Abstract
Purpose/Objectives
To evaluate the process of survivorship care plan (SCP) completion and to survey oncology staff and primary care physicians (PCPs) regarding challenges of implementing SCPs.
Design
Descriptive pilot study.
Setting
Two facilities in Vermont, an urban academic medical center and a rural community academic cancer center.
Sample
17 oncology clinical staff created SCPs, 39 PCPs completed surveys, and 58 patients (breast or colorectal cancer) participated in a telephone survey.
Methods
Using Journey Forward tools, SCPs were created and presented to patients. PCPs received the SCP with a survey assessing its usefulness and barriers to delivery. Oncology staff were interviewed to assess perceived challenges and benefits of SCPs. Qualitative and quantitative data were used to identify challenges to the development and implementation process as well as patient perceptions of the SCP visit.
Main Research Variables
SCP, healthcare provider perception of barriers to completion and implementation, and patient perception of SCP visit.
Findings
Oncology staff cited the time required to obtain information for SCPs as a challenge. Completing SCPs 3–6 months after treatment ended was optimal. All participants felt advanced practice professionals should complete and review SCPs with patients. The most common challenge for PCPs to implement SCP recommendations was insufficient knowledge of cancer survivor issues. Most patients found the care plan visit very useful, particularly within six months of diagnosis.
Conclusions
Creation time may be a barrier to widespread SCP implementation. Cancer survivors find SCPs useful, but PCPs feel insufficient knowledge of cancer survivor issues is a barrier to providing best follow-up care. Incorporating SCPs in electronic medical records may facilitate patient identification, appropriate staff scheduling, and timely SCP creation.
Implications for Nursing
Oncology nurse practitioners are well positioned to create and deliver SCPs, transitioning patients from oncology care to a PCP in a shared-care model of optimal wellness. Institution support for the time needed for SCP creation and review is imperative for sustaining this initiative.
Knowledge Translation
Accessing complete medical records is an obstacle for completing SCPs. A 3–6 month window to develop and deliver SCPs may be ideal. PCPs perceive insufficient knowledge of cancer survivor issues as a barrier to providing appropriate follow-up care.
As of January 2012, an estimated 13.7 million cancer survivors were living in the United States (Siegel et al., 2012). The five-year relative survival rate in the United States for all cancers has improved from 49% for cases diagnosed from 1975–1979 to 67% for cases diagnosed in 2004 (Howlader et al., 2011). The cancer survivor population is growing concurrently with a projected shortage of oncology physicians (Erikson, Salsberg, Forte, Bruinooge, & Goldstein, 2007). With total oncology visits projected to increase from 38 million in 2005 to 57 million in 2020, the United States is expected to face a 48% increase in demand for oncologist services by 2020 (Erikson et al., 2007). The rapidly increasing survivor population and predicted inevitable shortages of both oncology specialists and primary care physicians (PCPs) present a barrier to ensuring high-quality surveillance care for cancer survivors (Potosky et al., 2011).
Cancer survivors face several challenges, including late and long-term effects of therapy and uncertainty regarding follow-up care. The Institute of Medicine (IOM) recommended that patients with cancer and their PCP receive a written survivorship care plan (SCP) at the end of active treatment that communicates what occurred during cancer treatment. That document should include a comprehensive care summary and a plan specifically outlining the responsibility of each provider in follow-up care (Hewitt, Greenfield, & Stovall, 2005). Despite the recommendation by the IOM that an SCP is integral to achieving high-quality care, practical barriers exist to the creation of written documents (Earle, 2006). With oncology care often taking place in multiple outpatient and inpatient settings, compiling information can be arduous and time-consuming. Oncology providers may need to request multiple medical charts to document a single episode of care or a set of services required to manage a patient with cancer over time.
In urban areas, a patient with cancer may have surgery at one hospital, receive radiation therapy at another institution, undergo chemotherapy at a private oncologist’s office, and return to see their PCP closer to home (National Research Council, 2007). Although those challenges to creating SCPs are recognized, some argue that an SCP is not unlike a hospital discharge summary or operative note, both of which are considered standard of care (Hewitt et al., 2005). Some have suggested that oncologists are unaware of cancer survivors’ desires for information contained in the SCP (Harrington, Hansen, Moskowitz, Todd, & Feuerstein, 2010). Other reports indicate that the quality of cancer care is optimal when responsibility for care is shared by oncologists and PCPs (Salz, Oeffinger, McCabe, Layne, & Bach, 2012).
The goal of the current pilot study was to evaluate oncology staff perceptions of and perceived barriers and facilitators to developing and implementing SCPs. Obstacles to the use of an SCP by PCPs also were assessed. Patient perceptions regarding the care plan visit were obtained. These results can be used to modify the future design of care plans and the systems that provide them to facilitate ease of transition into clinical practice.
The shared-care model provided the conceptual framework for this study (Gilbert, Miller, Hollenbeck, Montie, & Wei, 2008) because it underscores coordination between healthcare providers who practice in different specialties or locations with consideration of patient involvement. Knowledge transfer, channels of communication, and patient input provide the underlying structure for the model, underscoring the reintegration of PCPs into survivorship care. The role of the advanced practice professional (APP) is enmeshed within the multidisciplinary oncology care team. In this pilot study, an APP is defined as a nurse practitioner or physician assistant.
Methods
Sample
The study was conducted at two sites: Fletcher Allen Health Care, an urban academic medical center in Burlington, VT, and Norris Cotton Cancer Center North, a rural academic medical center in St. Johnsbury, VT. Eligible participants were patients with stage 0–III breast cancer or stage II–IV colorectal cancer, aged 18 years and older, who had completed treatment with intent to cure up to 12 months before or during the study time period of November 2010 to April 2011. A total of 89 patients were invited to participate in the study and 78 agreed (88%), including 61 with breast cancer and 17 with colorectal cancer. Fifty-eight patients, including 48 with breast cancer and 10 with colorectal cancer, completed a telephone survey. The remaining 20 patients either refused to complete the telephone interview (n = 6) or could not be contacted (n = 14). Nonrespondents had similar patterns of cancer stage and treatment to those who completed the interview. Sixteen of 17 oncology staff members (94%), including oncologists, APPs, and nurses, completed a telephone interview at completion of the study. Fifty-five surveys were sent to PCPs, with 39 returned for a response rate of 71%. Patients provided written informed consent. Consent for PCPs and oncology staff was implied by their willingness to complete the survey or be interviewed. The study was approved by the institutional review boards for research with human subjects at both study sites and was Health Insurance Portability and Accountability Act (HIPAA) compliant.
The Survivorship Care Plan
The SCPs were prepared by APPs in consultation with oncologists at each study site using the Survivorship Care Plan Builder software tool developed by Journey Forward (Hausman, Ganz, Sellers, & Rosenquist, 2011), a joint program of Wellpoint, Inc., the University of California Los Angeles Jonsson Comprehensive Cancer Center, the National Coalition for Cancer Survivorship, and Genentech. Each care plan contained the following domains: (a) a summary of the patient diagnosis and treatment, (b) information on recommended follow-up care and secondary prevention, (c) information on late effects of cancer treatments received, and (d) a list of national and local health promotion resources. The care plans were modified, if necessary, with patient input and finalized. If late or long-term side effects were identified during the SCP visit, appropriate specialty referral was made. The SCP was delivered to and discussed with patients by the APPs during a one-hour care plan visit at the clinic.
Sources of Information
At both clinical sites, data for the Journey Forward care plan was obtained from the patient chart that included records from all treating practices. The treatment summary information was obtained from patient paper and electronic medical records and from the chemotherapy ordering system. Both sites had similar distribution of records across paper and electronic files. National resources were drawn from Hewitt et al. (2005), the Journey Forward resource document (http://journeyforward.org/patients/resource-patients), and the Centers for Disease Control and Prevention (CDC) resource links (www.cdc.gov/cancer/survivorship/links.htm). A local resource list was developed at each site.
Implementation
Prior to beginning data collection, meetings were held at both study sites with oncologists and clinic staff to review examples of SCPs and surveys. That was done to refine care plans and discuss the process of delivery and surveys. A Journey Forward packet was downloaded and given to each staff member (http://journeyforward.org/professionals/oncology-professionals). Prior to initiating data collection, the investigators met with the entire staff of the oncology clinic to present the study, discuss perceived challenges to implementation, and share ideas for improving the study. Journey Forward training was available to the APPs through the Journey Forward toolkit on the Web site (http://journeyforward.org/sites/journeyforward.org/files/oncologist-toolkit_1.pdf).
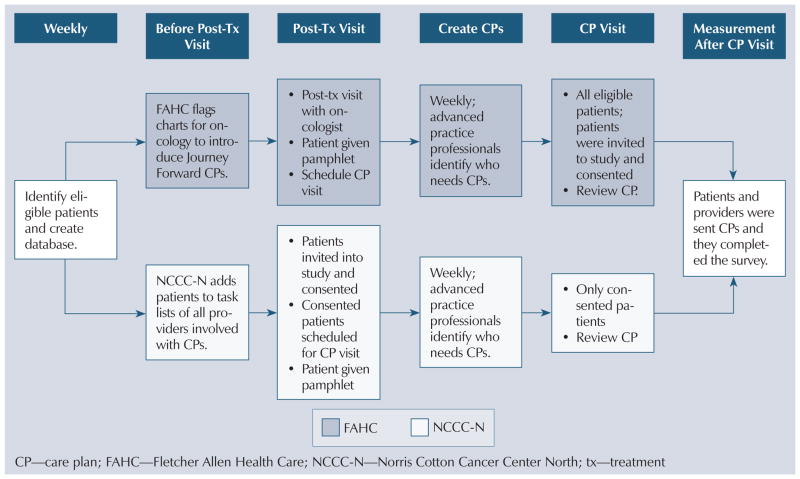
The mechanism for providing the SCPs was slightly different at each site to accommodate variations in practice at the respective institutions. At the time of the study, Fletcher Allen had established post-treatment survivor visits as standard of care and, therefore, all patients presenting for a first or second post-therapy visit were informed that their next follow-up visit would be an hour-long survivor visit in which they would receive an SCP. At the survivor visit, they were offered the opportunity to participate in a study to evaluate the SCP by the nurse practitioner or physician assistant. The patients received the SCP whether they did or did not consent to participation. At Norris Cotton Cancer Center North, where survivor visits were not standard of care at the time of the study, patients were approached at the end of initial oncologic therapy and offered participation in the study by the research nurse. If they consented, they were scheduled for an hour-long survivor visit 1–3 months later. The nurse practitioner presented and discussed the SCP with cancer survivors at that appointment. Several days prior to the visit, patients at both sites received a telephone call to remind them of the upcoming appointment. Figure 1 outlines the study schema at each site. A research assistant who was not involved in the clinics evaluated 10 randomly selected Journey Forward care plans for accuracy and completeness at each clinical site.
Figure 1.
Flow Diagram of Implementation Process at Both Clinical Sites
Clinical Staff Survey and Primary Care Provider and Patient Data
The APP responsible for developing the Journey Forward care plan and for the care plan visit kept a log that included the amount of time to create the SCP and any problems in retrieving the information, as well as the amount of time spent in the care plan visit. The oncology providers (e.g., oncologists, APPs), staff, and administrators completed a post-study implementation phone interview conducted by the principal investigator, who was not involved in the clinics, to evaluate perceived benefits and challenges of implementing the SCPs.
A survey was developed to evaluate PCP-perceived barriers to facilitating an SCP. Demographic information, including number of years in practice, was obtained. The survey also contained an open-ended question to elicit specific comments about the SCP. The SCP was mailed to the PCPs with a cover letter explaining the study, the consent form, and the survey with a self-addressed stamped return envelope. Two attempts to contact the PCP by mail were carried out. PCPs who did not return the survey within 4–8 weeks were contacted by an oncologist involved in the study either by e-mail or telephone at the urban site; an administrative staff member contacted PCPs at the rural site.
Telephone interviews were conducted with patients about two months after the care plan visit. As many as 15 attempts were made to contact participants, including calls at varying times including weekdays, week-nights, and weekends, as well as voice mails left with a toll-free number to return the call.
Statistical and Qualitative Analyses
All statistical analyses were conducted using SAS, version 9, statistical software. Descriptive statistics were determined for survey responses and demographic variables. Tests for interaction by cancer site and facility type were conducted using Fisher’s exact tests. For certain questions pertaining to the care plan in general, the complete set of response frequencies is described. Likert scale response options for perceived barriers PCPs reported that may interfere with their ability to provide follow-up care for adult cancer survivors were used. Lack of time, insufficient knowledge of cancer survivor issues, inadequate recommendations from oncology staff, poor reimbursement for service, and limited access to cancer survivors were dichotomized as “very significant barrier” or ”moderate barrier” and “hardly a barrier” or “not a barrier.” The response “other,” with an option to write in perceived barriers, was a separate response option.
Results
The APPs who developed and delivered SCPs to patients provided data (three nurse practitioners and one physician assistant). All of the APPs were women and held a Master of Science degree; three had a Master of Science in Nursing. Two nurse practitioners also had AOCNP® certification.
The mean care plan preparation time was 53.9 minutes. The most frequently reported barrier to completion of SCPs by APPs was the time required to read through medical records, particularly for patients who received care in multiple settings. Obtaining prior or outside records, including chemotherapy records, also was reported as an obstacle to creating SCPs. Consensus did not exist among the APPs as to whether the diagnosis of a new primary cancer should trigger the creation of a new and distinct care plan. As a result, dual cancer diagnoses were cited as a barrier to ease of completion of the SCP.
The majority (83%, n = 10) of clinical staff (oncologists, APPs, and RNs) reported that the optimal time to complete the care plan visit was 3–6 months after definitive treatment. Most clinical staff felt that an SCP should be provided to all patients with cancer; one APP felt that the SCP should only be given to patients treated with curative intent. All medical oncologists, APPs, and RNs interviewed felt that the APP should be responsible for completing and reviewing the SCP with patients. Two medical oncologists and one APP responded that the SCP should be completed by the APP and felt that either the APP or the oncologist could review the SCP with the patient during an office visit. Although administrative and scheduling staff reported no problems in scheduling SCP visits, it was suggested by a medical oncologist that a notification in the electronic medical record flagging the need to schedule a date for the SCP at the end of adjuvant therapy would facilitate compliance. When asked about the process for updating SCPs for progression of disease or new primary, mixed responses were received. More than half of the clinicians (oncologist, APPs, RNs) thought the SCP should be updated at the time of diagnosed progression of disease.
Sixty-four percent of PCPs surveyed cited limited access to survivors as a barrier to providing follow-up survivorship care. Insufficient knowledge of cancer survivor issues was reported as an obstacle by 58% of PCPs, followed by inadequate recommendations from oncology, as reported by 49% of PCPs. Other challenges reported by PCPs included lack of established survivor care guidelines (47%) and lack of time (45%). Poor reimbursement for services was reported as a barrier by 18% of PCPs. No statistically significant differences were reported in barriers by practice site. Some variation existed by years in practice, with 79% of PCPs with 18 years or less in practice reporting insufficient knowledge as a barrier, whereas only 37% of those with more than 18 years in practice reporting it as such (p = 0.02 for interaction).
The median age of patient respondents was 54 years (range = 35–75) for patients with breast cancer and 59 years (range = 41–70) for patients with colorectal cancer. The mean duration of the care plan visit was 59.7 minutes. All patients surveyed (N = 58) replied that the care plan visit provided adequate time. Only 30% of patients responded “yes” when asked if they knew what to expect during the care plan visit. The majority of patients (43%) stated they didn’t know what to expect, and 28% reported being “unsure” of what the appointment would entail. When asked what was different from what they anticipated, a variety of responses were given. More than half of patients replied that they simply did not know what to expect of the visit. Twelve percent reported that the appointment was more detailed than they expected; those respondents perceived this as positive. One patient replied that it would have been useful to have the SCP review prior to the visit; another did not expect to get a written packet of information specific to them. Despite not having expectations of the care plan appointment, the majority of respondents reported finding the care plan visit useful, with 83% of patents stating that the visit was “very useful” and 15% reporting the visit to be “somewhat useful.”
In response to the question, “During the visit, how much did [name of the APP] check to make sure you understood everything,” the majority of patients replied “all the time” (40%), “very much” (22%), or “quite a bit” (31%). When asked “Was the care plan given to you at a time for you to best use the information provided or would a different time have been better,” the responses were equally divided, with 48% of patients agreeing that the SCP was given to them at an optimal time and 50% responding that another time would have been better; 2% of participants did not respond to this question. Among patients who had their SCP visit within six months of diagnosis, 64% agreed that the care plan was given to them at the right time. For patients seen at 7–12 months after diagnosis, 55% agreed. Only 29% of patients having an SCP visit more than 12 months after cancer diagnosis replied that the timing of the appointment was favorable. Of those who didn’t agree (replied “no”) that the SCP visit was optimally scheduled, the most frequent response as to a better time was “before treatment ends” (31%).
Discussion
Data from the APPs in this pilot study indicate that accessing complete medical records, including information regarding prior oncology treatment received at different facilities, is an obstacle to completing SCPs. Initiating a summary report at the start of treatment and updating the SCP with changes, such as late effects, progression of disease, or recurrence, in real time may streamline completion of the SCP and decrease the burden of time needed to complete the entire document at the end of treatment. Standardized templates within electronic medical records should be designed to automatically populate the SCP with pertinent clinical data in real time during treatment. That would reduce the provider time needed to complete the SCP at the end of treatment. Additional research is needed to standardize the approach to development of SCPs in patients with more than one cancer diagnosis to determine if multiple SCPs are necessary.
According to data from this study, oncology providers felt that 3–6 months after completion of definitive treatment is the optimal time for patients to receive the SCP. The timing was best for those patients surveyed who received the SCP during a care plan visit within six months after diagnosis. Additional research is needed to establish a time frame for developing and delivering SCPs that is feasible for providers and most valuable to survivors, but this study suggests that the 3–6 month window may be a promising starting point.
The findings of the study reinforce those of Potosky et al. (2011), who found that PCPs perceive insufficient knowledge of cancer survivor issues as a barrier to providing appropriate follow-up care. Providing details within the SCP regarding late and long-term effects and standard monitoring tests may enhance the usefulness of SCPs. Increased communication between oncologists, survivors, and other healthcare providers through an SCP not only regarding what has been done, but also what needs to be done in the future, may help to more clearly delineate and facilitate the role of PCPs in survivorship care.
Although working with electronic medical record vendors may facilitate implementation, more research is necessary to examine whether creating an SCP can be efficient. Electronic medical records may facilitate identification of patients and aid in the creation of care plans and appropriate scheduling of patients by support staff when patients are cared for within a single system. For patients who receive care in multiple settings without shared information systems, obtaining information integral to the SCP remains a challenge. Although reimbursement was not reported as a major obstacle to completion or delivery of an SCP in this study, linking receipts of SCPs to reimbursement also may increase their use.
Limitations
The study’s findings have several limitations. The small sample size may impact the generalizability. Because this was a one-year pilot study with limited funding, the authors were only able to measure very short-term outcomes. Despite including rural and urban settings, the study was conducted in a geographically localized area in Vermont. The size of the study and lack of racial and ethnic diversity also limit the generalizability of the results.
Implications for Nursing
Nurse practitioners in oncology settings are well positioned to create and deliver SCPs, transitioning patients from their oncology care provider to their community PCP in a shared-care model of achieving optimal wellness. Institutional support for the time needed to prepare the SCP and review the document with patients is imperative for sustaining such an initiative.
Advocacy organizations have promoted the concept of SCPs; however, oncology nurses providing education to increase patient knowledge and understanding of an SCP may be a strong motivator for establishing SCPs as standard of care. Nursing informatics specialists working with electronic medical records vendors have an opportunity to create an infrastructure that eases development and implementation.
Conclusions
Treatment communication and coordination may be facilitated with SCP for survivors, but more research is needed to examine exactly how the SCP can serve to improve coordination of care between PCPs and oncologists and to further establish the unique role of nurse practitioners in survivorship care. Additional study also is needed to determine the optimal method for the clinical delivery of SCPs and to validate their importance.
Acknowledgments
The authors gratefully acknowledge Jennifer Hausman, MPH, and others at Journey Forward for their assistance in using the Survivorship Care Plan Builder, and Kathleen Howe, Penelope Gibson, PA, Janet Ely, APRN, Elizabeth McGrath, APRN, Jane Hatch, Lori Grimes, Amy Stansfield, RN, MBA, Marie Miller, RN, Amy Nolan, Anne Dorwaldt, MA, Greg Dana, MPA, Dawn Pelkey, and Rachel Chicoine for their assistance in the creation of the survivorship care plans, participant recruitment, data collection, and study support.
This research was supported, in part, through the Centers for Disease Control and Prevention (No. 5U48DP001935-02; SIP 10-029).
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Preliminary results from this study were presented during at the Sixth Biennial Cancer Survivorship Research Conference, “Cancer Survivorship Research: Translating Science to Care,” in Arlington, VA, from June 14–16, 2012.
References
- Earle CC. Failing to plan is planning to fail: Improving the quality of care with survivorship care plans. Journal of Clinical Oncology. 2006;24:5112–5116. doi: 10.1200/JCO.2006.06.5284. [DOI] [PubMed] [Google Scholar]
- Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M. Future supply and demand for oncologists: Challenges to assuring access to oncology services. Journal of Oncology Practice. 2007;3(2):79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert SM, Miller DC, Hollenbeck BK, Montie JE, Wei JT. Cancer survivorship: Challenges and changing paradigms. Journal of Urology. 2008;179:431–438. doi: 10.1016/j.juro.2007.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington CB, Hansen JA, Moskowitz M, Todd BL, Feuerstein M. It’s not over when it’s over: Long-term symptoms in cancer survivors—A systematic review. International Journal of Psychiatry in Medicine. 2010;40:163–181. doi: 10.2190/PM.40.2.c. [DOI] [PubMed] [Google Scholar]
- Hausman J, Ganz PA, Sellers TP, Rosenquist J. Journey forward: The new face of cancer survivorship care. American Journal of Managed Care. 2011;17(5 Suppl):e187–e193. [PubMed] [Google Scholar]
- Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: Lost in transition. Washington, DC: National Academies Press; 2005. [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Cronin KA, editors. SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations) 2011 Retrieved from http://seer.cancer.gov/csr/1975_2009_pops09/
- National Research Council. Implementing cancer survivorship care planning. Washington, DC: National Academies Press; 2007. [Google Scholar]
- Potosky AL, Han PK, Rowland J, Klabunde CN, Smith T, Aziz N, Stefanek M. Differences between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. Journal of General Internal Medicine. 2011;26:1403–1410. doi: 10.1007/s11606-011-1808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salz T, Oeffinger KC, McCabe MS, Layne TM, Bach PB. Survivorship care plans in research and practice. CA: A Cancer Journal for Clinicians. 2012;62:101–117. doi: 10.3322/caac.20142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Ward E. Cancer treatment and survivorship statistics, 2012. CA: A Cancer Journal for Clinicians. 2012;62:220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]