Abstract
Introduction
Orthodontic bands cause periodontal inflammation. In theory, the use of a buccal tube (bond) instead of a band should prevent or minimize periodontal changes because the bonds are positioned away from the gingival margins.
Objective
The primary aim of this study was to investigate the periodontal status of orthodontic bands compared with bonds in the first three months of orthodontic treatment.
Materials and methods
Twenty-four orthodontic patients (mean age = 12.6 years) were enrolled in this Randomized Controlled Trial (RCT). Using the cross-mouth technique, bands and bonds were used in opposite quadrants. Periodontal parameters including the presence or absence of Bleeding On Probing (BOP) and Probing Depths (PDs) were taken at the start and three months into treatment.
Results
Bands caused a statistically significant change in the Bleeding On Probing (BOP) (P = 0.001 and 0.021) and bonds displayed a statistically insignificant change in the Bleeding On Probing (BOP) (P = 0.125 and 1.00) for the upper and lower arch. The difference in Probing Depths (PDs) between bands and bonds was also statistically significant (P = 0.001).
Conclusion
Molar bands are associated with greater periodontal inflammation compared with molar bonds in the first three months of fixed orthodontic treatment.
Keywords: Periodontal parameters, Fixed appliances, Orthodontic bands, Orthodontics buccal tubes
1. Introduction
The effects of using orthodontic bands or orthodontic bonded attachments on periodontal disease have been investigated. Gingival inflammation and hyperplasia may occur quickly after the placement of a fixed appliance such as orthodontic bands (Baer and Cocarro, 1964; Zachrisson and Zachrisson, 1971; Kloehn and Pfeifer, 1974; Sandere, 1999; Naranjo et al., 2006), and the development of these problems appears to occur more frequently in interproximal sites and more commonly in posterior teeth compared with anterior teeth (Zachrisson, 1976).
Four possible reasons may cause this phenomenon (increase in the gingival inflammation associated with orthodontic bands) (Atack et al., 1996). First, orthodontic bands mechanically irritate gingival tissues. Second, chemical irritation may occur due to the cement used to retain the band, which is in close proximity to the gingival tissues. Third, a greater risk of food impaction and hence posterior gingival and periodontal irritation may occur. Finally, patients may have a tendency to clean their anterior teeth more effectively than their posterior teeth.
A trial (Boyd and Baumrind, 1992) assessed the difference between banded and bonded teeth regarding plaque accumulation, gingival inflammation and loss of attachment. In this trial, no significant differences were observed in gingival inflammation between maxillary and mandibular banded and bonded teeth during the pre-treatment phase. However, during the course of the treatment, both maxillary and mandibular banded teeth showed significantly greater plaque accumulation and gingival inflammation than the bonded molars. In addition, three months after the removal of the fixed appliance, the banded maxillary molars continued to show greater levels of gingival inflammation and loss of attachment compared with the bonded molars.
Researchers have also investigated supra- and subgingival plaque associated with bands in more detail. An early study (Diamanti-Kipioti et al., 1987) evaluated the changes occurring in the subgingival microflora in children following the placement of orthodontic bands. The samples were collected from subgingival plaque, and the patients were followed up for a period of four months. The results showed an increase in the percentage of black-pigmented Bacteroides in these children.
Another study (Huser et al., 1990) conducted a clinical trial in which the clinical and microbiological parameters of the test sites where the orthodontic bands were fitted were compared with the control sites where no bands were fitted. The authors showed that an increase in the percentage of spirochetes, motile rods, filaments and fusiform occurred in the group with the bands compared with the group with no bands. An impressive three-year longitudinal study using specific culture methods demonstrated that young orthodontic patients harbor Actinobacillus actinomycetemcomitans to a significantly greater extent than matched controls (Paolantonio et al., 1997).
Overall, the added advantages of using bonds and not bands are as follows: (1) maintaining a large stock of various sized bands is unnecessary; (2) a separation appointment is not needed and (3) the extensive pain associated with the separation visit does not occur (Ngan et al., 1994). Therefore, every effort should be made to prevent or at least reduce these potential treatment effects of bands, especially in medically compromised individuals (Burden et al., 2001 and National Institute for Health and Clinical Excellence, 2013). Therefore, the aim of this study was to compare the changes in the clinical periodontal parameters associated with banding and bonding teeth during orthodontic treatment.
2. Materials and methods
The North Somerset and South Bristol Research Ethics Committee in the UK granted ethics committee approval for the present study. Twenty-four consecutive patients, 12 females and 12 males, aged 11–14 years [Mean (SD) age = 12.6 ± 1.01 years] about to begin orthodontic treatment with fixed appliances were included in the study. The age group was chosen to obtain a homogenous sample of patients likely to have similar oral hygiene practice and no potential age-related differences in oral flora.
Exclusion criteria included patients requiring arch expansion or distalization of molars with auxiliary appliances because these additional appliances may interfere with oral hygiene practices. Furthermore, patients with systemic diseases and patients on antibiotics for less than three months before the start of treatment were excluded to not disturb the oral flora, which may influence the results.
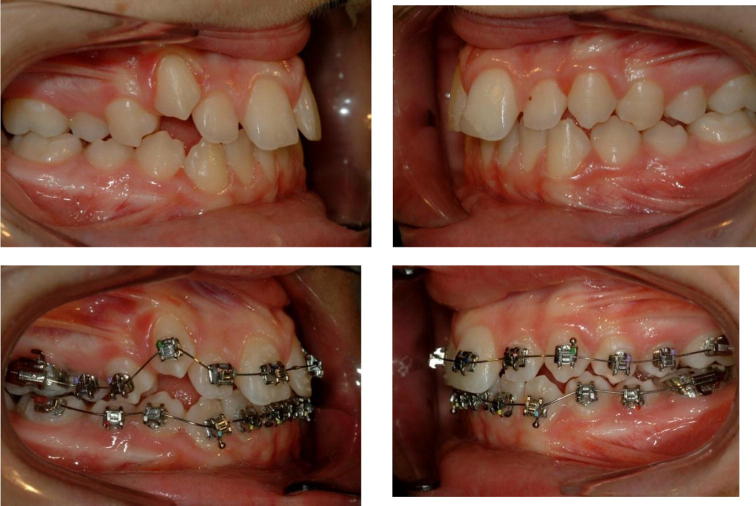
The selected participants and their parents were provided information about the study, and informed consent was obtained. This study was a cross mouth controlled clinical trial, and the randomization was performed using a random number table and sealed envelopes (Fig. 1). This randomization permitted the assignment of molar bands and bonded molar tubes to opposing contra-lateral quadrants of the mouth (Fig. 2); therefore, in this cross-quadrant design, each patient was his/her own control. Clinical assessment of periodontal health, including the presence or absence of Bleeding On Probing (BOP, Lang et al., 1986) and Probing Depth (PD) measurements using UNC15 Probe (Hu-Friedy, Chicago, IL, USA), was taken at the start of treatment (T0) and three months into treatment (T3) (Kalkwarf et al., 1986). PDs were recorded to the total sulcus depth at two points (mesial and distal) on the buccal surface of the molars using the interproximal technique. The two buccal measurements from each tooth were added to provide a total value.
Figure 1.
A diagram showing the random number table and a system of sealed envelopes to ensure the randomisation process in this cross mouth trial.
Figure 2.
Clinical photographs of one of the subjects illustrating the assignment of molar bands and bonded molar tubes to opposing contra-lateral quadrants of the mouth. At the start of treatment, T0 (Top) and three months into treatment, T3 (Bottom).
3. Results
3.1. BOP
A statistically significant increase in the BOP between T0 and T3 for bands was observed, and a slight but not statistically significant reduction in BOP for bonds from T0 to T3 was detected (Table 1). The changes in BOP in the lower arch were similar to the upper arch (Table 2). The bands showed a significant increase in BOP from the start of treatment to three months into treatment. The bond values in the lower arch were very similar at T0 and T3, and the change was not statistically significant. In summary, bands were associated with an increase in BOP in both the upper and lower arches in the first three months of treatment; however, in comparing bonds to bands, no statistically significant difference was observed.
Table 1.
BOP of banded and bonded molars for the upper arch at the start of treatment (T0) and at three months into treatment (T3).
| Time | Percentage | Number | McNemar P value | |
|---|---|---|---|---|
| Bands | T0 | 12.5 | 3 | 0.001 |
| T3 | 83.3 | 20 | ||
| Bonds | T0 | 12.5 | 3 | 0.125 |
| T3 | 4.2 | 1 | ||
Table 2.
BOP for banded and bonded molars for the lower arch at (T0) and (T3).
| Time | Percentage | Number | McNemar P value | |
|---|---|---|---|---|
| Bands | T0 | 16.7 | 4 | 0.021 |
| T3 | 50 | 12 | ||
| Bonds | T0 | 16.7 | 4 | 1.00 |
| T3 | 20.8 | 5 | ||
3.2. PDs
A statistically significant increase was observed in the mean PD values in banded teeth between the start of treatment and three months into treatment (Table 3). The difference in the PD in bonded teeth at the start of treatment compared with three months into treatment was not statistically significant; however, the difference in the means between the banded/bonded molars was statistically significant.
Table 3.
Mean and 95% confidence intervals of the mean change in total buccal probing depth per patient on molar teeth with bands at (T0) and (T3).
| Mean change | 95% CI | t | P | ||
|---|---|---|---|---|---|
| Probing depths on bands at (T3) to (T0) |
1.61 | 0.593 | 2.62 | 3.28 | 0.003 |
| Probing depths on bonds at (T3) to (T0) |
0.478 | 0.461 | 1.41 | 1.05 | 0.302 |
| Difference in probing depths Bands vs. Bonds |
1.31 | 0.95 | 3.21 | 3.83 | 0.001 |
4. Discussion
Plaque retention surrounding orthodontic appliances leads to enamel decalcification and periodontal disease (Davies et al., 1991); therefore, the employment of mechanics that facilitate oral hygiene measures performed by the patients to reduce plaque accumulation is important. In this study and in agreement with several previous clinical trials (Zachrisson, 1976; Boyd and Baumrind, 1992; Huser et al., 1990), bands have been shown to cause statistically significantly more bleeding when probing the buccal surfaces of the upper and lower molars compared with bonded molar tubes (Tables 1 and 2). This finding clearly demonstrates that bands cause statistically more BOP than bonds, which may be explained by factors such as the mechanical irritation caused by bands (Atack et al., 1996), which are likely to be in contact with the gingival margin. Furthermore, this band-mediated effect caused may be due to the chemical irritation caused by the band cement material, the greater likelihood of posterior food impaction and the tendency to brush more effectively anteriorly rather than posteriorly (Kilicoglu et al., 1997).
The changes in PDs were also different between bands and bonds. The mean increase in PDs per patient was 1.61 and 0.478 for bonded and banded molars, respectively (Table 3). A previous study assessed fifteen subjects, and the investigators recorded several clinical parameters (plaque index, BOP and PDs) and collected plaque samples from test and control sites at 7, 12, 47, 71 and 90 days after the beginning of orthodontic treatment (Huser et al., 1990). The authors demonstrated a statistically significant increase in the plaque index and BOP and a small increase in the PDs in the test sites over three months.
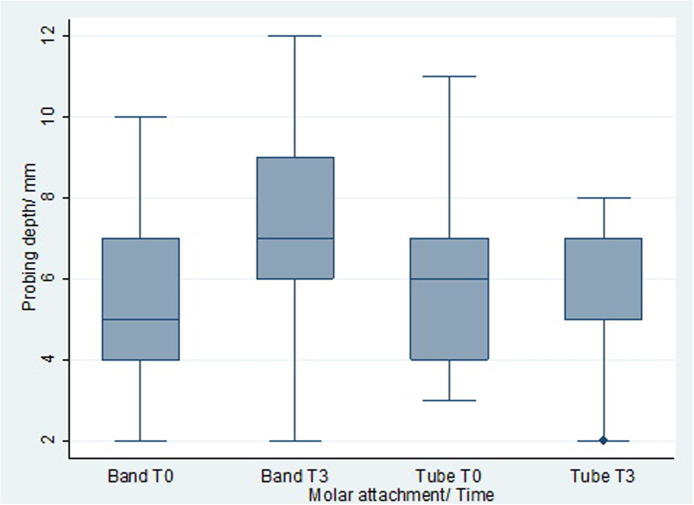
In the current study, the PDs significantly increased in the banded teeth and did not significantly change in bonded teeth. The changes per tooth were approximately half of the values per patient; therefore, for teeth with bands, the average increase in PD was approximately 0.8 mm (Fig. 3). This modest average increase in PD over three months may primarily be due to “false pocketing”. Bonded tubes are more distant from the gingival tissues and may contribute to the minimal change in PDs observed in bonded teeth. A clinical and microbiological study showed that an increase in pocket PD occurred following tooth banding; however, the plaque index and gingival index remained unaffected (Diamanti-Kipioti et al., 1987). Overall, the authors concluded that subgingivally placed orthodontic bands changed the subgingival ecosystem.
Figure 3.
Box and whisker plots of total buccal probing depth (mm) for molar bands vs. molar tubes (bonds) at times (T0) and (T3).
As stated above, the increase in PD in banded teeth may be significantly affected by false pocketing rather than true pocketing. Indeed, an early study suggested that gingival hyperplasia dramatically diminished within forty-eight hours following appliance removal and continued to decrease during the first four months of retention (Kloehn and Pfeifer, 1974). This finding suggests that these changes may be short term and that true pocketing in adolescent patients undergoing treatment employing fixed appliances rarely occurs. Nevertheless, in our study, only the data collected over three months were analyzed, and the results do not support or refute the effects of orthodontic treatment on long term periodontal health.
A longitudinal study compared the periodontal status of bonded and banded teeth before, during and after treatment with fixed appliances (Boyd and Baumrind, 1992). During treatment, both maxillary and mandibular teeth showed significantly greater gingival inflammation and plaque accumulation compared with the bonded molars. Although the specific measures of gingival inflammation differed from the present study, these results are supported by the findings of our study. Similar long term conclusions have also been made by other studies (Polson et al., 1988; Sadowsky and BeGole, 1981).
Weaknesses of this study include not examining subgingival plaque like in several studies (Slots and Listgarten, 1988; Socransky et al., 1998), and sophisticated mechanisms were not employed such as electron microscopy (Sukontapatipark et al., 2001). However, the evidence obtained using the designated clinical parameters of this study supports previous findings. Therefore, this present study has demonstrated that bands are associated with a greater increase in gingival inflammation and PDs than bonds; however, the long term effects of both bands and bonds have not yet been evaluated. Orthodontic bands may play a role in contemporary orthodontics when headgear or rapid maxillary expansion is used. Nevertheless, bonds display clear advantages over the use of bands and do not involve any additional appointments for separation and pain associated with separation (Ngan et al., 1994). Furthermore, bonds may benefit several medical conditions in which maintaining a good standard of oral hygiene is important during treatment (Burden et al., 2001). Although the recommendations involving antibiotic use to treat endocarditis have recently changed (National Institute for Health and Clinical Excellence, 2013), taking any known steps to reduce potential bacteremia during dental treatment is advised.
5. Conclusions
The results of this study show that in the early stages of orthodontic treatment, molar bands are associated with more BOP and an increase in PDs compared with molar bonds. This study is a pilot, and the short term effects were analyzed; however, the long term effects should be elucidated in future studies.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgment
I would like to thank Dr. Nigel Harradine and Mrs. Hazel Taylor from the University of Bristol for their help in this research.
Footnotes
Peer review under responsibility of King Saud University.
References
- Atack N.E., Sandy J.R., Addy M. Periodontal and microbiological changes associated with the placement of orthodontic appliances. A review. J. Periodontol. 1996;67:78–85. doi: 10.1902/jop.1996.67.2.78. [DOI] [PubMed] [Google Scholar]
- Baer P.N., Cocarro J. Gingival enlargement coincident with orthodontic therapy. J. Periodontol. 1964;35:436–439. [Google Scholar]
- Boyd R.L., Baumrind S. Periodontal implications in the use of bonds or bands on molars in adolescents and adults. Angle Orthod. 1992;62:117–126. doi: 10.1043/0003-3219(1992)062<0117:PCITUO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Burden D., Mullally B., Sandler J. Orthodontic treatment of patients with medical disorders. Eur. J. Orthod. 2001;23:363–372. doi: 10.1093/ejo/23.4.363. [DOI] [PubMed] [Google Scholar]
- Davies T.M., Shaw W.C., Addy M., Dummer P., Kingdon A. The effect of orthodontic treatment on plaque and gingivitis. Am. J. Orthod. Dentofacial Orthop. 1991;99:155–162. doi: 10.1016/0889-5406(91)70118-G. [DOI] [PubMed] [Google Scholar]
- Diamanti-Kipioti A., Gusberti F.A., Lang N.P. Clinical and microbiological effects of fixed orthodontic appliances. J. Clin. Periodontol. 1987;14:326–333. doi: 10.1111/j.1600-051x.1987.tb00979.x. [DOI] [PubMed] [Google Scholar]
- Huser M.C., Baehni P.C., Lang R. Effects of orthodontic bands on microbiological and clinical parameters. Am. J. Orthod. Dentofacial Orthop. 1990;97:213–218. doi: 10.1016/S0889-5406(05)80054-X. [DOI] [PubMed] [Google Scholar]
- Kalkwarf K.L., Kaldahl W.B., Patil K.D. Comparison of manual and pressure-controlled periodontal probing. J. Clin. Periodontal. 1986;57(8):467–471. doi: 10.1902/jop.1986.57.8.467. [DOI] [PubMed] [Google Scholar]
- Kilicoglu H., Yildirim M., Polater H. Comparison of the effectiveness of two types of toothbrushes on oral hygiene of patients undergoing orthodontic treatment with fixed appliances. Am. J. Orthod. Dentofacial Orthop. 1997;111:591–594. doi: 10.1016/s0889-5406(97)70309-3. [DOI] [PubMed] [Google Scholar]
- Kloehn J.S., Pfeifer J.S. The effect of orthodontic treatment on the periodontium. Angle Orthod. 1974;44:127–134. doi: 10.1043/0003-3219(1974)044<0127:TEOOTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Lang N.P., Joss A., Orsanic T., Gusberti F.A., Siegrist B.E. Bleeding on probing. A predictor for the progression of periodontal disease? J. Clin. Periodontol. 1986;13(6):590–596. doi: 10.1111/j.1600-051x.1986.tb00852.x. [DOI] [PubMed] [Google Scholar]
- Naranjo A.A., Trivino M.L., Jaramillo A., Betancourth M., Botero J.E. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am. J. Orthod. Dentofacial Orthop. 2006;130(275):17–275. doi: 10.1016/j.ajodo.2005.10.022. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence, 2013. Prophylaxis against infective endocarditis. [PubMed]
- Ngan P., Wilson S., Shanfeld J., Amini H. The effect of ibuprofen on the level of discomfort in patients undergoing orthodontic treatment. Am. J. Orthod. Dentofacial Ortho. 1994;106:88–95. doi: 10.1016/S0889-5406(94)70025-7. [DOI] [PubMed] [Google Scholar]
- Paolantonio M. Clinical significance of Actinobacillus actinomycetemcomitans in young individuals during orthodontic treatment. J. Clin. Periodontol. 1997;24:610–617. doi: 10.1111/j.1600-051x.1997.tb00237.x. [DOI] [PubMed] [Google Scholar]
- Polson A.M. Long-term periodontal status after orthodontic treatment. Am. J. Orthod. Dentofacial Orthop. 1988;93:51–58. doi: 10.1016/0889-5406(88)90193-x. [DOI] [PubMed] [Google Scholar]
- Sadowsky C., BeGole E. Long-term effects of orthodontic treatment on periodontal health. Am. J. Orthod. Dentofacial Orthop. 1981;80:156–172. doi: 10.1016/0002-9416(81)90216-5. [DOI] [PubMed] [Google Scholar]
- Sandere N.L. Evidence-based care in Orthodontics and Periodontics. J. Am. Dent. Assoc. 1999;130:521–527. doi: 10.14219/jada.archive.1999.0246. [DOI] [PubMed] [Google Scholar]
- Slots J., Listgarten M.A. Bacteroides gingivalis, Bacteroides intermedius and Actinobacillus actinomycetemcomitans in human periodontal diseases. J. Clin. Periodontol. 1988;15:85–93. doi: 10.1111/j.1600-051x.1988.tb00999.x. [DOI] [PubMed] [Google Scholar]
- Socransky S.S. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998;25:134–144. doi: 10.1111/j.1600-051x.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- Sukontapatipark W. Bacterial colonisation associated with fixed orthodontic appliances. A scanning electron microscopy study. Eur. J. Orthod. 2001;23:475–484. doi: 10.1093/ejo/23.5.475. [DOI] [PubMed] [Google Scholar]
- Zachrisson B.U. Cause and prevention of injuries to teeth and supporting structures during orthodontic treatment. Am. J. Orthod. Dentofacial Orthop. 1976;69:285–300. doi: 10.1016/0002-9416(76)90077-4. [DOI] [PubMed] [Google Scholar]
- Zachrisson B.U., Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Scand. J. Dent. Res. 1971;79:394–401. doi: 10.1111/j.1600-0722.1971.tb02028.x. [DOI] [PubMed] [Google Scholar]