Abstract
Objective
To document the lived experiences of people with both poor mental health and suboptimal adherence to antiretroviral therapy in high HIV prevalence settings.
Methods
In-depth qualitative interviews were conducted with 47 (female =31) HIV-positive adults who scored above the cut-point on a locally-validated scale for common mental disorders. Purposive sampling was used to recruit participants with evidence of poor adherence. Six additional key informant interviews (female = 6) were conducted with healthcare workers. Data were collected and analysed inductively by an interdisciplinary coding team.
Results
The major challenges faced by participants were stressors (poverty, stigma, marital problems) and symptoms of common mental disorders (“thinking too much”, changes to appetite and sleep, “burdened heart”, and low energy levels). Thinking too much, which appears closely related to rumination, was the symptom with the greatest negative impact on adherence to antiretroviral therapy among HIV-positive adults with common mental disorders. In turn, thinking too much was commonly triggered by the stressors faced by people living with HIV/AIDS, especially poverty. Finally, participants desired private counselling, access to income generating activities, and family engagement in mental health care.
Conclusions
Better understanding of the local expression of mental disorders and of underlying stressors can inform the development of culturally sensitive interventions to reduce common mental disorders and poor adherence to antiretroviral therapy.
Keywords: HIV/AIDS, depression, mental health, adherence, antiretroviral therapy, barriers
Introduction
In low and middle countries (LMICs), common mental disorders (CMDs), mainly mood and anxiety disorders, have an estimated lifetime prevalence of 22% [1] and often remain undiagnosed and untreated [2]. CMDs, especially depression, are often comorbid with other chronic illnesses, such as diabetes [3], epilepsy [4], cardiovascular disease [5], and HIV/AIDS [6-8]. For people with these chronic diseases, CMDs can be a major barrier to adherence to daily medication routines. In particular, the effects of depression on antiretroviral therapy (ART) adherence for people living with HIV/AIDS (PLWHA) are well established in several contexts [9-18]. Depression may affect adherence by impairing concentration, memory, problem solving, and motivation [19-22]. Moreover, poor mental health predicts faster HIV progression when controlling for adherence [23-26]. Developing interventions to tackle depression and other CMDs in PLWHA is thus critical in addressing the global HIV/AIDS pandemic [12,27,28].
Core experiences of CMDs appear to differ cross-culturally [29-32]. In Zimbabwe, a core experience of CMDs is ‘kufungisisa,’ which translates directly from Shona as “thinking too much” [33-35] and is experienced by up to 80% of Zimbabweans with CMDs [36]. Research from several other countries including Uganda [37], Tanzania [38], Nepal [39], Nicaragua [40], Cambodia [41], and Haiti [42] have demonstrated that thinking too much is a common core component of common mental disorders in many different contexts and has now been included in the new Diagnostic and statistical manual of mental disorders (DSM-5) [43]. Kufungisisa appears closely related to symptoms of worry and rumination associated with depression and anxiety disorders [44]. Research in Zimbabwe has also provided preliminary evidence that brief psychological therapy based on problem solving therapy (PST) is an appropriate and effective intervention for CMDs and symptoms such as kufungisisa [45]. This baseline understanding of CMDs in Zimbabwe provides a useful starting point in the development of a culturally appropriate psychosocial intervention for PLWHA. Additional research on quality of life for patients on ART has become a major public health focus [46], and has improved our understanding of the factors that play into wellbeing for PLWHA such as “live-ability” of the patient's environment. While several studies that use this framework have been conducted in countries such as Uganda [47,48], no such research have been conducted in Zimbabwe and there is still limited understanding of the determinants or nature of CMDs specifically among PLWHA in Zimbabwe.
This qualitative study sought to inform the development of a culturally-appropriate intervention in Zimbabwe for PLWHA with comorbid CMDs and poor adherence to ART. Research from the United States (US) has shown that interventions based on motivational interviewing, problem-solving around barriers to adherence, and cognitive behavioral therapy (CBT) can improve mental health and adherence to ART in depressed PLWHA [49-51]. A key step in designing a similar intervention is to understand the lived experiences of patients within their local context. For an intervention focused on both CMDs and adherence, an appreciation of the major factors contributing to both poor mental health and poor adherence is crucial. In addition, it is useful to understand the facilitators for an intervention in this population in order to meet context-specific needs and preferences. Since very little was known about the lived experiences of HIV- positive adults with co-morbid CMDs and poor adherence in Zimbabwe, qualitative methods were appropriate for exploring in-depth features of their lives to help develop a culturally-appropriate intervention [52].
Methods
Setting
The study was conducted from August 2013 to July 2014 at the HIV clinic of Parirenyatwa Hospital in Harare, Zimbabwe: one of the largest HIV treatment facilities in the country with a total enrolment of over 8000 patients. Adherence counseling is provided for all patients, and those with mental health problems are referred to psychiatric services. Prior to our study, adherence counseling at the clinic included giving a broad range of information about HIV, ART, and sexual behavior rather than focusing on helping the patient with adherence. Sometimes, this included reprimanding patients for non-adherence and describing the grave, potentially fatal consequences of poor adherence
Study Design and Sample
We conducted 47 in-depth, qualitative interviews. Inclusion criteria were adult patients (18 years and older) who scored greater than 5 on the Shona version of the Self Report Questionnaire (SRQ-8) [53] - a culturally-adapted and validated psychiatric screening tool for CMDs in Zimbabwe. We used purposive sampling to capture participants thought likely to benefit from additional support to promote adherence. Indication of potential poor adherence was via any one of: 1) referral of patients with biological surrogates suggesting poor adherence (a CD4 count below 350 that had fallen since the last clinic visit or a viral load that had increased since the last clinic visit); 2) self reported missed doses in the last 6 months; or 3) self reported missed clinic visits in the last 6 months. Following interviews, all clients with significant mental health needs were linked to psychiatric services in an adjacent hospital. Additionally, we conducted 6 key informant interviews with healthcare workers (HCWs) involved in the HIV management of these patients. Among HCWs, several key informants such as counselors, nurse practitioners, and a clinical psychologist were identified as particularly knowledgeable about the psychosocial issues affecting clinic attendees. Characteristics of the interview sample are presented in Table 1.
Table 1.
Participant Characteristics
| Patients | |
| Male | 16 (34.04%) |
| Female | 31 (65.96%) |
| Age | Mean 41.7; SD. 11.3 |
| SRQ | Mean 5.6; SD. 1.5 |
| CD4 | Mean 306.2; SD. 187.9 |
| 1st line ART | 27 (57.4%) |
| 2nd line ART | 20 (42.5%) |
| Healthcare Workers | |
| Female | 6 (100%) |
| Adherence counsellors | 3 (50%) |
| Nurse Practitioners | 2 (33.3%) |
| Clinical Psychologist | 1 (16.7%) |
Data Collection
Interviews lasted between 45 and 65 minutes. The interviewers were local Zimbabweans with training in qualitative research and fluency in the local vernacular (Shona). The initial interview guide was written in English, translated into Shona, and back translated to ensure clarity. The guide was piloted in a non-clinical setting and adjusted in order to ensure that conversations were non-leading and flowed well. Interviewers were trained to use the interview guide (Table 2) in both languages and gave participants the option of participating in English, Shona, or a combination of the two. The interviewers used the guide (and a modified version for HCWs) to speak to participants about their experiences on ART, their challenges in life, and what motivated them to stay alive.
Table 2.
Interview Guide
| 1. How are you? |
| 2. How did you travel here today? |
| 3. Tell me a little bit about your medication. |
| 4. When was the last time you missed a dose? |
| a. Can you tell me about what happened? |
| 5. Describe the experience of getting drugs at the clinic for you. |
| 6. When you were first diagnosed wit HIV and they started you on ARVs, what did they tell you? |
| a. Was it useful? |
| 7. What challenges do you face? |
| 8. What are your reasons for staying alive? |
| 9. I'm going to read out a list of things. (Slowly read list of symptoms of common mental disorders). Do you ever feel any of these things? |
| a. Tell me about it. |
| 10. What do you understand by “depression”? |
| a. What causes it? |
| b. What can be done for it? |
| 11. We are trying to see if we can give counselling to some people who are struggling to take their medication. Has counselling been beneficial for you? |
| a. If not, how can we help improve it? |
| 12. What would be some of the difficulties you would face if you had to come for counselling once a week, for a month? |
| a. What could make it easier to come? |
| 13. If you wanted to talk about some of the problems you have been facing, what would be the best setting? |
Researchers ensured a constant comparative approach to data collection by discussing emerging themes throughout the data collection process [54]. In weekly meetings, the interviewers gave feedback to the senior qualitative researcher (KK) about emerging themes and the suitability of the interview guide. These discussions formed an important preliminary analysis, which allowed the interview guide to evolve in parallel with data collection and assisted in determining when theoretical saturation had been reached [55], after which no additional interviews were conducted. All interviews were audio-recorded and later transcribed verbatim. Two participants elected not to be audio recorded, so interviewers took hand-written notes instead.
Data Analysis
Two Zimbabweans with Master's degrees and training in qualitative health research (KK, DM) each independently reviewed three randomly-selected transcripts and met three times in order to develop a mutually-agreeable, initial coding framework. The same researchers then performed line-by-line open coding of each individual transcript using the initial framework and met frequently to reconcile codes. NVivo QSR 10 was used to assist data analysis and retrieval.
The research team then met several more times, both face-to-face and via video conferencing. The team developed hypotheses inductively, performing axial coding (sorting codes into categories and determining how these categories are interconnected) and then selective coding (integrating concepts to form a descriptive model) [54]. Selected quotations are used in the results section to illustrate the major themes that emerged.
Ethical Considerations
We obtained informed written consent from all participants. Ethical approval for the study was obtained from: Research Council of Zimbabwe, Medical Research Council of Zimbabwe, the Joint Research and Ethics Committee of the University of Zimbabwe, and the Research Ethics Office of King's College, London.
Results
This study provides insight into the experiences of PLWHA with comorbid depression and poor adherence to ART. Participants described the major challenges they experienced in their daily lives, which were stress-ors (poverty, stigma, and marital problems) and symptoms of CMDs (thinking too much kufungisisa, burdened heart moyo unorwadza, changes to appetite and sleep, and low energy levels). These challenges further impacted on adherence and access to ART in variety of ways. Participants also described ideas for the intervention. A description of these results is presented below and illustrating quotations from participants are provided in Table 3 and Table 4. Figure 1 is a diagrammatic representation of our findings.
Figure 1.
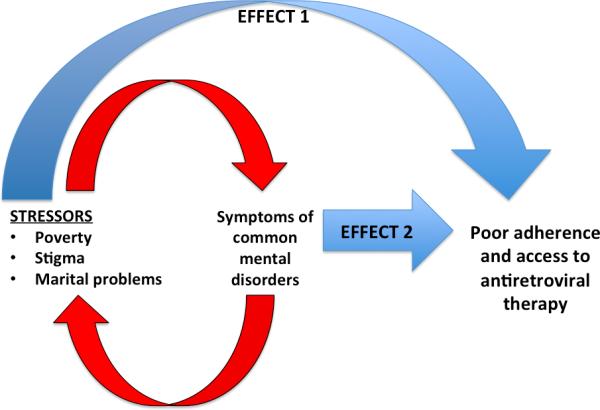
Effects of stressors and symptoms of common mental disorders on ART adherence
Challenges
Poverty
Poverty was the most significant challenge faced by participants in this is study, most of whom attended the clinic because ART is dispensed free of charge. HCWs noted that the plight of many patients at the clinic was related to the overarching economic climate and high unemployment rate in Zimbabwe:
A lot of patients who come to us are people who are not working, because they get their medication for free, they get medical facilities free ... So obviously they have financial problems and because the economy is not doing very well, they do not have any support from the government ... the economy is so bad, so these things affect them. And you notice them when they come, they're talking about these problems: ‘No money for rent. No money for school fees.’ A lot of their children have dropped out of school because of a lack of finances. So that has affected a lot of our clients (Clinical psychologist).
Not having enough money was a barrier to meeting essential needs such as food and also reduced the mobility of patients, who could not afford rising transport costs. Participants cited poverty as a cause of their symptoms:
Now my child has been sent back home from school. What am I supposed to do with the child? I started crying. I don't have anything to do. I don't go to work. Sometimes I wash clothes and sweep for people for money. But right now, I don't have anything to do, not even selling sweets. My child is not going to school (ID# 28, Female, 44yrs).
I was thinking about money to pay rent so I had a lot on my mind ... Sometimes I feel depressed when my money is not enough (ID#23, Female, 32yrs).
Stigma
Participants faced stigma both within the wider community and in their families:
Where I go for laundry they don't know that I am [HIV] positive. Today, I told them that my mother is not feeling well and I want to go with her for a check up. I cannot tell them that [I am HIV-positive]... stigma is still there (ID#28, Female, 44yrs).
If the family undergoes counselling they get to understand the need that there is no need to discriminate or isolate their relative living with HIV in terms of food and beverages as well as ablution facilities. This helps in that if this person is accepted, he will not be stressed as he has a support system (Nurse 3).
Self-disclosure was a major issue and most participants experienced internalized stigma and felt that they could not tell work colleagues, friends, or family about their HIV statuses. Participants were also prone to external stigma, and were often ostracized from communities or families: “If our friends and relatives understand that being HIV-positive does not mean you are promiscuous, life would be much better” (ID#16, Female, 32yrs). The constant battle with stigma and difficulty in maintaining privacy was often a source of stress and worry for participants.
Marital problems
Most married women in this study, including those married to serconcordant men, faced marital problems. They frequently made comments such as, “I sometimes get depressed because my husband wants a baby but my cells have not yet reached the required number for me to get pregnant” (ID#23, Female, 32yrs). These problems were entangled in greater issues of HIV status disclosure, economic hardship, the maternal burden of care, and patriarchy. Women described husbands to be stingy with sharing their incomes, compounding the stress of financial constraints for many women:
My husband does not give me a single cent. He earns a lot of money but he does not give us a cent ... The other day, he said to me, ‘let's go to a wedding.’ I said, ‘I don't have clothes to wear,’ so he said, ‘that's okay,’ and just left me alone and went by himself. I think what my husband is doing actually depresses me (ID#30, Female, 44yrs).
The burden of maternal care for women was also significant, as several felt abandoned and had to perform all parental duties alone:
I was once married before and I have a child. Then I got married a second time, so my husband doesn't like my child that much. The living conditions for my child are harsh. That's what stresses me a lot (ID#26, Female, 30yrs).
Many women said that their husbands abused them verbally and physically, or asserted their dominance in the household to a degree that severely limited the perceived freedom of most women: I was being mentally abused and physically abused, so it was tough for me (ID#38, Female, 28yrs).
Symptoms of CMDs
For many participants, the symptoms they experienced relating to depression and anxiety posed a significant challenge because many of these symptoms hindered their daily activities. Some participants described having ‘burdened hearts’ (moyo unorwadza) when explaining their worries, giving the impression that they were weighed down by this anxiety and worry: My heart feels burdened and I think about how long I will survive like this. (ID#25, Female, 39yrs).Respondents also experienced low energy, lack of appetite, and social withdrawal:
After crying, I fell asleep. I didn't even think of cooking for my child. I spent the whole day like that.” (ID#28, Female, 44yrs)
What I've noticed, when I'm very much under stress, although my stress sometimes happens maybe before or after, you don't have appetite. (ID#33, Female, 49yrs)
However, the most prominent and challenging symptom mentioned by every participant was kufungisisa, or ‘thinking too much’: Being depressed is thinking too much. It's when you are burdened (ID#32, Male, 66yrs). Participants described kufungisisa as negative or stressful thoughts that filled their minds all the time. Participants would ‘think too much’ about the other challenges in their lives such as financial constraints, stigma, and marital problems:
I was thinking about money to pay rent so I had a lot on my mind... If your mind is always occupied you will not become strong because your brains will be occupied always (ID#23, Female, 32yrs).
You start to ask yourself questions which were answered long back. You revisit some of these questions. Till when am I going to be taking this medication? When is the cure going to be discovered? When it's discovered will I be still alive? (ID#10, Female, 40yrs).
They would also think too much about the causes of past failures and present difficulties (“I ask myself if this is happening in other people's marriages”) and about potential future problems (“Who will look after the child?”). These negative thoughts were very absorbing and often occupied patients’ minds to the degree that it hindered accomplishing tasks within their daily routine, including ART adherence.
Impact of challenges on adherence and access to ART
Below we describe how the challenges faced by participants were not only stressors that led to poor mental health but also difficulties that impacted ART access and adherence (See Figure 1).
Poverty
Respondents described poverty as a barrier to adherence and access to ART in several ways. The most common challenge was that without enough money, participants could not pay for transport costs from rural locations to the clinic – thus posing a barrier to access of ART:
A lot of people are now going to the rural areas because they can't afford to pay rent in the urban areas, which will affect pill taking as well, because when they go to the rural area they don't have money to come back and get their medication (Clinical Psychologist).
Many participants said they could not afford to feed themselves or their families:
Money is a very big problem. Sometimes I have to sell a chicken, and they're almost finished. I have to sell two chickens for me to come here [the HIV clinic], 7 dollars each, to and fro (ID#31, Male, 37yrs).
I usually come here around 7:30 or 8:00, depending on whether I get transport from Mtoko... When I get into town, I walk from Fourth street to Parirenyatwa Hospital carrying my child on my back so that I can save money to buy her food (ID#34, Female, 33yrs).
Stigma
Stigma faced by participants made it difficult both to take ART and to access it. Participants were afraid that members in their communities (neighbours, friends, relatives) would find out where they had been when they came to the clinic. This deterred them from attending the clinic, and reduced access to ART. Participants avoided taking their medications in public settings and even in their own homes in the presence of close family members. This particularly became an issue at events where many family members or friends were gathered, such as at funerals:
Usually when you travel and also when you attend some functions, such as funerals. If you don't find time to get away and have your pills, as you know, people are still looking down on you. Stigmatizing you (ID#18, Female, 65yrs).
Marital problems
The challenges faced by women in their marriages also led to difficulties adhering to or accessing ART. For example, women married to seroconcordant men often had to share their ART with their husbands, who were too embarrassed to attend clinics on their own:
In married couples the female might be the one who has been tested and is supposed to be put on medication. Then the husband is not tested and he'll just say your status is the same as mine. So the wife will be having the problem that ... the husband will be taking the medication as well. So the wife might not feel comfortable to come back and say my medication is no longer enough (Nurse 1).
Other women in abusive relationships had to flee their homes, forgetting to take their ART with them:
Sometimes I would quarrel with my husband and he would threaten to shoot me. I could run to the police station but at that time I could have left my tablets at home, you see (ID#38, Female, 28yrs).
Symptoms of CMDs
Symptoms of CMDs, especially kufungisisa, reduced adherence to ART. Participants perceived their minds to be occupied by thoughts about the challenges they were experiencing in life. These negative thoughts were very consuming and made it difficult for participants to concentrate on their daily tasks. Respondents said that kufungisisa made them forgetful and that this was a common cause for skipping doses of ART:
It's the thinking too much that makes me forget to take my medication. If I am not thinking too much about anything, I remember to take my medication on time. When nothing is in my brain, I remember and take them on time (ID#25, Female, 39yrs).
For some participants, these negative thoughts were so absorbing that they did not even notice the regular reminders (such as alarms) that they had in place to help with taking ART on time:
When I am thinking too much then I forget, even if the phone [alarm] rings, if my thoughts are not collected, I fail to realize that it is ringing for me to take my medication (ID#5. Female, 31yrs).
Intervention Ideas
Family engagement and disclosure
Nearly all respondents said that relationships with family members, especially children, were a source of hope and reason to stay alive. Participants wanted to support their children financially and emotionally and live to see them grow up. Many participants cited a future celebratory occasion such as child's graduation or coming of age as moments to look forward to and be present for:
My children motivate me to live longer because when I look at their age, it inspires me. I always wish that God could increase the number of years I live, so that I can see my children grow up and take care of themselves (ID#2, Female, 37yrs).
Participants also depended on family as a source of support for dealing with the realities of being HIV-positive and the routine of ART. For example, respondents said that their children often reminded them to take their ART on time:
I usually forget to take my medication. Like on Monday I had forgotten, but my child reminded me when I was going to bed. She said, ‘Mum, you haven't taken your pills.’ ... What happened is I had a lot on my mind and I was thinking too much (kufungisisa)... (ID#25, Female, 39yrs).
HCWs were in favour of engaging family members to help with adherence and with mental health. They confirmed that self-disclosure to family members was an important step for attaining good adherence. The family is important because they support a person living with HIV. That is why we encourage family members to be informed. They are also supposed to undergo counselling to get assistance... It encourages him to take medication, peace of mind knowing that the people at home love him as he is. It will be easier. The family plays an important role. So informing the family and other close friends might benefit him especially if they empowered with information on HIV they will be able to help him (Nurse 3).
Income generation and transport
Since poverty was the most significant challenge for most participants, many felt that they needed direct financial assistance and/or support seeking employment. Some participants had heard of income generation projects at other clinics and wanted to know more about accessing this type of assistance:
I also wanted to say something concerning these projects which are being talked about especially for [HIV]-positive people. I am being taught, but I don't have the capital. I think there should be a small fund from the government or NGOs to assist (ID#45, Female, 42yrs).
Participants needed financial assistance particularly for transport costs, and many stated that they would attend clinic more regularly if they could meet these costs. HCWs suggested that improving transportation for patients was a key area for improvement to assist patients: You might [provide] money for transport so we don't have a situation that someone will say they cannot come because they have no money for transport. I think if this happens it would help a lot (HCW 4).
Private settings
Privacy was a major priority for participants, who wanted to be able to discuss their personal affairs in a setting that afforded personalized psychosocial care from HCWs that they could trust. Respondents bemoaned the current lack of confidentiality at the clinic and said that they often received counselling in clinical compartments separated only by curtains, allowing other patients and HCWs to overhear personal conversations.
Somewhere private, definitely private. I'm the kind of person who doesn't want to divulge my personal information to everyone, so a private setting would do. These curtains give you a sense of privacy, but they are not private (ID#33, Female, 49yrs).
When asked for the ideal environment in which to deliver a psychological intervention, most respondents stressed that one-on-one sessions were preferable to group therapy, especially during initial stages immediately following status disclosure: One to one would be more effective, because I can actually ask you where did I get it, and you can actually help me in the problems, in my personal problems (ID#36, Male, 49yrs).
Discussion
This study explored the lived experiences of adults on ART with co-morbid CMDs and poor adherence in Zimbabwe. It highlighted major challenges, the impact of these challenges on adherence and access to ART, and proposed interventions for this population. We confirm findings from previous research that challenges such as poverty and stigma are key barriers to ART adherence in LMICs [56-59], including Zimbabwe [60] (Effect 1 in Figure 1). Our study finds that these barriers have an additional negative effect on ART adherence: they contribute to poor mental health, which in turn causes poor adherence (Effect 2 in Figure 1) [10,17,61]. For example, poverty makes it difficult to access ART for patients attending an urban hospital through inability to meet transport costs, however, it also acts as a stressor that feeds into CMDs, leading to poor adherence.
This study documents the importance of ‘thinking too much’ or ‘kufungisisa’ in linking low mood and poor adherence to ART. Kufungisisa was commonly triggered by the severe stressors faced by PLWHA, especially poverty. Many of the experiences of kufungisisa appear to align with rumination, in that they involved repetitive negative thinking about past, present, and future events [62].
Our findings are consistent with research from South Africa on HIV-positive women with depression, which showed that poverty, stigma, and marital problems were major challenges for this population [63]. However, our study was unique in that it included PLWHA with both CMDs and suboptimal adherence to ART. While previous research in Zimbabwe has suggested that kufungisisa may be a significant component of poor mental health for PLWHA in Zimbabwe [45], our study confirms this and suggests that it is the symptom with the greatest negative impact on adherence to ART in Zimbabwe. Since this is the first study to explore how kufungisisa may affect ART compliance, we extend current literature on barriers to ART adherence in Zimbabwe [60,64], and in other countries where ‘thinking too much’ is a core experience of CMDs.
Although dealing with the symptoms of CMDs was a major challenge itself for participants, many linked their symptoms to specific life stressors such as poverty, stigma, and marital problems. The symptoms of CMDs exacerbated the negative experiences of stressors, creating a cyclical relationship between those stressors and CMDs [65] (See Figure 1). Notably, kufungisisa was instrumental in establishing and sustaining the negative depressive cycle, because patients would ‘think too much’ about the difficulties that they were facing in their daily lives.
The most common challenge that participants ‘thought too much’ about was financial hardship. Poverty was pervasive among participants in the study, underscoring the close relationship between economic hardship and poor mental health. Although it is well established that in low- and middle- income countries mental illness and poverty are linked in a cyclical, mutually-reinforcing manner [66], the effect of such a relationship may be further pronounced in Zimbabwe, a country that not only has a high HIV prevalence but also has endured a serious economic recession over the last decade.
Our findings have several implications for the integration of mental health into HIV services in Zimbabwe – a key goal of the country's mental health policy [67] and an area of active engagement by international organizations working in the country such as USAID [68]. Given the twofold impact of stressors such as poverty on both CMDs and adherence to ART, this study emphasizes that mental health interventions for CMDs alone may not be sufficient to completely address the burden of CMDs in this population, especially when a concurrent goal is to improve adherence and access to ART. Tackling the stressors that feed into CMDs – poverty, stigma, marital problems – serves a dual purpose and is key to breaking the negative depressive cycle and to addressing major barriers to ART adherence.
Within our setting, these results can inform an intervention in a number of ways. First, our findings underscore the need for educating HCWs about how poverty, stigma, and marital problems impact on their patients’ ability to adhere to ART. Second, information about the sources of hope for this population, such as family relationships, is useful for motivating patients to engage with care and break the negative depressive cycle. This underscores the importance of disclosure and involvement of family members in the delivery of mental health care and promotion of adherence, as has been established in previous research [69-73]. Third, the emphasis on privacy in participants’ responses highlights the need for one-on-one interactions with HCWs, over group counseling interventions.
A significant limitation of our findings was social desirability bias among participants. We noted that participants were reticent to open up about episodes of poor ART adherence during the interview, likely due to fears of being reprimanded by clinic staff members. Despite this, we took several measures to ensure that participants felt comfortable to speak freely, including making audio-recording optional, phrasing questions in an open-ended manner, and using private rooms to conduct our interviews.
Our findings are limited in their generalizability to other contexts. The sample included only PLWHA with CMDs at one major HIV clinic, and did not incorporate the perspectives of those without CMDs or good adherents with CMDs. However, we prioritized an information-rich, purposive sample of poor-adhering clinic attendees with CMDs because this was the population for whom we were designing an intervention. Comprehensive perspectives on CMDs among PLWHA in the wider Zimbabwean community are still lacking, and this is an important area for future research.
Conclusions
Since this study was conducted, we have used our understandings of the challenges of PLWHA in Zimbabwe to adapt an adherence intervention that uses motivational interviewing techniques [19] and culturally-appropriate metaphors for HIV and ART. We have incorporated PST techniques focused on problem-solving around stigma and financial constraints. For example, by helping clients to change their appointment times to suit their schedules, to identify ways to take medication in private, and to generate solutions that enable them to seek employment, earn small amounts of capital, save, and invest. Ultimately, our findings demonstrate that an appreciation of stressors such as poverty on the mental health of PLWHA and a better understanding of the local expression of mental disorders are both crucial for developing culturally sensitive psychological interventions for adherence to ART and CMDs.
Acknowledgments and funding
This study was supported by NIH Research Grant 1R21MH094156-01 funded by the National Institute of Mental. We thank Helen Jack and Julia Weigel for reading and commenting on earlier drafts of this manuscript. We would also like to thank Jessica Magidson, Dr. C. Ndlovhu, and the personnel on the TENDAI project who have made this study possible. Finally, we thank the participants and healthcare workers at Parirenyatwa OI Clinic for taking the time to be part of this study.
References
- 1.Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohn . The treatment gap in mental health care. Bulletin of the World Health Organization; 2004. pp. 858–866. [PMC free article] [PubMed] [Google Scholar]
- 3.Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31:2398–2403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehndiratta P, Sajatovic M. Treatments for patients with comorbid epilepsy and depression: a systematic literature review. Epilepsy Behav. 2013;28:36–40. doi: 10.1016/j.yebeh.2013.03.029. [DOI] [PubMed] [Google Scholar]
- 5.Prince M, Patel V, Saxena S, Maj M, Maselko J, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 6.Olatunji BO, Mimiaga MJ, O'Cleirigh C, Safren SA, Olatunji BO, et al. Review of treatment studies of depression in HIV. Topics in HIV Medicine. 2006;14:112–124. [PubMed] [Google Scholar]
- 7.Brandt R. The mental health of people living with HIV/AIDS in Africa: a systematic review. African Journal of AIDS Research. 2009;8:123–133. doi: 10.2989/AJAR.2009.8.2.1.853. [DOI] [PubMed] [Google Scholar]
- 8.Chibanda D, Benjamin L, Weiss HA, Abas M. Mental, Neurological, and Substance Use Disorders in People Living With HIV/AIDS in Low- and Middle-Income Countries. J Acquir Immune Defic Syndr. 2014;67(Suppl 1):S54–67. doi: 10.1097/QAI.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 9.Amberbir A, Woldemichael K, Getachew S, Girma B, Deribe K. Predictors of adherence to antiretroviral therapy among HIV-infected persons: a prospective study in Southwest Ethiopia. BMC Public Health. 2008;8:265. doi: 10.1186/1471-2458-8-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campos L, Guimarães M, Remien R. Anxiety and Depression Symptoms as Risk Factors for Non-adherence to Antiretroviral Therapy in Brazil. AIDS and Behavior. 2010;14:289–299. doi: 10.1007/s10461-008-9435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Etienne M, Hossain M, Redfield R, Stafford K, Amoroso A. Indicators of adherence to antiretroviral therapy treatment among HIV/AIDS patients in 5 African countries. J Int Assoc Physicians AIDS Care (Chic) 2010;9:98–103. doi: 10.1177/1545109710361383. [DOI] [PubMed] [Google Scholar]
- 12.Nakimuli-Mpungu E, Bass J, Alexandre P, Mills E, Musisi S, et al. Depression, Alcohol Use and Adherence to Antiretroviral Therapy in Sub-Saharan Africa: A Systematic Review. AIDS and Behavior. 2011:1–18. doi: 10.1007/s10461-011-0087-8. [DOI] [PubMed] [Google Scholar]
- 13.Mayston R, Kinyanda E, Chishinga N, Prince M, Patel V. Mental disorder and the outcome of HIV/AIDS in low-income and middle-income countries: a systematic review. 2012;26(Suppl 2):S117–S135. doi: 10.1097/QAD.0b013e32835bde0f. [DOI] [PubMed] [Google Scholar]
- 14.Gupta R, Dandu M, Packel L, Rutherford G, Leiter K, et al. Depression and HIV in Botswana: a population-based study on gender-specific socioeconomic and behavioral correlates. PloS one. 2010;5:e14252. doi: 10.1371/journal.pone.0014252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, et al. Adherence to HAART: A Systematic Review of Developed and Developing Nation Patient-Reported Barriers and Facilitators. PLoS Med. 2006;3:e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nachega JB, Mills EJ, Schechter M. Antiretroviral therapy adherence and retention in care in middle-income and low-income countries: current status of knowledge and research priorities. Current Opinion in HIV and AIDS. 2010;5:70–77. doi: 10.1097/COH.0b013e328333ad61. 10.1097/COH.1090b1013e328333ad328361. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS Treatment Nonadherence: A Review and Meta-analysis. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2011;58:181–187. doi: 10.1097/QAI.0b013e31822d490a. 110.1097/QAI.1090B1013E31822D31490A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep. 2014;11:291–307. doi: 10.1007/s11904-014-0220-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Safren SA, W. Otto M, Worth JL, Salomon E, Johnson W, et al. Two strategies to increase adherence to HIV antiretroviral medication: Life-Steps and medication monitoring. Behaviour Research and Therapy. 2001;39:1151–1162. doi: 10.1016/s0005-7967(00)00091-7. [DOI] [PubMed] [Google Scholar]
- 20.Papakostas GI. Cognitive symptoms in patients with major depressive disorder and their implications for clinical practice. J Clin Psychiatry. 2014;75:8–14. doi: 10.4088/JCP.13r08710. [DOI] [PubMed] [Google Scholar]
- 21.Watkins E, Brown RG. Rumination and executive function in depression: an experimental study. J Neurol Neurosurg Psychiatry. 2002;72:400–402. doi: 10.1136/jnnp.72.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levens SM, Muhtadie L, Gotlib IH. Rumination and impaired resource allocation in depression. J Abnorm Psychol. 2009;118:757–766. doi: 10.1037/a0017206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leserman J. Role of Depression, Stress, and Trauma in HIV Disease Progression. Psychosomatic Medicine. 2014:76. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- 24.Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, et al. Mortality, CD4 Cell Count Decline, and Depressive Symptoms Among HIV-Seropositive Women: Longitudinal Analysis From the HIV Epidemiology Research Study. JAMA. 2001;285:1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 25.Ironson G, O'Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med. 2005;67:1013–1021. doi: 10.1097/01.psy.0000188569.58998.c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsai A, Chan B, Boum Y, Haberer J, Kembabazi A, et al. Mental Health and Mortality in an HIV Treatment Cohort in Rural Uganda. IAS-USA; Boston, MA: Mar 3-6, 2014. 2014. [Google Scholar]
- 27.Sherr L, Clucas C, Harding R, Sibley E, Catalan J. HIV and depression--a systematic review of interventions. Psychology Health & Medicine. 2011;16:493–527. doi: 10.1080/13548506.2011.579990. [DOI] [PubMed] [Google Scholar]
- 28.Abas M, Ali G, Nakimuli-Mpungu E, Chibanda D. Depression in people living with HIV in sub-Saharan Africa: time to act. Tropical Medicine and International Health. 2014 doi: 10.1111/tmi.12382. [DOI] [PubMed] [Google Scholar]
- 29.Andrew G, Cohen A, Salgaonkar S, Patel V. The explanatory models of depression and anxiety in primary care: a qualitative study from India. BMC research notes. 2012;5:499. doi: 10.1186/1756-0500-5-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patel V, Pednekar S, Weiss H, Rodrigues M, Barros P, et al. Why do women complain of vaginal discharge? A population survey of infectious and pyschosocial risk factors in a South Asian community. Int J Epidemiol. 2005;34:853–862. doi: 10.1093/ije/dyi072. [DOI] [PubMed] [Google Scholar]
- 31.Wolpert L. Malignant Sadness: the Anatomy of Depression. Faber & Faber; London: 2001. [Google Scholar]
- 32.Psaros C, Haberer JE, Boum Y, 2nd, Tsai AC, Martin JN, et al. The Factor Structure and Presentation of Depression Among HIV-Positive Adults in Uganda. AIDS Behav. 2014 doi: 10.1007/s10461-014-0796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abas M, Broadhead JC, Mbape P, Khumalo-Sakatukwa G. Defeating depression in the developing world: a Zimbabwean model. British Journal of Psychiatry. 1994;164:293. doi: 10.1192/bjp.164.3.293. [DOI] [PubMed] [Google Scholar]
- 34.Patel V, Abas M, Broadhead J, Todd C, Reeler A. Depression in developing countries: lessons from Zimbabwe. BMJ. 2001;322:482–484. doi: 10.1136/bmj.322.7284.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abas M, Broadhead JC. Depression and anxiety among women in an urban setting in Zimbabwe. Psychological Medicine. 1997;27:59–71. doi: 10.1017/s0033291796004163. [DOI] [PubMed] [Google Scholar]
- 36.Patel V, Simunyu E, Gwanzura F. The explanatory models and phenomenology of common mental disorders in primary care in Harare. Psychological Medicine. 1995;25:1191. doi: 10.1017/s003329170003316x. al e. [DOI] [PubMed] [Google Scholar]
- 37.Okello ES, Ekblad S. Lay concepts of depression among the Baganda of Uganda: a pilot study. Transcult Psychiatry. 2006;43:287–313. doi: 10.1177/1363461506064871. [DOI] [PubMed] [Google Scholar]
- 38.Kaaya S, Mbwambo J, Smith Fawzi M, Van Den Borne H, Schaalma H, et al. Understanding women's experiences of distress during pregnancy in Dar es Salaam, Tanzania. Tanzania Journal of Health Research. 2010;12:36–46. doi: 10.4314/thrb.v12i1.56277. [DOI] [PubMed] [Google Scholar]
- 39.Kohrt BA, Hruschka DJ. Nepali concepts of psychological trauma: the role of idioms of distress, ethnopsychology and ethnophysiology in alleviating suffering and preventing stigma. Cult Med Psychiatry. 2010;34:322–352. doi: 10.1007/s11013-010-9170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yarris K. “Pensado Mucho” (“Thinking Too Much”): Embodied Distress Among Grandmothers in Nicarguan Transnational Families. Cult Med Psychiatry. 2014:472–498. doi: 10.1007/s11013-014-9381-z. [DOI] [PubMed] [Google Scholar]
- 41.Hinton DE, Hinton AL, Eng KT, Choung S. PTSD and key somatic complaints and cultural syndromes among rural Cambodians: the results of a needs assessment survey. Med Anthropol Q. 2012;26:383–407. doi: 10.1111/j.1548-1387.2012.01224.x. [DOI] [PubMed] [Google Scholar]
- 42.Kaiser BN, Kohrt BA, Keys HM, Khoury NM, Brewster AR. Strategies for assessing mental health in Haiti: local instrument development and transcultural translation. Transcult Psychiatry. 2013;50:532–558. doi: 10.1177/1363461513502697. [DOI] [PubMed] [Google Scholar]
- 43.Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; Washington, D.C.: 2013. [Google Scholar]
- 44.Smith JM, Alloy LB. A roadmap to rumination: A review of the definition, assessment, and conceptualization of this multifaceted construct. Clin Psychol Rev. 2009;29:116–128. doi: 10.1016/j.cpr.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, et al. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. 2011;11:828. doi: 10.1186/1471-2458-11-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu AW. Quality of life assessment comes of age in the era of highly active antiretroviral therapy. AIDS. 2000;14:1449–1451. doi: 10.1097/00002030-200007070-00019. [DOI] [PubMed] [Google Scholar]
- 47.Mutabazi-Mwesigire D, Seeley J, Martin F, Katamba A. Perceptions of quality of life among Ugandan patients living with HIV: a qualitative study. BMC Public Health. 2014:14. doi: 10.1186/1471-2458-14-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stangl AL, Wamai N, Mermin J, Awor AC, Bunnell RE. Trends and predictors of quality of life among HIV-infected adults taking highly active antiretroviral therapy in rural Uganda. AIDS Care. 2007;19:626–636. doi: 10.1080/09540120701203915. [DOI] [PubMed] [Google Scholar]
- 49.Simoni J, Wiebe J, Sauceda J, Huh D, Sanchez G, et al. A Preliminary RCT of CBT-AD for Adherence and Depression Among HIV Positive Latinos on the U.S.-Mexico Border: The Nuevo Día Study. AIDS Behavior. 2013;17:2816–2829. doi: 10.1007/s10461-013-0538-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Safren SA, O'Cleirigh C, Bullis JR, Otto MW, Stein MD, et al. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2012;80:404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Safren SA, O'Cleirigh C, Judy T, Raminani S, Reilly LC, et al. A Randomized Controlled Trial of Cognitive Behavioral Therapy for Adherence and Depression (CBT-AD) in HIV-infected Individuals. Health Psychology. 2009;28:1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sofaer S. Qualitative methods: what are they and why use them? Health Services Research. 1999;34:1101–1118. [PMC free article] [PubMed] [Google Scholar]
- 53.Patel V, Todd C. The validity of the Shona version of the self report questionnaire (SRQ) and the development of the SRQ8. International Journal of Methods in Psychiatric Research. 1996;6:153. [Google Scholar]
- 54.Strauss A, Corbin J. Basics of Qualitative Research: Grounded theory procedures and techniques. 1990 [Google Scholar]
- 55.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for qualitative research. 1967.
- 56.Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19:658–665. doi: 10.1080/09540120701244943. [DOI] [PubMed] [Google Scholar]
- 57.Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM, Bimirew MA, et al. Barriers and facilitators of adherence to antiretroviral drug therapy and retention in care among adult HIV-positive patients: a qualitative study from Ethiopia. PLoS One. 2014;9:e97353. doi: 10.1371/journal.pone.0097353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tuller D, Bangsberg D, Senkungu J, Ware N, Emenyonu N, et al. Transportation Costs Impede Sustained Adherence and Access to HAART in a Clinic Population in Southwestern Uganda: A Qualitative Study. AIDS and Behavior. 2010;14:778–784. doi: 10.1007/s10461-009-9533-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Murray LK, Semrau K, McCurley E, Thea DM, Scott N, et al. Barriers to acceptance and adherence of antiretroviral therapy in urban Zambian women: a qualitative study. AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV. 2009;21:78–86. doi: 10.1080/09540120802032643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Skovdal M, Campbell C, Nhongo K, Nyamukapa C, Gregson S. Contextual and psychosocial influences on antiretroviral therapy adherence in rural Zimbabwe : towards a systematic framework for programme planners. Int J Health Plann Mgmt. 2011:296–318. doi: 10.1002/hpm.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30(Suppl 2):S171–176. doi: 10.1086/313849. [DOI] [PubMed] [Google Scholar]
- 62.Nolen-Hoeksema S, Wisco B, Lyubomirsky S. Rethinking Rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- 63.Petersen I, Hancock J, Bhana A, Govender K. Closing the treatment gap for depression co-morbid with HIV in South Africa: Voices of afflicted women. Health. 2013;5:557–566. [Google Scholar]
- 64.Campbell C, Skovdal M, Mupambireyi Z, Madanhire C, Nyamukapa C, et al. Building adherence-competent communities: Factors promoting children's adherence to anti-retroviral HIV/AIDS treatment in rural Zimbabwe. Health & Place. 2012;18:123–131. doi: 10.1016/j.healthplace.2011.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–615. [PMC free article] [PubMed] [Google Scholar]
- 66.Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. The Lancet. 2011;378:1502–1514. doi: 10.1016/S0140-6736(11)60754-X. [DOI] [PubMed] [Google Scholar]
- 67.Welfare MoHaC . Zimbabwe National Mental Health Policy. Harare; Zimbabwe: 2004. [Google Scholar]
- 68.Pitorak H, Duffy M, Sharer M. “There is no Health without Mental Health”: Mental Health and HIV Service Integration in Zimbabwe, Situational Analysis. Arlington, VA: 2012. [Google Scholar]
- 69.Wright S, Zalwango F, Seeley J, Mugisha J, Scholten F. Despondency Among HIV-Positive Older Men and Women in Uganda. J Cross Cult Gerontol. 2012:319–333. doi: 10.1007/s10823-012-9178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Burgoyne RW. Exploring direction of causation between social support and clinical outcome for HIV-positive adults in the context of highly active antiretroviral therapy. AIDS Care. 2005;17:111–124. doi: 10.1080/09540120412331305179. [DOI] [PubMed] [Google Scholar]
- 71.Simoni JM, Frick PA, Lockhart D, Liebovitz D. Mediators of social support and antiretroviral adherence among an indigent population in New York City. AIDS Patient Care STDS. 2002;16:431–439. doi: 10.1089/108729102760330272. [DOI] [PubMed] [Google Scholar]
- 72.Wouters E, van Loon F, van Rensburg D, Meulemans H. Community support and disclosure of HIV serostatus to family members by public-sector antiretroviral treatment patients in the Free State Province of South Africa. AIDS Patient Care STDS. 2009;23:357–364. doi: 10.1089/apc.2008.0201. [DOI] [PubMed] [Google Scholar]
- 73.Power R, Koopman C, Volk J, Israelski DM, Stone L, et al. Social support, substance use, and denial in relationship to antiretroviral treatment adherence among HIV-infected persons. AIDS Patient Care STDS. 2003;17:245–252. doi: 10.1089/108729103321655890. [DOI] [PubMed] [Google Scholar]


