Abstract
Tracheal bronchus is a rare anatomic variant in which a bronchus originates from the trachea. Patients may be asymptomatic or present with a variety of respiratory symptoms. We present a case of a patient who presented with a history of poorly controlled asthma and a persistent abnormality of the flow-volume loop. Bronchoscopy revealed a tracheal bronchus with narrowed right-sided bronchial orifices. An unrecognized tracheal bronchus may result in serious complications during elective or emergent endotracheal intubation. Spirometry testing may reveal abnormalities of the flow-volume loop associated with altered airflow. Relying on spirometric values without assessing the shape of the flow-volume loop may lead to misdiagnosis and inappropriate management of lung pathology.
Keywords: Flow-volume loop, Spirometry, Tracheal bronchus
Introduction
Correct assessment of the flow-volume loop morphology is a requisite component of spirometry interpretation. Classic flow-volume loop shapes have been described for obstructive and restrictive lung pathology as well as for certain anatomic abnormalities. Identification of an unusual pattern by spirometry may lead to an alternate diagnosis and a change in management.
Case presentation
A 33 year old female was referred to the outpatient Respirology clinic for further management of poorly controlled asthma. She had had persistent symptoms of wheezing and cough since early childhood. Her past medical history included a hemicolectomy for ulcerative colitis, chronic sinusitis, and gastroesophageal reflux. She had been intubated three times, once emergently in the intensive care unit and twice electively for general anesthetic, with no complications. She had had no hospital admissions for her respiratory symptoms. She was an ex-smoker with a seven pack year history. There was a history of limitation in activity due to dyspnea along with nocturnal symptoms of cough and wheeze. She denied a history of recurrent lung infections.
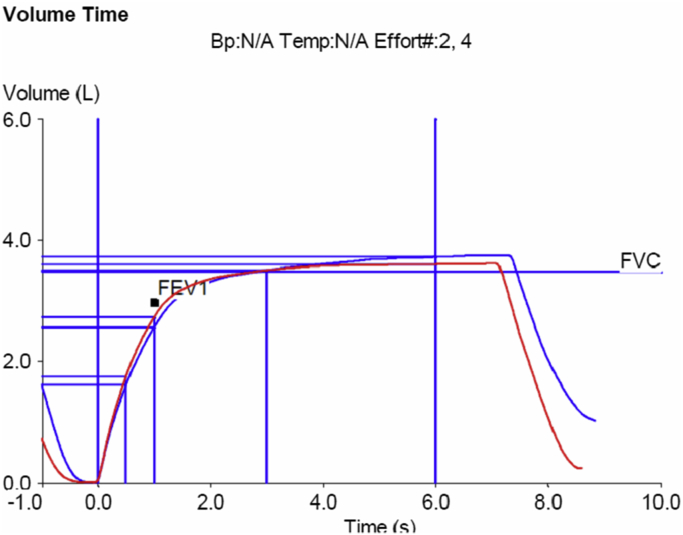
Physical examination revealed normal vital signs including a room air oxygen saturation of 96%. Her respiratory exam was unremarkable. Spirometry was performed. Both the expiratory and inspiratory phases were abnormal (Fig. 1). The inspiratory curve demonstrated mild plateauing. There was a reduction in the initial peak expiratory flow. The expiratory slope was less steep than in flow-volume loops from normal patients. Near end-expiration, the flow rate increased. This pattern was consistently found on repeated spirometric maneuvers. Post-bronchodilator forced expiratory volume in one second (FEV1) was 2.73 L (92% predicted), forced vital capacity (FVC) was 3.64 L (105% predicted), and FEV1/FVC was 0.75. There was no significant bronchodilator response. Previous spirometry tests were reviewed and this flow-volume abnormality was found on all tests, although it had not been reported. The finding prompted re-examination of the patient's previous chest radiographs, which had been interpreted as normal. However, upon review, a complete right upper lobe bronchus was seen originating from the trachea (Fig. 2). Bronchoscopy was performed, confirming the right-sided tracheal bronchus (Fig. 3). The orifice of the tracheal bronchus and the right mainstem bronchus were narrowed. Computerized tomography (CT) scan of the chest was performed for an unrelated indication. Curved multiplanar reformatted images demonstrated the true right tracheal bronchus (Fig. 4).
Fig. 1.
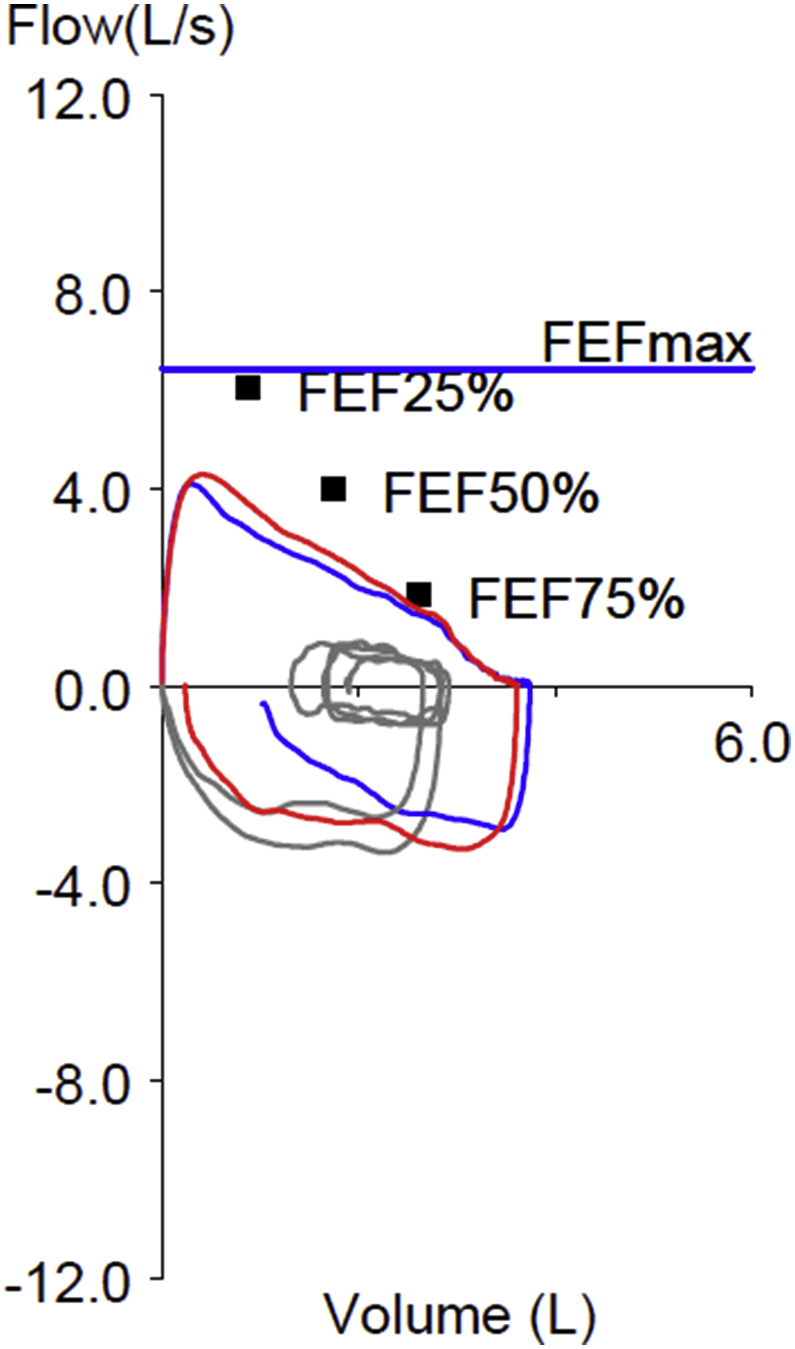
Patient's flow-volume loop demonstrating abnormalities in the inspiratory and expiratory limbs. There was no significant difference between pre- (blue) and post- (red) bronchodilator curves. The black squares represent the predicted expiratory flows (25%, 50%, 75%) for this patient. The predicted maximum forced expiratory flow is represented by the blue horizontal line.
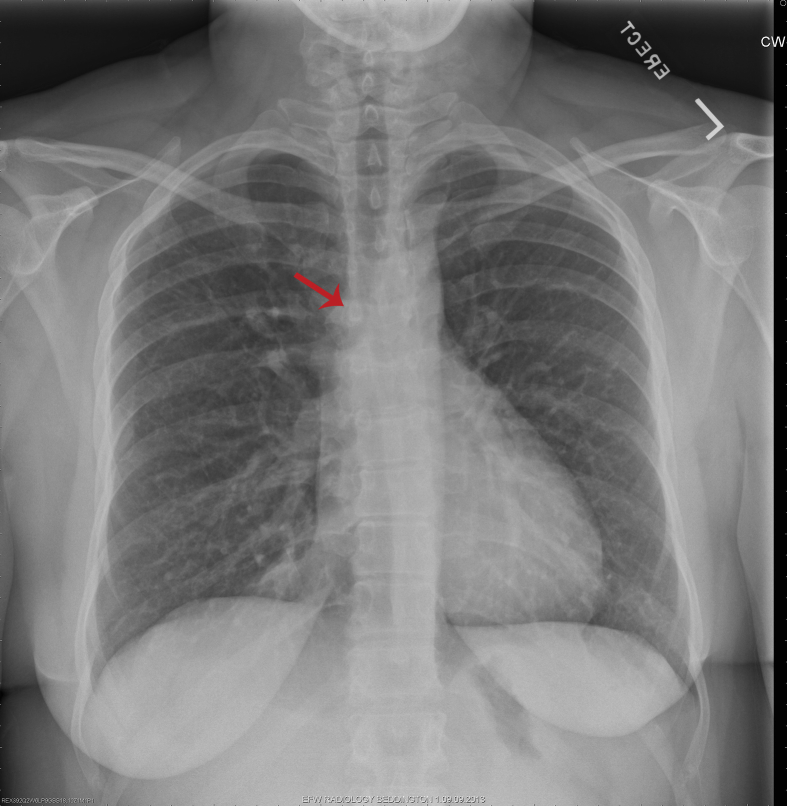
Fig. 2.
Chest X-ray demonstrating the right tracheal bronchus (red arrow pointing at bronchial orifice).
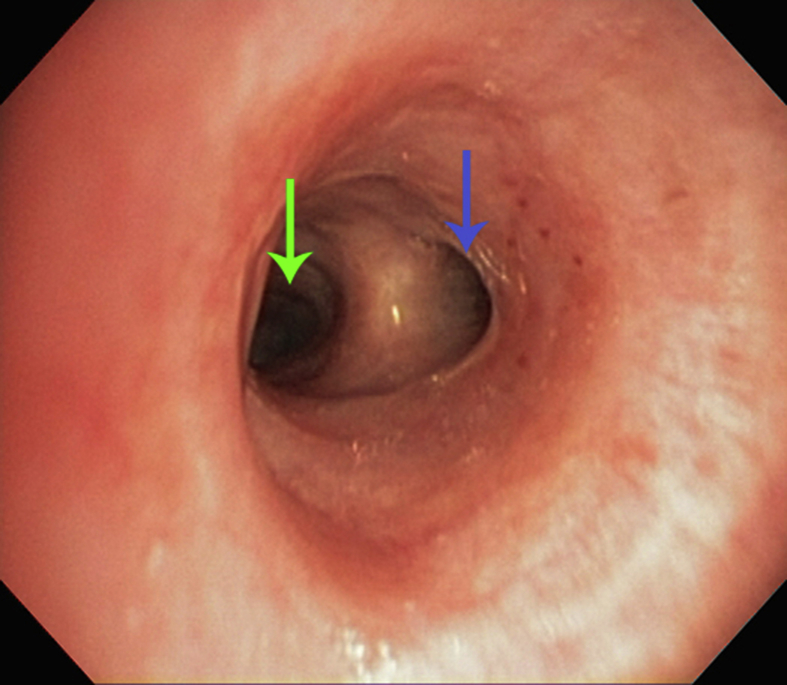
Fig. 3.
Right tracheal bronchus (blue arrow) taking off proximally to the right mainstem bronchus (green arrow).
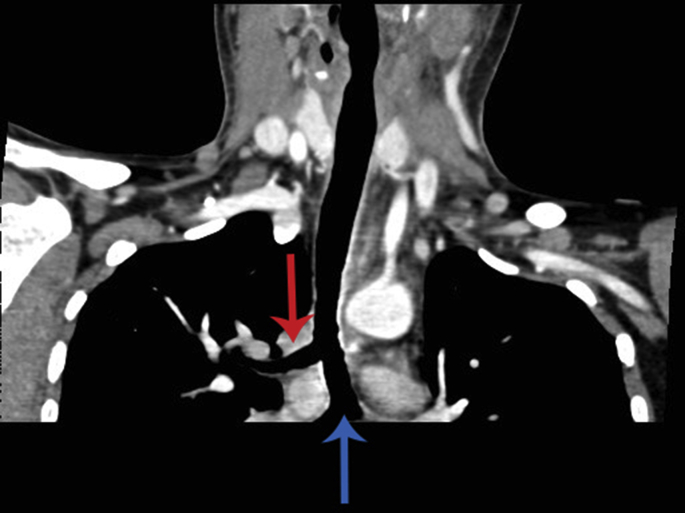
Fig. 4.
Curved multiplanar reformatted images from the patient's computerized tomography demonstrated the right tracheal bronchus (red arrow) proximal to the carina (blue arrow).
Discussion
Tracheal bronchus describes various bronchial abnormalities originating from the trachea or main bronchus [1]. Right tracheal bronchus has a prevalence estimated at 0.1–2% in bronchoscopic reports, and are more common than left sided anomalies [2,3]. A complete right upper lobe bronchus originating from the trachea, referred to as a true right tracheal bronchus or “pig bronchus”, is less common than other forms with an estimated prevalence of 0.2% [1]. Patients with a tracheal bronchus may be asymptomatic but have also been reported to present with dyspnea, persistent cough or wheeze mimicking asthma or COPD, recurrent pneumonias, bronchiectasis, or hemoptysis. An unrecognized tracheal bronchus may result in serious complications during elective or emergent endotracheal intubation if the bronchus is excluded by the endotracheal tube or, less commonly, if the tracheal bronchus itself is intubated, excluding the rest of the lung. This has lead to persistent hypoxemia, atelectasis, or lung collapse during intubation [4,5]. Tracheal bronchi may be found incidentally on investigations performed for other indications, or unexpectedly as an explanation for symptoms that had been attributed to more common respiratory conditions.
No classic shape has been described for the flow-volume loop in tracheal bronchus. We found one case report of spirographic abnormalities associated with a tracheal bronchus [6]. The spirogram showed a straighter initial expiratory phase suggestive of main airways obstruction [6]. Unfortunately, no flow-volume loop was provided for comparison with our result. In our case, the volume–time curve demonstrated the same pattern (Fig. 5). The expiratory limb recorded in our patient appears to have two distinct rates of flow, an initial, reduced rate, followed by a near normal slope at the end of the exhalation.
Fig. 5.
Volume–time curve demonstrating a slight reduction in the initial expiratory phase. There was no significant difference between pre (blue) and post (red) bronchodilator curves.
The subtle plateauing of the inspiratory limb is likely related to the proximal location of the narrowed tracheal bronchus to the thoracic inlet. The shape of the expiratory limb of our patient's spirogram may be attributed to the narrowing of the orifice of the tracheal bronchus and right mainstem bronchus that was seen on bronchoscopy. During forced expiration, the elevated pleural pressures reduce airway diameter, resulting in a degree of airflow obstruction. Given the proximal displacement of the tracheal bronchus relative to the right mainstem bronchus, the reduction in expiratory flow as the narrowed right-sided bronchi approach their smallest size, will occur at different times and explain the reduced slope in the expiratory curve.
The patient's symptoms of exertional dyspnea, wheeze, and cough, have been described in other patients with a unilaterally stenosed mainstem bronchus. These symptoms are likely manifestations of large airway obstruction, and can be mistaken for asthma if analysis of the flow-volume loop has not been performed [7,8]. A similar case to ours involving a patient who was found to have distal tracheal stenosis and a tracheal bronchus has been previously presented by Hosker et al. [6]. This patient presented with obstructive symptoms and evidence of main airways obstruction on spirometry. The evaluating team postulated that the patient's wheeze and exertional breathlessness were more fully explained by the coexisting tracheal stenosis than the presence of the tracheal bronchus [6]. This conclusion is supported by the observation that many tracheal bronchi are incidental findings on imaging performed for other reasons and are asymptomatic [9]. Thus, our patient's clinical presentation may be better explained by the component of narrowing of the right-sided major bronchi rather than the tracheal bronchus itself. It is possible that for a tracheal bronchus to have a symptomatic presentation, it must be accompanied by an additional abnormality such as abnormal drainage leading to recurrent infection or stenosis leading to obstructive symptoms.
Relying on spirometric values without assessing the shape of the flow-volume loop may lead to misdiagnosis and inappropriate management of lung pathology. Case reports describe patients who have been treated unsuccessfully as asthmatics, with multiple medications and often systemic steroids, when further examination of the flow-volume loop morphology led to additional investigations and alternate diagnoses [10,11].
Our case highlights the importance of close review of abnormal flow-volume loops, especially in patients who have suboptimal response to usual medications. Although our patient had a clinical diagnosis of asthma, the response to conventional medical therapy was suboptimal. Furthermore, the shape of the expiratory portion of the flow-volume loop suggested additional pathology. Although the patient had been intubated three times without complication, the discovery of the displaced tracheal bronchus may have clinical implications for further endotracheal tube insertions. In addition, the patient's bronchial anatomy may contribute to respiratory symptoms which had previously been attributed to asthma. The morphology of the flow-volume loop should be examined closely to ensure consistency with the patient's diagnosis. Further investigation with imaging or bronchoscopy may be useful in patients with an abnormal flow-volume loop and symptoms refractory to usual medical therapy.
References
- 1.Ghaye B., Szapiro D., Fanchamps J., Dondelinger R. Congenital bronchial abnormalities revisited. Radiographics. 2001;21:105–119. doi: 10.1148/radiographics.21.1.g01ja06105. [DOI] [PubMed] [Google Scholar]
- 2.Ritsema G.H. Ectopic right bronchus: indications for bronchography. AJR Am J Roentgenol. 1983;140:671–674. doi: 10.2214/ajr.140.4.671. [DOI] [PubMed] [Google Scholar]
- 3.Lee D., Kim Y., Kim H., Lim S. Right upper lobe tracheal bronchus: anesthetic challenge in one-lung ventilated patients – a report of three cases. Korean J Anesthesiol. 2013;64(5):448–450. doi: 10.4097/kjae.2013.64.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Sullivan B., Frassica J., Rayder S. Tracheal bronchus: a cause of prolonged atelectasis in intubated children. Chest. 1998;113(2):537–540. doi: 10.1378/chest.113.2.537. [DOI] [PubMed] [Google Scholar]
- 5.Pribble C., Dean J. An unusual cause of intraoperative hypoxemia. J Clin Anesth. 1994;6:247–249. doi: 10.1016/0952-8180(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 6.Hosker H., Clague H., Morritt G. Ectopic right upper lobe bronchus as a cause of breathlessness. Thorax. 1987;42:473–474. doi: 10.1136/thx.42.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seccombe L.M., Polley L., Rogers P.G., Ing A.J. All that wheezes is not asthma: the value of curves. Thorax. 2012;67:564–565. doi: 10.1136/thoraxjnl-2011-201097. [DOI] [PubMed] [Google Scholar]
- 8.Mazzei J.A., Barro A., Mazzei M.E., Portas T., Esteva H. Biphasic flow volume curve due to obstruction of main bronchus by bronchogenic cyst. Respir Med CME. 2011;4:116–118. [Google Scholar]
- 9.Dave M.H., Gerber A., Bailey M., Gysin C., Hoeve H., Hammer J. The prevalence of tracheal bronchus in pediatric patients undergoing rigid bronchoscopy. J Bronchol Interv Pulmonol. 2014;21(1):26–31. doi: 10.1097/LBR.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 10.Ravenna F., Caramori G., Panella G., Papi A., Benea G., Adcock I.M. An unusual case of congenital short trachea with very long bronchi mimicking bronchial asthma. Thorax. 2002;57:372–373. doi: 10.1136/thorax.57.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozkaya S., Sengul B., Hamsici S., Findik S., Sahin U., Gumus A. Right sided arcus aorta as a cause of dyspnea and chronic cough. Multidiscip Respir Med. 2012;7(1) doi: 10.1186/2049-6958-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]