Abstract
Purpose:
To measure the choroidal thickness (CT) after dynamic exercise by using enhanced depth imaging optical coherence tomography (EDI-OCT).
Materials and Methods:
A total of 19 healthy participants performed 10 min of low-impact, moderate-intensity exercise (i.e., riding a bicycle ergometer) and were examined with EDI-OCT. Each participant was scanned before exercise and afterward at 5 min and 15 min. CT measurement was taken at the fovea and 1000 μ away from the fovea in the nasal, temporal, superior, and inferior regions. Retinal thickness, intraocular pressure, ocular perfusion pressure (OPP), heart rate, and mean blood pressure (mBP) were also measured.
Results:
A significant increase occurred in OPP and mBP at 5 min and 15 min following exercise (P ˂ 0.05). The mean subfoveal CT at baseline was 344.00 ± 64.71 μm compared to 370.63 ± 66.87 μm at 5 min and 345.31 ± 63.58 μm at 15 min after exercise. CT measurements at all locations significantly increased at 5 min following exercise compared to the baseline (P ˂ 0.001), while measurements at 15 min following exercise did not significant differ compared to the baseline (P ˃ 0.05). There was no significant difference in retinal thickness at any location before and at 5 min and 15 min following exercise (P ˃ 0.05).
Conclusion:
Findings revealed that dynamic exercise causes a significant increase in CT for at least 5 min following exercise.
Keywords: Choroidal thickness, dynamic exercise, exercise, optical coherence tomography
The choroid's vasculature is the major supplier of oxygen and nutrients to the outer retina.[1] Abnormal choroidal blood volume or impairment of oxygen flow from the choroid to the retina, or both, may result in photoreceptor dysfunction and death.[2] Most ocular blood flow is accounted for by the choriocapillaris.[3] Choroidal blood flow, which has one of the highest rates of blood flow in the body, may also cool and warm the retina.[3]
Imaging the choroid with conventional commercial spectral-domain optical coherence tomography (SD-OCT) has proven difficult, due to weak signal transmission beyond the retinal pigment epithelium (RPE). However, the introduction of enhanced depth imaging (EDI)-OCT has provided a new means of assessing the choroid with commercially available SD-OCTs. EDI-OCT is a simple, noninvasive technique that provides in vivo evaluation of the choroid with high repeatability.[4] Choroidal thickness (CT) measurement may be influenced by many physiologic factors, including aging, refractive status, axial length, and several pathological diseases, including diabetic retinopathy, and central serous retinopathy.[5,6] Previous studies have also reported that measurements of CT have been decreased after caffeine intake and topical mydriatics.[7,8,9]
Physical exercise increases both systemic arterial blood pressure (BP) and blood flow, as well as decreases intraocular pressure (IOP).[10,11] Previous studies have reported that, due to the presence of autoregulative mechanisms, blood flow in retinal circulation remains constant during exercise.[12,13] However, since some controversy accompanies the presence of autoregulative mechanisms in choroidal circulation,[14,15] we considered that CT may be influenced by physical exercise. In light of growing interest in research of choroidal structures, in this study we aimed to evaluate the acute effect of dynamic exercise on CT, as measured by EDI-OCT in healthy patients.
Materials and Methods
This prospective, observational study was performed at the Department of Ophthalmology at Istanbul Kanuni Sultan Suleyman Education and Research Hospital. The study followed the tenets of the Declaration of Helsinki for human experimentation. All participants received oral and written information about the study, and each participant provided written, informed consent prior to participating. The study was performed on 19 eyes of 19 healthy male volunteers who ranged in age from 23 to 33 (mean 27 ± 4.08) years old. One eye, randomized for left or right, was measured in each volunteer. Since previous studies have indicated that CT and choroidal blood flow regulation may be altered in acute and chronic smokers, no regular cigarette smokers were included in the study.[16,17]
All of the participants underwent a comprehensive ophthalmologic examination that included a review of medical history, spherical equivalent of refractive error, corrected distance visual acuity, visual field testing if indicated, slit-lamp microscopy, IOP, and a dilated fundus examination. Volunteers with any concomitant history of any systemic abnormalities (e.g., vascular disease, hypertension, or diabetes mellitus), previous intraocular surgery or laser therapy, and high myopia or hyperopic were excluded.
Participants were asked to not consume alcoholic or caffeinated drinks for at least 12 h before having their measurements taken, as well as instructed to refrain from ingesting any food or liquids in the 30 min before the experiment. Prior to exercise, all baseline OCT scans and measurements for heart rate (HR), BP, and IOP were performed. Each participant then performed 10 min of low-impact, moderate-intensity exercise by riding a bicycle ergometer. To standardize the intensity of the exercise between participants, HR was monitored throughout the exercise task, and participants were instructed to cycle to an intensity that would keep their HR in a target range from 50% to 70% of the “HR reserve” above their baseline HR. Here, HR reserve was defined as the maximum HR minus the baseline HR,[18] the maximum HR defined as 208−(0.7 × age) and the baseline HR derived from pulse readings taken after 20 min of rest.[19] These measurements were repeated after completion of the exercise task at both 5 min and 15 min. All measurements were collected with participants seated. The order of measurements at each session was standardized: OCT scan, HR and BP, and lastly IOP measurement. OCT scans and both HR and BP measurements were taken at the same time.
Intraocular pressure was measured with the TonoPen XL (Mentor, USA) following the instillation of a drop of local anesthetic (0.4% oxybuprocaine hydrochloride). Three successive IOP measurements were taken and the average value recorded, as suggested by previous studies.[20,21] HR was automatically recorded from a finger pulse oximeter (HP-CMS patient monitor; Hewlett-Packard, Palo Alto, CA, USA). Systolic BP (sBP) and diastolic BP (dBP) were measured on the upper arm by using an automated oscillometric device. Mean BP (mBP) was calculated as dBP plus one-third the difference between sBP and dBP:
mBP = dBP + 1/3 (sBP − dBP)
Ocular perfusion pressure (OPP) was calculated by measuring the difference between two of three of the mBP and IOP values:[22,23]
OPP = 2/3 (mBP)−IOP
All participants were examined with the Cirrus HD-OCT 4000 (Carl Zeiss Meditec, Inc., Dublin, CA, USA). The scan pattern used on the Zeiss Cirrus, HD 5-line raster, is a line of 6 mm consisting of 4096 A-scans. These images were taken with the vitreoretinal interface adjacent to the zero delay and were not inverted to bring the choroid adjacent to zero delay, since image inversion using Cirrus software results in a low-quality image. The HD 5-line raster has 20 B-scans averaged together without tracking. The procedure for EDI-OCT measurements has been previously described.[4] CT was measured from the outer portion of the hyper reflective line corresponding to the RPE of the inner surface of the sclera. The horizontal and vertical sections running through the center of the fovea were selected for further analysis. Thus, the CT measurement was taken both at the fovea and 1000 μ away from the fovea in the nasal, temporal, superior, and inferior regions. Perpendicular lines were drawn from the posterior edge of the RPE to the choroid/sclera junction by using Cirrus HD-OCT software [Fig. 1]. These images were taken by an experienced technician and assessed by two masked experienced physicians. The estimates of CT from the two physicians correlated closely (r: 0.91) and we used the measurements of one of the physicians in the results section. All OCT measurements were taken in nondilated eyes because topical mydriatics have decreased the CT.[8]
Figure 1.
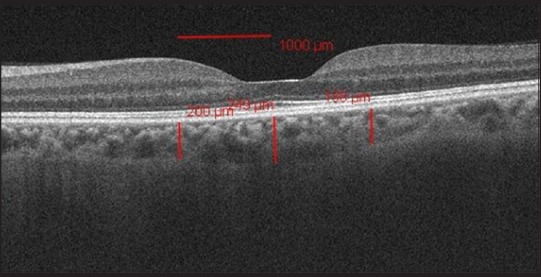
The choroidal thickness measurements at central fovea and 1000 μaway from the fovea in the nasal and temporal regions
All participants were examined by the macular cube 512 × 128 for the Cirrus protocol. All OCT were performed by the experienced technician. The macular cube 512 × 128 protocol performs 512 horizontal B-scan sections with 128 A-scans for each section over an area of 6 mm × 6 mm, which provides a thickness map with concentric sectors. The retina map image displays the retinal thickness in five locations in the perifoveal area.
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 16 (Chicago, IL). For each continuous variable, normality was checked by the Kolmogorov–Smirnov test. Comparisons of CT values between pre- and post-exercise (at 5 min and 15 min) were performed by a paired t-test. Pearson's correlation was used to examine the relationships among the measured variables, and interobserver Pearson's correlation was calculated for CT measurements. A P < 0.05 was considered significant.
Results
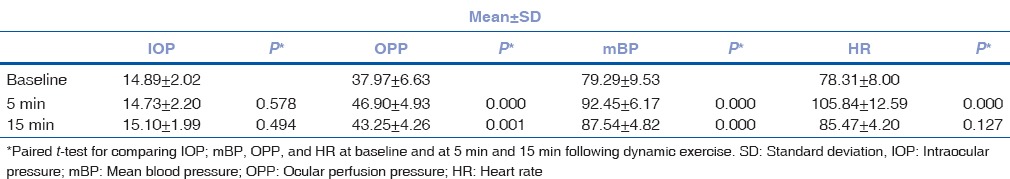
There was a significant increase in both OPP and mBP at 5 min and at 15 min following exercise (P ˂ 0.05) compared to the baseline measurement. There was no significant difference in IOP before or after the exercise at either 5 or 15 min (P ˃ 0.05) [Table 1].
Table 1.
Average and SD for the IOP, OPP, mBP, and HR measurements at baseline and at 5 min and 15 min following dynamic exercise
Choroidal thickness measurements at all locations at baseline and at 5 and 15 min after exercise are shown in Table 2, and retinal thickness measurements are presented in Table 3. CT measurements at all locations significantly increased at 5 min following exercise compared to the baseline measurement (P ˂ 0.001 for all locations), while measurements at 15 min following exercise were not significantly different compared to the baseline (P ˃ 0.05 for all locations) [Fig. 2]. The mean subfoveal CT (SFCT) at baseline was 344.00 ± 64.71 μm (range 243–435 μm) compared to 370.63 ± 66.87 μm (range 252–471 μm) at 5 min and 345.31 ± 63.58 μm (range 241–439 μm) at 15 min after exercise. There was no significant difference in retinal thickness at any location before or at 5 min or 15 min following exercise (P ˃ 0.05 for all locations) [Fig. 3].
Table 2.
Average and SD for the CT measurements at the different locations at baseline and at 5 min and 15 min following dynamic exercise
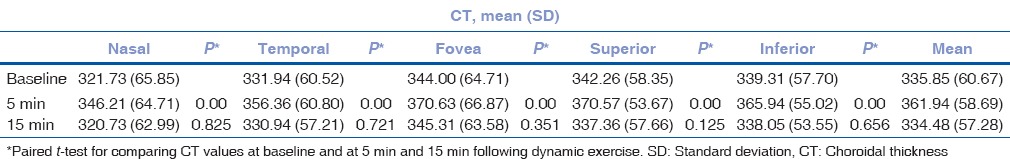
Table 3.
Average and SD for the retinal thickness measurements at the five locations at baseline and at 5 min and 15 min following dynamic exercise
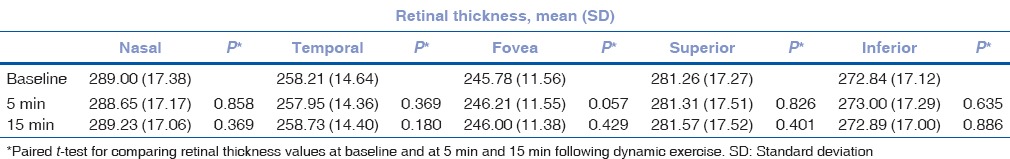
Figure 2.
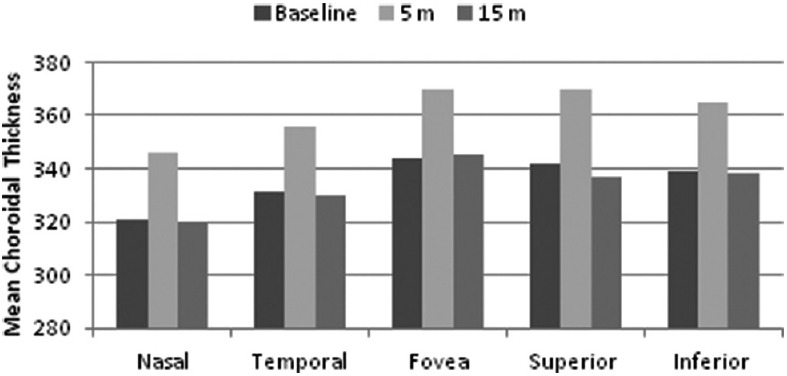
Graph showing the mean choroidal thickness at all locations before and at 5 min, and 15 min following exercise
Figure 3.
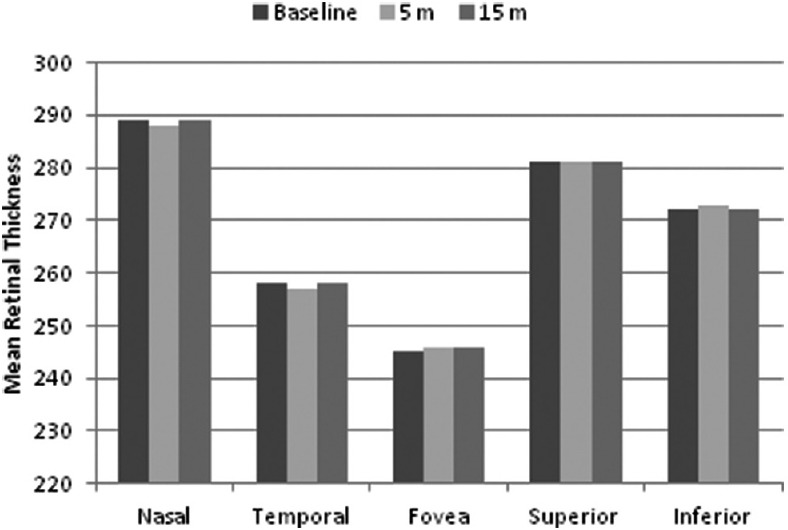
Graph showing the retinal thickness at all locations before and at 5 min, and 15 min following exercise
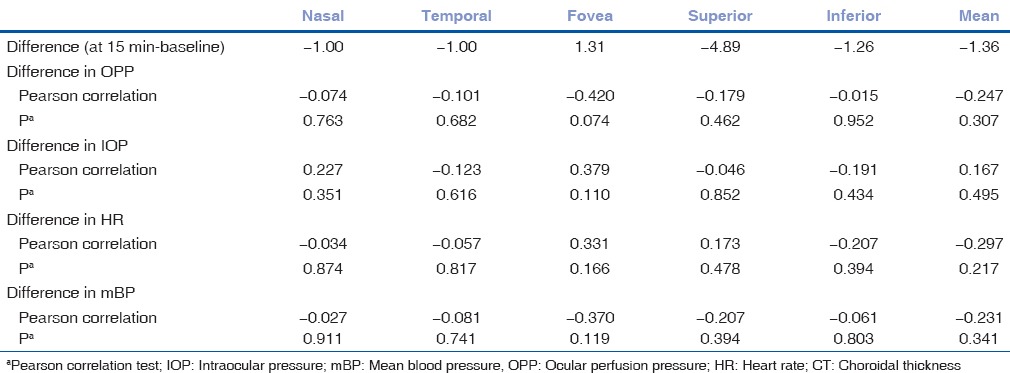
Tables 4 and 5 show the correlation analysis between changes in CT after exercise at 5 min and 15 min and changes in OPP, IOP, HR, and mBP measurements. No linear correlations among changes in OPP, IOP, HR, mBP, and CT following exercise emerged (P ˃ 0.05 for all).
Table 4.
Correlation analyses between changes in CT and other changes in clinical measurements at 5 min after dynamic exercise
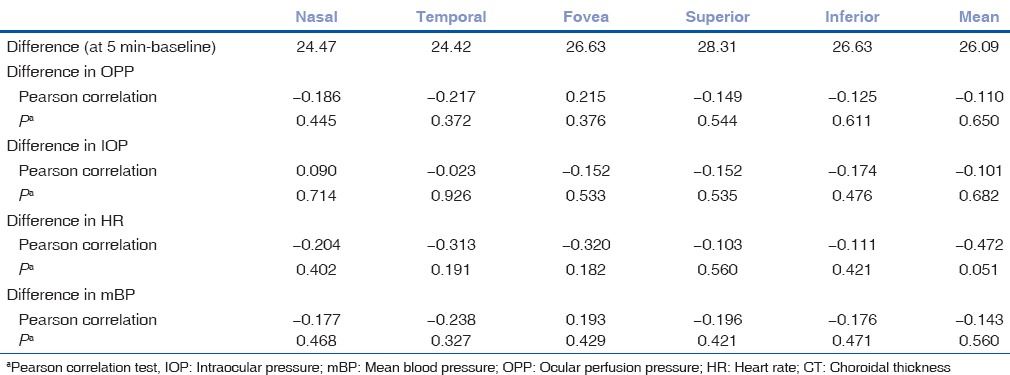
Table 5.
Correlation analyses between changes in CT and other changes in clinical measurements at 15 min after dynamic exercise
Discussion
This study investigated the acute effects of dynamic exercise on CT and found that CT values increased significantly at 5 min following dynamic exercise and returned to baseline values at 15 min following the exercise. At the same time, retinal thickness values did not significantly differ after the exercise.
Ocular blood flow comprises two systems: Retinal and choroidal circulations. In healthy patients, retinal blood flow is autoregulated during dynamic exercise by increased vascular resistance in proportion to the increase in OPP. As a result, there is only a minor increase in blood flow with increased OPP.[24] The choroid is similarly autoregulated but to a lesser degree, as is demonstrated by choroidal blood flow increases in the immediate postexercise period.[25]
Previous studies have reported that dynamic exercise can affect blood flow differently in retinal and choroidal circulations,[26,27] which would mean that the retinal system can supply stable amounts of blood to the central retinal artery both during exercise and rest, whereas the choroidal flow supplied by the ciliary arteries[28] increases with exercise intensity.
Okuno et al., observed increases in choroidal blood flow during dynamic exercise along with increases in OPP of ˂10% from the baseline.[25] Alwassia et al. measured CT before exercise and within 3 min after exercise using a portable SD-OCT device.[29] They also evaluated the relationship between sBP induced by exercise as well as choroidal and retinal thickness and reported that neither choroidal nor retinal thickness changed after dynamic exercise. Read and Collins observed a trend for a small increase in CT after exercise, but the changes in CT did not reach statistical significance.[30] Their theory was that these increase in CT were associated with reduction in axial length. Some clinical studies performed on patients with large IOP reduction following trabeculectomy, the change in IOP was shown to be negatively correlated with CT SFCT as measured by EDI-OCT.[31,32] On the other hand, Alwassia et al. and Hong et al., found that there was no significant difference in SFCT following isometric exercise.[29,33] In another study, diabetic patients with retinopathy had thinner choroids and showed a decrease in mean subfoveal choroidal blood flow, as measured by laser Doppler flowmetry.[34] Lovasik and Kergoat supported the findings of increased ocular blood flow, but concluded a transient but significant increase in pulsatile blood flow after exercise.[35]
A lot of mechanisms are responsible for keeping the CT from changing OPP or BP, but our study does not address the regulator mechanisms. Previous study showed that CT did not change despite the increase sBP[29] and they suggested that sympathetic innervation, and autoregulation of choroid were important for keeping the CT. On the other hand, previous studies have shown that there are no always correlation between OPP and CT. Maul et al.[36] showed that CT decreased in glaucoma patients with lower OPP, whereas the other studies found positive and negative correlation between changes in CT and changes in sBP.[37,38] Another study showed that there was no significant correlation between CT and BP.[29,39] Polska et al. reported that the choroidal regulatory capacity was influenced by the mode of OPP change, besides the change in OPP.[40]
In our study, after dynamic exercise choroidal thickening at 5 min might have been associated with an increase in OPP and mBP. Though the increase in OPP and mBP occured within 15 min, CT values returned to baseline value at 15 min. However, retinal thickness did not change after exercise. These findings may suggest that the autoregulatory mechanisms and retinal and choroidal blood flow are very complex. The interplay of a lot of systemic and local control mechanisms may be one of the major factors to affect the tone of the smooth muscles in the choroid influencing CT. However, we suggest that blood flow regulation within the retinal and choroidal circulation differs slightly. Plus, while choroidal circulation is characterized by high blood flow, the retinal circulation is characterized by low blood flow. The dense network of sympathetic innervations in the choroid suggests a mechanism of choroidal blood flow regulation.[41,42]
Although, CT is not a direct measure of choroidal blood flow, which, is mainly evaluated by laser doppler flowmetry,[43] we demonstrated the regulation of blood flow in choroidal and retinal circulation in vivo, as measured by thickness measurements that used EDI-OCT. Kim et al., revealed that CT may be indirectly indicative of choroidal perfusion status and changes in OPP may effect CT.[38] Measurements of CT with EDI-OCT technology provide only an indirect index of the consequence of blood flow regulation in a vascular bed, yet cannot measure blood flow, volume, or velocity there. We, therefore, suggest that EDI-OCT can be used to evaluate the issue of blood flow regulation.
The reproducibility of CT measurements using OCT is still debatable. However, some studies have found a high interobserver correlation, high repeatability, and high intersystem, interexaminer, and intervisit reproducibility in CT.[4,44,45] In our study, we found a high interobserver correlation in CT measurements, which is consistent with the results of previous studies.[4,44,45]
A limitation of the present study is that the manual measurement of CT is a principal drawback. Current OCT equipment does not provide software for the automated measurement of CT; therefore all identifications of the RPE and inner scleral border were conducted manually. It is our hope that software for segmenting the choroid automatically will be available in the near future.
We also did not measure axial length, thus there is always the possibility that axial length changes transiently during dynamic exercise and may cause apparent changes in CT. Read et al., found that dynamic exercise leads to decrease in axial length.[30] On the other hand, another study showed that there was no significant difference axial length, anterior chamber depth, and vitreous length before and after exercise measurement.[33] However, we endeavored to standardize the measurements after exercise, and all of the measurements, we made after exercise, took too long. The nonrandomized design and relatively small number of participants in this study represent additional weaknesses. In our study, we evaluated only male individuals because it might be a possible difference in performance between men and women and it has been shown that CT is affected by hormonal factors in women of reproductive age, so we have included only male to the study.[39,46]
Conclusion
This study investigated the CT response to dynamic exercise in 19 participants and showed that a short period of dynamic exercise leads to a significant increase in CT in healthy adults lasting for up to 15 min, whereas there was no significant change in retinal thickness. These findings demonstrate that, though CT increases after dynamic exercise, retinal thickness remains stable. This result should be considered when choroidal and retinal thickness is evaluated in chorioretinal disease or clinical research.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Alm A, Bill A. Ocular and optic nerve blood flow at normal and increased intraocular pressures in monkeys (Macaca irus): A study with radioactively labelled microspheres including flow determinations in brain and some other tissues. Exp Eye Res. 1973;15:15–29. doi: 10.1016/0014-4835(73)90185-1. [DOI] [PubMed] [Google Scholar]
- 2.Cao J, McLeod S, Merges CA, Lutty GA. Choriocapillaris degeneration and related pathologic changes in human diabetic eyes. Arch Ophthalmol. 1998;116:589–97. doi: 10.1001/archopht.116.5.589. [DOI] [PubMed] [Google Scholar]
- 3.Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res. 2010;29:144–68. doi: 10.1016/j.preteyeres.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146:496–500. doi: 10.1016/j.ajo.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 5.Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol. 2009;148:445–50. doi: 10.1016/j.ajo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 6.Kim SW, Oh J, Kwon SS, Yoo J, Huh K. Comparison of choroidal thickness among patients with healthy eyes, early age-related maculopathy, neovascular age-related macular degeneration, central serous chorioretinopathy, and polypoidal choroidal vasculopathy. Retina. 2011;31:1904–11. doi: 10.1097/IAE.0b013e31821801c5. [DOI] [PubMed] [Google Scholar]
- 7.Zengin MO, Cinar E, Karahan E, Tuncer I, Kucukerdonmez C. The effect of caffeine on choroidal thickness in young healthy subjects. Cutan Ocul Toxicol. 2014;27:1–5. doi: 10.3109/15569527.2014.912659. [DOI] [PubMed] [Google Scholar]
- 8.Kara N, Demircan A, Karatas G, Ozgurhan EB, Tatar G, Karakucuk Y, et al. Effects of two commonly used mydriatics on choroidal thickness: Direct and crossover effects. J Ocul Pharmacol Ther. 2014;30:366–70. doi: 10.1089/jop.2013.0093. [DOI] [PubMed] [Google Scholar]
- 9.Vural AD, Kara N, Sayin N, Pirhan D, Ersan HB. Choroidal thickness changes after a single administration of coffee in healthy subjects. Retina. 2014;34:1223–8. doi: 10.1097/IAE.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 10.Segal SS. Regulation of blood flow in the microcirculation. Microcirculation. 2005;12:33–45. doi: 10.1080/10739680590895028. [DOI] [PubMed] [Google Scholar]
- 11.Qureshi IA. Effects of exercise on intraocular pressure in physically fit subjects. Clin Exp Pharmacol Physiol. 1996;23:648–52. doi: 10.1111/j.1440-1681.1996.tb01751.x. [DOI] [PubMed] [Google Scholar]
- 12.Németh J, Knézy K, Tapasztó B, Kovács R, Harkányi Z. Different autoregulation response to dynamic exercise in ophthalmic and central retinal arteries: A color Doppler study in healthy subjects. Graefes Arch Clin Exp Ophthalmol. 2002;240:835–40. doi: 10.1007/s00417-002-0552-1. [DOI] [PubMed] [Google Scholar]
- 13.Iester M, Torre PG, Bricola G, Bagnis A, Calabria G. Retinal blood flow autoregulation after dynamic exercise in healthy young subjects. Ophthalmologica. 2007;221:180–5. doi: 10.1159/000099298. [DOI] [PubMed] [Google Scholar]
- 14.Delaey C, Van De Voorde J. Regulatory mechanisms in the retinal and choroidal circulation. Ophthalmic Res. 2000;32:249–56. doi: 10.1159/000055622. [DOI] [PubMed] [Google Scholar]
- 15.Harris A, Arend O, Bohnke K, Kroepfl E, Danis R, Martin B. Retinal blood flow during dynamic exercise. Graefes Arch Clin Exp Ophthalmol. 1996;234:440–4. doi: 10.1007/BF02539410. [DOI] [PubMed] [Google Scholar]
- 16.Wimpissinger B, Resch H, Berisha F, Weigert G, Polak K, Schmetterer L. Effects of isometric exercise on subfoveal choroidal blood flow in smokers and nonsmokers. Invest Ophthalmol Vis Sci. 2003;44:4859–63. doi: 10.1167/iovs.03-0391. [DOI] [PubMed] [Google Scholar]
- 17.Sizmaz S, Küçükerdönmez C, Pinarci EY, Karalezli A, Canan H, Yilmaz G. The effect of smoking on choroidal thickness measured by optical coherence tomography. Br J Ophthalmol. 2013;97:601–4. doi: 10.1136/bjophthalmol-2012-302393. [DOI] [PubMed] [Google Scholar]
- 18.Fletcher GF. How to implement physical activity in primary and secondary prevention. A statement for healthcare-professionals from the task force on risk-reduction, American Heart Association. Circulation. 1997;96:355–7. doi: 10.1161/01.cir.96.1.355. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37:153–6. doi: 10.1016/s0735-1097(00)01054-8. [DOI] [PubMed] [Google Scholar]
- 20.Deuter CM, Schlote T, Hahn GA, Bende T, Derse M. Measurement of intraocular pressure using the Tono-Pen in comparison with Goldmann applanation tonometry - A clinical study in 100 eyes. Klin Monbl Augenheilkd. 2002;219:138–42. doi: 10.1055/s-2002-26718. [DOI] [PubMed] [Google Scholar]
- 21.Horowitz GS, Byles J, Lee J, D’Este C. Comparison of the Tono-Pen and Goldmann tonometer for measuring intraocular pressure in patients with glaucoma. Clin Experiment Ophthalmol. 2004;32:584–9. doi: 10.1111/j.1442-9071.2004.00907.x. [DOI] [PubMed] [Google Scholar]
- 22.Barbosa CP, Stefanini FR, Penha F, Góes MÂ, Draibe SA, Canziani ME, et al. Intraocular pressure and ocular perfusion during hemodialysis. Arq Bras Oftalmol. 2011;74:106–9. doi: 10.1590/s0004-27492011000200007. [DOI] [PubMed] [Google Scholar]
- 23.Schmidl D, Weigert G, Dorner GT, Resch H, Kolodjaschna J, Wolzt M, et al. Role of adenosine in the control of choroidal blood flow during changes in ocular perfusion pressure. Invest Ophthalmol Vis Sci. 2011;52:6035–9. doi: 10.1167/iovs.11-7491. [DOI] [PubMed] [Google Scholar]
- 24.Lovasik JV, Kergoat H, Riva CE, Petrig BL, Geiser M. Choroidal blood flow during exercise-induced changes in the ocular perfusion pressure. Invest Ophthalmol Vis Sci. 2003;44:2126–32. doi: 10.1167/iovs.02-0825. [DOI] [PubMed] [Google Scholar]
- 25.Okuno T, Sugiyama T, Kohyama M, Kojima S, Oku H, Ikeda T. Ocular blood flow changes after dynamic exercise in humans. Eye (Lond) 2006;20:796–800. doi: 10.1038/sj.eye.6702004. [DOI] [PubMed] [Google Scholar]
- 26.Bill A. Blood circulation and fluid dynamics in the eye. Physiol Rev. 1975;55:383–417. doi: 10.1152/physrev.1975.55.3.383. [DOI] [PubMed] [Google Scholar]
- 27.Bill A, Sperber GO. Control of retinal and choroidal blood flow. Eye (Lond) 1990;4 (Pt 2):319–25. doi: 10.1038/eye.1990.43. [DOI] [PubMed] [Google Scholar]
- 28.Netter FH. 4th ed. Philadelphia: Saunders; 2006. Atlas of Human Anatomy. [Google Scholar]
- 29.Alwassia AA, Adhi M, Zhang JY, Regatieri CV, Al-Quthami A, Salem D, et al. Exercise-induced acute changes in systolic blood pressure do not alter choroidal thickness as measured by a portable spectral-domain optical coherence tomography device. Retina. 2013;33:160–5. doi: 10.1097/IAE.0b013e3182618c22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Read SA, Collins MJ. The short-term influence of exercise on axial length and intraocular pressure. Eye (Lond) 2011;25:767–74. doi: 10.1038/eye.2011.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kara N, Baz O, Altan C, Satana B, Kurt T, Demirok A. Changes in choroidal thickness, axial length, and ocular perfusion pressure accompanying successful glaucoma filtration surgery. Eye (Lond) 2013;27:940–5. doi: 10.1038/eye.2013.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saeedi O, Pillar A, Jefferys J, Arora K, Friedman D, Quigley H. Change in choroidal thickness and axial length with change in intraocular pressure after trabeculectomy. Br J Ophthalmol. 2014;98:976–9. doi: 10.1136/bjophthalmol-2013-304433. [DOI] [PubMed] [Google Scholar]
- 33.Hong J, Zhang H, Kuo DS, Wang H, Huo Y, Yang D, et al. The short-term effects of exercise on intraocular pressure, choroidal thickness and axial length. PLoS One. 2014;9:e104294. doi: 10.1371/journal.pone.0104294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagaoka T, Kitaya N, Sugawara R, Yokota H, Mori F, Hikichi T, et al. Alteration of choroidal circulation in the foveal region in patients with type 2 diabetes. Br J Ophthalmol. 2004;88:1060–3. doi: 10.1136/bjo.2003.035345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lovasik JV, Kergoat H. Consequences of an increase in the ocular perfusion pressure on the pulsatile ocular blood flow. Optom Vis Sci. 2004;81:692–8. doi: 10.1097/01.opx.0000144748.65471.e5. [DOI] [PubMed] [Google Scholar]
- 36.Maul EA, Friedman DS, Chang DS, Boland MV, Ramulu PY, Jampel HD, et al. Choroidal thickness measured by spectral domain optical coherence tomography: Factors affecting thickness in glaucoma patients. Ophthalmology. 2011;118:1571–9. doi: 10.1016/j.ophtha.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tan CS, Ouyang Y, Ruiz H, Sadda SR. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:261–6. doi: 10.1167/iovs.11-8782. [DOI] [PubMed] [Google Scholar]
- 38.Kim M, Kim SS, Kwon HJ, Koh HJ, Lee SC. Association between choroidal thickness and ocular perfusion pressure in young, healthy subjects: Enhanced depth imaging optical coherence tomography study. Invest Ophthalmol Vis Sci. 2012;53:7710–7. doi: 10.1167/iovs.12-10464. [DOI] [PubMed] [Google Scholar]
- 39.Li XQ, Larsen M, Munch IC. Subfoveal choroidal thickness in relation to sex and axial length in 93 Danish university students. Invest Ophthalmol Vis Sci. 2011;52:8438–41. doi: 10.1167/iovs.11-8108. [DOI] [PubMed] [Google Scholar]
- 40.Polska E, Simader C, Weigert G, Doelemeyer A, Kolodjaschna J, Scharmann O, et al. Regulation of choroidal blood flow during combined changes in intraocular pressure and arterial blood pressure. Invest Ophthalmol Vis Sci. 2007;48:3768–74. doi: 10.1167/iovs.07-0307. [DOI] [PubMed] [Google Scholar]
- 41.Schrödl F, De Laet A, Tassignon MJ, Van Bogaert PP, Brehmer A, Neuhuber WL, et al. Intrinsic choroidal neurons in the human eye: Projections, targets, and basic electrophysiological data. Invest Ophthalmol Vis Sci. 2003;44:3705–12. doi: 10.1167/iovs.03-0232. [DOI] [PubMed] [Google Scholar]
- 42.Schrödl F, Tines R, Brehmer A, Neuhuber WL. Intrinsic choroidal neurons in the duck eye receive sympathetic input: Anatomical evidence for adrenergic modulation of nitrergic functions in the choroid. Cell Tissue Res. 2001;304:175–84. doi: 10.1007/s004410100362. [DOI] [PubMed] [Google Scholar]
- 43.Riva CE, Geiser M, Petrig BL. Beijing 100193, PR China Ocular Blood Flow Research Association. Ocular blood flow assessment using continuous laser Doppler flowmetry. Acta Ophthalmol. 2010;88:622–9. doi: 10.1111/j.1755-3768.2009.01621.x. [DOI] [PubMed] [Google Scholar]
- 44.Rahman W, Chen FK, Yeoh J, Patel P, Tufail A, Da Cruz L. Repeatability of manual subfoveal choroidal thickness measurements in healthy subjects using the technique of enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:2267–71. doi: 10.1167/iovs.10-6024. [DOI] [PubMed] [Google Scholar]
- 45.Ikuno Y, Maruko I, Yasuno Y, Miura M, Sekiryu T, Nishida K, et al. Reproducibility of retinal and choroidal thickness measurements in enhanced depth imaging and high-penetration optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:5536–40. doi: 10.1167/iovs.10-6811. [DOI] [PubMed] [Google Scholar]
- 46.Ulas F, Dogan U, Duran B, Keles A, Agca S, Celebi S. Choroidal thickness changes during the menstrual cycle. Curr Eye Res. 2013;38:1172–81. doi: 10.3109/02713683.2013.811258. [DOI] [PubMed] [Google Scholar]


