Abstract
Background
Accurate intra ocular pressure (IOP) measurement and monitoring using tonometry is a common clinical measurement in diagnosis and management of glaucoma, this is often a challenge in children. The ICare and Perkins tonometers are both handheld tonometers, Perkins uses applanation while ICare measures IOP with a rebound method.
Objectives
The objectives of research were to study the IOP values from each tonometer, compare the value of IOP readings from both tonometers, determined the ease of their use in young children and document the various positions in which the tonometers were used successfully in children.
Method
Intra ocular pressure readings were taken by two experienced examiners in upright position without sedation or anaesthesia. ICare tonometer was first used. Data were entered and analysed with SPSS 17 statistical package. The means were compared using paired sample T-test.
Results
A total of 480 eyes of 240 persons, aged between 2months and 90years with a mean of 46.2±22 years had their intra-ocular pressure range between 3 and 44mmHg( Mean16.3±6) measured using ICare and Perkins tonometry. There was a high correlation, and no statistically significant differences in the mean IOP comparing ICare and Perkins tonometers. The mean difference in average IOP readings between ICare and Perkins was -0.08±2.8 (95% CI: 0.45-0.30; r=0.87, p= 0.68) for right eye and -0.15±2.8mmHg (95% CI -0.53 to 0.23; r=0.86, p=0.44) in the left eye
The difference in the average IOP reading from both tonometers was within 2mmHg 288(66.2%) eyes. Among the 147 (33.8%) eyes with a difference in IOP greater than 2mmHg, Perkins was responsible for the higher IOP reading in 76(51.7%) and ICare in 71(48.3%) p=0.56.
Among 42 eyes of 21 children aged ≤6years, IOP reading was successfully taken in 41(97.6%) and 21(50%) eyes with ICare and Perkins respectively without sedation or anaesthesia.
Conclusion
The IOP readings using the ICare tonometer compares well with that of Perkins tonometer. The ICare was easier to use in young children (≤6year olds) without sedation or anaesthesia in this African population.
Keywords: Intra-ocular pressure, Perkins, ICare, Tonometer, Children
Introduction
Intraocular pressure measurement is one of the most common parameters assessed in patients presenting with eye complaints. It has special applications in the screening, diagnosis and monitoring of glaucoma which is the second leading cause of blindness in Nigeria.
In Glaucoma, raised intra ocular pressure (IOP) and African descent are two important risk factors in its presentation1. A relatively new equipment such as the ICare tonometer needs to be compared with an established and tested equipment such as the Perkins tonometer in this population.
Being sure of the response to treatment is a major concern in childhood glaucoma management especially in children 0-5years who often do not co-operate for IOP measurements with many of the available equipment used for adults. The use of Perkins tonometer in young children often requires a form of sedation/controlled anaesthesia which usually alters the value of IOP readings; ketamine when used as an anaesthetic agent increases IOP readings while the intravenous and inhalational anaesthetic agents reduce IOP readings such that the real IOP values are not known and this impact negatively on monitoring outcome of treatment in addition to the impracticability of repeating anaesthesia as many times as follow up care will demand2.
Different principles have been employed in various instruments used to check IOP; Indentation (Schiotz), Applanation (Perkins and Goldmann), Rebound (ICare), Non- contact tonometry (Air puff). The different models have certain features to make them more attractive to both the eye care providers and the patients.
The best tonometer is one that gives a reliable and valid result, able to be used in any position of the patient, with minimal discomfort to patients, with reduced technicalities, affordable and one that may even allow self-assessment/monitoring by patients3.
The Goldmann applanation tonometer has been the gold standard by which the other tonometers are judged4,5. It is used with a slit lamp microscope with the patient in the upright position. Applanation tonometry by Goldmann or Perkins require the use of fluorescein dye and topical anaesthetic agent which gives a stingy sensation and leaves a sense of heaviness in the eye and so causes more discomfort to the patients and may reduce co-operation in children .
The Perkins tonometer is a non-digital handheld applanation tonometer which does not require a slit lamp like Goldmann applanation tonometer and can be used in supine and upright positions. The intraocular pressure measurement with Perkins has been found to be comparable to that measured with Goldmann Applanation Tonometer. Intra ocular pressure check using the Goldmann tonometer being slit lamp mounted is practically difficult in young children, uncooperative and bed ridden adults in which hand held tonometer like the Perkins, Tonopen and ICare tonometers remain the options available6.
The ICare (ICare Finland Oy, Helsinki, Finland) tonometer is a relatively new portable tonometer that measures intraocular pressure (IOP) using a rebound method, in which a very light probe which is 24mm long and weighs 11mg and with a plastic cover make momentary contact with the cornea in slow motion. The probe slows down faster as the IOP increases and consequently, the higher the IOP the shorter is the duration of impact7.
The ICare tonometer has a small plastic – tipped probe (diameter 0.9mm) surrounded by a magnetic field. It contains an assembly of 2 coils coaxial to a probe shaft that bounces a magnetic probe off the cornea and detects the deceleration of the probe caused by the eye.The moving magnet in the probe induces voltage in the solenoid and the motion parameters of the object are monitored. Whereas the plastic prism used with the Perkins has a diameter of 3.06mm.
The I Care tonometer is digital and has in-built mechanism to reject poor readings while providing an average IOP after taking 6 readings. A peculiar sound heralds the endpoint such that there is no need to look at the readings while being taken.
The probes used by the tonometer are disposable but have been discovered to be reusable with no risk of microbial transmission from one patient to the other8.
The ICare tonometer was shown to be comparable with Goldmann tonometer and can be used by non-ophthalmologists and paramedical personnel during screening tests of populations.9 It has however been shown to give a slightly higher value than Goldmann applanation tonometry in treated glaucoma patients10,11.
ICare was found to overestimate IOP when compared with Perkins in previous studies. The mean difference between Perkins and ICare done on 65 eyes of healthy children was -3.35 ± 2.28 mmHg 12, this is similar to an over estimation of IOP of 3.57mmHg found in the study on 28 eyes of glaucomatous patients receiving travaprost 0.004%13.
The Perkins applanation tonometer is commonly used in our clinic to check IOP of both adults and children when they cooperate; otherwise their IOP is checked during Examination Under Anaesthesia (EUA) limiting the frequency of monitoring because of cost and attendant logistics and risk.
It is therefore important to determine how well the newly acquired ICare tonometer (whose cost is about five times that of Perkins) compares with the handheld Perkins tonometer in this African population since it may serve as the reference instrument especially in the paediatric age group.
The objectives of study were therefore to study the IOP values from each tonometer, compare the value of IOP readings from both tonometers, determined the ease of their use in young children and document the various positions in which the tonometers were used successfully in children.
Patients & Methods
The study was to compare ICare rebound tonometer with the established Perkins applanation tonometer among individuals of all age groups attending the eye clinic in terms of the intraocular pressure values, ease of use and various positions for successful use in children. Ethical clearance for the study was obtained from the Ethical Review Board of our hospital. The study was conducted in adherence to theDeclaration of Helsinki
Study design
A Non- randomized comparative study of diagnostic equipment.
Study Population
Informed consent for inclusion in the study was obtained from patients/care givers of all age groups attending the eye clinic. Consecutive patients were recruited for the study until the sample size was reached. The study was done over a 3-month period in year 2012
Two Intraocular pressure (IOP) readings were taken first with ICare, then Perkins in upright position of patients, in the right eye and then the left eye. ICare tonometer was used first by the first researcher, thereafter, Perkins by the second researcher. The two are experienced in the use of the tonometers.
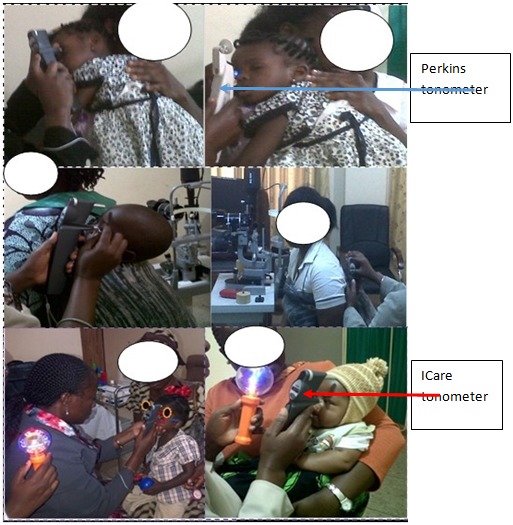
Successful use in children less than 6 years was determined by the number of eyes whose IOP were successfully taken without sedation. Distracting the young children was often needed and was accomplished with the swirling multi-colour light as shown in figure3 which documents the upright positions adopted in which IOP were successfully taken in children. Consent to publish photograph was obtained from the care givers.
Figure 3 . Various Positions the Tonometers were used in Children Less than 6years.
Paired sample T test was employed to compare the means of the IOP readings from tonometers at 95% confidence interval and p-value at 0.05. The data obtained were entered and analyzed with Statistical Package for the Social Sciences - SPSS - version 17.0® Chicago Inc 2003.
Results
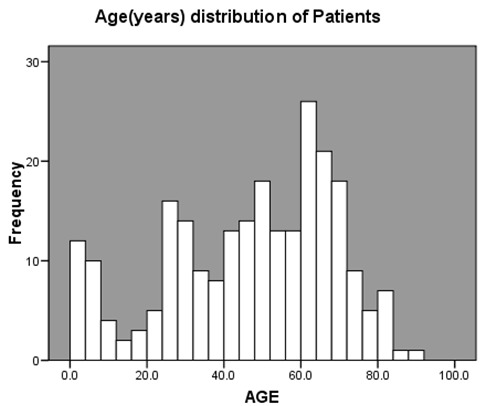
Four hundred and eighty eyes of two hundred and forty (240) patients were included in the study. There were 106(44.2%) males and 134 (55.8%) females with a male: female ratio of 0.8:1 The age range was 2months - 90years with a mean of 46.2±22.04. Twenty-eight (11.7%) patients were children aged <16years, 21(8.8%) were ≤6years- figure1.
Figure 1. Age distribution of the patients.
The IOP reading was within 21mmHg in 405 (85.5%) and 382(87.8%) of the eyes with ICare and Perkins tonometers respectively. In the right eye, the average range of IOP readings was 3 to 42.5mmHg( Mean 17.2±6) with ICare and 2 to 39mmHg( Mean 17.2±5.3) with Perkins, while in the Left Eye (LE), the average range for ICare was 3 to 44mmHg( Mean16.3±6) and for Perkins 2 to 37mmHg (Mean 16.3±5.1). There was no statistically significant difference in the mean IOP values p=0.79 -Table 1.
Table 1 . The First, Second and the Average IOP Readings with the tonometers.
| Frequency | Minimum | Maximum | Mean | SD | |
| 1st reading ICARE RE | 238 | 3.0 | 40 | 17.1 | 6.0 |
| 2nd reading ICARE RE | 237 | 3.0 | 46 | 17.3 | 6.1 |
| Average reading ICARE RE | 237 | 3.0 | 42.5 | 17.2 | 6.0 |
| 1st reading Perkins RE | 216 | 2.0 | 38 | 17.0 | 5.3 |
| 2nd reading Perkins RE | 217 | 2.0 | 40 | 17.3 | 5.4 |
| Average reading Perkins RE | 217 | 2.0 | 39.0 | 17.1 | 5.3 |
| 1st reading ICARE LE | 236 | 3.0 | 46 | 16.3 | 6.1 |
| 2nd Reading ICARE LE | 235 | 3.0 | 44 | 16.4 | 6.1 |
| Average reading ICare LE | 235 | 3.0 | 44.0 | 16.3 | 6.0 |
| 1st reading Perkins LE | 219 | 2.0 | 36 | 16.1 | 5.1 |
| 2nd reading Perkins LE | 218 | 2.0 | 38 | 16.6 | 5.2 |
| Average reading Perkins LE | 218 | 2.0 | 37.0 | 16.3 | 5.1 |
| p=0.79 | |||||
| RE- Right Eye, LE- Left Eye, SD – Standard Deviation, p= p-value | |||||
Two IOP readings were taken with Perkins and ICare tonometers. The two readings from each tonometer showed statistically significant (p=0.00) high correlation coefficient (r=0.96 for ICare and r=0.98 for Perkins). In about half of the cases, the second IOP readings were more likely to be higher than the first IOP readings with either Perkins( p=0.01) or ICare (p=0.04) tonometers, Perkins 196(45.1%) however had more cases of same first and second IOP readings than ICare 137(29.1%).
This differences in the first and second IOP readings with either of the two tonometers were within 2mmHg in about 420(89%) of the eyes using ICare and 421(97%) for Perkins tonometer making it not statistically significant p=0.79-Table 1.
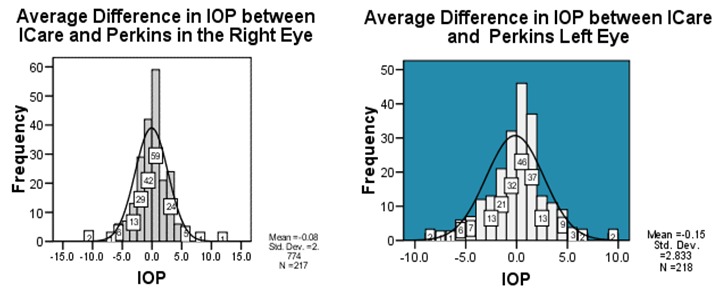
Comparing the Perkins and ICare revealed a high correlation coefficient and no statistically significant differences in their IOP readings; the mean difference in average IOP readings between ICare and Perkins was -0.08±2.8 (95% CI: 0.45-0.30; r=0.87, p= 0.68) for right eye and -0.15±2.8mmHg (95% CI -0.53 to 0.23; r=0.86, p=0.44) in the left eye–Table 2.
Table 2 . Correlation and Differences in IOP readings with the Tonometers.
| Paired sample correlation | Paired Sample Difference | |||||||
| 95% CI | ||||||||
| N | Correlation | P | Mean | SD | Upper | Lower | P | |
| 1st reading ICARE RE - 2nd reading I CARE RE | 237 | .969 | .000 | -0.25 | 1.5 | -0.45 | -0.06 | .010 |
| 1st reading Perkins RE - 2nd reading Perkins RE | 215 | .983 | .000 | -0.35 | 1.0 | -0.49 | -0.22 | .000 |
| Average reading ICARE RE - Average reading Perkins RE | 217 | .873 | .000 | -0.08 | 2.8 | -0.45 | 0.30 | .685 |
| 1st reading ICARE LE - 2nd Reading ICARE LE | 236 | .963 | .000 | -0.20 | 1.7 | -0.41 | 0.01 | .070 |
| 1st reading Perkins LE - 2nd reading Perkins LE | 218 | .980 | .000 | -0.46 | 1.0 | -0.60 | -0.32 | .000 |
| Average reading ICare LE -Average reading Perkins LE | 218 | .862 | .000 | -0.15 | 2.8 | -0.53 | 0.23 | .438 |
| N= Frequency, CI= Confidence Interval., P= p-value , SD= Standard Deviation, | ||||||||
The difference in the average IOP reading from both tonometers was within 2mmHg 288(66.2%) eyes and more than 2mmHg in 147(33.8%) eyes- figure2. Among the 147 eyes with a difference in IOP greater than 2mmHg, Perkins was responsible for the higher IOP reading in 76(51.7%) and ICare in 71(48.3%) p=0.56, this was not statistically significant.
Figure 2. Distribution of Difference in Average IOP between ICare and Perkins Tonometers.
Success of IOP Measurement without Sedation or anaesthesia in Children aged ≤6years
Among 42 eyes of 21 children 6years or less, it was possible to take the IOP in 41(97.6%) and 21(50%) eyes with ICare and Perkins tonometer respectively. IOP were successfully taken in the awake or sleeping young children in natural and traditional positions like child strapped on mother’s back, child placed on the shoulder or prodded on the lap and distracted with toys as shown in figure3. Because of the small size of the tip of the ICare probe, it was possible to take IOP in crying children, this was however found to increase the IOP reading by about 10mmHg when compared to IOP readings taken in the same children while calm.
Discussion
The high correlation between the first and second IOP readings with both the ICare and perkins tonometers with a difference within 2mmHg in about 89% of the eyes with ICare and 97% for Perkins tonometer points to a high reproducibility of their readings.
The first and second readings were same in 29.1% with ICare and 45.1% of eyes using Perkins; the observable differences between the two tonometers might probably be because the ICare is a more a dynamic tonometer based on making a moving object collide with an eye and on monitoring the motion parameters of this object following contact14 this might have made the ICare more responsive to changing dynamics as the probe bounces on and off the corneal. Davies15also found that the Inter-sessional repeatability of IOP taken with ICare is poorer than that of IOP taken with the Goldmann tonometer, but is comparable with that of other non Goldmann-type tonometers currently available.
The statistically significant high correlation(r=0.86, P=0.000) between the average IOP readings of Perkins and ICare tonometers and the findings of no statistically significant differences in their mean IOP readings is similar to the findings from other studies13,16,17.
The differences in IOP readings from both tonometers were within 2mmHg in about two third of the eyes checked, this is similar to the findings of Rosenterer17 and within 3mmHg in about 78% of the eyes unlike 69% and 53% within 3mmHg reported by Schild18and Diaz13 respectively.
Among the 147 eyes with an IOP difference greater than 2mmHg ,the contributions of Perkins and ICare tonometers was almost equal, 76(51.7%) by Perkins and ICare 71(48.3%) p=0.56. This is at variance with other studies which reported a tendency for ICare tonometer to overestimate,12,13,17 this is probably because the other studies included much fewer eyes.
Being able to take IOP in more children with ICare without sedation/anaesthesia and in the various comfortable positions - figure3- for both the parents, children and the examiner has impacted positively on the care of children; this is because of the ability to monitor IOP as necessary without the known influence of anaesthetic agent of the IOP values, cheaper cost of checking IOP with ICare in the clinic and removal of logistic challenges of EUA. This is similar to the findings of Li and Grigorian19,16.
The ability to reuse the probe with minimal risk of transmission of infection as documented by Briesen8 also reduced the running cost thereby making it a more useful tool in developing economies such as ours.
Conclusions
The IOP readings using the ICare tonometer compared well with those of Perkins tonometer. Compared to Perkins tonometer, the use of ICare tonometer for IOP was successful in many young children (≤6year olds) without sedation/anaesthesia, it therefore presented a safe and cost effective monitoring of IOP in the follow up care of childhood glaucoma.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Grant support: None
References
- 1.Bron A, Chaine G, Villain M, Colin J, Nordmann JP, Renard JP. Risk factors for primary open-angle glaucoma. J Fr Ophtalmol. 2008;31:435–444. doi: 10.1016/s0181-5512(08)71443-8. [DOI] [PubMed] [Google Scholar]
- 2.Blumberg D, Congdon N, Jampel H, Gilbert D, Elliott R, Rivers R. The effects of sevoflurane and ketamine on intraocular pressure in children during examination under anesthesia. Am J Ophthalmol. 2007;143:494–499. doi: 10.1016/j.ajo.2006.11.061. [DOI] [PubMed] [Google Scholar]
- 3.Asrani S, Chatterjee A, Wallace DK, Santiago-Turla C, Stinnett S. Evaluation of the ICare rebound tonometer as a home intraocular pressure monitoring device. J Glaucoma. 2011;20(2):74–79. doi: 10.1097/IJG.0b013e3181d78811. [DOI] [PubMed] [Google Scholar]
- 4.Kass MA. Standardizing the measurement of intraocular pressure for clinical research. Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103:183–185. doi: 10.1016/s0161-6420(96)30741-0. [DOI] [PubMed] [Google Scholar]
- 5.Hager A, Wiegand W. Methods of measuring intraocular pressure independently of central corneal thickness. Ophthalmologie. 2008;105:840–844. doi: 10.1007/s00347-008-1729-8. [DOI] [PubMed] [Google Scholar]
- 16.Schreiber W, Vorwerk CK, Langenbucher A, Behrens-Baumann W, Viestenz A. A comparison of rebound tonometry (ICare) with TonoPenXL and Goldmann applanation tonometry. Ophthalmologe. 2007;104:299–304. doi: 10.1007/s00347-007-1487-z. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Resua C, González-Meijome JM, Gilino J, Yebra-Pimentel E. Accuracy of Icare tonometry. Optom Vis Sci. 2006;83(2):102–106. doi: 10.1097/01.opx.0000200673.96758.7b. [DOI] [PubMed] [Google Scholar]
- 8.Briesen S, Schulze SM, Roberts H, Kollmann M, Stachs O, Behrend D, Schäfer S, Guthoff R. Minimal cross-infection risk through Icare rebound tonometer probes: a useful tool for IOP-screenings in developing countries. Eye (Lond) 2010 Jun;24(7):1279–1283. doi: 10.1038/eye.2009.297. [DOI] [PubMed] [Google Scholar]
- 9.Abraham LM, Epasinghe NC, Selva D, Casson R. Comparison of the ICare rebound tonometer with the Goldmann applanation tonometer by experienced and inexperienced tonometrists. Eye (Lond) 2008;22:503–506. doi: 10.1038/sj.eye.6702669. [DOI] [PubMed] [Google Scholar]
- 10.Gandhi NG, Prakalapakorn SG, El-Dairi MA, Jones SK, Freedman SF. Care ONE rebound versus Goldmann applanation tonometry in children with known or suspected glaucoma. Am J Ophthalmol. 2012;154:843–849. doi: 10.1016/j.ajo.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Vincent SJ, Vincent VR, Shields D, Lee GA. Comparison of intraocular pressure measurement between rebound, non-contact and Goldmann applanation tonometry in treated glaucoma patients. Clin Experiment Ophthalmol. 2012 05 - 06;40(4):163–70. doi: 10.1111/j.1442-9071.2011.02670.x. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Resua C, Gonzalez-Meijome JM, Gilino J, Yebra-Pimentel E. Accuracy of the new ICare rebound tonometer vs. other portable tonometers in healthy eyes. Optom Vis Sci. 2006;83:102–107. doi: 10.1097/01.opx.0000200673.96758.7b. [DOI] [PubMed] [Google Scholar]
- 13.Diaz A, Yebra-Pimentel E, Resua CG, Gilino J, Giraldez MJ. Accuracy of the ICare rebound tonometer in glaucomatous eyes with topical ocular hypotensive medication. Ophthalmic Physiol Opt. 2008;28:29–34. doi: 10.1111/j.1475-1313.2007.00526.x. [DOI] [PubMed] [Google Scholar]
- 14.Detry-Morel M, Jamart J, Detry MB, Pourjavan S, Charlier L, Dethinne B. Clinical evaluation of the dynamic rebound tonometer Icare. J Fr Ophtalmol. 2006;29:1119–1127. doi: 10.1016/s0181-5512(06)73907-9. [DOI] [PubMed] [Google Scholar]
- 15.Davies LN, Bartlett H, Mallen EA, Wolffsohn JS. Clinical evaluation of rebound tonometer. Acta Ophthalmol Scand. 2006;84:206–209. doi: 10.1111/j.1600-0420.2005.00610.x. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Tang L, Xiao M, Jia S, Liu P, Zhou Y. omparison of the Icare Tonometer and the Hand-held Goldmann Applanation Tonometer in Pediatric Aphakia. J Glaucoma. 2013 Mar;22(3):250–254. doi: 10.1097/IJG.0b013e31825afc87. [DOI] [PubMed] [Google Scholar]
- 17.Rosentreter A, Schild AM, Lappas A, Krieglstein GK, Dietlein TS. Rebound tonometry and applanation tonometry during narcosis investigation of pediatric glaucoma. Ophthalmologe. 2011;108:331–336. doi: 10.1007/s00347-010-2286-5. [DOI] [PubMed] [Google Scholar]
- 18.Schild AM, Rosentreter A, Hermann MM, Muether PS, Schroeter SI, Lappas A. Comparison of Rebound tonometry versus Perkins tonometry in the supine glaucoma patient. Klin Monbl Augenheilkd. 2010;228:125–129. doi: 10.1055/s-0029-1245741. [DOI] [PubMed] [Google Scholar]
- 19.Grigorian F, Grigorian AP, Olitsky SE. The use of the Icare tonometer reduced the need for anesthesia to measure intraocular pressure in children. J AAPOS. 2012;16:508–510. doi: 10.1016/j.jaapos.2012.07.004. [DOI] [PubMed] [Google Scholar]


