Abstract
Purpose:
To correlate the structural and functional changes following intravitreal injection of dexamethasone 0.7 mg (Ozurdex®) implant in patients with recalcitrant uveitic cystoid macular edema (CME).
Materials and Methods:
In a prospective, interventional, nonrandomized study, 30 eyes (27 patients) with uveitic CME received Ozurdex® implant and were followed-up for 24 weeks at periodic intervals to monitor structural alterations seen on spectral domain optical coherence tomography (SD-OCT). The outcome measures included change in central macular thickness (CMT) and best-corrected visual acuity (BCVA) as well as structural alterations seen on OCT such as change in the height of cystoid spaces (CSs) and sub-foveal serous retinal detachment (SSRD). The integrity of external limiting membrane and inner-outer segment junction was assessed at baseline and follow-up visits.
Results:
Mean age of the patients was 46.09 ± 15.66 years. The mean CMT decreased by 96 μm at 1-day, 231.64 μm at 1-week, 254.21 μm at 4 weeks and 249.14 μm at 12 weeks (P < 0.001) compared with baseline. BCVA improved from a baseline mean of 0.62 LogMAR units to 0.49 on day 1 to 0.31 at 24 weeks (P < 0.001). A decrease in the mean height of CS, that is, 133.28 μm from a baseline of 317.71 μm was noted on the 1st day (P < 0.001). 4 eyes demonstrated the presence of CS at 4 weeks, 1 eye at 6 weeks and 3 eyes at 12 weeks. At baseline, 16 eyes (53.33%) demonstrated the presence of SSRD. Among these, 11 eyes showed resolution of SSRD on day 1. SSRD resolved in all patients at 4 weeks and was maintained up to 24 weeks.
Conclusions:
Ozurdex® implant improves the visual outcome of patients with recalcitrant uveitic CME. Reversibility of retinal changes may be possible following treatment with dexamethasone implant. Thus final visual outcome may be independent of pretreatment CMT, the height of CS or SSRD.
Keywords: Cystoid macular edema, dexamethasone implant, external limiting membrane, optical coherence tomography, Ozurdex, serous retinal detachment, uveitis
Cystoid macular edema (CME) and its sequelae are important causes of compromised vision in patients diagnosed with uveitis.[1] Imaging analysis and assessment of macular thickness using spectral domain optical coherence tomography (SD-OCT) has brought about a paradigm shift in the management of CME associated with various retinal pathologies, including uveitis and other macular diseases.[2,3,4,5,6,7,8,9] SD-OCT has also been used to study the effect of the integrity of the external limiting membrane (ELM) and photoreceptor inner and outer segment junctions (IS-OS) on the final visual acuity. Available data from studies suggests that disruption of these layers is associated with poor visual outcome in patients with retinal vein occlusions,[10,11,12,13] diabetic macular edema,[14,15] epiretinal membranes (ERM),[16,17,18] retinitis pigmentosa[19,20] and age-related macular degeneration.[21,22]
The HURON study group has shown promising results with long-acting intravitreal dexamethasone implant, Ozurdex® in patients with noninfectious intermediate or posterior uveitis to improve the visual acuity.[23] However, there is a lack of information available in the literature regarding the structural alterations following injection of dexamethasone implant in patients with recalcitrant uveitic CME. There is a need to identify the prognostic anatomic factors that may influence the final visual outcome in this patient population if any.
In the index study, we prospectively enrolled patients who were treated with intravitreal injection of dexamethasone implant to treat the uveitic CME. These patients were followed up closely to study various OCT parameters and reversibility of pathological changes in retinal layers that may influence the final visual outcome.
Materials and Methods
A prospective, interventional and nonrandomized study was conducted at the Retina and Uveitis Clinic of a Tertiary Care Referral Institute in North India. The Institutional Ethics Committee Approval was obtained for the use of dexamethasone implant and written informed consent was taken from all patients enrolled. The study adhered to the tenets of the declaration of Helsinki. Thirty eyes of 27 patients were included in the study.
Patients diagnosed with recalcitrant CME secondary to noninfectious intermediate or posterior uveitis were included in the study. CME was considered refractory in cases of no response to systemic treatment with steroids or immunosuppressants and/or intravitreal anti-vascular endothelial growth factor (anti-VEGF) therapy for ≥3 months. CME was defined as the presence of central macular thickness (CMT) of ≥275 μm on SD-OCT or presence of any intra or subretinal fluid. Patients with ERM, vitreomacular traction, choroidal neovascularization and macular chorioretinal lesions were excluded from the study. A detailed history of duration of CME and previous treatments in the form of oral, topical or intravitreal steroids and immunosuppression was noted. Patients with glaucoma, poor media clarity, cataract or conditions that may exacerbate CME, such as concomitant diabetes, vascular occlusions and ocular diseases limiting visual potential such as macular degeneration/scars, macular hole or optic atrophy too were excluded.
Pretreatment and follow-up assessment of best-corrected visual acuity (BCVA) was done using Snellen's visual acuity chart (by a single masked examiner) and measured in LogMAR scale, intraocular pressure (IOP) by Goldmann applanation tonometry, fundus photography and fundus fluorescein angiography (FFA) (Carl Zeiss FF 450 plus IR, Zeiss Meditech, Dublin, CA, USA). OCT was performed in all eyes using Cirrus OCT, Carl Zeiss, Dublin, CA, USA using HD 5 raster and Macular cube 512 μm × 128 μm scan protocol. All the parameters except FFA were recorded at baseline i.e., 1-day prior to injection and repeated at day, 1, 4, 6, 12 and 24 weeks after the implant injection. FFA was done at baseline, 12 weeks and 24 weeks to assess macular leakage and activity of the disease.
Central macular thickness was defined as the average thickness of the central 1 mm scanned retina on the Early Treatment Diabetic Retinopathy Study Circle (ETDRS). ELM and IS-OS junction were identified on HD 5 line raster scan protocol (horizontal and vertical) of the OCT up to 500 μm from the fovea in all directions. Disruption of the ELM and IS-OS was identified as loss of the high reflectivity layer. However, reduced reflectivity of these layers in the presence of large cystoid spaces (CSs) due to back shadowing was not considered as disruption. CS was defined as circular or oval intraretinal hypo-reflective spaces present within 500 μm from the foveal center. Sub-foveal serous retinal detachment (SSRD) was defined as fluid separating the neurosensory retina from the retinal pigment epithelium (RPE), which was visible on OCT as an optically clear space between the retina and RPE. Height of the maximum CS at or within 500 μm of the fovea was measured in the vertical meridian by drawing a line perpendicular from the roof of the CS to its floor using the Cirrus OCT software. Similarly, height of SSRD was manually measured by drawing a vertical line from outer photoreceptor layer up to the RPE (by two independent masked investigators: AA and PB). The OCT analysis is further illustrated in Fig. 1.
Figure 1.
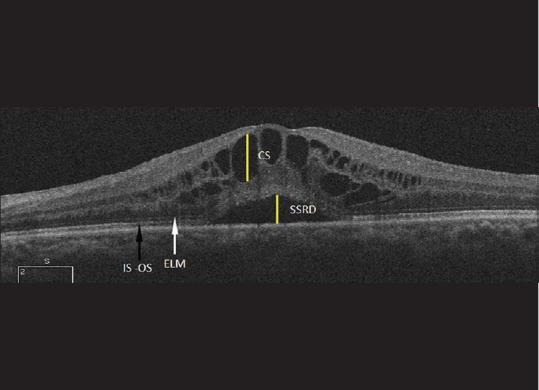
Optical coherence tomography scan in grayscale of a patient depicts the technique used to measure various parameters on raster scan. The cystoid space height and height of serous retinal detachment was manually measured using calipers on the Cirrus software as shown by the yellow lines, at or within 500 µm from the foveal center. The white arrow denotes the intact external limiting membrane seen preoperatively. Black arrow denotes the intact inner segment-outer segment junction
The outcomes of the study included the change in the BCVA by LogMAR visual acuity scale, CMT as measured by the OCT, structural parameters including change in height of CS, SSRD and integrity of ELM and IS-OS.
The measurable data were analyzed by an examiner (masked to the BCVA status while interpreting OCT) for its normality by the Kolmogrov–Smirnov test. Nonparametric tests were used to assess the measurable outcome variables. The mean change in the BCVA and CMT at the baseline and follow-up visits was analyzed by the Wilcoxon signed-rank test. Inter-group comparison was performed using Mann–Whitney U-test. Inter-observer correlation was measured using Spearman correlation coefficient. All the tests were 2-sided tests with the level of significance at 5% level. Statistical analysis was performed using Graph Pad Prism 5 (Graph Pad Software Inc., CA, USA).
Results
This study included 30 eyes of 27 patients diagnosed with uveitic CME (12 males and 15 females). Mean age of the patients was 46.09 ± 15.66 years. The baseline mean pretreatment visual acuity, as measured in LogMAR scale, was 0.62 ± 0.23. The preinjection mean IOP was 12.73 ± 1.85 mm Hg. Demographic profile, clinical details and treatment history of the patients is described in Table 1. All the patients completed the visits up to week 24. However, 3 eyes of 3 patients (10%) required re-treatment at week 12 due to recurrence of CME on SD-OCT and macular leakage on FFA and were excluded from further analysis.
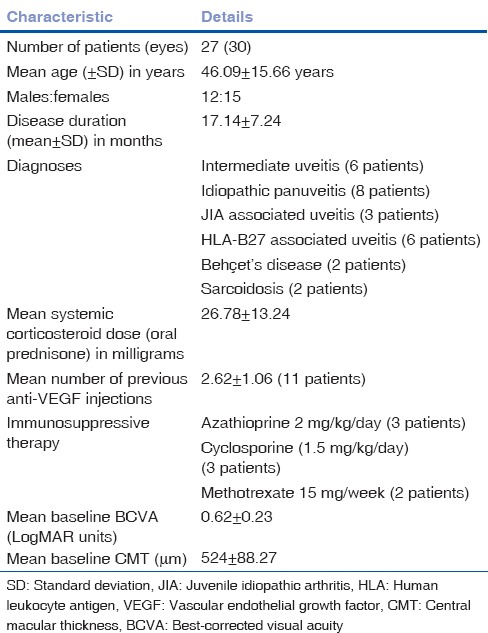
Table 1.
Demographic, clinical and treatment details of the patients included in the study
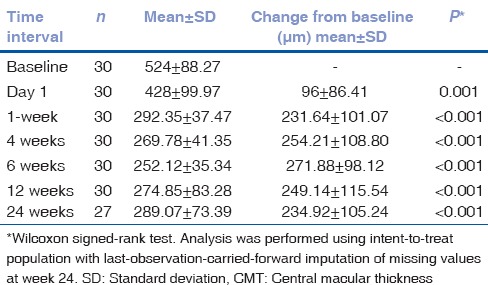
Improvement in visual acuity, as documented by LogMAR scale, is summarized in Fig. 2a. The mean LogMAR visual acuity values were significantly better at all-time points during the follow-up visits up to week 24. The BCVA was 0.49 ± 0.19 on the 1st day, 0.40 ± 0.22 at 1-week, 0.35 ± 0.24 at 4 weeks, 0.23 ± 0.17 at 6 weeks, 0.3 ± 0.23 at 12 weeks and 0.33 ± 0.31 at 24 weeks postoperatively [Table 2]. Analysis of SD-OCT scans revealed a baseline preinjection mean CMT of 524 ± 88.27 μm. The mean CMT values were 428 ± 99.97 at first postoperative day, 292.35 ± 37.47 at 1-week, 269.78 ± 41.35 at 4 weeks, 252.12 ± 35.34 at 6 weeks, 274.86 ± 83.28 at 12 weeks and 289.07 ± 73.39 at 24 weeks postoperatively. The reduction of CMT was statistically significant at all postoperative visits up to week 24. The values of CMT during the follow-up period are illustrated in Fig. 2b. Magnitude of change in the values of CMT is provided in Table 3.
Figure 2.
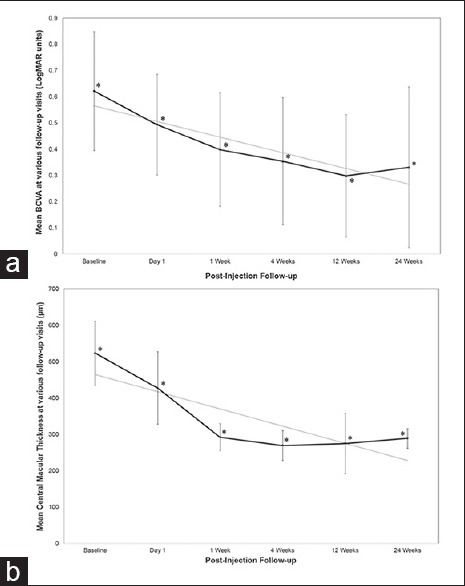
(a) Change in the mean best-corrected visual acuity in the total study population, (b) Change in the central macular thickness at various posttreatment visits. Vertical bars indicate standard deviation and asterisk indicates values that are significantly different compared to baseline (Wilcoxon signed-rank test). The dotted line represents the trend line over a period of 24 weeks. Intent-to-treat analysis was performed with imputation of last-observation-carried-forward for missing values at week 24
Table 2.
Change in the BCVA at various posttreatment visits
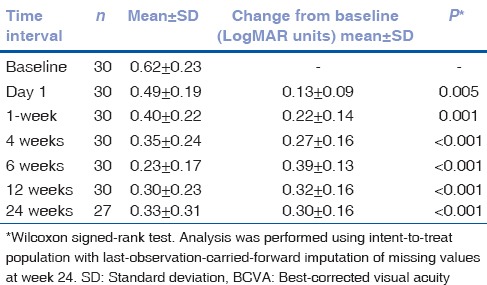
Table 3.
Change in the CMT at various posttreatment visits
The detailed analyses of the OCT scans including manual measurements were performed. There was a good correlation of the readings obtained from the two independent OCT analyzers by Spearman’ correlation coefficient (ρ = 0.91, P < 0.001). CSs were found in all eyes at baseline. Mean preoperative baseline CS was 317.71 (±131.58) μm. A mean decrease in CS, that is, 133.28 μm from a baseline of 317.71 μm was noted on the 1st day (P < 0.001), further decrease of 275 μm at 1-week (P < 0.001), decrease of 303.45 μm at 4 weeks (P < 0.001), 302.63 μm at 6 weeks (P < 0.001), decrease of 285.64 μm at 12 weeks (P < 0.001) and decrease of 290.94 μm at 24 weeks (P < 0.001) compared to the baseline visit. Four eyes (13.33%) demonstrated presence of CS at 4 weeks among which 3 eyes showed resolution at 6 weeks; 1 eye that showed presence of CS (3.33%) at 6 weeks showed resolution at 12 weeks. Three eyes (10%) showed presence of new cysts at 12 weeks (these eyes received retreatment at week 12) and 4 eyes at 24 weeks (out of the remaining 27 eyes; that is, 14.81%). At baseline, 16 eyes out of the 30 eyes (53.33%) demonstrated presence of SSRD. 11 eyes (68.75%) showed resolution of SSRD on the 1st day; the height of which decreased from baseline value of 60.43 (±76.96) μm to 29.57 μm. SSRD resolved in 13 out of 16 eyes (81.25%) at 1-week with a mean height of 4.93 μm in the remaining 3 eyes. SSRD resolved in all the patients at the 4 week visit and was maintained up to 24 weeks. These changes are summarized in Figs. 3 and 4. Eyes presenting with both CME and SSRD at baseline (n = 8) [Fig. 5] were compared to those presenting with CME alone [Fig. 6] (Mann–Whitney U-test). The mean preinjection BCVA was 0.70 ± 0.29 in eyes with SSRD compared to 0.57 ± 0.17 in eyes with CME alone (P = 0.4). However, at 12 weeks, the mean BCVA among eyes with CME alone at baseline (0.17 ± 0.07) was significantly better than those with SSRD and CME at baseline (0.46 ± 0.28) (P = 0.03). The final visual acuity at 24 weeks was significantly better in patients with CME alone (0.19 ± 0.10) compared to those presenting with CME and SSRD at baseline (0.5 ± 0.31) (P = 0.05).
Figure 3.
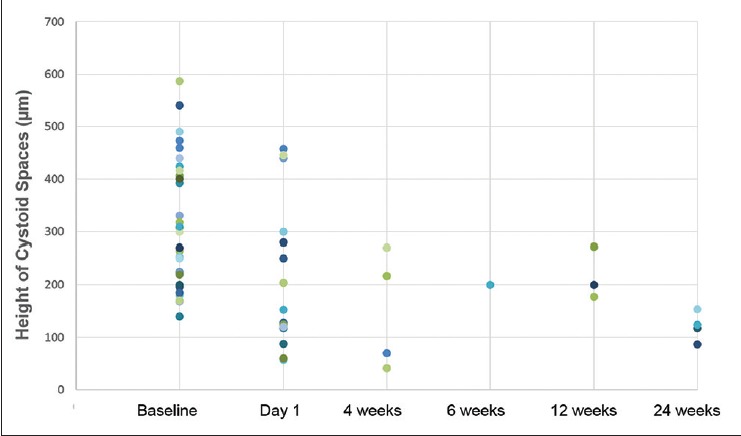
The decrease in the height of the cystoid spaces (CSs) at various follow-up visits in all eyes taken together. The colored dots represent individual eyes treated with intravitreal dexamethasone implant. At the baseline evaluation, CSs were present in all 30 eyes. Only 1 eye demonstrated CSs at 6 weeks, which resolved by 12 weeks. 3 eyes showing CSs at 12 weeks received retreatment. At the final visit (24 weeks), another 4 eyes demonstrated recurrence of CSs
Figure 4.
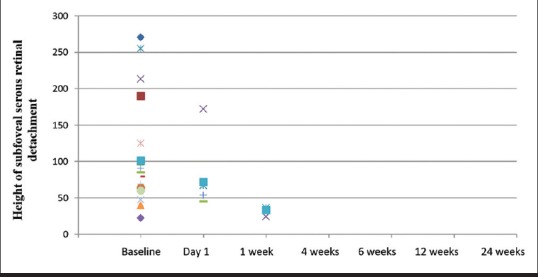
The decrease in the height of the sub-foveal serous retinal detachment at various visits in all eyes taken together. At the initial preinjection evaluation, 8 patients presented with serous retinal detachment. After injection Ozurdex, the serous detachment significantly decreased (P < 0.001) and resolved in all eyes by 4 weeks and was maintained up to 24 weeks
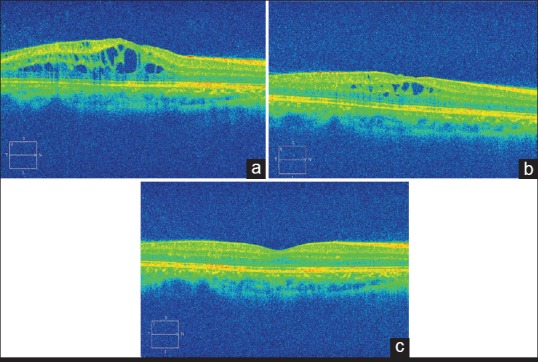
Figure 5.
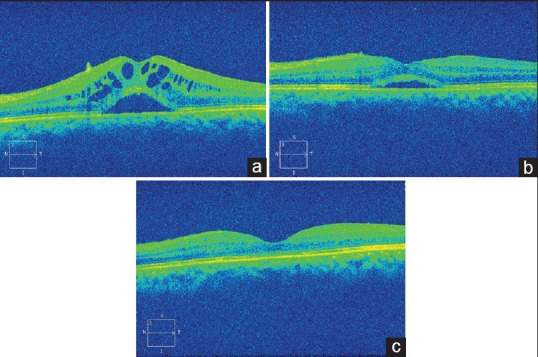
(Patient #1) (a) Optical coherence tomography (OCT) of a patient done at a preinjection visit demonstrates presence of large cystoid macular edema (CME) along with sub-foveal serous retinal detachment (SSRD), (b) On the 1st day after injection Ozurdex, the OCT scan shows marked resolution of the cysts and decrease in height of the subfoveal serous detachment, (c) At 12 weeks, there is complete resolution of the CME and SSRD, with return of visual acuity to 20/20
Figure 6.
(Patient #2) (a) Optical coherence tomography (OCT) of a patient performed preoperatively shows presence of large cystoid spaces (CS) in the fovea along with intact external limiting membrane and inner segment-outer segment junction, (b) OCT of the same patient performed 1 day after injection Ozurdex shows significant decrease in CS and central macular thickness, (c) Raster line scan shows resolution of cystoid macular edema and return of normal foveal contour with return of 20/20 visual acuity
The final visual acuities measured at 24 weeks did not correlate with the preoperative CMT on OCT (ρ = 0.02; P = 0.94). In addition, no correlation was found between the final visual acuity and the preoperative CS height (ρ = 0.17; P = 0.07) or the height of the SSRD (ρ = −0.23; P = 0.45). Presence of SSRD showed a fair correlation with poorer final visual acuity (ρ = −0.46; P = 0.09). Correlation values between the change in the visual acuity and the OCT parameters have been described in Table 4. There was a good correlation between the quantum of visual acuity change with a change in CMT and change in CS height over time.
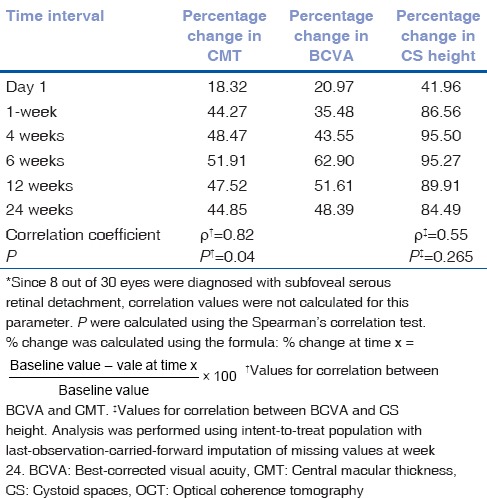
Table 4.
Correlation between the quantum of change in visual acuity and anatomic parameters on OCT compared to baseline values*
Baseline OCT scans done before injection demonstrated an intact ELM and IS-OS junction in 21 eyes (70%) while 4 eyes (13.33%) had a clear disruption of the ELM and IS-OS junction. The ELM and IS-OS junction could not be commented upon in 5 eyes due to reduced reflectivity because of the presence of large CSs. None of the 4 eyes that showed clear disruption of ELM and IS-OS junction at baseline have any significant gain in the visual acuity at the final follow-up visit compared to those with restored ELM and IS-OS junction as early at 1-week postoperative (P < 0.05).
Four eyes demonstrated a rise of IOP of more than 21 mm Hg after the implant injection at 1-week that was controlled with topical anti-glaucoma medications. None of the patients required glaucoma surgery during the 24 weeks of follow-up.
Discussion
Cystoid macular edema is responsible for visual morbidity in as many as 41% patients diagnosed with uveitis despite adequate control of intraocular inflammation.[24,25] It is the most common structural complication of uveitis. There are various treatment options available for treatment of CME in uveitis, including systemic or periocular corticosteroids, immunosuppressive agents, anti-VEGF injections and pars plana vitrectomy. However, there are yet, no guidelines available for treatment of macular edema associated with uveitis.[26] As many as 70% patients may be unresponsive to therapy despite maximum systemic therapy, including treatment with adalimumab or infliximab.[27,28] Thus, management of refractory CME remains a challenge in the present time.
The results of our study indicate that in addition to systemic therapy, treatment with intravitreal dexamethasone implant injection was able to achieve remission of CME in all patients by 12 weeks. Resolution of SSRD was seen at 4 weeks of therapy in all eyes which was maintained up to 24 weeks of follow-up [Fig. 5]. Recurrence of CME was seen in 3 eyes at 12 weeks requiring retreatment. During the follow-up visits, normalization and reversal of pathological retinal structural alterations caused by CS and SSRD correlated well with improvement in BCVA [Figs 5 and 6]. Thus, with repeated injections, it may be possible to maintain the anatomical integrity of the retinal layers at the time of recurrence. The current study provided only single injection treatment and thus, further studies with multiple dosing may enable assessment of the long-term benefit of dexamethasone implants in this patient population.
There have been a number of newer pharmacological agents that have been introduced for the management of uveitis.[29] Corticosteroids thus far, continue to remain the mainstay of therapy.[30] Dexamethasone implant has been used as an adjunct in the treatment of uveitis along with conventional anti-inflammatory therapy with reduction in disease activity and reduction in macular thickness.[31] The results of our study support these conclusions of the previous study. The effect of intravitreal dexamethasone on macular ultrastructural morphology and function in patients with central vein occlusions has also shown favorable results.[32] Thus, dexamethasone implant appears to be a promising novel adjunctive strategy to improve retinal structure and function in patients already on systemic therapy.
The results of our study support the hypothesis that the preservation of ELM and IS-OS junctions in eyes with CME may carry a better visual prognosis. This is in accordance with previous reports of macular edema seen in other macular pathologies including retinal vascular occlusions and diabetes.[10,11,12,13,14,15] All patients demonstrated an improvement in visual acuity significantly as compared to their preinjection values with no eye developing any worsening, including patients with disrupted outer retinal layers on OCT. This result is in accordance with conclusions of previous studies demonstrating the benefit of treatment of CME even in eyes with altered outer retinal layers.[33] The initial CMT did not correlate with the final visual acuity at 24 weeks suggesting that the final visual acuity was independent of the thickness of CME. However, in our study, the presence of SSRD along with CME was associated with the poorer visual outcome as compared to CME alone. This could be as a result of differences in the pathological processes resulting in SSRD as compared to CME.[34]
The dexamethasone implant had a quick onset of action with significant number of eyes (71.43%) showing response within 24 h of receiving the implant. All eyes in our study showed improvement in terms of visual acuity seen within 4 weeks of receiving the implant and were maintained at 12 weeks. Recurrence was observed in 3 eyes (10%) at week 12 and there was a trend toward worsening of BCVA and CMT at week 24 compared to week 12 [Fig. 2], but statistical significance could not be established.
Manual measurements were performed in the study to measure objectively structural retinal changes occurring as a result of CME. These measurements give us a good estimation in routine clinical practice in the management of such patients. A comprehensive study of the integrity of retinal layers without subjective errors is possible using SD-OCT.[8] There are few studies in the literature that demonstrate a correlation between microstructural alterations in retinal layers with the functional outcome in patients with uveitis.
The major limitation of our study is the relatively shorter period of follow-up. A longer follow-up of these patients is desirable to ensure longer stability of visual acuity and retinal structural alterations. Diverse characteristics of the patient population and small sample size are further limitations of the study. In addition, due to the shorter follow-up, the safety of dexamethasone implant could not be adequately assessed, as the development of cataract may require a longer period. In the absence of any alternative treatment arms, changes due to dexamethasone could not be compared to other agents such as intravitreal triamcinolone acetonide or biologic agents.
Conclusion
We report that Ozurdex implant has a promising role in the management of recalcitrant uveitic CME. Reversibility of retinal structural changes may occur following single injection of dexamethasone implant in patients who do not respond to systemic therapy alone. Evaluation of ELM and IS-OS junctions on OCT in patients with uveitic CME is important as it provides a clue to the possible visual recovery following treatment. The amount of retinal thickness, height of CSs and presence of serous retinal detachment do not affect the final visual outcome. Further studies with longer follow-up, multi-dosing strategy and comparative arms may be indicated to provide more information in the future.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Malinowski SM, Pulido JS, Folk JC. Long-term visual outcome and complications associated with pars planitis. Ophthalmology. 1993;100:818–24. doi: 10.1016/s0161-6420(93)31567-8. [DOI] [PubMed] [Google Scholar]
- 2.Hee MR, Puliafito CA, Duker JS, Reichel E, Coker JG, Wilkins JR, et al. Topography of diabetic macular edema with optical coherence tomography. Ophthalmology. 1998;105:360–70. doi: 10.1016/s0161-6420(98)93601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Otani T, Kishi S, Maruyama Y. Patterns of diabetic macular edema with optical coherence tomography. Am J Ophthalmol. 1999;127:688–93. doi: 10.1016/s0002-9394(99)00033-1. [DOI] [PubMed] [Google Scholar]
- 4.Hirakawa H, Iijima H, Gohdo T, Tsukahara S. Optical coherence tomography of cystoid macular edema associated with retinitis pigmentosa. Am J Ophthalmol. 1999;128:185–91. doi: 10.1016/s0002-9394(99)00100-2. [DOI] [PubMed] [Google Scholar]
- 5.Antcliff RJ, Stanford MR, Chauhan DS, Graham EM, Spalton DJ, Shilling JS, et al. Comparison between optical coherence tomography and fundus fluorescein angiography for the detection of cystoid macular edema in patients with uveitis. Ophthalmology. 2000;107:593–9. doi: 10.1016/s0161-6420(99)00087-1. [DOI] [PubMed] [Google Scholar]
- 6.Puliafito CA, Hee MR, Lin CP, Reichel E, Schuman JS, Duker JS, et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995;102:217–29. doi: 10.1016/s0161-6420(95)31032-9. [DOI] [PubMed] [Google Scholar]
- 7.Drexler W, Sattmann H, Hermann B, Ko TH, Stur M, Unterhuber A, et al. Enhanced visualization of macular pathology with the use of ultrahigh-resolution optical coherence tomography. Arch Ophthalmol. 2003;121:695–706. doi: 10.1001/archopht.121.5.695. [DOI] [PubMed] [Google Scholar]
- 8.Srinivasan VJ, Wojtkowski M, Witkin AJ, Duker JS, Ko TH, Carvalho M, et al. High-definition and 3-dimensional imaging of macular pathologies with high-speed ultrahigh-resolution optical coherence tomography. Ophthalmology. 2006;113:2054.e1–14. doi: 10.1016/j.ophtha.2006.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sakamoto A, Hangai M, Yoshimura N. Spectral-domain optical coherence tomography with multiple B-scan averaging for enhanced imaging of retinal diseases. Ophthalmology. 2008;115:1071–8.e7. doi: 10.1016/j.ophtha.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Coscas G, Coscas F, Zucchiatti I, Glacet-Bernard A, Soubrane G, Souïed E. SD-OCT pattern of retinal venous occlusion with cystoid macular edema treated with Ozurdex ®. Eur J Ophthalmol. 2011;21:631–6. doi: 10.5301/EJO.2011.7428. [DOI] [PubMed] [Google Scholar]
- 11.Shin HJ, Chung H, Kim HC. Association between integrity of foveal photoreceptor layer and visual outcome in retinal vein occlusion. Acta Ophthalmol. 2011;89:e35–40. doi: 10.1111/j.1755-3768.2010.02063.x. [DOI] [PubMed] [Google Scholar]
- 12.Ota M, Tsujikawa A, Murakami T, Yamaike N, Sakamoto A, Kotera Y, et al. Foveal photoreceptor layer in eyes with persistent cystoid macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2008;145:273–280. doi: 10.1016/j.ajo.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Ota M, Tsujikawa A, Kita M, Miyamoto K, Sakamoto A, Yamaike N, et al. Integrity of foveal photoreceptor layer in central retinal vein occlusion. Retina. 2008;28:1502–8. doi: 10.1097/IAE.0b013e3181840b3c. [DOI] [PubMed] [Google Scholar]
- 14.Otani T, Yamaguchi Y, Kishi S. Correlation between visual acuity and foveal microstructural changes in diabetic macular edema. Retina. 2010;30:774–80. doi: 10.1097/IAE.0b013e3181c2e0d6. [DOI] [PubMed] [Google Scholar]
- 15.Shin HJ, Lee SH, Chung H, Kim HC. Association between photoreceptor integrity and visual outcome in diabetic macular edema. Graefes Arch Clin Exp Ophthalmol. 2012;250:61–70. doi: 10.1007/s00417-011-1774-x. [DOI] [PubMed] [Google Scholar]
- 16.Oster SF, Mojana F, Brar M, Yuson RM, Cheng L, Freeman WR. Disruption of the photoreceptor inner segment/outer segment layer on spectral domain-optical coherence tomography is a predictor of poor visual acuity in patients with epiretinal membranes. Retina. 2010;30:713–8. doi: 10.1097/IAE.0b013e3181c596e3. [DOI] [PubMed] [Google Scholar]
- 17.Suh MH, Seo JM, Park KH, Yu HG. Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol. 2009;147:473–80.e3. doi: 10.1016/j.ajo.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 18.Mitamura Y, Hirano K, Baba T, Yamamoto S. Correlation of visual recovery with presence of photoreceptor inner/outer segment junction in optical coherence images after epiretinal membrane surgery. Br J Ophthalmol. 2009;93:171–5. doi: 10.1136/bjo.2008.146381. [DOI] [PubMed] [Google Scholar]
- 19.Aizawa S, Mitamura Y, Baba T, Hagiwara A, Ogata K, Yamamoto S. Correlation between visual function and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Eye (Lond) 2009;23:304–8. doi: 10.1038/sj.eye.6703076. [DOI] [PubMed] [Google Scholar]
- 20.Mitamura Y, Aizawa S, Baba T, Hagiwara A, Yamamoto S. Correlation between retinal sensitivity and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Br J Ophthalmol. 2009;93:126–7. doi: 10.1136/bjo.2008.141127. [DOI] [PubMed] [Google Scholar]
- 21.Sayanagi K, Sharma S, Kaiser PK. Photoreceptor status after antivascular endothelial growth factor therapy in exudative age-related macular degeneration. Br J Ophthalmol. 2009;93:622–6. doi: 10.1136/bjo.2008.151977. [DOI] [PubMed] [Google Scholar]
- 22.Hayashi H, Yamashiro K, Tsujikawa A, Ota M, Otani A, Yoshimura N. Association between foveal photoreceptor integrity and visual outcome in neovascular age-related macular degeneration. Am J Ophthalmol. 2009;148:83–9.e1. doi: 10.1016/j.ajo.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 23.Lowder C, Belfort R, Jr, Lightman S, Foster CS, Robinson MR, Schiffman RM, et al. Ozurdex HURON study group. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol. 2011;129:545–53. doi: 10.1001/archophthalmol.2010.339. [DOI] [PubMed] [Google Scholar]
- 24.Rothova A, Suttorp-van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol. 1996;80:332–6. doi: 10.1136/bjo.80.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaap-Fogler M, Amer R, Friling R, Priel E, Kramer M. Anti-TNF-α agents for refractory cystoid macular edema associated with noninfectious uveitis. Graefes Arch Clin Exp Ophthalmol. 2014;252:633–40. doi: 10.1007/s00417-013-2552-8. [DOI] [PubMed] [Google Scholar]
- 26.Tomkins-Netzer O, Talat L, Bar A, Lula A, Taylor SR, Joshi L, et al. Long-term clinical outcome and causes of vision loss in patients with uveitis. Ophthalmology. 2014;121:2387–92. doi: 10.1016/j.ophtha.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Díaz-Llopis M, Salom D, Garcia-de-Vicuña C, Cordero-Coma M, Ortega G, Ortego N, et al. Treatment of refractory uveitis with adalimumab: A prospective multicenter study of 131 patients. Ophthalmology. 2012;119:1575–81. doi: 10.1016/j.ophtha.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Markomichelakis NN, Theodossiadis PG, Pantelia E, Papaefthimiou S, Theodossiadis GP, Sfikakis PP. Infliximab for chronic cystoid macular edema associated with uveitis. Am J Ophthalmol. 2004;138:648–50. doi: 10.1016/j.ajo.2004.04.066. [DOI] [PubMed] [Google Scholar]
- 29.Barry RJ, Nguyen QD, Lee RW, Murray PI, Denniston AK. Pharmacotherapy for uveitis: Current management and emerging therapy. Clin Ophthalmol. 2014;8:1891–911. doi: 10.2147/OPTH.S47778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor SR, Isa H, Joshi L, Lightman S. New developments in corticosteroid therapy for uveitis. Ophthalmologica. 2010;224(Suppl 1):46–53. doi: 10.1159/000318021. [DOI] [PubMed] [Google Scholar]
- 31.Miserocchi E, Modorati G, Pastore MR, Bandello F. Dexamethasone intravitreal implant: An effective adjunctive treatment for recalcitrant noninfectious uveitis. Ophthalmologica. 2012;228:229–33. doi: 10.1159/000343060. [DOI] [PubMed] [Google Scholar]
- 32.Querques G, Lattanzio R, Querques L, Triolo G, Cascavilla ML, Cavallero E, et al. Impact of intravitreal dexamethasone implant (Ozurdex) on macular morphology and function. Retina. 2014;34:330–41. doi: 10.1097/IAE.0b013e31829f7495. [DOI] [PubMed] [Google Scholar]
- 33.Lardenoye CW, van Kooij B, Rothova A. Impact of macular edema on visual acuity in uveitis. Ophthalmology. 2006;113:1446–9. doi: 10.1016/j.ophtha.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 34.Munk MR, Kiss CG, Steiner I, Sulzbacher F, Roberts P, Kroh M, et al. Systematic correlation of morphologic alterations and retinal function in eyes with uveitis-associated cystoid macular oedema during development, resolution and relapse. Br J Ophthalmol. 2013;97:1289–96. doi: 10.1136/bjophthalmol-2012-303052. [DOI] [PubMed] [Google Scholar]


