Abstract
Background
LDL cholesterol (LDL-C) is the traditional measure of risk attributable to LDL. Non-HDL-cholesterol (NHDL-C), apolipoprotein B (apoB), and LDL particle number (LDL-P) are alternative measures of LDL-related risk. However, the clinical utility of these measures may only become apparent among individuals for whom levels are inconsistent (discordant) with LDL-C.
Methods and Results
LDL-C was directly measured, NHDL-C was calculated, apoB was measured with immunoassay, and LDL-P with nuclear magnetic resonance spectroscopy among 27,533 healthy women (median follow-up 17.2 years; 1,070 incident coronary events). Participants were grouped by median LDL-C (121 mg/dL) and each of NHDL-C, apoB, and LDL-P. Discordance was defined as LDL-C ≥median and the alternative measure <median, or vice versa. Despite high LDL-C correlations with NHDL-C, apoB, and LDL-P (r=0.910, 0.785, and 0.692, all p<0.0001), prevalence of LDL-C discordance as defined by median cut-points was 11.6%, 18.9%, and 24.3% for NHDL-C, apoB, and LDL-P, respectively. Among women with LDL-C<median, coronary risk was underestimated for women with discordant (≥median) NHDL-C (age-adjusted hazard ratio 2.92, 95% CI 2.33-3.67), apoB (2.48, 2.01-3.07), or LDL-P (2.32, 1.88-2.85), compared to women with concordant levels. Conversely, among women with LDL-C ≥median, risk was overestimated for women with discordant (<median) NHDL-C (0.40, 0.29-0.57), apoB (0.34, 0.26-0.46), or LDL-P (0.42, 0.33-0.53). After multivariable adjustment for potentially mediating factors including HDL cholesterol and triglycerides, coronary risk remained under or overestimated by ≈20-50% for women with discordant levels.
Conclusions
For women with discordant LDL-related measures, coronary risk may be under or overestimated when relying on LDL-C alone.
Clinical Trial Registration Information
ClinicalTrials.gov. Identifier: NCT00000479
Keywords: lipids, lipoproteins, prevention
Current U.S. guidelines recommend measuring a standard lipid panel in adults and targeting lifestyle and lipid lowering therapy based on levels of LDL cholesterol (LDL-C).1, 2 Furthermore, non-HDL cholesterol (NHDL-C), the cholesterol carried by LDL and VLDL particles and calculated as total minus HDL cholesterol, is currently a secondary target of therapy in individuals with hypertriglyceridemia.1 Recent guidelines from Europe,3, 4 Canada,5 as well as recent U.S. consensus statements/recommendations6-9 continue to endorse LDL-C as the primary lipid measure before and after treatment, but acknowledge that NHDL-C or apolipoprotein B (apoB) could be recommended for individuals with hypertriglyceridemia or cardiometabolic abnormalities.
Because a substantial proportion of individuals with “normal” or below average LDL-C experience coronary events,10-12 it has been proposed that some of these individuals are at increased risk as a result of higher concentrations of NHDL-C, apoB, or LDL particles (LDL-P), which may not be readily apparent from their LDL-C values.13 Hence, risk in these individuals may be underestimated based on their LDL-C alone. Conversely, individuals with higher concentrations of LDL-C may have below average NHDL-C, apoB, or LDL-P, and their risk may be overestimated based on LDL-C.
Glasziou et al14 have proposed that when evaluating a new test in relation to an old test, the consequences of the new test are best understood through the disagreements between the old and new tests (discordance analysis). Since there is significant controversy regarding when to use “new tests” such as NHDL-C, apoB, or LDL-P in clinical practice in relation to the “old test” (LDL-C),1, 2 we aimed to examine the prognosis of individuals with discordant values of the new and old tests. In cases where the new and old tests are in agreement (concordant), such individuals may be best suited by either test, and other considerations become important including familiarity of clinicians with the test, widespread availability of the test, or cost considerations.
Prior studies in healthy individuals have suggested that cardiovascular risk may be more closely related to NHDL-C, apoB, or LDL-P compared with LDL-C,15-19 and that this difference is more clinically relevant when levels are discordant.20-22 However, prior studies did not measure all of these parameters nor did they directly measure LDL-C, relying instead on estimating LDL-C values from three other lipid measurements (total cholesterol, triglycerides, and HDL cholesterol) which may also introduce additional measurement error.21, 22 Thus, the aim of this study was to determine the prevalence and long-term prognosis of discordant levels of directly-measured LDL-C compared with NHDL-C, apoB, or LDL-P among 27,533 apparently healthy women followed for over 17 years.
Methods
Study Population
Participants were drawn from the Women’s Health Study (WHS), an on-going prospective cohort including 28,345 initially healthy women.23, 24 Participants were apparently healthy female health care professionals, ages 45 years or older, free of self-reported cardiovascular disease and cancer at study entry. At enrollment, women gave written informed consent and completed questionnaires on demographics, anthropometrics, medical history, and lifestyle factors. Women were also asked whether their mother or father had a myocardial infarction (MI), and parental history of MI before age 60 years was considered premature.25
Of the 27,790 women with baseline lipid measurements, we excluded women with missing values for any of the lipid measurements (N=257) resulting in 27,533 women for analysis. The study was approved by the institutional review board of the Brigham and Women’s Hospital (Boston, Mass).
Laboratory measurements
EDTA blood samples were obtained at enrollment and stored in vapor phase liquid nitrogen (-170° C). In a laboratory certified by the NHLBI/CDC Lipid Standardization program, LDL-C was determined by a homogenous direct method from Roche Diagnostics.26 Total and HDL cholesterol were determined using direct enzymatic colorimetric assays. Triglycerides were measured enzymatically with correction for endogenous glycerol. NHDL-C was calculated as total minus HDL cholesterol. ApoB was measured using an immunoturbidimetric assay (DiaSorin, Stillwater, MN). LDL-P (nmol/L) was measured by nuclear magnetic resonance (NMR) spectroscopy using the Lipo-Profile-3 algorithm at LipoScience, Inc. (Raleigh, NC).27, 28
Ascertainment of Coronary Events
The primary endpoint of interest was incident coronary events (nonfatal MI, percutaneous coronary intervention, coronary artery bypass grafting, or coronary death). Every six months for the first year and annually thereafter, women received follow-up questionnaires about the occurrence of end points. Nonfatal endpoints were based on self-reports from follow-up questionnaires, letters, or telephone calls. For each reported endpoint, we requested permission from the participant to examine the relevant medical records. A copy of the death certificate and additional records were requested as needed. Cases were reviewed by the Endpoints Committee and fulfilled the necessary confirmation criteria.23
Statistical Analysis
Statistical analyses were done using STATA version 10.1. First, we determined medians, 25th, and 75th percentiles for LDL-C, NHDL-C, apoB, and LDL-P. We calculated Spearman rank correlation coefficients (r) for LDL-C with each of NHDL-C, apoB, and LDL-P, and examined them graphically with scatterplots. To examine the extent to which discordance or concordance of LDL-C and these alternative LDL measures was associated with risk, we categorized participants into categories according to < or ≥ median levels of LDL-C (121 mg/dL) and each of NHDL-C (154 mg/dL), apoB (100 mg/dL), and LDL-P (1216 nmol/L). Discordance was defined as LDL-C ≥median and the alternative measure <median, or vice versa. We chose median cut-points to define discordance to make it easier to apply clinically, as there is no physiologic cut-point for discordance. Differences between baseline characteristics of participants across these categories were analyzed using the Kruskal-Wallis rank test for comparing medians and analysis of variance for comparing means of continuous measures. Chi-square tests were used to analyze categorical variables.
We constructed cumulative probability curves for incident coronary events across the categories and tested for differences with the log-rank test. Absolute event rates were calculated per 1000-person-years. Cox proportional hazard models were used to calculate the hazard ratios and 95% confidence intervals (CIs). Age-, minimally-, and fully-adjusted multivariate models were examined. The minimally adjusted models, which did not include other lipid or potentially mediating mechanisms, adjusted for age, randomized treatment assignment, hormone use, postmenopausal status, smoking, and blood pressure. The fully-adjusted models additionally included diabetes, body mass index, HDL cholesterol, triglycerides, high-sensitivity C-reactive protein (hsCRP), and parental history of premature MI.
Finally, we repeated all analyses substituting Friedewald-estimated LDL-C instead of directly-measured LDL-C after excluding the 592 women with triglycerides >400 mg/dL.
All reported p values were two-tailed, and a p value <0.05 was considered statistically significant.
Results
Despite high correlations of LDL-C with NHDL-C, apoB, and LDL-P (Spearman r [95%CI]: 0.910 [0.908-0.912], 0.785 [0.780-0.789], and 0.692 [0.686-0.698], all p<0.0001), the prevalence of LDL-C discordance (as defined by median cut-points) with NHDL-C, apoB, and LDL-P was 11.6%, 18.9%, and 24.3%, respectively (Figure 1). Although most individuals had concordant levels of LDL-C with NHDL-C (Figure 1A, top right and bottom left quadrants), apoB (Figure 1B), or LDL-P (Figure 1C), there were many individuals with discordant levels (top left and bottom right quadrants).
Figure 1.
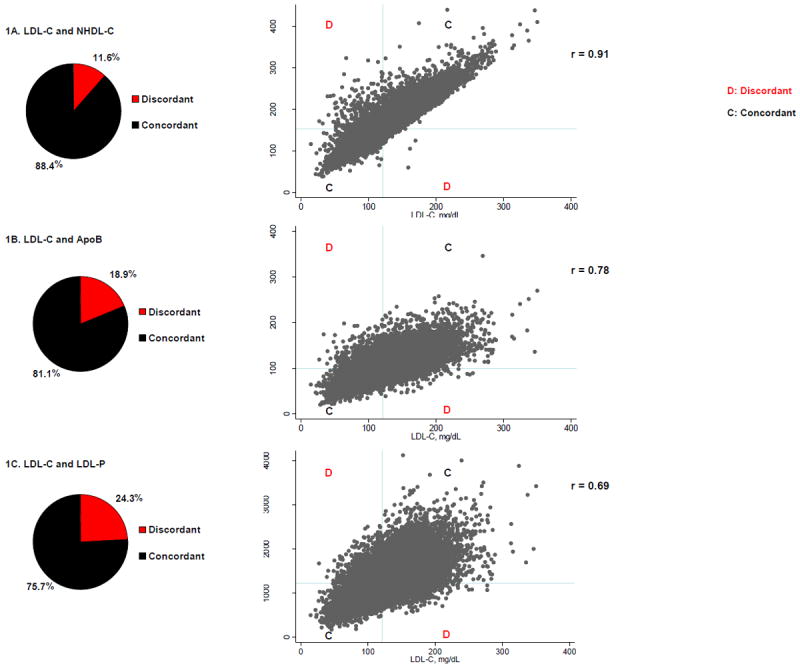
Scatterplots and prevalence of discordance and concordance defined according to median values of LDL-C (x-axis) and each of NHDL-C (1A), apoB (1B), and LDL-P (1C). Median values were for LDL-C 121 mg/dL, NHDL-C 154 mg/dL, apoB 100 mg/dL, and LDL-P 1216 nmol/L.
In order to further characterize the clinical characteristics of individuals with discordant or concordant levels of LDL-C and each of the alternative LDL-related measures, we examined discordant or concordant subgroups according to LDL-C < or ≥ median (Supplemental Tables 1-3). Among discordant individuals, the concentration of LDL-C either under or overrepresented the concentration of NHDL-C, apoB, or LDL-P. As expected, individuals with concordantly low levels of LDL-C and either NHDL-C, apoB, or LDL-P had favorable risk factor profiles. By contrast, unfavorable risk profiles were noted for individuals with LDL-C below median but discordant (above median) levels of either NHDL-C, apoB, or LDL-P. These individuals had elevated triglycerides, low HDL-C, smaller LDL particles that were cholesterol-depleted, in addition to having higher hsCRP and increased BMI compared with the other groups.
Furthermore, as expected, individuals with concordantly high levels of LDL-C and NHDL-C had unfavorable risk factor profiles. By contrast, despite having an LDL-C above median, individuals with discordant (below median) levels of either NHDL-C, apoB, or LDL-P had the lowest prevalence of smoking, hypertension, diabetes, and the lowest BMI and hsCRP. Moreover, these individuals had elevated LDL-C because their LDL particles were larger in size and more cholesterol-enriched, despite having fewer overall number of LDL or apoB particles.
During a median follow-up of 17.2 years, a total of 1,070 incident CHD events occurred. Among the 13,595 women with below median LDL-C, coronary risk was underestimated by three-fold for women whose level of LDL-C was discordant with NHDL-C (age-adjusted HR 2.92, 95% CI 2.33-3.67) compared with being concordant (reference group, Figure 2 and Table 1). Similar underestimation of coronary risk was observed for women with discordant levels of LDL-C with apoB (age-adjusted HR 2.48, 2.01-3.07) or with LDL-P (age-adjusted HR 2.32, 1.88-2.85), all p<0.0001. Coronary risk remained underestimated by ~30-50% after fully adjusting for other known risk factors, including potentially mediating factors such as diabetes, body mass index, HDL cholesterol, triglycerides, and hsCRP.
Figure 2.
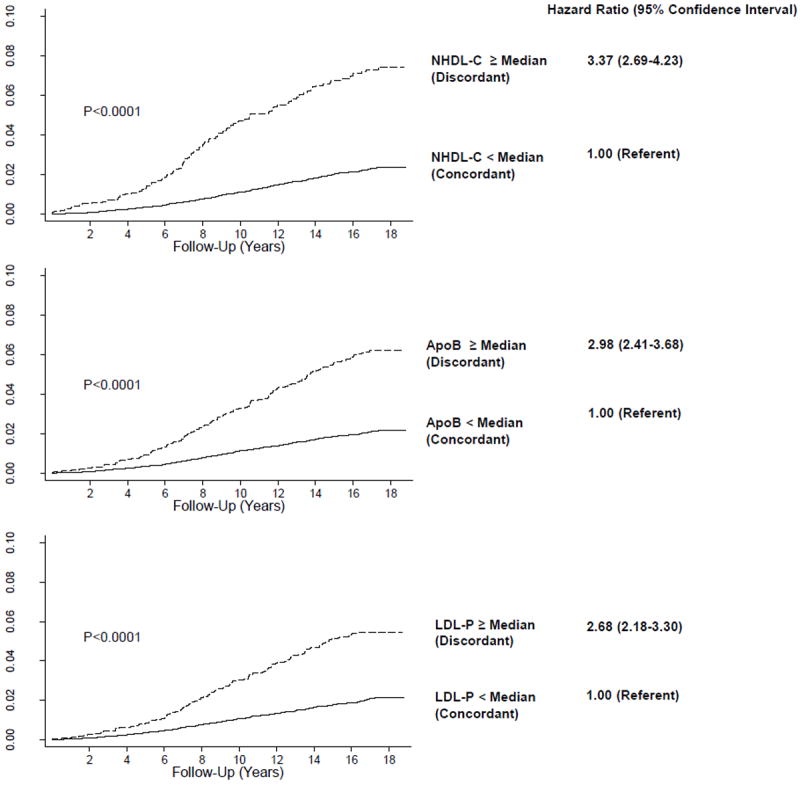
Cumulative probability of incident CHD events among 13,595 women with LDL-C < median (121 mg/dL). As shown, coronary risk is underestimated for women with discordant (≥median) levels of NHDL-C (154 mg/dL), apoB (100 mg/dL), or LDL-P (1216 nmol/L), compared with concordant levels. Hazard ratios and 95% confidence intervals obtained from Cox regression models. P for trend obtained from log-rank test.
Table 1.
Underestimation of coronary risk among women with LDL-C below median but discordant NHDL-C, apoB, or LDL-P (N=13,595)
| NHDL-C < median (Concordant) | NHDL-C ≥ median (Discordant) | P value | |
|---|---|---|---|
| NHDL-C, median (25th-75th percentile), mg/dL | 126 (111-138) | 164 (158-175) | |
| LDL-C, median (25th-75th percentile), mg/dL | 98 (86-109) | 113 (105-118) | |
| No. events/N | 256/12,026 | 106/1,569 | |
| Incidence rate, per 1000 p-y (95% CI) | 1.32 (1.17-1.49) | 4.42 (3.65-5.35) | |
| Age-adjusted HR (95% CI) | 1.00 | 2.92 (2.33-3.67) | <0.001 |
| Minimally-adjusted HR (95% CI) * | 1.00 | 2.37 (1.87-2.99) | <0.001 |
| Fully-adjusted HR (95% CI) † | 1.00 | 1.50 (1.08-2.06) | 0.01 |
|
| |||
| ApoB < median (Concordant) | ApoB ≥ median (Discordant) | ||
|
| |||
| ApoB, median (25th-75th percentile), mg/dL | 81 (71-89) | 112 (106-121) | |
|
| |||
| LDL-C, median (25th-75th percentile), mg/dL | 98 (85-108) | 111 (101-117) | |
|
| |||
| No. events/N | 218/11,033 | 144/2,562 | |
|
| |||
| Incidence rate, per 1000 p-y (95% CI) | 1.22 (1.07-1.40) | 3.63 (3.08-4.27) | |
|
| |||
| Age-adjusted HR (95% CI) | 1.00 | 2.48 (2.01-3.07) | <0.001 |
|
| |||
| Minimally-adjusted HR (95% CI) | 1.00 | 2.06 (1.65-2.56) | <0.001 |
|
| |||
| Fully-adjusted HR (95% CI) | 1.00 | 1.33 (1.01-1.74) | 0.04 |
|
| |||
| LDL-P < median (Concordant) | LDL-P ≥ median (Discordant) | ||
|
| |||
| LDL-P, median (25th-75th percentile), nmol/L | 931 (794-1057) | 1374 (1282-1511) | |
|
| |||
| LDL-C, median (25th-75th percentile), mg/dL | 97 (84-108) | 109 (99-115) | |
|
| |||
| No. events/N | 200/10,341 | 162/3,254 | |
|
| |||
| Incidence rate, per 1000 p-y (95% CI) | 1.20 (1.04-1.37) | 3.20 (2.74-3.73) | |
|
| |||
| Age-adjusted HR (95% CI) | 1.00 | 2.32 (1.88-2.85) | <0.001 |
|
| |||
| Minimally-adjusted HR (95% CI) | 1.00 | 1.95 (1.57-2.41) | <0.001 |
|
| |||
| Fully-adjusted HR (95% CI) | 1.00 | 1.38 (1.07-1.77) | 0.01 |
Minimally-adjusted model included age, treatment assignment, hormone use, postmenopausal status, smoking, blood pressure
Minimally-adjusted model variables plus diabetes, body mass index, HDL cholesterol, triglycerides, high-sensitivity C-reactive protein, parental history of premature myocardial infarction
Median values of LDL-C, NHDL-C, apoB, and LDL-P were 121 mg/dL, 154 mg/dL, 100 mg/dL, and 1216 nmol/L, respectively.
Conversely, for the 13,938 women with above median LDL-C (Figure 3 and Table 2), coronary risk was overestimated by approximately three-fold when their LDL-C levels were discordant with NHDL-C, apoB, or LDL-P. Coronary risk remained overestimated by ~ 20-40% in fully-adjusted models, but this was statistically significant only for discordance of LDL-C with apoB.
Figure 3.
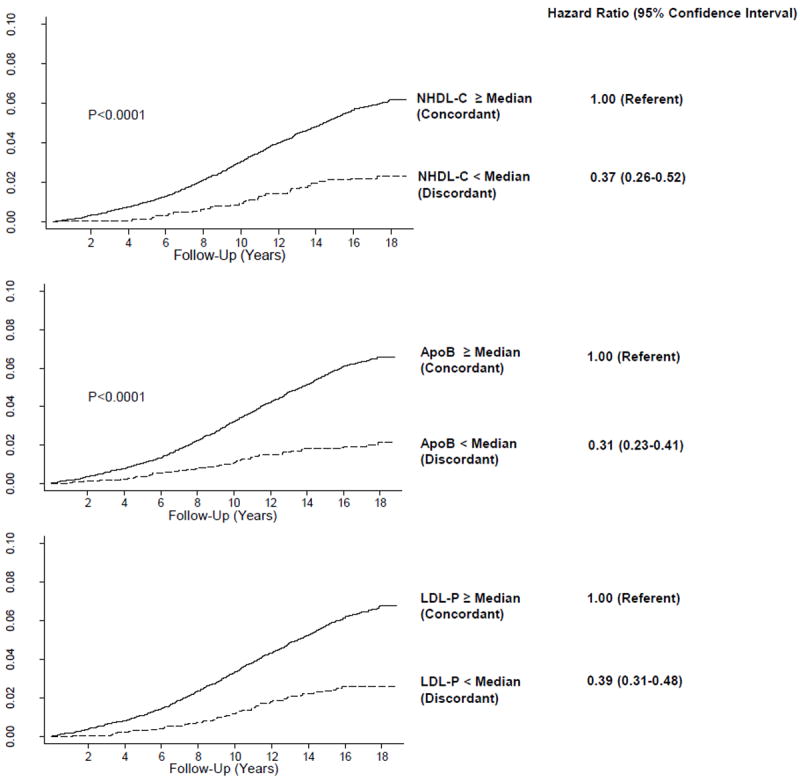
Cumulative probability of incident CHD events among 13,938 women with LDL-C ≥median (121 mg/dL). As shown, coronary risk is underestimated for women with discordant (<median) levels of NHDL-C (154 mg/dL), apoB (100 mg/dL), or LDL-P (1216 nmol/L), compared with concordant levels. Hazard ratios and 95% confidence intervals obtained from Cox regression models. P for trend obtained from log-rank test.
Table 2.
Overestimation of coronary risk among women with LDL-C above median but discordant NHDL-C, apoB, or LDL-P (N=13,938)
| NHDL-C < median (Discordant) | NHDL-C ≥ median (Concordant) | ||
|---|---|---|---|
| NHDL-C, median (25th-75th percentile), mg/dL | 148 (144-151) | 184 (169-207) | |
| LDL-C, median (25th-75th percentile), mg/dL | 126 (123-130) | 148 (135-165) | |
| No. events/N | 34/1,616 | 674/12,322 | |
| Incidence rate, per 1000 p-y (95% CI) | 1.30 (0.93-1.82) | 3.50 (3.25-3.78) | |
| Age-adjusted HR (95% CI) | 0.40 (0.29-0.57) | 1.00 | <0.001 |
| Minimally-adjusted HR (95% CI) * | 0.47 (0.33-0.66) | 1.00 | <0.001 |
| Fully-adjusted HR (95% CI) † | 0.70 (0.47-1.01) | 1.00 | 0.06 |
|
| |||
| ApoB < median (Discordant) | ApoB ≥ median (Concordant) | ||
|
| |||
| ApoB, median (25th-75th percentile), mg/dL | 93 (88-97) | 124 (113-138) | |
|
| |||
| LDL-C, median (25th-75th percentile), mg/dL | 130 (125-139) | 148 (135-166) | |
|
| |||
| No. events/N | 50/2,634 | 658/11,304 | |
|
| |||
| Incidence rate, per 1000 p-y (95% CI) | 1.16 (0.88-1.54) | 3.75 (3.47-4.04) | |
|
| |||
| Age-adjusted HR (95% CI) | 0.34 (0.26-0.46) | 1.00 | <0.001 |
|
| |||
| Minimally-adjusted HR (95% CI) | 0.40 (0.30-0.53) | 1.00 | <0.001 |
|
| |||
| Fully-adjusted HR (95% CI) | 0.59 (0.43-0.82) | 1.00 | 0.001 |
|
| |||
| LDL-P < median (Discordant) | LDL-P ≥ median (Concordant) | ||
|
| |||
| LDL-P, median (25th-75th percentile), nmol/L | 1093 (997-1158) | 1555 (1379-1787) | |
|
| |||
| LDL-C, median (25th-75th percentile), mg/dL | 133 (126-145) | 149 (135-167) | |
|
| |||
| No. events/N | 82/3,430 | 626/10,508 | |
|
| |||
| Incidence rate, per 1000 p-y (95% CI) | 1.48 (1.19-1.84) | 3.83 (3.54-4.14) | |
|
| |||
| Age-adjusted HR (95% CI) | 0.42 (0.33-0.53) | 1.00 | <0.001 |
|
| |||
| Minimally-adjusted HR (95% CI) | 0.48 (0.38-0.61) | 1.00 | <0.001 |
|
| |||
| Fully-adjusted HR (95% CI) | 0.82 (0.63-1.06) | 1.00 | 0.13 |
Minimally-adjusted model included age, treatment assignment, hormone use, postmenopausal status, smoking, blood pressure
Minimally-adjusted model variables plus diabetes, body mass index, HDL cholesterol, triglycerides, high-sensitivity C-reactive protein, parental history of premature myocardial infarction
Median values of LDL-C, NHDL-C, apoB, and LDL-P were 121 mg/dL, 154 mg/dL, 100 mg/dL, and 1216 nmol/L, respectively
When we repeated the analysis for discordance of LDL-C with all three alternative LDL-related measures simultaneously (i.e. NHDL-C, apoB, and LDL-P), the underestimation or overestimation of coronary risk became more pronounced for women with LDL-C discordant with all three measures (Supplemental Table 4).
Alternatively, as some have proposed initial risk assessment with NHDL-C, apoB, or LDL-P instead of LDL-C, we reversed our analysis order and sought to determine the clinical utility of LDL-C as a second lipid measure. As shown (Supplemental Figure A and B), if either NHDL-C, apoB, or LDL-P were obtained as the initial test, then the effect of discordance with LDL-C on coronary risk was negligible.
Additional Analysis with Friedewald LDL-C
When the analyses were repeated using Friedewald-calculated LDL-C (median 127 mg/dL) instead of directly-measured LDL-C, we further excluded the 592 participants with triglycerides >400 mg/dL.26 Among these 26,940 participants, the age-adjusted and minimally-adjusted results were similar to the Table 1 and 2 results obtained using directly-measured LDL-C, whether for women with LDL-C below median or above median. However, among women with Friedewald LDL-C below median, the fully-adjusted HR (95% CI) for discordant NHDL-C was attenuated and no longer significant (1.30, 0.92-1.84, p=0.14), while the fully-adjusted results for discordant apoB (1.45, 1.09-1.92, p=0.01) or discordant LDL-P (1.42, 1.09-1.86, p=0.01) were slightly strengthened and remained statistically significant. Furthermore, in fully-adjusted models, among women with Friedewald LDL-C above median, having discordantly low NHDL-C, apoB, or LDL-P was no longer statistically significant.
Discussion
In this study of apparently healthy women, we observed that the prevalence of discordance defined according to median concentrations of LDL-C with either NHDL-C, apoB, or LDL-P was common, reaching nearly 25 percent for LDL-P. Among discordant individuals, the concentration of LDL-C either under or overrepresented the concentration of NHDL-C, apoB, or LDL-P. Furthermore, among these discordant individuals, coronary risk was also either under or overestimated by LDL-C. These data support the concept that for most individuals with concordant levels of LDL-C and an alternative LDL-related measure (NHDL-C, apoB, or LDL-P), the clinical utility of these measures is similar. However, among the subgroup of individuals (up to a quarter of this population) with discordance of LDL-C with another LDL-related measure, risk may be over or underestimated when relying on LDL-C alone.
Although LDL-C and alternative LDL-related measures are closely correlated, they reflect different aspects of LDL. LDL-P is the number of LDL particles, while LDL-C is the amount of cholesterol carried by these LDL particles. Similarly, apoB is the number of apoB particles (most of which are LDL particles), while NHDL-C is the amount of cholesterol carried by these apoB particles. Mechanistically, the cholesterol content of LDL particles can vary substantially (more than two-fold) across individuals because of differences in particle size as well as the LDL particle’s relative content of cholesterol ester and triglycerides.29 Accordingly, at any particular LDL-C concentration, individuals may have higher or lower concentrations of LDL particles, as reflected in their concentrations of NHDL-C, apoB, or LDL-P. Discordantly high NHDL-C, apoB, or LDL-P generally reflects increased concentrations of smaller, cholesterol-depleted LDL particles which predominate in the presence of high triglycerides, low HDL-C, and insulin resistance. Not surprisingly, the increased risk associated with discordantly high NHDL-C, apoB, or LDL-P in this study was attenuated after adjusting for these traits. However, even after adjustment, systematic underestimation of risk remained substantial for such discordant women.
To our knowledge, this is the first report assessing LDL-C with all three proposed alternative LDL-related measures (NHDL-C, apoB, and LDL-P) in the same population, and to compare them with directly-measured LDL-C. Previously, when discordance analysis was used to compare Friedewald-estimated LDL-C with apoB and NHDL-C among men in the Quebec Cardiovascular Study, results favored apoB and NHDL-C over LDL-C.20 Subsequently, two discordance analyses of Friedewald-estimated LDL-C vs LDL-P were conducted in the Framingham study and the Multi-Ethnic Study of Atherosclerosis, both of which favored LDL-P over LDL-C among discordant individuals.21, 22 Although Friedewald-estimated LDL-C is routinely used for clinical practice, it requires three primary measurements (total cholesterol, HDL cholesterol, and triglycerides), potentially decreasing the accuracy and precision of the derived LDL-C concentration. In our study, we directly measured LDL-C, and thus avoided assay imprecision on this basis.
Additional strengths of our study include its large sample size and long follow-up, which allowed for accrual of an adequate number of events among participants in the subgroups of discordant LDL categories. However, since we studied an apparently healthy cohort of women at low overall risk for CHD events, the current results may not be generalizable to men or other patient groups. Furthermore, our data do not address the question of clinical utility for risk assessment and treatment strategies for higher risk patients, such as those with known CHD, or for the monitoring of patients taking lipid altering therapy. Such studies need to be performed in the appropriate patient settings, preferably within the context of randomized trials of primary or secondary prevention.
Despite following 27,533 women for more than 17 years, our study was not structured to address specific differences between NHDL-C, apoB, and LDL-P; when compared to LDL-C among discordant women, the confidence intervals for all three of these alternative lipid measures overlap each other. However, the proportion of women found to be discordant with each measure varied more than two-fold with the highest rate observed for LDL-P.
In conclusion, among initially healthy women, variations in long-term coronary risk may stem in part from differences between their baseline levels of LDL-C and other LDL-related measures such as NHDL-C, apoB, or LDL-P. For the majority of women with concordant LDL measures, LDL-C has similar clinical utility to NHDL-C, apoB, or LDL-P. But for women with discordant LDL-related measures, coronary risk may be systematically over or underestimated when relying on LDL-C alone. Thus, the current results support the use of alternative lipid testing among such discordant women.
Supplementary Material
Acknowledgments
Funding Sources: The research for this article was supported by grants K08 HL094375 (Dr. Mora) and HL 43851, HL 080467, and CA 47988 from the National Heart, Lung, and Blood Institute and the National Cancer Institute, National Institutes of Health. The funding agencies played no role in the design, conduct, data management, analysis, or manuscript preparation related to this manuscript.
Footnotes
Conflict of Interest Disclosures: Dr Mora has received research grant support from AstraZeneca and Atherotec Diagnostics, served as a consultant for Pfizer, Quest Diagnostics, and Genzyme, and received non-promotional speaker honorarium from Abbott, AstraZeneca, and the National Lipid Association. Dr Buring reports no disclosures. Dr. Ridker has received research grant support from AstraZeneca, Novartis, Amgen, and NHLBI and has served as a consultant to Genzyme, Jannsen, Aegerion, ISIS, Vascular Biogenics, Boeringer, and Merck. Dr. Ridker is listed as a co-inventor on patents held by the Brigham and Women’s Hospital that relate to the use of inflammatory biomarkers in cardiovascular disease that have been licensed to AstraZeneca and Seimens.
References
- 1.Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 2.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, Foster E, Hlatky MA, Hodgson JM, Kushner FG, Lauer MS, Shaw LJ, Smith SC, Jr, Taylor AJ, Weintraub WS, Wenger NK, Jacobs AK. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:e584–636. doi: 10.1161/CIR.0b013e3182051b4c. [DOI] [PubMed] [Google Scholar]
- 3.Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D. ESC/EAS guidelines for the management of dyslipidaemias: The task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) Eur Heart J. 2011;32:1769–1818. doi: 10.1093/eurheartj/ehr158. [DOI] [PubMed] [Google Scholar]
- 4.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F. European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The fifth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2012;33:1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 5.Anderson TJ, Gregoire J, Hegele RA, Couture P, Mancini GB, McPherson R, Francis GA, Poirier P, Lau DC, Grover S, Genest J, Jr, Carpentier AC, Dufour R, Gupta M, Ward R, Leiter LA, Lonn E, Ng DS, Pearson GJ, Yates GM, Stone JA, Ur E. 2012 update of the Canadian Cardiovascular Society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2013;29:151–167. doi: 10.1016/j.cjca.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 6.Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, Witztum JL. Lipoprotein management in patients with cardiometabolic risk: Consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care. 2008;31:811–822. doi: 10.2337/dc08-9018. [DOI] [PubMed] [Google Scholar]
- 7.Contois JH, McConnell JP, Sethi AA, Csako G, Devaraj S, Hoefner DM, Warnick GR. Apolipoprotein B and cardiovascular disease risk: Position statement from the AACC lipoproteins and vascular diseases division working group on best practices. Clin Chem. 2009;55:407–419. doi: 10.1373/clinchem.2008.118356. [DOI] [PubMed] [Google Scholar]
- 8.Davidson MH, Ballantyne CM, Jacobson TA, Bittner VA, Braun LT, Brown AS, Brown WV, Cromwell WC, Goldberg RB, McKenney JM, Remaley AT, Sniderman AD, Toth PP, Tsimikas S, Ziajka PE, Maki KC, Dicklin MR. Clinical utility of inflammatory markers and advanced lipoprotein testing: Advice from an expert panel of lipid specialists. J Clin Lipidol. 2011;5:338–367. doi: 10.1016/j.jacl.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, Dagogo-Jack S, Davidson MB, Einhorn D, Garvey WT, Grunberger G, Handelsman Y, Hirsch IB, Jellinger PS, McGill JB, Mechanick JI, Rosenblit PD, Umpierrez G, Davidson MH. AACE comprehensive diabetes management algorithm 2013. Endocr Pract. 2013;19:327–336. doi: 10.4158/endp.19.2.a38267720403k242. [DOI] [PubMed] [Google Scholar]
- 10.Wald NJ, Hackshaw AK, Frost CD. When can a risk factor be used as a worthwhile screening test? BMJ. 1999;319:1562–1565. doi: 10.1136/bmj.319.7224.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347:1557–1565. doi: 10.1056/NEJMoa021993. [DOI] [PubMed] [Google Scholar]
- 12.Law MR, Wald NJ. Risk factor thresholds: Their existence under scrutiny. BMJ. 2002;324:1570–1576. doi: 10.1136/bmj.324.7353.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barter PJ, Ballantyne CM, Carmena R, Castro Cabezas M, Chapman MJ, Couture P, de Graaf J, Durrington PN, Faergeman O, Frohlich J, Furberg CD, Gagne C, Haffner SM, Humphries SE, Jungner I, Krauss RM, Kwiterovich P, Marcovina S, Packard CJ, Pearson TA, Reddy KS, Rosenson R, Sarrafzadegan N, Sniderman AD, Stalenhoef AF, Stein E, Talmud PJ, Tonkin AM, Walldius G, Williams KM. Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: Report of the thirty-person/ten-country panel. J Intern Med. 2006;259:247–258. doi: 10.1111/j.1365-2796.2006.01616.x. [DOI] [PubMed] [Google Scholar]
- 14.Glasziou P, Irwig L, Deeks JJ. When should a new test become the current reference standard? Ann Intern Med. 2008;149:816–822. doi: 10.7326/0003-4819-149-11-200812020-00009. [DOI] [PubMed] [Google Scholar]
- 15.Shai I, Rimm EB, Hankinson SE, Curhan G, Manson JE, Rifai N, Stampfer MJ, Ma J. Multivariate assessment of lipid parameters as predictors of coronary heart disease among postmenopausal women: Potential implications for clinical guidelines. Circulation. 2004;110:2824–2830. doi: 10.1161/01.CIR.0000146339.57154.9B. [DOI] [PubMed] [Google Scholar]
- 16.Benn M, Nordestgaard BG, Jensen GB, Tybjaerg-Hansen A. Improving prediction of ischemic cardiovascular disease in the general population using apolipoprotein B: The Copenhagen City Heart Study. Arterioscler Thromb Vasc Biol. 2007;27:661–670. doi: 10.1161/01.ATV.0000255580.73689.8e. [DOI] [PubMed] [Google Scholar]
- 17.Ingelsson E, Schaefer EJ, Contois JH, McNamara JR, Sullivan L, Keyes MJ, Pencina MJ, Schoonmaker C, Wilson PW, D’Agostino RB, Vasan RS. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. 2007;298:776–785. doi: 10.1001/jama.298.7.776. [DOI] [PubMed] [Google Scholar]
- 18.Mora S, Otvos JD, Rifai N, Rosenson RS, Buring JE, Ridker PM. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation. 2009;119:931–939. doi: 10.1161/CIRCULATIONAHA.108.816181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar N, Packard CJ, Collins R, Thompson SG, Danesh J. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sniderman AD, St-Pierre AC, Cantin B, Dagenais GR, Despres JP, Lamarche B. Concordance/discordance between plasma apolipoprotein B levels and the cholesterol indexes of atherosclerotic risk. Am J Cardiol. 2003;91:1173–1177. doi: 10.1016/s0002-9149(03)00262-5. [DOI] [PubMed] [Google Scholar]
- 21.Cromwell WC, Otvos J, Keyes MJ, Pencina MJ, Sullivan D, Vasan RS, Wilson PWF, D’Agostino RB. Ldl particle number and risk for future cardiovascular disease in the Framingham Offspring Study - implications for LDL management. J Clin Lipidol. 2007;1:583–592. doi: 10.1016/j.jacl.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Otvos JD, Mora S, Shalaurova I, Greenland P, Mackey RH, Goff DC., Jr Clinical implications of discordance between low-density lipoprotein cholesterol and particle number. J Clin Lipidol. 2011;5:105–113. doi: 10.1016/j.jacl.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, Hennekens CH, Buring JE. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–1304. doi: 10.1056/NEJMoa050613. [DOI] [PubMed] [Google Scholar]
- 24.Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE. Low-dose aspirin in the primary prevention of cancer: The women’s health study: A randomized controlled trial. JAMA. 2005;294:47–55. doi: 10.1001/jama.294.1.47. [DOI] [PubMed] [Google Scholar]
- 25.Sesso HD, Lee IM, Gaziano JM, Rexrode KM, Glynn RJ, Buring JE. Maternal and paternal history of myocardial infarction and risk of cardiovascular disease in men and women. Circulation. 2001;104:393–398. doi: 10.1161/hc2901.093115. [DOI] [PubMed] [Google Scholar]
- 26.Mora S, Rifai N, Buring JE, Ridker PM. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888–894. doi: 10.1373/clinchem.2008.117929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jeyarajah EJ, Cromwell WC, Otvos JD. Lipoprotein particle analysis by nuclear magnetic resonance spectroscopy. Clin Lab Med. 2006;26:847–870. doi: 10.1016/j.cll.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Mora S. Advanced lipoprotein testing and subfractionation are not (yet) ready for routine clinical use. Circulation. 2009;119:2396–2404. doi: 10.1161/CIRCULATIONAHA.108.819359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sacks FM, Campos H. Clinical review 163: Cardiovascular endocrinology: Low-density lipoprotein size and cardiovascular disease: A reappraisal. J Clin Endocrinol Metab. 2003;88:4525–4532. doi: 10.1210/jc.2003-030636. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


