injured brain through increase in VEGF-A signalling.39
Small animal models
Pre-clinical studies were performed primarily in Sprague-Dawley and Wistar rats, with a few using C57BL/6 mice.14,30 Cyclosporine A was administered as an immune suppressive in some studies with animals receiving human MSCs,28,30,31 although Pischiutta and colleagues31 found no clinical or biological benefit of Cyclosporine A in mice receiving human MSCs. The principal model of TBI used was the controlled cortical impact (CCI),17,19,20,22–25,27,30–35,39–49 considered to induce mostly focal injuries. The second model most widely used was the fluid percussion injury (FPI),37,38,50,51 inducing mostly diffuse injuries. Weight drop impact (WDI)21,29,36 and the penetrating brain injury (PBI),14 considered to induce respectively diffuse and focal brain damages, and the cryogenic lesion28 were other models used as well.
Delivery of stem cells
Two principal methods were used for MSC delivery: stereotactic injection14,17,21,23,24,27,28,35,37,38,40,44,48,49 and i.v. administration.19,20,25,29,32,33,39,41–43,45–47,49,51 Internal carotid artery29,34,50 and lateral ventricle30,31,36 injection methods were used infrequently. There is minimal literature comparing the delivery methods and outcomes. Mahmood and colleagues45 found enhanced proliferation of transplanted cells in the ischaemic boundary zone and the SVZ when MSCs were administered stereotactically compared with i.v., but no difference was shown in terms of functional improvements. Lundberg and colleagues29 found a higher brain engraftment of MSCs administered in the internal carotid artery vs those delivered i.v. but they did not evaluate the animal behaviour.
The timing of administration of MSC ranged from just before TBI27 to one week after the injury,17,21,33,44 but most studies administered the cells 24 hours after TBI.19,20,25,29–32,34–37,39–42,45,46,49,50 No study evaluated the effects of MSCs according to their timing of administration. Nevertheless, animal behaviour improvements have been shown even with late administrations.
Some studies used a scaffold, such as fibrin,22,28 matrigel,21,24 collagen,44 or chitosan with gelatin,23 to increase stem cell engraftment rates. The scaffold supplied extracellular matrix to maintain the viability of the implanted cells.52 In addition, it preserved the phenotype of the stem cell and had the capacity for spontaneous in vivo degradation. Guan and colleagues44 showed that the use of collagen scaffold increased the number of MSCs in the lesion site, cell survival and neuronal outgrowth, while improving motor function and learning ability.
Main outcomes
The animals were followed for a variety of time-points, ranging from four hr42 to three months.17,33,37 Regardless of the route of administration, most studies showed improvements in motor function assessed by the modified Neurological Severity Score, the Rotarod test, Stepping or Balance Beam tests and learning ability assessed by the Morris Water Maze test.
Transplanted MSCs reduced cerebral lesion volume, in particular when delivered by stereotactic injection,17,21,23,24,27,28,30,40,51 either in the centre of the injury, the cortical area adjacent to the injury, the ipsilateral hippocampus region, or the ipsilateral or contralateral ventricle. The assessment of cerebral lesion volume was done in almost all cases by histology; only a few studies used magnetic resonance imaging, positron emission tomography or a gamma camera to evaluate the effects of MSCs on cerebral lesion.42–44
Transplanted MSCs delivered by stereotactic injection down-regulated the serum concentration of the pro-inflammatory cytokines, IL-1β, IL-6, and TNF-α, 24 hours after their injection in the host brain.14 As release of pro-inflammatory cytokines after TBI can induce brain damage, this systemic effect of MSCs may contribute to improve neurological outcomes. MSCs also enhanced BDNF concentrations in the cerebrospinal fluid or in the injured brain, even more when previously transfected with the BDNF gene.30,33,37,45
Transplanted MSCs delivered by stereotactic injection showed some ability to migrate into the ischaemic boundary zone,45 the ipsilateral parenchyma,35–37,40 hippocampus,36,45 and SVZ,45 and to the contralateral parenchyma to a lower extent.36 Apart from the brain, i.v. administration of MSCs migrated to the heart, lung, liver, kidney, and spleen.19,20,25,32,33,45,46 Brain uptake in injured rats was very low, varying from 1.4%41 to less than 0.001%,47 and even lower in uninjured animals,41,42 making it unlikely that cell engraftment would have any direct effect on outcomes. The survival rate of transplanted MSCs was also low: 14.4% at one week for Lu and colleagues,34 0.6% at one month and 0.16% at three months for Tajiri and colleagues.17 But, a few MSCs expressed neuronal markers, such as microtubule-associated protein-2 (between 4.1 and 8.4% at one week),34 the neuronal nuclear antigen (between 2.9 and 5.6% at two weeks),25,34 and the neurone-specific class III beta-tubulin (Tuj-1).20,45 Others expressed the glial fibrillary acidic protein (between 7.1% and 15.8% at one week).25,34 In addition, proliferation of transplanted cells into the host brain was shown in several studies.17,38,49 Even more interesting, bone marrow derived MSCs delivered stereotactically and conditioned medium derived from these MSCs, increased NSC proliferation in vivo and in vitro, respectively.14 Rats exposed to the conditioned medium derived from MSCs exhibited a significant reduction in damaged brain volume assessed by histology, compared with rats exposed to control medium,51 and modifications of MSC conditioning (e.g. hypoxic exposure) had significant effects on the resulting damaged brain volume.51
These findings suggest that functional improvements after TBI may result from different mechanisms, other than cell replacement, such as local and systemic interactions between transplanted MSCs and cells involved in immunity or neural cell proliferation in the injured brain. Up-regulation of matrix metalloproteinase-9 in the injured brain17 and early restoration and preservation of cerebral blood flow43 have also been suggested to be responsible for the therapeutic response.
Neural stem/Progenitor cells and NTera2 cells
Cells origin, dose, and potency
NSCs and NPCs, the second most frequently used stem and progenitor cells for therapy in experimental TBI, were isolated from the postnatal mouse olfactory bulb and cerebellum,53 embryonic murine ganglionic eminence,54 embryonic rat hippocampus and forebrain tissue,40,55 adult rat hippocampus,56 and from first-trimester embryonic human forebrain57 (Supplementary Table). NTera2 cells are human derived teratocarcinoma cells that differentiate into post-mitotic neurones when cultured in vitro with retinoic acid.58
In small animal models of TBI, the number of cells used varied from 1.5×105 59 to 2.5×107 60 cells per kg body weight, with most doses between 105 and 106. No study evaluated the effects of NSCs, NPCs or NTera2 cells according to the dose administered, but individual studies with lower doses have not shown animal behaviour improvements when evaluated.59
The potency of the stem cells was often enhanced by adding EGF and FGF-2 (also named basic FGF)57,60–68 or FGF-2 alone54,56,69–71 in the culture medium. In other studies, the stem and progenitor cells were transduced or transfected with a gene implicated in neuronal growth or differentiation.55,62,70,72,73 Philips and colleagues55 found increased survival rate of pyramidal cells in the ipsilateral hippocampus but no clinical benefit, when delivering NGF transduced-NPCs compared with NPCs alone. Makri and colleagues70 found an increased generation of neuronal cells compared with glial cells when delivering NSCs and NPCs transduced with the cell cycle exit and neuronal differentiation (Cend)-1 gene. Ma and colleagues64 and Bakshi and colleagues73 demonstrated improvements in motor function and learning ability in rats with higher survival rate and migration and neuronal differentiation of transplanted cells transfected with the BDNF gene or the glial cell-derived neurotrophic factor gene.
Small animal models
Traumatic brain injury was induced in adult Sprague-Dawley rats,56,57,59,61,63,65–68,72–74 C57BL/6 mice,53,54,60,69–71, 75,76 and Wistar rats.40,55,62,64 Cyclosporine A was usually administered in animals receiving human stem cells59,61,63,65,67,68,76 and in rats receiving mouse-derived stem cells.72,73 Wennersten and colleagues67 showed in rats which received human NSCs and NPCs by stereotactic injection, that Cyclosporine A improved cell graft survival. The principal models of TBI used were the CCI,40,53,54,57,60–64,69,71,74–76 followed by FPI.55,59,66,68,72,73
Delivery of stem cells
The delivery method used for NSCs, NPCs and NTera2 cells was predominantly stereotactic injection. Skardelly and colleagues63 studied the effects of pre-differentiated NPCs, adding an i.v. cell delivery to the stereotactic injection. They found no additional benefit of the i.v. injection. Wallenquist and colleagues60 had higher transplanted cell survival when injected in the lateral ventricle, compared with stereotactic injection. No study compared i.v. to stereotactic injections alone.
The timing of delivery from TBI ranged from immediately after injury57,60,65,67,70 to one month later.59 Cells were often delivered 24 hours40,55,63,66,68,73,75,76 or one week53,54,56,60,62,64,69,71,72,74 after TBI. Shear and colleagues71 found that stereotactic injection in the ipsilateral striatum, carried out two days or one week after TBI, led to better outcomes than two weeks after. Zhang and colleagues59 also found no difference in motor and cognitive functions in rats receiving NTera2 cells by stereotactic injection one month after the TBI.
The few pre-clinical studies using scaffolds such as fibronectin,69 laminin,69 or collagen56 suggested improved outcomes, with long term transplanted cell survival and distribution into the injured brain.69
Main outcomes
In the studies, the animals were followed for multiple time-points, from three days68 to six months,67 with most from one to three months.53,56,59–64,69–71,73,76 Interestingly, all studies showed improvements in motor function and learning ability. Transplanted cells were found to decrease the cerebral lesion volume63 and shown to migrate to the ischaemic boundary zone,55,60,61,63,65 ipsilateral parenchyma,40,53,54,56,59,61,62,65 hippocampus,54,55,64–67 SVZ,61 rostral migration stream,62,64 and olfactory bulb,62 and to the contralateral parenchyma to a lesser extent.61,65,72 Stem and progenitor cell engraftment persisted for up to six months.67
The transplanted cell survival rate was low: 1.9% at two weeks for Harting and colleagues74 and 4.1% at two months for Ma and colleagues.62 In addition, most studies failed to demonstrate the proliferation of transplanted cells in the host brain. Nevertheless, Zhang and colleagues59 and Ma and colleagues64 found that some transplanted cells expressed synatophysin, a synaptic vesicle glycoprotein used for synapses quantification. Also, some transplanted cells expressed both neuronal markers, especially in the ipsilateral hippocampus,53,60,66,70 and glial markers.56 A potential systemic effect of cells injected stereotactically or i.v. has not been demonstrated yet.
Similar to MSCs, these findings seemed to indicate improvements after TBI, despite limited stem cell engraftment. Increased angiogenesis in the injury border zone63 and decreased amyloid precursor protein accumulation and α-smooth muscle actin expression in ipsilateral hippocampus (site of NSCs transplantation)68 have been suggested to be responsible for some of the beneficial effects.
Embryonic stem cells
Embryonic stem cells were studied less frequently than NSCs, NPCs or MSCs, in the context of TBI (Supplementary Table). In all cases, they were isolated from the inner cell mass of murine blastocysts.77,78 The number of cells used varied from 3×105 8,79,80 to 107 78 cells per kg body weight. Some embryonic stem cells were pre-differentiated before use,79 and some were cultured with retinoic acid to further differentiate to neurone like cells,78,81 but without obvious biological or clinical improvements.
Studies were performed with Sprague-Dawley rats8,79,80 or C57BL/6 mice.78,81 Cyclosporine A was administered in two studies using murine embryonic stem cells in rats, without any benefit.8,80 Three models of TBI were used: the FPI,8,80 the cryogenic lesion78,81 and the CCI79 model. All embryonic stem cells were delivered by stereotactic injection, between three days8,80 and one week78,79,81 after TBI.
Time-endpoints ranged between three78 and seven8,80 weeks. Studies showed animal behavioural but no learning improvements. Transplanted embryonic stem cells migrated into the site of injury78,79 and to the ipsilateral hippocampus.79 Some embryonic stem cells differentiated into neurone like cells,78,79,81 while others expressed glial markers.79 Some implanted cells were phagocytosed by activated macrophages.8 Interestingly, Riess and colleagues80 showed almost no detection of transplanted embryonic stem cells in the injured brain, but tumour formations were found seven weeks after their injection.
Multipotent adult progenitor cells
Multipotent adult progenitor cells are undifferentiated cells derived from the bone marrow (Supplementary Table). They are self-renewing and multipotent, precursors for adult progenitor cells, and able to differentiate to neural, endothelial and hematopoietic cells, in vitro and in vivo. Their surface markers include CD10, CD13, CD49b, CD49d, CDw90 and VEGFR-2.82
Only one research team used human multipotent adult progenitor cells as a potential treatment of TBI in Sprague-Dawley rats83,84 and C57BL/6 mice.85 The number of cells used in each experiment was around 106, injected i.v. two and 24 hours after TBI. The cells prevented increase in blood brain barrier permeability after TBI, primarily through modulation of immune cells,83,85,86 which was associated with increased anti-inflammatory macrophages (M2 phenotype) in the brain and higher IL-10 concentrations.85
Endothelial progenitor cells
Endothelial progenitor cells, isolated from bone marrow and adipose tissue,87,88 were used in Sprague-Dawley87 and Wistar88 rats undergoing CCI (Supplementary Table). Chen and colleagues88 found restored cerebral blood perfusion and increased cerebral microvasculature in the injured region at one week, when endothelial progenitor cells were administered six and twelve hours after TBI. Xue and colleagues87 showed accumulation of endothelial progenitor cells in the injury site, their incorporation into capillaries, and reduced astrogliosis and inflammation, leading to better neurological outcomes.
Clinical studies
Only two clinical trials using stem and progenitor cells as treatment for acute or sub-acute TBI have been published.89,90 Cox and colleagues89 conducted a prospective, non-random, open label, phase 1/2 clinical trial (NCT00254722) on 10 children aged five to fourteen yr with a post-resuscitation GCS of five to eight. They administered i.v. 6×106 autologous bone marrow derived mononuclear cells (from which MSCs and multipotent adult progenitor cells are derived) per kg body weight within 48 hours after brain injury and conducted a six months follow-up. They found no episodes of post-injury seizures, refractory intra-cranial pressure, alteration in cerebral perfusion pressure, or new ischaemic event. Every patient showed some neurological improvement, but only three patients recovered completely. No significant brain morphologic change was found by magnetic resonance imaging between one and six months. Tian and colleagues90 conducted a prospective, non-random, open label, phase 1/2 study, on 97 patients in the sub-acute phase of TBI. They administered a mean dose of 4×106 autologous bone marrow derived mononuclear cells, intrathecally by lumbar puncture, within two months after the injury and conducted a 40 day follow-up. They found no serious complications or adverse events. Twenty seven patients showed improvements in motor functions, and 11 of 24 patients in vegetative state showed improvements in consciousness. The outcome was better for younger patients and for patients who received therapy earlier after injury.
Three clinical trials are currently ongoing. NCT01851083 is a randomized controlled phase 1/2 trial, studying the effects of autologous bone marrow derived mononuclear cells, delivered i.v. in children aged five to seventeen years, with a hospital admission GCS of three to eight. The primary outcome is improvement by brain magnetic resonance imaging, and the secondary outcome is improvement in functional and neurocognitive deficits. One potential implication of this study will be the ability to determine the relationship between neurological status and brain morphology. NCT01575470 is an open label phase 1/2 trial studying the effects of autologous bone marrow derived mononuclear cells delivered i.v. in adults aged 18-55 yr with a post-resuscitation GCS of five to eight. The primary outcomes are the number of neurological events and cerebral vascular accidents, and the secondary outcomes are the global functional status and the level of the disability. And lastly, NCT02028104 is an open label phase 1/2 trial, studying the effects of autologous bone marrow derived mononuclear cells, delivered intrathecally in brain injured patients aged six months to 65 yr. Primary and secondary outcomes are the change in clinical symptoms and the level of the disability rating scale. One potential implication of this study will be the ability to determine the optimal route of deliver of the stem and progenitor cells.
Clinical trial and research perspectives
These early clinical trials are encouraging, in particular because they have showed safety with the absence of serious side-effects. There is strong rationale for the use of MSCs, NSCs or NPCs as treatment for TBI. Currently, the potential use of NSCs and NPCs in clinical trials is mainly limited by the difficulty generating large quantities of NSCs or NPCs for administration. Whereas, the potential use of MSCs is very promising based on their relative ease of procurement, immune-privileged property allowing an allogeneic source, and well documented safety profile.91 Surprisingly, all the current clinical trials have used bone marrow derived mononuclear cells as treatment after TBI, primarily because of the autologous source of the cells. One wonders whether similar or improved neurological benefits can be achieved with MSCs compared with a similar dose of mononuclear cells.
However, questions still remain concerning the optimal route and timing of delivery of the cells after TBI and the monitoring parameters utilized for safety and efficacy. Stereotactic injection, although feasible, is highly invasive and will require the skills of a neurosurgeon, whereas i.v. and intrathecal injections are much more accessible delivery routes. As the long term engraftment rates are very low, i.v. delivery may be as efficacious as stereotactic or intrathecal delivery. Most pre-clinical trials have delivered the cells early after TBI to suppress the initial inflammatory response and activation of the cells of innate and adaptive immunity. There is minimal pre-clinical evidence of benefit when stem and progenitor cells are delivered more than one week after TBI.92 Initial monitoring for safety and efficacy should combine magnetic resonance imaging for its ability to show cerebral lesion and perfusion, biological parameters such as the systemic concentrations of pro- and anti-inflammatory cytokines, and multiple neurological tests allowing a comprehensive overview of the patient's neurological state. Although functional recovery of the hippocampus may be an attractive endpoint for clinical trials, many of the effects of stem and progenitor cells are nonspecific, such as the stabilization of the blood-brain barrier preventing excessive cerebral oedema.
Significant obstacles still remain for conducting randomized controlled trials for efficacy. The optimal cell type, dose, delivery route, and timing of administration and which monitoring parameters would be necessary and for how long needs to be determined in humans. In addition, the cost of conducting such clinical trials, specifically the cost of generating and storage/processing of the stem and progenitor cells before administration, is significant. Lastly, although using adult stem cells and an autologous source will diminish the long term risk of iatrogenic tumour formation, patients in clinical trials will generally receive 5 to 10×106 cells kg−1 or up to 1 billion cells per treatment. There is no adequate monitoring device (i.e. CT or MRI scan) yet, which can differentiate iatrogenic tumour foci from inflamed or injured tissue immediately.
Conclusion
TBI is a major public health issue in need of innovative treatment options. Cell-based therapy may be a promising approach. Pre-clinical research in small animal models of TBI has paved the way for early phase 1/2 clinical trials. Nevertheless, more studies are needed to address the optimal stem cell used, dose and delivery method. And above all, more preclinical work is necessary to further understand the mechanisms underlying the therapeutic effect of stem and progenitor cells in the injured brain.
Supplementary material
Supplementary Material is available at British Journal of Anaesthesia online.
Authors' contributions
Study design/planning: S.G., J.W.L.
Writing paper: S.G., A.M., Q.H., J.L., V.G., E.L.B., J.W.L.
Revising paper: All authors.
Declaration of interest
None declared.
Funding
This review was supported by the National Heart, Lung, and Blood Institute Grant HL-113022 (to Jae W Lee, USA) & Hamilton Endowment Funds (to Jae W Lee, UCSF Department of Anesthesiology, San Francisco, CA, USA).
Supplementary Material
References
- 1.Centers for Disease Control and Prevention. 2014. Available from: http://www.cdc.gov/traumaticbraininjury/severe.html
- 2.Guidelines for the Management of Severe Traumatic Brain Injury 3rd Edition. J Neurotrauma 2007; 24: S1–106. Available from: http://www.braintrauma.org/pdf/protected/Guidelines_Management_2007w_bookmarks.pdf [DOI] [PubMed] [Google Scholar]
- 3.Jain KK. Neuroprotection in traumatic brain injury. Drug Discov Today 2008; 13: 1082–9 [DOI] [PubMed] [Google Scholar]
- 4.Ugoya SO, Tu J. Bench to bedside of neural stem cell in traumatic brain injury. Stem Cells Int 2012; 2012: 141624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kotapka MJ, Graham DI, Adams JH, Gennarelli TA. Hippocampal pathology in fatal human head injury without high intracranial pressure. J Neurotrauma 1994; 11: 317–24 [DOI] [PubMed] [Google Scholar]
- 6.Umile EM, Sandel ME, Alavi A, Terry CM, Plotkin RC. Dynamic imaging in mild traumatic brain injury: support for the theory of medial temporal vulnerability. Arch Phys Med Rehabil 2002; 83: 1506–13 [DOI] [PubMed] [Google Scholar]
- 7.Kelley BJ, Lifshitz J, Povlishock JT. Neuroinflammatory responses after experimental diffuse traumatic brain injury. J Neuropathol Exp Neurol 2007; 66: 989–1001 [DOI] [PubMed] [Google Scholar]
- 8.Molcanyi M, Riess P, Bentz K, et al. Trauma-associated inflammatory response impairs embryonic stem cell survival and integration after implantation into injured rat brain. J Neurotrauma 2007; 24: 625–37 [DOI] [PubMed] [Google Scholar]
- 9.Richardson RM, Singh A, Sun D, Fillmore HL, Dietrich DW, III, Bullock MR. Stem cell biology in traumatic brain injury: effects of injury and strategies for repair. J Neurosurgery 2010; 112: 1125–38 [DOI] [PubMed] [Google Scholar]
- 10.Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006; 8: 315–7 [DOI] [PubMed] [Google Scholar]
- 11.Sun D, Colello RJ, Daugherty WP, et al. Cell proliferation and neuronal differentiation in the dentate gyrus in juvenile and adult rats following traumatic brain injury. J Neurotrauma 2005; 22: 95–105 [DOI] [PubMed] [Google Scholar]
- 12.Qu K, Ortoleva P. Understanding stem cell differentiation through self-organization theory. J Theor Biol 2008; 250: 606–20 [DOI] [PubMed] [Google Scholar]
- 13.Walker PA, Shah SK, Harting MT, Cox CS., Jr Progenitor cell therapies for traumatic brain injury: barriers and opportunities in translation. Dis Model Mech 2009; 2: 23–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galindo LT, Filippo TR, Semedo P, et al. Mesenchymal stem cell therapy modulates the inflammatory response in experimental traumatic brain injury. Neurol Res Int 2011; 2011: 564089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen XH, Iwata A, Nonaka M, Browne KD, Smith DH. Neurogenesis and glial proliferation persist for at least one year in the subventricular zone following brain trauma in rats. J Neurotrauma 2003; 20: 623–31 [DOI] [PubMed] [Google Scholar]
- 16.Spees JL, Olson SD, Ylostalo J, et al. Differentiation, cell fusion, and nuclear fusion during ex vivo repair of epithelium by human adult stem cells from bone marrow stroma. Proc Nat Acad Sci USA 2003; 100: 2397–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tajiri N, Kaneko Y, Shinozuka K, et al. Stem cell recruitment of newly formed host cells via a successful seduction? Filling the gap between neurogenic niche and injured brain site. PloS One 2013; 8: e74857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monsel A, Zhu YG, Gennai S, Hao Q, Liu J, Lee JW. Cell-based therapy for acute organ injury: preclinical evidence and ongoing clinical trials using mesenchymal stem cells. Anesthesiology 2014; 121: 1099–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu D, Mahmood A, Wang L, Li Y, Lu M, Chopp M. Adult bone marrow stromal cells administered intravenously to rats after traumatic brain injury migrate into brain and improve neurological outcome. Neuroreport 2001; 12: 559–63 [DOI] [PubMed] [Google Scholar]
- 20.Mahmood A, Lu D, Lu M, Chopp M. Treatment of traumatic brain injury in adult rats with intravenous administration of human bone marrow stromal cells. Neurosurgery 2003; 53: 697–702 [DOI] [PubMed] [Google Scholar]
- 21.Hong SQ, Zhang HT, You J, et al. Comparison of transdifferentiated and untransdifferentiated human umbilical mesenchymal stem cells in rats after traumatic brain injury. Neurochem Res 2011; 36: 2391–400 [DOI] [PubMed] [Google Scholar]
- 22.Lam PK, Lo AW, Wang KK, et al. Transplantation of mesenchymal stem cells to the brain by topical application in an experimental traumatic brain injury model. J Clin Neurosci 2013; 20: 306–9 [DOI] [PubMed] [Google Scholar]
- 23.Gao S, Zhao P, Lin C, et al. Differentiation of human adipose-derived stem cells into neuron-like cells which are compatible with photocurable three-dimensional scaffolds. Tissue Eng Part A 2014; 20: 1271–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yan ZJ, Zhang P, Hu YQ, et al. Neural stem-like cells derived from human amnion tissue are effective in treating traumatic brain injury in rat. Neurochem Res 2013; 38: 1022–33 [DOI] [PubMed] [Google Scholar]
- 25.Mahmood A, Lu D, Wang L, Li Y, Lu M, Chopp M. Treatment of traumatic brain injury in female rats with intravenous administration of bone marrow stromal cells. Neurosurgery 2001; 49: 1196–203 [PubMed] [Google Scholar]
- 26.Castro RF, Jackson KA, Goodell MA, Robertson CS, Liu H, Shine HD. Failure of bone marrow cells to transdifferentiate into neural cells in vivo. Science 2002; 297: 1299. [DOI] [PubMed] [Google Scholar]
- 27.Heile AM, Wallrapp C, Klinge PM, et al. Cerebral transplantation of encapsulated mesenchymal stem cells improves cellular pathology after experimental traumatic brain injury. Neurosci Lett 2009; 463: 176–81 [DOI] [PubMed] [Google Scholar]
- 28.Bhang SH, Lee YE, Cho SW, et al. Basic fibroblast growth factor promotes bone marrow stromal cell transplantation-mediated neural regeneration in traumatic brain injury. Biochem Biophys Res Commun 2007; 359: 40–5 [DOI] [PubMed] [Google Scholar]
- 29.Lundberg J, Le Blanc K, Soderman M, Andersson T, Holmin S. Endovascular transplantation of stem cells to the injured rat CNS. Neuroradiology 2009; 51: 661–7 [DOI] [PubMed] [Google Scholar]
- 30.Zanier ER, Montinaro M, Vigano M, et al. Human umbilical cord blood mesenchymal stem cells protect mice brain after trauma. Crit Care Med 2011; 39: 2501–10 [DOI] [PubMed] [Google Scholar]
- 31.Pischiutta F, D'Amico G, Dander E, et al. Immunosuppression does not affect human bone marrow mesenchymal stromal cell efficacy after transplantation in traumatized mice brain. Neuropharmacology 2014; 79: 119–26 [DOI] [PubMed] [Google Scholar]
- 32.Mahmood A, Lu D, Qu C, Goussev A, Chopp M. Human marrow stromal cell treatment provides long-lasting benefit after traumatic brain injury in rats. Neurosurgery 2005; 57: 1026–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahmood A, Lu D, Qu C, Goussev A, Chopp M. Long-term recovery after bone marrow stromal cell treatment of traumatic brain injury in rats. J Neurosurgery 2006; 104: 272–7 [DOI] [PubMed] [Google Scholar]
- 34.Lu D, Li Y, Wang L, Chen J, Mahmood A, Chopp M. Intraarterial administration of marrow stromal cells in a rat model of traumatic brain injury. J Neurotrauma 2001; 18: 813–9 [DOI] [PubMed] [Google Scholar]
- 35.Mahmood A, Lu D, Wang L, Chopp M. Intracerebral transplantation of marrow stromal cells cultured with neurotrophic factors promotes functional recovery in adult rats subjected to traumatic brain injury. J Neurotrauma 2002; 19: 1609–17 [DOI] [PubMed] [Google Scholar]
- 36.Liu Y, Yi XC, Guo G, et al. Basic fibroblast growth factor increases the transplantationmediated therapeutic effect of bone mesenchymal stem cells following traumatic brain injury. Mol Med Rep 2014; 9: 333–9 [DOI] [PubMed] [Google Scholar]
- 37.Wang Z, Yao W, Deng Q, Zhang X, Zhang J. Protective effects of BDNF overexpression bone marrow stromal cell transplantation in rat models of traumatic brain injury. J Mol Neurosci 2013; 49: 409–16 [DOI] [PubMed] [Google Scholar]
- 38.Tu Y, Chen C, Sun HT, et al. Combination of temperature-sensitive stem cells and mild hypothermia: a new potential therapy for severe traumatic brain injury. J Neurotrauma 2012; 29: 2393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Menge T, Zhao Y, Zhao J, et al. Mesenchymal stem cells regulate blood-brain barrier integrity through TIMP3 release after traumatic brain injury. Sci Transl Med 2012; 4: 161ra150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lu D, Li Y, Mahmood A, Wang L, Rafiq T, Chopp M. Neural and marrow-derived stromal cell sphere transplantation in a rat model of traumatic brain injury. J Neurosurgery 2002; 97: 935–40 [DOI] [PubMed] [Google Scholar]
- 41.Yoon JK, Park BN, Shim WY, Shin JY, Lee G, Ahn YH. In vivo tracking of 111In-labeled bone marrow mesenchymal stem cells in acute brain trauma model. Nucl Med Biol 2010; 37: 381–8 [DOI] [PubMed] [Google Scholar]
- 42.Park BN, Shim W, Lee G, et al. Early distribution of intravenously injected mesenchymal stem cells in rats with acute brain trauma evaluated by (99m)Tc-HMPAO labeling. Nucl Med Biol 2011; 38: 1175–82 [DOI] [PubMed] [Google Scholar]
- 43.Li L, Jiang Q, Qu CS, et al. Transplantation of marrow stromal cells restores cerebral blood flow and reduces cerebral atrophy in rats with traumatic brain injury: in vivo MRI study. J Neurotrauma 2011; 28: 535–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guan J, Zhu Z, Zhao RC, et al. Transplantation of human mesenchymal stem cells loaded on collagen scaffolds for the treatment of traumatic brain injury in rats. Biomaterials 2013; 34: 5937–46 [DOI] [PubMed] [Google Scholar]
- 45.Mahmood A, Lu D, Chopp M. Intravenous administration of marrow stromal cells (MSCs) increases the expression of growth factors in rat brain after traumatic brain injury. J Neurotrauma 2004; 21: 33–9 [DOI] [PubMed] [Google Scholar]
- 46.Bakhtiary M, Marzban M, Mehdizadeh M, et al. Comparison of transplantation of bone marrow stromal cells (BMSC) and stem cell mobilization by granulocyte colony stimulating factor after traumatic brain injury in rat. Iran Biomed J 2010; 14: 142–9 [PMC free article] [PubMed] [Google Scholar]
- 47.Harting MT, Jimenez F, Xue H, et al. Intravenous mesenchymal stem cell therapy for traumatic brain injury. J Neurosurgery 2009; 110: 1189–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Walker PA, Harting MT, Jimenez F, et al. Direct intrathecal implantation of mesenchymal stromal cells leads to enhanced neuroprotection via an NFkappaB-mediated increase in interleukin-6 production. Stem Cells Dev 2010; 19: 867–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mahmood A, Lu D, Chopp M. Marrow stromal cell transplantation after traumatic brain injury promotes cellular proliferation within the brain. Neurosurgery 2004; 55: 1185–93 [DOI] [PubMed] [Google Scholar]
- 50.Okuma Y, Wang F, Toyoshima A, et al. Mannitol enhances therapeutic effects of intra-arterial transplantation of mesenchymal stem cells into the brain after traumatic brain injury. Neurosci Lett 2013; 554: 156–61 [DOI] [PubMed] [Google Scholar]
- 51.Chang CP, Chio CC, Cheong CU, Chao CM, Cheng BC, Lin MT. Hypoxic preconditioning enhances the therapeutic potential of the secretome from cultured human mesenchymal stem cells in experimental traumatic brain injury. Clin Sci 2013; 124: 165–76 [DOI] [PubMed] [Google Scholar]
- 52.Walker PA, Aroom KR, Jimenez F, et al. Advances in progenitor cell therapy using scaffolding constructs for central nervous system injury. Stem Cell Rev 2009; 5: 283–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Riess P, Zhang C, Saatman KE, et al. Transplanted neural stem cells survive, differentiate, and improve neurological motor function after experimental traumatic brain injury. Neurosurgery 2002; 51: 1043–52 [DOI] [PubMed] [Google Scholar]
- 54.Shear DA, Tate MC, Archer DR, et al. Neural progenitor cell transplants promote long-term functional recovery after traumatic brain injury. Brain Res 2004; 1026: 11–22 [DOI] [PubMed] [Google Scholar]
- 55.Philips MF, Mattiasson G, Wieloch T, et al. Neuroprotective and behavioral efficacy of nerve growth factor-transfected hippocampal progenitor cell transplants after experimental traumatic brain injury. J Neurosurgery 2001; 94: 765–74 [DOI] [PubMed] [Google Scholar]
- 56.Elias PZ, Spector M. Implantation of a collagen scaffold seeded with adult rat hippocampal progenitors in a rat model of penetrating brain injury. J Neurosci Methods 2012; 209: 199–211 [DOI] [PubMed] [Google Scholar]
- 57.Hagan M, Wennersten A, Meijer X, Holmin S, Wahlberg L, Mathiesen T. Neuroprotection by human neural progenitor cells after experimental contusion in rats. Neurosci Lett 2003; 351: 149–52 [DOI] [PubMed] [Google Scholar]
- 58.Trojanowski JQ, Kleppner SR, Hartley RS, et al. Transfectable and transplantable postmitotic human neurons: a potential “platform” for gene therapy of nervous system diseases. Exp Neurol 1997; 144: 92–7 [DOI] [PubMed] [Google Scholar]
- 59.Zhang C, Saatman KE, Royo NC, et al. Delayed transplantation of human neurons following brain injury in rats: a long-term graft survival and behavior study. J Neurotrauma 2005; 22: 1456–74 [DOI] [PubMed] [Google Scholar]
- 60.Wallenquist U, Brannvall K, Clausen F, Lewen A, Hillered L, Forsberg-Nilsson K. Grafted neural progenitors migrate and form neurons after experimental traumatic brain injury. Restor Neurol Neurosci 2009; 27: 323–34 [DOI] [PubMed] [Google Scholar]
- 61.Wennersten A, Meier X, Holmin S, Wahlberg L, Mathiesen T. Proliferation, migration, and differentiation of human neural stem/progenitor cells after transplantation into a rat model of traumatic brain injury. J Neurosurgery 2004; 100: 88–96 [DOI] [PubMed] [Google Scholar]
- 62.Ma H, Yu B, Kong L, Zhang Y, Shi Y. Transplantation of neural stem cells enhances expression of synaptic protein and promotes functional recovery in a rat model of traumatic brain injury. Mol Med Rep 2011; 4: 849–56 [DOI] [PubMed] [Google Scholar]
- 63.Skardelly M, Gaber K, Burdack S, et al. Long-term benefit of human fetal neuronal progenitor cell transplantation in a clinically adapted model after traumatic brain injury. J Neurotrauma 2011; 28: 401–14 [DOI] [PubMed] [Google Scholar]
- 64.Ma H, Yu B, Kong L, Zhang Y, Shi Y. Neural stem cells over-expressing brain-derived neurotrophic factor (BDNF) stimulate synaptic protein expression and promote functional recovery following transplantation in rat model of traumatic brain injury. Neurochemical Res 2012; 37: 69–83 [DOI] [PubMed] [Google Scholar]
- 65.Al Nimer F, Wennersten A, Holmin S, Meijer X, Wahlberg L, Mathiesen T. MHC expression after human neural stem cell transplantation to brain contused rats. Neuroreport 2004; 15: 1871–5 [DOI] [PubMed] [Google Scholar]
- 66.Gao J, Prough DS, McAdoo DJ, et al. Transplantation of primed human fetal neural stem cells improves cognitive function in rats after traumatic brain injury. Exp Neurol 2006; 201: 281–92 [DOI] [PubMed] [Google Scholar]
- 67.Wennersten A, Holmin S, Al Nimer F, Meijer X, Wahlberg LU, Mathiesen T. Sustained survival of xenografted human neural stem/progenitor cells in experimental brain trauma despite discontinuation of immunosuppression. Exp Neurol 2006; 199: 339–47 [DOI] [PubMed] [Google Scholar]
- 68.Wang E, Gao J, Yang Q, et al. Molecular mechanisms underlying effects of neural stem cells against traumatic axonal injury. J Neurotrauma 2012; 29: 295–312 [DOI] [PubMed] [Google Scholar]
- 69.Tate CC, Shear DA, Tate MC, Archer DR, Stein DG, LaPlaca MC. Laminin and fibronectin scaffolds enhance neural stem cell transplantation into the injured brain. J Tissue Eng Regen Med 2009; 3: 208–17 [DOI] [PubMed] [Google Scholar]
- 70.Makri G, Lavdas AA, Katsimpardi L, Charneau P, Thomaidou D, Matsas R. Transplantation of embryonic neural stem/precursor cells overexpressing BM88/Cend1 enhances the generation of neuronal cells in the injured mouse cortex. Stem Cells 2010; 28: 127–39 [DOI] [PubMed] [Google Scholar]
- 71.Shear DA, Tate CC, Tate MC, et al. Stem cell survival and functional outcome after traumatic brain injury is dependent on transplant timing and location. Restor Neurol Neurosci 2011; 29: 215–25 [DOI] [PubMed] [Google Scholar]
- 72.Boockvar JA, Schouten J, Royo N, et al. Experimental traumatic brain injury modulates the survival, migration, and terminal phenotype of transplanted epidermal growth factor receptor-activated neural stem cells. Neurosurgery 2005; 56: 163–71 [DOI] [PubMed] [Google Scholar]
- 73.Bakshi A, Shimizu S, Keck CA, et al. Neural progenitor cells engineered to secrete GDNF show enhanced survival, neuronal differentiation and improve cognitive function following traumatic brain injury. Eur J Neurosci 2006; 23: 2119–34 [DOI] [PubMed] [Google Scholar]
- 74.Harting MT, Sloan LE, Jimenez F, Baumgartner J, Cox CS., Jr Subacute neural stem cell therapy for traumatic brain injury. J Surg Res 2009; 153: 188–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Watson DJ, Longhi L, Lee EB, et al. Genetically modified NT2N human neuronal cells mediate long-term gene expression as CNS grafts in vivo and improve functional cognitive outcome following experimental traumatic brain injury. J Neuropathol Exp Neurol 2003; 62: 368–80 [DOI] [PubMed] [Google Scholar]
- 76.Longhi L, Watson DJ, Saatman KE, et al. Ex vivo gene therapy using targeted engraftment of NGF-expressing human NT2N neurons attenuates cognitive deficits following traumatic brain injury in mice. J Neurotrauma 2004; 21: 1723–36 [DOI] [PubMed] [Google Scholar]
- 77.Ikeda R, Kurokawa MS, Chiba S, et al. Transplantation of neural cells derived from retinoic acid-treated cynomolgus monkey embryonic stem cells successfully improved motor function of hemiplegic mice with experimental brain injury. Neurobiol Dis 2005; 20: 38–48 [DOI] [PubMed] [Google Scholar]
- 78.Chiba S, Iwasaki Y, Sekino H, Suzuki N. Transplantation of motoneuron-enriched neural cells derived from mouse embryonic stem cells improves motor function of hemiplegic mice. Cell Transplant 2003; 12: 457–68 [DOI] [PubMed] [Google Scholar]
- 79.Hoane MR, Becerra GD, Shank JE, et al. Transplantation of neuronal and glial precursors dramatically improves sensorimotor function but not cognitive function in the traumatically injured brain. J Neurotrauma 2004; 21: 163–74 [DOI] [PubMed] [Google Scholar]
- 80.Riess P, Molcanyi M, Bentz K, et al. Embryonic stem cell transplantation after experimental traumatic brain injury dramatically improves neurological outcome, but may cause tumors. J Neurotrauma 2007; 24: 216–25 [DOI] [PubMed] [Google Scholar]
- 81.Chiba S, Ikeda R, Kurokawa MS, et al. Anatomical and functional recovery by embryonic stem cell-derived neural tissue of a mouse model of brain damage. J Neurol Sci 2004; 219: 107–17 [DOI] [PubMed] [Google Scholar]
- 82.Jiang Y, Jahagirdar BN, Reinhardt RL, et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature 2002; 418: 41–9 [DOI] [PubMed] [Google Scholar]
- 83.Walker PA, Shah SK, Jimenez F, et al. Intravenous multipotent adult progenitor cell therapy for traumatic brain injury: preserving the blood brain barrier via an interaction with splenocytes. Exp Neurol 2010; 225: 341–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bedi SS, Hetz R, Thomas C, et al. Intravenous multipotent adult progenitor cell therapy attenuates activated microglial/macrophage response and improves spatial learning after traumatic brain injury. Stem Cells Transl Med 2013; 2: 953–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Walker PA, Bedi SS, Shah SK, et al. Intravenous multipotent adult progenitor cell therapy after traumatic brain injury: modulation of the resident microglia population. J Neuroinflammation 2012; 9: 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ajmo CT, Jr, Collier LA, Leonardo CC, et al. Blockade of adrenoreceptors inhibits the splenic response to stroke. Exp Neurol 2009; 218: 47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xue S, Zhang HT, Zhang P, et al. Functional endothelial progenitor cells derived from adipose tissue show beneficial effect on cell therapy of traumatic brain injury. Neurosci Lett 2010; 473: 186–91 [DOI] [PubMed] [Google Scholar]
- 88.Chen X, Yin J, Wu X, et al. Effects of magnetically labeled exogenous endothelial progenitor cells on cerebral blood perfusion and microvasculature alterations after traumatic brain injury in rat model. Acta Radiol 2013; 54: 313–23 [DOI] [PubMed] [Google Scholar]
- 89.Cox CS, Jr, Baumgartner JE, Harting MT, et al. Autologous bone marrow mononuclear cell therapy for severe traumatic brain injury in children. Neurosurgery 2011; 68: 588–600 [DOI] [PubMed] [Google Scholar]
- 90.Tian C, Wang X, Wang X, et al. Autologous bone marrow mesenchymal stem cell therapy in the subacute stage of traumatic brain injury by lumbar puncture. Exp Clin Transplant 2013; 11: 176–81 [DOI] [PubMed] [Google Scholar]
- 91.Lalu MM, McIntyre L, Pugliese C, et al. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systemic review and meta-analysis of clinical trials. PloS One 2012; 7: e47559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Woodcock T, Morganti-Kossmann MC. The role of markers of inflammation in traumatic brain injury. Front Neurol 2013; 4: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.