Abstract
Anterior sacral meningocele is a very rare clinical entity characterized by herniation of a meningeal sac through a sacrococcygeal defect. We report a case of a 20-year old female with Marfan syndrome who presented with abdominal distention that was misdiagnosed as an ovarian cyst on pelvic ultrasound. Pelvic magnetic resonance (MR) imaging showed large, well-defined multiloculated intrasacral and presacral cysts communicating via two separate broad necks and extending through defects in anterior aspect of sacral vertebrae. This case emphasizes that anterior sacral meningocele should be considered in the differential diagnosis of cases with pelvic cysts particularly in patients with underlying connective tissue disorders. Because severe neurologic complications or even death may occur without proper preoperative planning in such cases, MR imaging should always be performed for evaluation and characterization of pelvis cystic lesions.
Key words: Abdominal distension, anterior sacral meningocele, Marfan syndrome, ovarian cyst
Introduction
Anterior sacral meningocele (ASM) is a very rare presentation of spinal dysraphism, characterized by herniation of the meningeal sac through a bone defect (focal erosion or hypogenesis of segments of the sacrum and coccyx) in the anterior aspect of the sacrum.1,2 ASM is primarily an isolated congenital anomaly, but it may be associated with underlying connective tissue disorders including neurofibromatosis type 1 (NF-1), Marfan syndrome, and Ehlers-Danlos syndrome.3-5 In this article, a rare case of ASM misdiagnosed as an ovarian cyst on pelvic ultrasonography (US) and characterized by the magnetic resonance imaging (MRI) findings of ASM in a patient with Marfan syndrome is reported and the role of imaging is discussed for diagnostic workup of ASM.
Case Report
A 20-year old female was admitted to our gynecology department from an outside hospital with the presumed diagnosis of an ovarian cystic mass. The patient’s complaint was gradual abdominal distension for one year. Pelvic US at the outside hospital was suggestive of an ovarian cystic mass occupying nearly the entire pelvis and displacing the uterus. The patient was referred to our hospital for operation. She had a history of Marfan syndrome manifesting with kyphoscoliosis, mitral valve prolapsus and severe mitral valve regurtation. Pelvic examination revealed a pelvic mass extending up to the umbilical region. There were no focal neurological deficits. Routine blood biochemical tests were within normal limits. Preoperative contrast-enhanced pelvic MRI, performed for characterization of cystic mass, demonstrated large, well-defined multiloculated intrasacral and presacral cysts communicating via two separate broad necks and extending through defects in anterior aspect of sacral vertebrae (Figure 1). A connection between the pelvic multicystic lesion and dural sac was clearly observed on sagittal MRI images. The cystic fluid was similar to cerebrospinal fluid (CSF) signal intensity. There were neither nerve roots nor solid components within the mass. No contrast enhancement was detected. Uterus and adnexa were inferiorly displaced by the mass. A diagnosis of ASM was established based on these findings. The patient was informed about surgical management. The operation for ASM was planned after mitral valve repair surgery because of severe mitral valve regurgitation.
Figure 1.
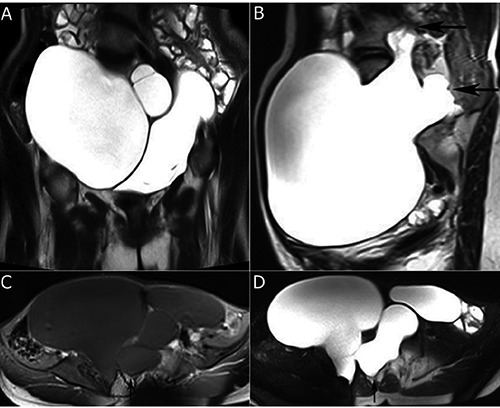
Anterior sacral meningocele in a patient with Marfan syndrome. Coronal T2-weighted magnetic resonance (MR) image (A) shows very large, well-defined multiloculated cystic mass occupying nearly entire pelvis. Sagittal T2-weighted MR image (B), axial T1- (C) and T2-weighted (D) images demonstrate the connection between presacral and intrasacral cysts via two separate broad necks (arrows).
Discussion
ASM occurs as a result of a sacrococcygeal defect with herniation of a meningeal sac occasionally with neural elements into the pelvis presenting as a presacral pelvic mass.1,2 The average incidence of neural tube defects is 1-2 per 1000 births; however, the incidence of ASM remains unknown because of the asymptomatic characteristics.3 ASM is associated with the heritable (autosomal dominant) Currarino syndrome, characterized by the triad of sacral defect, presacral mass (i.e. meningocele), and anorectal malformations.3
ASMs account for approximately 5% of retrorectal masses and commonly present in the second and third decades of life, more often in women, at a ratio 4:1.2,6 They may be asymptomatic or may present with a pelvic mass causing symptoms in two-thirds of cases related to compression of surrounding structures by the herniated meningeal sac; neurological symptoms due to spinal cord tethering; or compression on sacral nerve roots including urinary dysfunction, dysmenorrhea, dyspareunia, constipation, perineal hypoalgesia, lower back pain, sacral numbness, and paresthesia in the lower extremity; central neurological symptoms including headache and nausea secondary to increased intraabdominal pressure or its complications in the form of meningitis.6-9 Our patient had no symptoms other than abdominal distention despite a significantly large ASM.
Marfan syndrome is an inherited connective tissue disorder with classical manifestations of cardiovascular, skeletal, and ocular abnormalities.3,9 It is suggested that weakness of the dura mater, which cannot protect the bony structures against the pressure of CSF pulsations, results in dural ectasia with gradual remodeling and bone erosion.9 Arachnoid herniation due to focal dural tears can cause meningocele formation with cyst expansion and further bone erosion. High frequency of dural ectasia (up to 92%) has been reported in patients with Marfan syndrome.3 Several ASM cases associated with Marfan syndrome have been described in the literature,10-13 but only a few cases have been presented as a pelvic cyst, as in our case.5,7,9 Few cases of isolated ASM misdiagnosed as an ovarian cyst have been reported.7,8,14 Ultrasonography is usually the first-line imaging study for suspected pelvic lesion and a very useful screening tool in the diagnosis of cysts as well as in follow-ups. However, as the case was presented in this report, the extent and origin of the pelvic cystic lesion can be difficult to detect with US. A detailed clinical examination and further imaging studies with computed tomography (CT) and/or MRI may be required to differentiate ASM from other causes of cystic presacral masses, including ovarian cyst, rectal duplication cyst, neuroectodermal cyst, perineural cyst, teratoma, dermoid/epidermoid cysts, hydatid cyst, pyogenic abscess, lymphangioma, and aneurysmal bone cyst.6,7
ASMs can mimic an adnexal cystic lesion on physical examination, but they are located more posteriorly unless they are very large, as in this case.7,9 Rectal examination may provide diagnosis by revealing soft presacral mass. The other diagnostic studies include plain radiograph, US, myelography, contrast enema, CT, and MRI. Imaging studies show a deficient sacrum and variably sized cysts extending into the pelvis through an enlarged sacral foramen. To provide the diagnosis, communication between the cyst and the subarachnoid space must be determined.
It is generally accepted that a scimitar shaped sacrum (a smooth concave unilateral sacral defect) is considered to be diagnostic of ASM on plain radiograph.2 However, bone defects vary from an enlarged foramen to complete sacral agenesis.1 Contrast enema may show displacement of rectum, sigmoid colon, and urinary bladder. However, CT and MRI are the most valuable methods in depicting the detailed anatomy of the ASM and in the planning of the surgical treatment.
CT is helpful in providing comprehensive information about bony anomalies and CSF density of the cyst.7 Intrathecal contrast-enhanced CT is the technique of choice because it demonstrates the communication between the meningocele and the dural sac and also visualizes associated tumors with filling defects. However, this technique has been replaced by MRI as the radiological investigation of choice because CT is invasive and has the disadvantage of radiation.
MR imaging is often diagnostic with particular advantages in the evaluation of ASM. MR is a rapid, safe, and noninvasive modality with high soft tissue contrast and multiplanar imaging capability. MRI can better characterize the details including the size, shape, anatomical relations to the surrounding structures, and internal characteristic CSF intensity of the cystic mass without use of intrathecal contrast material in the spinal canal.7 MRI can demonstrate communication between the ASM and the dural sac and also can provide comprehensive information about any associated pathologies such as a tumor and/or spinal cord tethering.4 However, MRI may fail to demonstrate narrow subarachnoid communications of a small-necked lesion with the subarachnoid space in which CT myelography may be useful.6,7
Conservative management is indicated in cases of asymptomatic stable ASM.15 Neurosurgical approach is recommended for symptomatic lesions, particularly when there are neurological deficits or bowel and bladder involvement, or an increase in the size of the lesion due to increased hydrostatic pressure.7,15 The goals of the surgery are to obliterate the communication between the ASM and subarachnoid space, and to release tethering of the spinal cord and/or spinal roots, if necessary.
Conclusions
ASM, a rare clinical entity, can easily be misdiagnosed as a commonly seen ovarian cyst. The diagnosis of ASM should always be considered in cases with atypical pelvic cysts, particularly in patients with a diagnosis of Marfan syndrome or NF-1. Because severe neurologic complications or even death may occur without proper preoperative planning in such cases, MR imaging should always be performed for evaluation and characterization of pelvis cystic lesions.
References
- 1.Wilkins RH. Lateral and anterior spinal meningoceles. Wilkins RH, Regachary SS, Neurosurgery, 2nd ed New York, NY: McGraw-Hill; 1996. pp 3521-5. [Google Scholar]
- 2.Villarejo F, Scavone C, Blazquez MG, et al. Anterior sacral meningocele: review of the literature. Surg Neurol 1983;19:57-71. [DOI] [PubMed] [Google Scholar]
- 3.Chen CP. Syndromes, disorders and maternal risk factors associated with neural tube defects (II). Taiwan J Obstet Gynecol 2008;47:10-7. [DOI] [PubMed] [Google Scholar]
- 4.Shedid D, Roger EP, Benzel EC. Presacral meningocele: diagnosis and treatment. Semin Spine Surg 2006;18:161-7. [Google Scholar]
- 5.Nallamshetty L, Ahn NU, Ahn UM, et al. Dural ectasia and back pain review of the literature and case report. J Spinal Disord Tech 2002;15:326-9. [DOI] [PubMed] [Google Scholar]
- 6.Beyazal M. An asymptomatic large anterior sacral meningocele in a patient with a history of gestation: a case report with radiological findings. Case Rep Radiol 2013;2013:ID842620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polat AV, Belet U, Aydin R, Katranci S. Anterior sacral meningocele mimicking ovarian cyst: a case report. Med Ultrason 2013;15:67-70. [DOI] [PubMed] [Google Scholar]
- 8.Erdogmus B, Yazici B, Ozdere BA, Safak AA. Anterior sacral meningocele simulating ovarian cyst. J Clin Ultrasound 2006;34:244-6. [DOI] [PubMed] [Google Scholar]
- 9.Voyvodic F, Scroop R, Sanders RR. Anterior sacral meningocele as a pelvic complication of Marfan syndrome. Aust NZJ Obstet Gynaecol 1999;39:262-5. [DOI] [PubMed] [Google Scholar]
- 10.Strand RD, Eisenberg HM. Anterior sacral meningocele in association with Marfan’s syndrome. Radiology 1971;99:653-4. [DOI] [PubMed] [Google Scholar]
- 11.Raftopoulos C, Pierard GE, Rétif C, et al. Endoscopic cure of a giant sacral meningocele associated with Marfan’s syndrome: case report. Neurosurgery 1992;30:765-8. [DOI] [PubMed] [Google Scholar]
- 12.Schneider MB, Dittmar S, Boxer RA. Anterior sacral meningocele presenting as a pelvic/abdominal mass in a patient with Marfan syndrome. J Adolesc Health 1993;14:325-8. [DOI] [PubMed] [Google Scholar]
- 13.Rigante D, Segni G. Anterior sacral meningocele in a patient with Marfan syndrome. Clin Neuropathol 2001;20:70-2. [PubMed] [Google Scholar]
- 14.Ficicioglu C, Baykal C, Arioglu P, et al. Anterior meningocele misdiagnosed as an ovarian cyst. Gynecol Obstet Invest 2008;65:21-3. [DOI] [PubMed] [Google Scholar]
- 15.Trapp C, Farage L, Clatterbuck RE, et al. Laparoscopic treatment of anterior sacral meningocele. Surg Neurol 2007;68:443-8. [DOI] [PubMed] [Google Scholar]


