Abstract
Hereditary fructose intolerance (HFI) is a difficult-to-confirm diagnosis, requiring either invasive liver biopsy-enzyme assay or potentially hazardous fructose challenge test or expensive molecular genetic analysis. Therefore, worldwide there has been a trend towards finding “common mutations” in distinct ethnic groups to simplify the process of diagnosis. The nonspecific presentation of the disease often leads to diagnostic confusion with other metabolic liver disorders such as glycogenoses, galactosemia, and tyrosinemia. This leads to much delay in diagnosis with consequent harm to the patient.
We report mutations in the ALDOB gene, from eleven Indian patients, seven of whom belong to the Agarwal community. Six patients from the Agarwal community and two non-Agarwal patients harbored one novel mutation, c.324+1G>A (five homozygous and one heterozygous), in the ALDOB gene. Haplotyping performed in families confirmed a founder effect. The community has been known to harbor founder mutations in other genes such as the MLC1, PANK2, and CAPN3 genes, thus providing another evidence for a founder effect in the community in case of HFI. This may pave the path for a simpler and quicker test at least for this community in India. In addition to the founder mutation, we report four other novel mutations, c.112+1delG, c.380-1G>A, c.677G>A, and c.689delA, and a previously reported mutation, c.1013C>T, in the cohort from India.
Introduction
Hereditary fructose intolerance (HFI, OMIN #229600) is a potentially fatal inborn error of metabolism (IEM) resulting from deficiency of aldolase B enzyme (EC 4.1.2.13), encoded by the ALDOB gene (OMIM *612724) in the liver and kidneys. The disorder is extremely important to recognize as it is easy to treat and has excellent outcome on avoidance of fructose- and sucrose-containing foods and dietary products (Steinmann and Santer 2012). Therapy does not involve any expensive diets or medications. In view of its rarity and practical difficulties in diagnosis, many HFI patients remain undiagnosed and suffer permanent liver damage, increasing the morbidity and sometimes mortality. The most difficult part in HFI has been establishing a diagnosis. Traditionally, these children when suspected on clinical grounds were subjected to “fructose challenge test” which is potentially life-threatening in view of sudden hypoglycemia in patients (Steinmann and Gitzelmann 1981). It has therefore become obsolete now. Enzyme assay requires a liver biopsy, an invasive test, and estimation can be performed only in a few laboratories around the world. The liver sample requires to be shipped under dry ice which adds to the cost and is not often feasible for long distances. Further, the enzyme activity in the liver may be secondarily reduced in a damaged liver (Steinmann and Santer 2012). Thus, the most accurate method to diagnose is through gene studies. Worldwide, many founder and common mutations have been identified in many communities, which has simplified the ALDOB molecular analysis by using population-specific custom protocols (Coffee et al. 2010; Esposito et al. 2010). India is a unique mix of many populations but marriage within communities creates the background for the presence of founder mutations in various IEMs.
We performed sequencing of the ALDOB gene in eleven patients from nine families, who were strongly suspected to have HFI. We report the existence of a founder mutation in the Agarwal community from North India. The single most common mutation, c.324+1G>A, in the ALDOB gene was observed in homozygous form in five and heterozygous state in one of seven patients from the Agarwal community. This mutation was also noted in two non-Agarwal patients in heterozygous state. Sequencing of the ALDOB gene also revealed presence of four new mutations in the cohort.
Materials and Methods
Consecutive patients presenting to genetics clinics at Sir Ganga Ram Hospital and All India Institute of Medical Sciences, New Delhi, with history consistent with HFI were recruited. There were 11 patients in the cohort from 9 families from North India, including a trio of mother and two children.
Clinical data was collected from each patient and family including the demographic details, the ethnic group, age of presentation, main clinical features, and investigation details that were performed prior to diagnosis of HFI in each family. Few patients had been on clinical follow-up for few years before recruitment into the study.
Molecular analysis was performed for a diagnostic purpose. Informed consent was taken for the test as well as for haplotype analysis from parents of each case. As this was a diagnostic study of a small scale, no ethical clearance was required from the hospital ethics committee.
Molecular Analysis
DNA was isolated by salting out method from 2 mL of whole blood (Miller et al. 1988). All nine exons and exon-intron boundaries of the ALDOB gene were amplified using intronic primers flanking the exons (primer sequences available on request). PCR was performed using 10 pmol of each primer, 1U of Taq DNA polymerase, 1.5 mM MgCl2, and 0.1 mM dNTPs in the recommended buffer with the initial denaturation at 94°C for 5 min, 35 cycles of denaturation at 94°C for 30s, annealing at 58°C for 30 s, and extension at 72°C for 45 s. Sequencing was carried out on ABI 3500 analyzer covering all the nine coding exons encompassing nearly 80 bp of the exon-intron boundaries (Applied biosystems, California). Sequence chromatograms obtained were analyzed with Chromas software (Technelysium, Tewantin, Australia) and blasted with UCSC ALDOB genome browser.
Haplotype analysis was performed to determine if mutation carriers shared a common ancestry. Members from five families were analyzed using eight single-nucleotide polymorphic markers (rs9299349, rs12686025, rs970385, rs10819926, rs2417251, rs10989471, rs10989412, rs1338739) spanning approximately 1 Mb interval at the chromosomal region 9q31.1, which contains the ALDOB gene.
Bioinformatics Analysis
Gene-prediction tools GENSCAN, AUGUSTUS, GeneID, and GeneMark were used to analyze the effect of intronic mutations c.112+1delG, c.324+1G>A, and c.380-1G>A (Burge and Karlin 1997; Stanke et al. 2004; Blanco et al. 2007; Lomsadze et al. 2005). The aldolase B protein structure was modeled based on 1XDL.pdb (a thermolabile A149P aldolase B mutant) using Modeller (Sali and Blundell 1993).
Results
In the cohort of 11 patients, 7 were from the Agarwal community. Consanguinity was noted in one family (family 8). Children presented in infancy with typical symptoms of failure to thrive with either vomiting and diarrhea or progressive liver disease. A detailed account of the cases is provided in Table 1. There was only one adult in the cohort, the mother of two children (family 3), who gave history of aversion to fruits and sugar since childhood. Few unusual features are also highlighted in the table such as the custom of offering honey to newborns resulting in much earlier clinical presentation than expected in a few children.
Table 1.
Detailed clinical presentation and mutation analysis results of cases
| Family number | 1 | 2 | 3 | 3 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases (initials) | ST | AA | PJ | BJ | BG(mother of PJ and BJ) | RS | SR | SS | MG | SYK | B |
| Age at onset of Symptoms | 2.5 monthsa | 4 months | 5 months | Birtha | Infancy | 1 year | 1.6 years | 10 months | 4 months | 7 months | 9 months |
| Age at diagnosis | 18 months | 18 months | 1 year | Birth | Adult | 1 year | 2.5 years | 2.5 years | 9 months | 13 months | 3 years |
| Presenting complaints | Diarrhea, failure to thrive | Abdominal distension, failure to thrive | Vomiting, failure to thrive | Vomiting | Vomiting, aversion to sugar in milk | Vomiting, failure to thrive | Vomiting, failure to thrive | Vomiting after sugar in milk, failure to thrive | Vomiting at weaning (4 months), diarrhea at 8 months | Failure to thrive, constipation, liver disease | Vomiting, diarrhea, and jaundice |
| Hepatomegaly | Yes | Yes | Yes | No | Not known | Yes | Yes | Yes | Yes | Yes, 4 cm BCM | Yes, 4 cm BCM |
| Liver dysfunction before treatment | Yes | Yes | Yes | No | Yes (childhood and pregnancy) | Yes, mildly deranged liver enzymes | Yes | Yes | Yes | Yes | Yes, mildly deranged SGPT |
| Renal involvement | Yes | Yes | No | No | No | No | No | No | No | Yes | No |
| Liver biopsy performed, findings | Yes, granulomatous hepatitis, macrosteatosis | Yes, details not available | Yes, details not available | No | No | Yes, details not available | Yes, details not available | No | Yes, details not available | Yes, disarrayed lobular architecture, porto-portal bridging fibrosis. Panlobular macro- and microvesicular steatosis | No |
| Fructose challenge test | Not performed | Not performed | Performed, positive | Not performed | Not performed | Performed, positive | Performed, positive | Performed, positive | Not performed | Not performed | Not performed |
| Hypoglycemia | No | Yes | No | Yesa | Never tested | Yes | No | No | No | No | Yes |
| Other significant finding | Developmental delay, abnormal transferrin isoforms | Occasional epistaxis, requires vit. K. LFTs normal | No | Seizure at day 17 of life. Normal development | No | No | No | Idiopathic hypokalemia at the age of 10 months | Milk protein allergy (milk allergen specific IgE 41.8 [<0.1]), hyperreactive airway disease | No | Mild gross motor delay |
| Diet history suggestive | Yes (in retrospect) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Gene study: mutations in the ALDOB gene | Homozygous | Homozygous | Homozygous | Homozygous | Homozygous | Compound heterozygous | Homozygous | Homozygous | Compound heterozygous | Homozygous | Compound heterozygous |
| c.324+1G>A, exon 3/intron 3 boundary | c.324+1G>A, exon 3/intron 3 boundary | c.324+1G>A, exon 3/intron 3 boundary | c.324+1G>A, exon 3/intron 3 boundary | c.324+1G>A, exon 3/intron 3 boundary | c.324+1G>A, exon 3/intron 3 boundary | c.112+1 del G, exon 2/ intron 2 boundary | c.677G>A, exon 7 | c.324+1G>A, exon 3/intron 3 boundary | c.1013C>T, exon 9 | c.324+1G>A, exon 3/intron 3 boundary | |
| c.1013C>T, exon 9 | c.689delA, exon 7 | c.380-1G>A intron 4/exon 5 boundary | |||||||||
| Current clinical status | 5 years – mild developmental delay – attends normal school but learning difficulty+, hepatomegaly (12 cm span at 5 years), normal liver function and renal function | 5 years – normal development, attending regular school. Mild hepatomegaly (span 9 cm at 5 years), Liver function tests normal, spleen 8 cm, mild nephrocalcinosis with normal renal functions | 7.5 years – normal development, in grade 2 at regular school, mild hepatomegaly, normal liver and renal function | 3 years of age – normal development, attending preschool, mild hepatomegaly, normal liver and renal function | Adult – mild hepatomegaly, normal liver and renal functions | 10 years – normal development. No seizures, attends regular school. Liver 5 cm below costal margin. Liver function test normal | 7 years – mild developmental delay, no seizures, doing well, normal liver and renal functions | 7 year 10 months – normal development. Liver palpable 3.5 cm below costal margin. Normal liver and renal function | 2 year 7 months – normal development, poor weight gain, liver about 3 cm below costal margin, normal liver function and renal function | 3.3 years old well child. No hepatomegaly. Normal liver and renal functions | 4 years – normal development, failure to thrive, seizure, liver palpable 3 cm and spleen 2 cm below costal margins, normal liver and renal function |
| Response to treatment | Satisfactory | Good | Very good | Very good | Good | Very good | Satisfactory | Very good | Good (also has milk protein allergy) | Excellent | Satisfactory |
aIntake of honey
Molecular and Computational Analysis
Molecular genetic analysis of the ALDOB gene through sequencing revealed six new sequence variants in 22 mutated alleles, of which c.324+1G>A mutation was noted in 13 of 22 (5 in homozygous state and three heterozygous). Other mutations were: homozygous c.112+1 delG and c.677G>A in one patient each, heterozygous c.689delA and c.380-1G>A in one patient each, and heterozygous and homozygous c.1013C>T mutation in one patient each.
Mutations c.324+1G>A, c.112+1delG, c.380-1G>A, c.677G>A, and c.689delA were noted to be novel, whereas c.1013C>T is a previously reported mutation. A widely used and one of the most accurate gene-prediction program, GENSCAN, predicted that all the three intronic mutations c.112+1delG, c.324+1G>A, and c.380-1G>A disrupt splicing and result in abnormal protein with 8, 4, and 6 amino acids deletion, respectively (Figs. 1 and 2). The GENSCAN predictions were in corroboration with those of three other tools (AUGUSTUS, GeneMark, and GeneID) for c.324+1G>A and c.380-1G>A mutations. However, for the c.112+1delG mutation, AUGUSTUS predicted an insertion of amino acid valine at position 36 (Fig. 1), while both GeneMark and GeneID predicted that the single aldolase B polyprotein would break into two smaller fragments (data not shown). The exonic mutation c.677G>A leads to a p.G226D mutation in the aldolase B protein (Figs. 1 and 2). Although homology modeling predicted that this alteration does not affect the protein structure (data not shown), a distinct single amino acid mutation p.A149P is known to cause losses in thermal stability, quaternary structure, and activity (Malay et al. 2005). The effects of p.A149P mutation could also not be predicted by homology modeling and underscores the difficulties in predicting perturbations due to single amino acid changes (Malay et al. 2005). On the other hand, the second exonic mutation c.689delA is a frameshift mutation that results in premature termination of the polypeptide and deletion of ~130 C-terminal amino acids of aldolase B protein (Figs. 1 and 2). All five mutations were detected to be damaging using SIFT, Polyphen II, and Mutation Taster (http://sift.jcvi.org/www/SIFT_enst_submit.html, http://genetics.bwh.harvard.edu/pph2/, http://www.mutationtaster.org/).
Fig. 1.
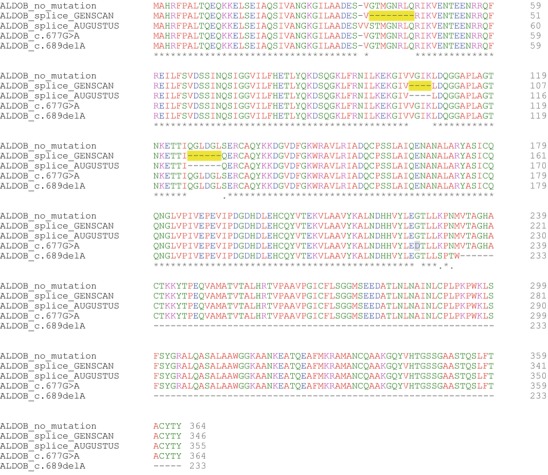
Alignment of aldolase B protein sequences. The intronic mutations c.112+1delG, c.324+1G>A, and c.380-1G>A result in 8, 4, and 6 amino acid deletions, respectively (shaded in yellow; GENSCAN program prediction). The residue 226 altered due to exonic mutation c.677G>A is shaded in gray. Alignment was performed using Clustal Omega at http://www.ebi.ac.uk/Tools/msa/clustalo/. ALDOB_no_mutation, wild-type protein sequence; ALDOB_splice_GENSCAN and ALDOB_splice_AUGUSTUS, predicted proteins of gene with intronic mutations by GENSCAN and AUGUSTUS, respectively; ALDOB_c.677G>A and ALDOB_c.689delA, protein sequence of gene with exonic mutations c.677G>A and c.689delA, respectively
Fig. 2.

Modeled structure of wild-type aldolase B. The residues that get deleted (predicted by GENSCAN program) due to intronic mutations c.112+1delG, c.324+1G>A, and c.380-1G>A have been shown in orange, pink, and blue, respectively. The residue 226 altered due to exonic mutation c.677G>A is highlighted in red. The structure marked in brown gets deleted in gene with c.689delA mutation. The structure in panel B is derived by rotating the panel A structure by 260° along y-axis
Homozygous mutation c.324+1G>A was noted in five of seven Agarwal patients. In addition, it also occurred in heterozygous form in one Agarwal and two non-Agarwal patients. Another child from the Agarwal community harbored a different c.112+1delG mutation in homozygous state. These findings led us to investigate the presence of a founder effect in the community, which is known to harbor other founder mutations (Gorospe et al. 2004; Bahl et al. 2005; Chabbria et al. 2007).
Haplotype Analysis
Eight single-nucleotide polymorphisms (SNPs) were analyzed flanking the mutation c.324+1G>A. These included both intragenic and flanking regions mapping up to 1 Mb. Homozygosity mapping in the families using trios of child and parents revealed identical haplotypes with the c.324+1G>A mutation as shown in the Fig. 3. All patients harboring homozygous mutation had identical haplotype on both chromosomes. The Agarwal patient with heterozygous mutation showed a different haplotype on one chromosome. All the markers tested seemed to be in linkage disequilibrium with the mutation c.324+1G>A in the ALDOB gene. This haplotype was different from haplotype in another Agarwal patient who had a different mutation, c.112+1delG. These findings confirm the presence of a founder effect in the subpopulation.
Fig. 3.

Haplotype analysis in Agarwal families
Discussion
HFI is a unique inborn error of metabolism where the major hurdle lies in making an accurate diagnosis rather than treatment which is as simple as removal of fructose and sucrose from the diet. The outcome is related to severity of initial presentation, comorbidities, and the time taken for diagnosis after onset of symptoms and commencement of therapy. In our cases, majority of children are doing well, with no developmental delay and only mild hepatomegaly. Two children have developmental delay related to the severity of the symptoms at onset and delay in diagnosis. Traditionally, the disorder has either remained unconfirmed or diagnosed only after invasive liver biopsy enzymology or a fructose challenge test which can prove hazardous in view of rapid hypoglycemia after fructose intake (Steinmann and Gitzelmann 1981). Worldwide, common mutations such as p.A149P mutation, which showed a founder effect in studies, have simplified the diagnostic strategy in certain populations (Brooks and Tolan 1993). There is a paucity of literature on HFI and ALDOB gene studies from India, as only few case reports, without mutations, have been reported (Bharadia and Shivpuri 2012; Ananth et al. 2003). This is the first report of mutations in the ALDOB gene from India.
In our cohort of patients, all patients have shown remarkable improvement in clinical condition and catch-up growth once treatment is commenced after diagnosis. This is consistent with the established literature (Steinmann and Santer 2012; Steinmann and Gitzelmann 1981) and emphasizes the need for an early and accurate diagnosis.
The Indian population is a heterogeneous mix of various communities, and the common Caucasian mutations are not expected to be present. The gene pool is expected to be heterogeneous but with pockets of homogeneity because of the general trend of marriages within closed communities. The Agarwal community is a large enterprising community consisting of affluent business-class North Indian population originating from a small town of Agroha, near Delhi and spreading all over the world (Singhal 2005). Genetic studies have suggested founder effect in Agarwals in some other genetic disorders like megalencephalic leukoencephalopathy with subcortical cysts (MLC, OMIM #604004), spinocerebellar ataxia type 12 (OMIM #183090), and pantothenate kinase-associated neurodegeneration (PKAN, OMIM#234200) (Gorospe et al. 2004; Bahl et al. 2005; Chabbria et al. 2007). Recently, two mutations have been shown to have founder effect in Agarwals in calpain-3 gene (CAPN3, OMIM *114240) in patients of LGMD type 2A (OMIM #253600) (Ankala et al. 2013).
Our molecular analysis in the Agarwal families revealed homozygous segment of DNA spanning 1 mb flanking the ALDOB gene, on haplotype analysis. This haplotype was in linkage disequilibrium with the mutation c.324+1G>A, as this did not match with another Agarwal patient harboring a different mutation, thus confirming a founder effect.
The information about the common mutation is likely to benefit our Indian patients who have been visiting the clinics of pediatricians, gastroenterologists, and geneticists for years without a diagnosis. It will simplify the diagnosis of this condition, at least in the Agarwal community, thus leading to an excellent outcome after early diagnosis.
We also report four other novel mutations from our cohort, including splice site mutations c.112+1 delG and c.380-1G>A as well as exonic mutations c.677G>A and c.689delA. The presence of more novel mutations than previously reported in literature is suggestive of a different gene pool among the Indian population. Only one of six mutations, c.1013C>T, is previously reported. Interestingly this mutation was noted in a child belonging to a consanguineous family from Kashmir. The Kashmir population has been noted by our group to share the gene pool with the Caucasian population based on genetic studies in other disorders, one notable example being cystic fibrosis. We propose a stepwise molecular diagnostic approach in children suspected to have HFI, based on their ethnicity within the Indian population.
Acknowledgements
We would like to acknowledge the contribution of Dr Rebecca Treacy and Dr J Drummond, East Anglican Medical Genetics Service Genetics Lab, Addenbrooke’s hospital, Cambridge, UK, for sequencing of the ALDOB gene in two patients. Deepak Sharma is thankful to his institute for the core grant for the bioinformatic study.
Take-Home Message
First report of molecular mutations in HFI from India, founder mutation in the Agarwal community. Simplifying diagnosis for easily treatable yet life-threatening metabolic condition.
Conflict of Interest
All the authors (Sunita Bijarnia-Mahay, Sireesha Movva, Neerja Gupta, Deepak Sharma, Ratna D. Puri, Udhaya Kotecha, Renu Saxena, Madhulika Kabra, Neelam Mohan and Ishwar C Verma) declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Details of the Contributions of Individual Authors
- Sunita Bijarnia-Mahay
- Conception and design
- Clinical management of children with HFI
- Analysis and interpretation of data
- Drafting the article
- Sireesha Movva
- Analysis and interpretation of data, haplotype analysis
- Drafting the article (molecular methodology)
- Neerja Gupta
- Conception and design
- Clinical management of children with HFI
- Drafting the article (provided patient information)
- Deepak Sharma
- Analysis and interpretation of data (computational analysis and bioinformatics)
- Drafting the article (methodology and results of bioinformatics)
- Ratna Dua Puri
- Conception and design
- Clinical management of children with HFI
- Drafting the article (provided patient information)
- Udhaya Kotecha
- Conception and design
- Clinical management of children with HFI
- Drafting the article (provided patient information)
- Renu Saxena
- Analysis and interpretation of data, haplotype analysis
- Revising it critically for important intellectual content)
- Madhulika Kabra
- Conception and design
- Clinical management of children with HFI
- Neelam Mohan
- Conception and design
- Clinical management of children with HFI
- Ishwar C Verma
- Clinical management of children with HFI
- Revising it critically for important intellectual content)
Footnotes
Competing interests: None declared
Contributor Information
Sunita Bijarnia-Mahay, Email: bijarnia@gmail.com, Email: sunitabijarnia@sgrh.com.
Collaborators: Johannes Zschocke
References
- Ananth N, Praveenkumar GS, Rao KA, Vasanthi, Kakkilaya S. Two cases of hereditary fructose intolerance. Indian J Clin Biochem. 2003;18(2):87–92. doi: 10.1007/BF02867372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ankala A, Kohn JN, Dastur R, Gaitonde P, Khadilkar SV, Hegde MR. Ancestral founder mutations in calpain-3 in the Indian Agarwal community: historical, clinical, and molecular perspective. Muscle Nerve. 2013;47(6):931–937. doi: 10.1002/mus.23763. [DOI] [PubMed] [Google Scholar]
- Bahl S, Virdi K, Mittal U, Sachdeva MP, Kalla AK, Holmes SE, O’Hearn E, Margolis RL, Jain S, Srivastava AK, Mukerji M. Evidence of a common founder for SCA12 in the Indian population. Ann Hum Genet. 2005;69:528–534. doi: 10.1046/j.1529-8817.2005.00173.x. [DOI] [PubMed] [Google Scholar]
- Bharadia L, Shivpuri D. Non responsive celiac disease due to coexisting hereditary fructose intolerance. Indian J Gastroenterol. 2012;31(2):83–84. doi: 10.1007/s12664-012-0169-1. [DOI] [PubMed] [Google Scholar]
- Blanco E, Parra G, Guigó R. Using gene id to identify genes. Curr Protoc Bioinformatics. 2007 doi: 10.1002/0471250953.bi0403s18. [DOI] [PubMed] [Google Scholar]
- Brooks CC, Tolan DR. Association of the widespread p.A149P hereditary fructose intolerance mutation with newly identified sequence polymorphisms in the Aldolase B gene. Am J Hum Genet. 1993;52:835–840. [PMC free article] [PubMed] [Google Scholar]
- Burge C, Karlin S. Prediction of complete gene structures in human genomic DNA. J Mol Biol. 1997;268(1):78–94. doi: 10.1006/jmbi.1997.0951. [DOI] [PubMed] [Google Scholar]
- Chabbria R, Udani V, Das S, Shah R. Founder mutation in the PANK gene of Agrawal children with neurodegeneration with brain iron accumulation (NBIA) Ann Indian Acad Neurol Suppl 2. 2007;10:33. [Google Scholar]
- Coffee EM, Yerkes L, Ewen EP, Zee T, Tolan ER. Increased prevalence of mutant null alleles that cause hereditary fructose intolerance in the American population. J Inherit Metab Dis. 2010;33(1):33–42. doi: 10.1007/s10545-009-9008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito G, Imperato MR, Ieno L, Sorvillo R, Benigno V, Parenti G, Parini R, Vitagliano L, Zagari A, Salvatore F. Hereditary fructose intolerance: functional study of two novel ALDOB natural variants and characterization of a partial gene deletion. Hum Mutat. 2010;31(12):1294–1303. doi: 10.1002/humu.21359. [DOI] [PubMed] [Google Scholar]
- Gorospe JR, Singhal BS, Kainu T, Wu F, Stephan D, Trent J, Hoffman EP, Naidu S. Indian Agarwal megalencephalic leukodystrophy with cysts is caused by a common MLC1 mutation. Neurology. 2004;62(6):878–882. doi: 10.1212/01.WNL.0000115106.88813.5B. [DOI] [PubMed] [Google Scholar]
- Lomsadze A, Ter-Hovhannisyan V, Chernoff YO, Borodovsky M. Gene identification in novel eukaryotic genomes by self-training algorithm. Nucleic Acids Res. 2005;33(20):6494–6506. doi: 10.1093/nar/gki937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malay AD, Allen KN, Tolan DR. Structure of the thermolabile mutant aldolase B, A149P: molecular basis of hereditary fructose intolerance. J Mol Biol. 2005;347(1):135–144. doi: 10.1016/j.jmb.2005.01.008. [DOI] [PubMed] [Google Scholar]
- Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic acid Res. 1988;16:1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sali A, Blundell TL. Comparative protein modelling by satisfaction of spatial restraints. J Mol Biol. 1993;234(3):779–815. doi: 10.1006/jmbi.1993.1626. [DOI] [PubMed] [Google Scholar]
- Singhal BS. Leukodystrophies – Indian scenario. Indian J Pediatr. 2005;72(4):315–318. doi: 10.1007/BF02724013. [DOI] [PubMed] [Google Scholar]
- Stanke M, Steinkamp R, Waack S, Morgenstern B (2004) AUGUSTUS: a web server for gene finding in eukaryotes. Nucleic Acids Res 32(Web server issue):W309–W312 [DOI] [PMC free article] [PubMed]
- Steinmann B, Gitzelmann R. The diagnosis of hereditary fructose intolerance. Helv Paediatr Acta. 1981;36:297–316. [PubMed] [Google Scholar]
- Steinmann B, Santer R. Disorders of fructose metabolism. In: Saudubray JM, van den Berghe G, Walter JH, editors. Inborn metabolic disorders – diagnosis and treatment. 5. New York: Springer; 2012. pp. 159–165. [Google Scholar]


