Abstract
Automated Implantable Cardioverter Defibrillators (AICD), simply known as an Implantable Cardioverter Defibrillator (ICD), has been used in patients for more than 30 years. An Implantable Cardioverter Defibrillator (ICD) is a small battery-powered electrical impulse generator that is implanted in patients who are at a risk of sudden cardiac death due to ventricular fibrillation, ventricular tachycardia or any such related event. Typically, patients with these types of occurrences are on anticoagulant therapy. The desired International Normalized Ratio (INR) for these patients is in the range of 2–3 to prevent any subsequent cardiac event. These patients possess a challenge to the dentist in many ways, especially during oral surgical procedures, and these challenges include risk of sudden death, control of post-operative bleeding and pain.
This article presents the dental management of a 60 year-old person with an ICD and concomitant anticoagulant therapy. The patient was on multiple medications and was treated for a grossly neglected mouth with multiple carious root stumps. This case report outlines the important issues in managing patients fitted with an ICD device and at a risk of sudden cardiac death.
Keywords: Cardioverter Defibrillator, Arrhythmia, Warfarin, Dental extraction, INR
1. Introduction
Automated Implantable Cardioverter Defibrillators (AICDs) or otherwise simply known as Implantable Cardioverter Defibrillators (ICDs) have been in use for more than 30 years. An ICD is a small battery-powered electrical impulse generator that is implanted in patients who are at a risk of sudden cardiac death due to ventricular fibrillation and ventricular tachycardia (Roedig et al., 2010). ICDs are widely used in patients with malignant ventricular tachyarrhythmias and prevention of sudden cardiac death (Washizuka et al., 2005). ICD devices are also utilized to treat Brugada syndrome, and the devices were found to provide full protection against sudden death related to primary ventricular fibrillation (Cappato et al., 2012). Pacemaker or ICD implantation among patients receiving anticoagulant therapies is a common occurrence (Bernard et al., 2012). The device is programed to detect cardiac arrhythmia and correct the condition by delivering a jolt of electricity (Theodotou et al., 2009). ICD definitively reduces the incidence of sudden cardiac death in younger patients on optimal medical therapy; however, whether the elderly population derives similar benefits remains unknown (Revenco et al., 2011). Maintaining anticoagulation increases the risk of bleeding complications for most operative procedures, whereas discontinuing anticoagulant therapy over a period of time may increase the risk of thromboembolic complications (Bernard et al., 2012). Patients with cardiovascular disease constitute risk cases in dental practice, particularly in the absence of adequate medical controls (Steinhauer et al., 2005); therefore, dentists must understand the medical problems of each individual patient, the treatments received, and the potential dental treatments. The aim of presenting this case report is to outline the important issues when dealing with patients who present the risk of sudden cardiac death, who are fitted with an ICD device and who receive warfarin therapy.
2. Case report
A 60 year-old Saudi male patient was referred from the Interns’ clinic, College of Dentistry, King Saud University. The patient reported to the Special Care Dentistry clinic within the Maxillofacial Surgery Department in the College of Dentistry, King Saud University with a grossly neglected mouth. The patient had many decayed and missing teeth (Fig.1) and was unable to obtain proper dental consultation and treatment due to his complex medical history. Recently, he experienced pain and tenderness in the lower right posterior area of his mouth. The patient is married, living with his family and a non-smoker. He had previously undergone a few dental procedures in the past such as extractions, and he brushes occasionally with a fluoridated tooth paste.
Figure 1.

Oral health status of the patient at the initial visit.
The patient was on treatment and follow up for multiple medical conditions, including anterior wall myocardial infarction and a left ventricular (LV) apical clot with peripheral vascular lower limb embolism 10 years ago. The patient was hospitalized in July 2010 with a significant coronary artery disease and left ventricular dysfunction (LV failure), which was due to a large organized LV apical clot that caused shortness of breath. After cardiac catheterization, the patient was diagnosed with Ischemic Heart Disease (IHD), Acute Left Ventricular Failure (LVF) and New York Heart Association Class III (NYHA III) Heart Failure. Subsequently, the insertion of a subcutaneous Implantable Cardioverter Defibrillator (ICD) was necessitated. Although the patient was stable, he was categorized with NYHA III heart failure with a high risk of cardiac sudden death 5 months prior to his first dental visit to our department.
The patient is being followed up at the King Fahad Cardiac Centre, King Khalid University Hospital (KKUH), King Saud University, Riyadh. The patient is taking warfarin, and the desired therapeutic range for his International Normalized Ratio (INR) is 2–3. Blood investigations including INR and adjustment of warfarin dosage are performed every 2–3 weeks. The patient presented with laboratory investigation reports from the warfarin clinics at KKUH 1 week prior to his first dental appointment. The patient had been taking warfarin 4 mg once daily for the last few weeks; however, his dosage had been increased to 4.5 mg to achieve the target INR. Other than warfarin, the patient was on 20 mg Simvastatin, 6.25 mg Carvedilol and 81 mg Aspirin once daily.
A treatment plan was formulated for the patient during an initial consultation with his physician regarding the effect of dental treatment on his general health. A referral to anticoagulation clinics for INR regularization was arranged. The patient was given assurance, education and motivation for oral hygiene. Extraction of the lower right third molar and the remaining roots with the potential risks was explained to the patient. Subsequently, restoration of the upper right central incisor as well as realistic treatment options for prosthetic rehabilitation of missing teeth were discussed with the patient.
2.1. Summary at the initial visit
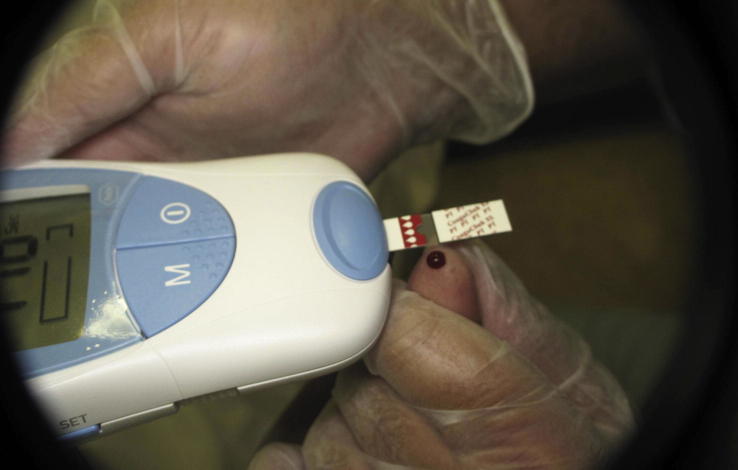
A Dental Panaromic Tomograph (DPT) (Fig. 2) and periapical radiographs of the lower right third molar and the upper right central incisor were taken. On the spot INR was performed using the CoaguChek apparatus, and the reading was 4.2 (Fig. 3). A pulp vitality test for the lower right third molar revealed irreversible pulpitis.
Figure 2.
OPG revealing the dental status and bone.
Figure 3.
On Spot INR testing with CoaguChek apparatus.
The patient was reassured of his situation and oral hygiene instructions were provided. The treatment plan was discussed with the patient, including possible alternatives and problems that may arise during the course of treatment. Consulting the anticoagulation clinics at KKUH for regulation of INR was recommended to the patient because the INR level (INR 4.2) was higher than the target level (INR 2–3) as well as higher than the level considered safe (INR 4) for any dental intervention (Perry et al., 2007). Furthermore, the patient was told that he would need a thorough maintenance of his oral hygiene due to the impact of any dental intervention on his underlying medical condition. The patient was instructed to bring the complete medical report during his next visit and was given a referral letter to be discussed with his physician at KKUH. The patient was advised to take a Paracetamol tablet for pain because Ibuprofen, which is a non-steroidal anti-inflammatory drug (NSAID), could lead to a possible interaction with warfarin (Hakonsen et al., 2009).
2.2. Subsequent visits
After revisiting the anticoagulation clinics at KKUH, the warfarin dosage for the patient was reverted to 4 mg for 1 week. The patient brought a letter from the medical specialist describing his condition and advising care to be taken during the dental treatment. No absolute contraindication was indicated for the proposed dental treatment. The patient did not require antibiotic prophylaxis for his cardiac condition as per the National Institute for Health and Clinical Excellence (NICHE) guidelines March-2008 (Stokes et al., 2008). Caries excavation was performed for the upper right central incisor, and temporary restoration was placed with a Dycal (calcium hydroxide cement) base. All procedures were performed using a stress reduction protocol and the patient was monitored throughout the treatment.
2.3. Follow up visits
Permanent restoration was performed on the upper central incisor using a glass ionomer cement base and was restored with composite. All root stumps were extracted sequentially with care. INR was conducted at each visit using the CoaguChek device. In total, 9 teeth were extracted in four visits. At first, the mobile remaining root stumps of tooth numbers 18 and 16 involving the upper right posterior quadrant were extracted. At this visit, the INR checked with CoaguChek was 2.07. All regional blocks were avoided, and a combination of Prilocaine + felypressine (Citanest 3%-Octapressin) was used as a local anesthetic of choice. Surgicel was used as a hemostatic agent for post-operative bleeding control and the wounds were sutured using Vicryl 3-0 absorbable sutures.
The patient was given verbal as well as written post-operative instructions for the use of a 4.8 % Tranexamic acid mouthwash (10 ml for 2 min in the mouth, 4–5 times a day for 3–5 days). In case of any complication or excessive post-operative bleeding, the patient was advised to attend the clinic or contact an oral surgeon on call by phone. Instructions for post-operative eating and mouth cleaning were given and the patient was asked to follow up after 1 week. Remaining root stumps of other quadrants were extracted according to the order of their mobility. During the next three visits (each a week apart), tooth numbers 13, 12, 21, 23, 24, 36 and 48 were extracted. First, the teeth in the right upper anterior quadrant were extracted then the left upper and lower quadrant teeth were extracted at the same time and lastly, tooth number 48 in the lower right posterior quadrant was extracted. Each appointment was kept as short as possible to not stress the patient. None of these appointments lasted more than 45 min including the post-operative measures and instructions. The patient’s INR was recorded at each visit with CoaguChek (Fig. 3), and the INR was found to be 2.04, 2.6 and 2.4, respectively. During extractions, the patient was continuously monitored with the help of a pulse oximeter. Topical anesthesia and local infiltration anesthesia (Prilocaine + felypressine (Citanest 3%-Octapressin) were used except for the lower right third molar on the last visit in which a careful Infra alveolar nerve block was used with a technique that minimizes chances of an intravascular injection (Khalil, 2014). A similar post-operative care was delivered as during previous visits, and Surgicel packs were used as hemostatic agents. The same post-operative instructions were given, including the use of Tranexamic acid mouth wash. The patient returned at each visit with an uneventful report, except for a minor oozing of blood. Moreover, the patient-reported post-operative pain was rated on a scale of 10, and the patient was recalled after 3 weeks.
2.4. Recall visit
The patient returned on the scheduled appointment, and his post-operative healing was uneventful with minimal post-operative pain and bleeding. The reported pain after the last extraction was more than the previous extractions; however, the tissue healing was progressing as expected. The patient desired to have an implant or undergo fixed prosthodontic rehabilitation for the lost teeth; however, these options were not feasible due to his medical condition. The patient agreed to receive a removable partial denture in both arches, and impressions were made of both the upper and lower jaws. Using a bite registration and re-confirmatory approach, the upper and lower partial dentures were fabricated. The patient was ultimately satisfied with the achieved occlusion and esthetics (Fig. 4).
Figure 4.

Patient satisfied with the final result and esthetics.
3. Discussion
3.1. Stress reduction protocol
Dentists are required to obtain a detailed medical history of patients with ICD. The presence of any signs of cardiac arrhythmia should be carefully evaluated and the patient’s physician should always be consulted. Stress reduction protocols should be implemented in all patients to reduce the risk of cardiovascular effects caused by stress during dental treatment. Stress reduction protocols involve the establishment of a good rapport with the patient, suitable appointment times and duration, successful local anesthesia and sedation if necessary (Steinhauer et al., 2005). The dental session should be kept as short as possible and should be terminated if the patient develops any signs or symptoms of being tired or cannot tolerate the procedure (Wraith, 1999). The patient was monitored with a pulse oximeter during the dental procedure to detect any changes in heart beat rate and oxygen saturation; however, no sedation was deemed necessary for the patient. Any complex dental procedure must be explained very clearly to the patients and can be discussed at several appointments to reduce patient stress.
3.2. The use and selection of local anesthetic
The stimulation of excessive amounts of adrenaline from the body and the use of external adrenaline in the local anesthetic solution may produce life threatening arrhythmias in several patients (Campbell et al., 1996). The use of local anesthetics in patients with ICD should be carefully evaluated. Local anesthetics should be used with caution, dose should be minimized and patients should be continuously monitored. In addition, excessive amounts of vasoconstrictor should be avoided. The most commonly used vasoconstrictor with lidocaine as the local anesthetic is adrenaline. Adrenaline can induce multiple changes in the cardiovascular dynamic system (Malamed, 2012). With our patient, to avoid any complications related to adrenaline, the combination of prilocaine and felypressine (Citanest 3%-Octapressin) was used as the local anesthetic. Effective pain control during and after dental treatment is important in such patients because the dental treatment may trigger cardiovascular changes and risk the development of arrhythmias (Jowett and Cabot, 2000). Aspiration is important during the local anesthetic injection to avoid intravascular injections, which are associated with many systemic complications (Malamed, 2012). If the dentist needs to use a nerve block, many techniques have been described in the literature as modifications of the conventional inferior alveolar nerve block to minimize the risk of intravascular injections (Khalil, 2014), such as injection at the retromolar area and the pterygomandibular space (Okamoto et al., 2000; Suazo Galdames et al., 2008). Moreover, all regional blocks were avoided in this case except the infra alveolar nerve block for the lower right third molar, which was firm and needed more adequate anesthetic control. Local infiltration was preferred to avoid chances of bleeding into the tissue spaces, particularly the lingual spaces. During oral surgical procedure preparation, the incision and tissue manipulation were reported to cause maximum changes in the heart rate and ECG waves (Miller et al., 1998). Care was exercised during the extraction of the root stumps to avoid any bone cutting and excessive tissue manipulation during the procedure (Fig. 5).
Figure 5.

Careful tissue manipulation during oral surgery for the patient.
3.3. Dental and surgical devices
Patients with fitted cardiac devices that control heart function are at a risk of any electrical devices used in dentistry. Several dental devices such as electrosurgery and ultrasonic scalers may interfere with the implanted defibrillator (Roedig et al., 2010), and several devices such as an electrical pulp tester, amalgamator, electric tooth brush, and curing light may not cause any interference with implantable devices such as the pacemaker (Miller et al., 1998). No significant event was observed when using the curing light for restoration of the anterior upper tooth.
3.4. Effect of warfarin
Many patients with ICD undergo anticoagulant therapy for their original event. Warfarin, which is the most commonly used oral anticoagulant drug, is a vitamin K antagonist that is rapidly absorbed one hour after ingestion and possess a half-life of 36 h. Extraction and several other dental procedures should be performed after evaluation of the patient’s International Normalized Ratio (INR) (Richards, 2008). The INR therapeutic range is 2.0–3.0 for most regimens and in several other conditions 3.0–4.0 is advised, like for patients with mechanical heart valves or recurrent episodes of emboli (Ishibashi et al., 1996). A theoretical risk of post-operative bleeding appears to be minimal because hemorrhages can be controlled by local hemostatic measures, avoiding thromboembolism, which may occur after anticoagulant therapy withdrawal (Kudsi et al., 2012). In our case, the INR therapeutic range was between 2 and 3. Dental surgical procedures can be safely performed up to INR levels of 4 (Barrett, 2004; Balevi, 2010; Perry et al., 2007). However, the patient reported an INR of 4.2 during the initial visit, thus needing readjustment of warfarin therapy. Furthermore, INR should be confirmed on the day of procedure (Karsli et al., 2011). With the help of CoaguChek, the patient's INR was monitored on the spot (Fig. 3). Local measures after dental surgical procedures are valuable to control bleeding. In our patient, bleeding control was achieved with local hemostatic agents (Surgicel), resorbable suturing and tranexamic acid mouth wash. Moreover, NSAID analgesics such as Ibuprofen was avoided for post-operative pain control; instead, a combination of Paracetamol and Codeine Phosphate tablets was prescribed.
3.5. Antibiotic prophylaxis
Prophylactic antibiotics are not recommended to be used in patients with ICDs before dental treatment according to the American Heart Association guidelines and the National Institute for Health and Clinical Excellence UK (NICE guidelines UK 2008) (Baddour et al., 2010, 2011). The risk of developing device-related infection in patients with ICD is considered low; therefore, antibiotic prophylaxis is not needed for these types of patients (Baddour et al., 2010). The patient was not advised to receive any antibiotic prophylaxis during the course of the treatment.
3.6. Prosthetic management options
The prosthodontic rehabilitation of patients with ICD has always been a challenge to prosthodontists and general practitioners because of uncontrolled post-operative bleeding. Recently, the dental implant placement has been a preferred choice as the prosthetic replacement because patients primarily prefer fixed prostheses compared with removable prostheses (Diz et al., 2013). The risk of implant surgery has restricted the treatment option for ICD patients, and high mortality rates have been shown in ICD patients compared with normal cardiac patients (Zareba et al., 2003). Fluctuating INR has also been of concern regarding dental surgical procedures (Tompkins et al., 2010). The risk of post-operative bleeding and the mortality rate of patients during surgical dental procedures have been documented (Steinhauer et al., 2005). Oral anti-coagulant treatment such as warfarin and prophylactic doses of aspirin in patients with ICD may need regular monitoring and change in doses, which may affect post-operative bleeding (Al-Khadra, 2003). In the above discussed case, the patient preferred the fixed prostheses; however, the fluctuating INR, physician concern, patient’s oral hygiene and periodontal condition only allowed the removable prostheses options. For example, dental implants were questionable because the OPG revealed progressive bone loss (Fig. 2), and the patient was satisfied with the rehabilitation results (Fig. 3). Further follow up visits are scheduled for this patient.
Such medically compromised patients experience a lot of inconveniences until they receive proper care, which can provide the patients with better oral health status. Although the systemic disease or condition can be intimidating, a detailed history, proper consultation and careful monitoring can make the case clear and manageable.
Conflict of interests
The authors declare no conflict of interests.
Ethical approval and patient’s consent
After obtaining an informed consent from the patient, ethical approval was granted from College of Dentistry Research Council (CDRC), College of Dentistry, King Saud University.
Acknowledgment
The authors would like to thank the Ex Director of Clinics, Dr. Sulieman AlJohany for procurement of the CoaguChek apparatus at the College of Dentistry, King Saud University.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Khadra A.S. Implantation of pacemakers and implantable cardioverter defibrillators in orally anticoagulated patients. Pacing Clin. Electrophysiol. 2003;26(1 Pt 2):511–514. doi: 10.1046/j.1460-9592.2003.00084.x. [DOI] [PubMed] [Google Scholar]
- Baddour L.M., Epstein A.E., Erickson C.C., Knight B.P., Levison M.E., Lockhart P.B. Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation. 2010;121(3):458–477. doi: 10.1161/CIRCULATIONAHA.109.192665. [DOI] [PubMed] [Google Scholar]
- Baddour L.M., Epstein A.E., Erickson C.C., Knight B.P., Levison M.E., Lockhart P.B. A summary of the update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. J. Am. Dent. Assoc. 2011;142(2):159–165. doi: 10.14219/jada.archive.2011.0058. [DOI] [PubMed] [Google Scholar]
- Balevi B. A decision-tree analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010;110:691–697. doi: 10.1016/j.tripleo.2010.03.018. [DOI] [PubMed] [Google Scholar]
- Barrett D. Management of dental patients on warfarin therapy in a primary care setting. Dent. Update. 2004;31(10):618. [PubMed] [Google Scholar]
- Bernard M.L., Shotwell M., Nietert P.J., Gold M.R. Meta-analysis of bleeding complications associated with cardiac rhythm device implantation. Circ. Arrhythm. Electrophysiol. 2012;5(3):468–474. doi: 10.1161/CIRCEP.111.969105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell J.H., Huizinga P.J., Das S.K., Rodriguez J.P., Gobetti J.P. Incidence and significance of cardiac arrhythmia in geriatric oral surgery patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1996;82(1):42–46. doi: 10.1016/s1079-2104(96)80376-3. [DOI] [PubMed] [Google Scholar]
- Cappato R., Smith W.M., Hood M.A., Crozier I.G., Jordaens L., Spitzer S.G. Subcutaneous chronic implantable defibrillation systems in humans. J. Interv. Card. Electrophysiol. 2012;34(3):325–332. doi: 10.1007/s10840-012-9665-6. [DOI] [PubMed] [Google Scholar]
- Diz P., Scully C., Sanz M. Dental implants in the medically compromised patient. J. Dent. 2013;41(3):195–206. doi: 10.1016/j.jdent.2012.12.008. [DOI] [PubMed] [Google Scholar]
- Hakonsen G.D., Pettersen M.H., Skurtveit S., Giverhaug T. Concomitant use of warfarin, analgesics and anti-inflammatory agents. Tidsskr. Nor. Laegeforen. 2009;129(12):1217–1220. doi: 10.4045/tidsskr.08.0127. [DOI] [PubMed] [Google Scholar]
- Ishibashi Y., Aoki H., Ohba J., Kamikubo Y., Morimoto K., Kumasaka A. PT-INR as a parameter for anticoagulant therapy after valve replacement surgery. Kyobu Geka. 1996;49(11):906–908. [PubMed] [Google Scholar]
- Jowett N.I., Cabot L.B. Patients with cardiac disease: considerations for the dental practitioner. Br. Dent. J. 2000;189(6):297–302. doi: 10.1038/sj.bdj.4800750. [DOI] [PubMed] [Google Scholar]
- Karsli E.D., Erdogan O., Esen E., Acarturk E. Comparison of the effects of warfarin and heparin on bleeding caused by dental extraction: a clinical study. J. Oral Maxillofac. Surg. 2011;69(10):2500–2507. doi: 10.1016/j.joms.2011.02.134. [DOI] [PubMed] [Google Scholar]
- Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth. Essays Res. 2014;8(1):3–8. doi: 10.4103/0259-1162.128891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudsi Z., Dalati M.H., Sibai L., Koussayer L.T. Management of bleeding disorders in the dental practice: managing patients on anticoagulants. Dent. Update. 2012;39(5):358–360. doi: 10.12968/denu.2012.39.5.358. 363. [DOI] [PubMed] [Google Scholar]
- Malamed S. sixth ed. Mosby; 2012. Handbook of Local Anesthesia. [Google Scholar]
- Miller C.S., Leonelli F.M., Latham E. Selective interference with pacemaker activity by electrical dental devices. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998;85(1):33–36. doi: 10.1016/s1079-2104(98)90394-8. [DOI] [PubMed] [Google Scholar]
- Okamoto Y., Takasugi Y., Moriya K., Furuya H. Inferior alveolar nerve block by injection into the pterygomandibular space anterior to the mandibular foramen: radiographic study of local anesthetic spread in the pterygomandibular space. Anesth. Prog. 2000;47(4):130–133. [PMC free article] [PubMed] [Google Scholar]
- Perry D.J., Noakes T.J., Helliwell P.S. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. Br. Dent. J. 2007;203(7):389–393. doi: 10.1038/bdj.2007.892. [DOI] [PubMed] [Google Scholar]
- Revenco D., Morgan J.P., Tsao L. The dilemma of implantable cardioverter-defibrillator therapy in the geriatric population. J. Geriatr. Cardiol. 2011;8(3):195–200. doi: 10.3724/SP.J.1263.2011.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards D. Guidelines for the management of patients who are taking oral anticoagulants and who require dental surgery. Evid. Based Dent. 2008;9(1):5–6. doi: 10.1038/sj.ebd.6400558. [DOI] [PubMed] [Google Scholar]
- Roedig J.J., Shah J., Elayi C.S., Miller C.S. Interference of cardiac pacemaker and implantable cardioverter-defibrillator activity during electronic dental device use. J. Am. Dent. Assoc. 2010;141(5):521–526. doi: 10.14219/jada.archive.2010.0224. [DOI] [PubMed] [Google Scholar]
- Steinhauer T., Bsoul S.A., Terezhalmy G.T. Risk stratification and dental management of the patient with cardiovascular diseases. Part I: etiology, epidemiology, and principles of medical management. Quintessence Int. 2005;36(2):119–137. [PubMed] [Google Scholar]
- Stokes T., Richey R., Wray D. Prophylaxis against infective endocarditis: summary of NICE guidance. Heart. 2008;94(7):930–931. doi: 10.1136/hrt.2008.147090. [DOI] [PubMed] [Google Scholar]
- Suazo Galdames I.C., Cantin Lopez M.G., Zavando Matamala D.A. Inferior alveolar nerve block anesthesia via the retromolar triangle, an alternative for patients with blood dyscrasias. Med. Oral Patol. Oral Cir. Bucal. 2008;13(1):E43–E47. [PubMed] [Google Scholar]
- Theodotou N., Cillo J.E., Jr. Brugada syndrome (sudden unexpected death syndrome): perioperative and anesthetic management in oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 2009;67(9):2021–2025. doi: 10.1016/j.joms.2009.04.043. [DOI] [PubMed] [Google Scholar]
- Tompkins C., Cheng A., Dalal D., Brinker J.A., Leng C.T., Marine J.E. Dual antiplatelet therapy and heparin “bridging” significantly increase the risk of bleeding complications after pacemaker or implantable cardioverter-defibrillator device implantation. J. Am. Coll. Cardiol. 2010;55(21):2376–2382. doi: 10.1016/j.jacc.2009.12.056. [DOI] [PubMed] [Google Scholar]
- Washizuka T., Chinushi M., Kazama R., Hirono T., Watanabe H., Komura S. Inappropriate discharges of intravenous implantable cardioverter defibrillators owing to lead failure. Int. Heart J. 2005;46(5):909–913. doi: 10.1536/ihj.46.909. [DOI] [PubMed] [Google Scholar]
- Wraith A. Pain and anxiety control in dentistry. SAAD Dig. 1999;16(3):2. [PubMed] [Google Scholar]
- Zareba W., Moss A.J., Daubert J.P., Hall W.J., Robinson J.L., Andrews M. Implantable cardioverter defibrillator in high-risk long QT syndrome patients. J. Cardiovasc. Electrophysiol. 2003;14(4):337–341. doi: 10.1046/j.1540-8167.2003.02545.x. [DOI] [PubMed] [Google Scholar]