Abstract
Aim
This study was conducted to measure the impact of orthognathic surgery on quality of life in Saudi patients.
Materials and methods
Patients with a discrepancy of 5 mm or more who underwent orthognathic surgery either single jaw or bimaxillary at the Department of Oral and Maxillofacial Surgery, College of Dentistry, King Saud University, between September 2007 and June 2013 were included in the study. They were asked to complete the Arabic version of the 22-item Orthognathic Quality of Life Questionnaire (OQLQ) preoperatively and postoperatively. Responses at these two timepoints were compared using paired t-tests, with the significance level set to P < 0.05.
Results
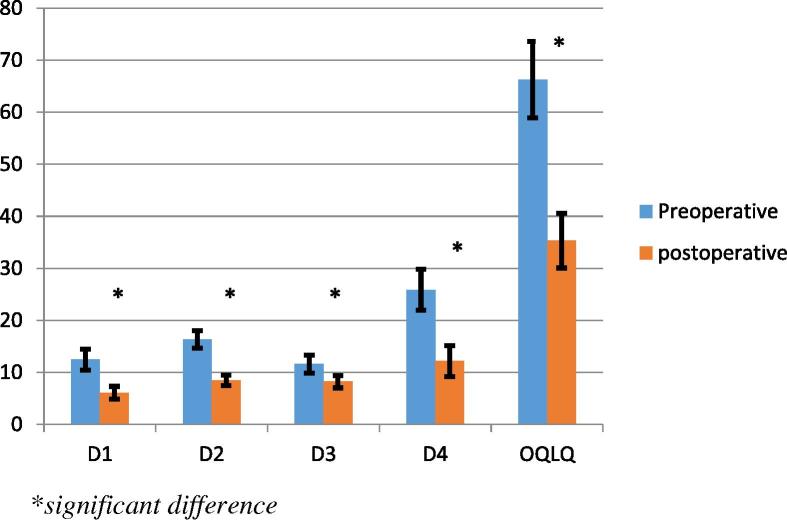
Seventeen patients participated in the study. Total OQLQ scores and those in the instrument’s four domains (oral function, facial aesthetics, awareness of dentofacial aesthetics, and social aspects) indicated that quality of life was significantly improved by orthognathic surgery (all P < 0.001).
The social aspect domain was shown to be more important for patients than were facial aesthetics and oral function.
Conclusion
The present study revealed highly significant improvement in Saudi patients’ quality of life following orthognathic surgery. This improvement was evident in all four OQLQ domains.
Keywords: Quality of life, Orthognathic surgery
1. Introduction
Modern society places great importance on physical appearance. Facial appearance and aesthetics affect a person’s self-confidence and acceptance in society, which in general affect his or her quality of life (Marques et al., 2006). Orthognathic surgery, a corrective jaw procedure, is indicated in cases of severe dentofacial deformity that cannot be corrected by orthodontic treatment alone (Ong, 2004; Sadek and Salem, 2007).
Current research reflects interest in how orthognathic surgery affects patients’ quality of life (Lee et al., 2007). Several quality of life measures are available in the field of dentistry. The Oral Health Impact Profile (Slade, 1997) was designed to determine the social impacts of oral disorders in older patients (mainly those aged ⩾60 years). Other instruments include the Social Impacts of Dental Disease measure (Cushing et al., 1986), the Geriatric/General Oral Health Assessment Index (Atchison, 1997), and the Dental Impact Profile (Cunningham et al., 2000). These instruments were developed for use among older adults and they focus mainly on dental problems, rather than dentofacial disorders, highlighting the need for a more specific tool to measure quality of life in patients with such disorders. Cunningham et al. (2002) developed the Orthognathic Quality of Life Questionnaire (OQLQ), a condition-specific quality of life measure targeting patients with dentofacial deformities.
Instruments developed to measure quality of life and health outcomes use disease-specific or generic measures (Rustemeyer and Gregersen, 2012). Generic measures assess overall health status, whereas instruments in the first category focus on specific diseases or problems (Cunningham et al., 2002; Garratt et al., 1996; Ware, 1993). The OQLQ is a brief disease-specific tool that has shown validity and reliability (Cunningham et al., 2002).
The aim of this study was to measure the impact of orthognathic surgery on patients’ quality of life using an arabic translated version of the 22-item self-reported OQLQ.
2. Materials and methods
2.1. Patients
Patients who underwent orthognathic surgery either single jaw or bimaxillary between September 2007 and June 2013 were included in this study. All surgeries were performed by the same team, including the author, at the Department of Oral and Maxillofacial Surgery, College of Dentistry, King Saud University, Riyadh, KSA. Exclusion criteria were: follow-up period <1 year; preoperative discrepancy ⩽5 mm; congenital deformity, psychological disorder, and/or physical disability; refusal to participate in the study or provide consent; and occurrence of any complication as a result of surgery or anaesthesia.
2.2. Ethical considerations
The study was approved by the Research Center and Ethics Committee of the College of Dentistry, King Saud University, Saudi Arabia with registration number FR0153. All patients signed an informative consent before participation in the study.
2.3. Data collection and measures
Each patient was asked to complete the 22-item self-reported OQLQ, translated into Arabic, immediately before surgery and at least 1 year postoperatively. The OQLQ measures the effects of dentofacial deformity on quality of life. Items are structured by a four-point scale ranging from 1 (“bothers you a little”) to 4 (“bothers you a lot”). Items are grouped into four domains: oral function (items 2, 3, 4, 5, and 6), score 0–20), facial aesthetics (items 1, 7, 10, 11, and 14; score 0–20), awareness of dentofacial aesthetics (items 8, 9, 12, and 13; score 0–16), and social aspects (items 15–22, score 0–32). Total scores range from 0 to 88, with lower scores indicating better quality of life (Cunningham et al., 2002).
Three bilingual (Arabic and English) native Arabic speakers translated the OQLQ into Arabic: the author; an associate professor in the Department of Oral and Maxillofacial Surgery, College of Dentistry, King Saud University; and a lecturer in Oral Biology, College of Applied Medical Sciences, King Saud University. After translating the questionnaire independently, the three translators developed the Arabic version of the OQLQ by consensus. The translated questionnaire was then validated in a sample of 15 bilingual (Arabic and English) volunteers: 10 students in the final year of study at the College of Dentistry and 5 faculty members. After administration and collection of the questionnaires, responses were discussed with these volunteers to identify any misunderstanding or vague expressions.
2.4. Statistical analysis
Questionnaire data collected from patients were analysed using SPSS (version 22, IBM Chicago, IL, USA). Paired t-tests were used to compare preoperative and postoperative responses, with the level of significance set to P < 0.05.
3. Results
Seventeen patients participated in the study. Table 1 presents demographic data and type of surgery for this sample. OQLQ total and domain scores indicated that quality of life was significantly improved by orthognathic surgery (all <0.001) Tables 2 and 3, Fig. 1).
Table 1.
Presents the demographic data and type of surgery of the patients.
| Male | Female | |
|---|---|---|
| Number | 5 | 12 |
| Age by years (mean) | 20–37 (25) | 19–27 (21.3) |
| Type of surgery | ||
| Bimaxillary | 2 | 6 |
| BSSO∗ | 3 | 6 |
BSSO: bilateral sagittal split osteotomy.
Table 2.
Showing the scores registered by the patients and its mean values.
| Patient | Gender | D1 pre. | D1 post. | D2 pre. | D2 post. | D3 pre. | D3 post. | D4 pre. | D4 post. | OQLQ pre. | OQLQ post. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 11 | 6 | 16 | 9 | 14 | 10 | 22 | 10 | 63 | 41 |
| 2 | F | 15 | 7 | 18 | 11 | 13 | 10 | 32 | 21 | 78 | 49 |
| 3 | M | 14 | 5 | 17 | 8 | 12 | 6 | 23 | 13 | 66 | 32 |
| 4 | M | 14 | 7 | 17 | 9 | 12 | 8 | 26 | 14 | 69 | 38 |
| 5 | F | 8 | 5 | 13 | 8 | 8 | 6 | 18 | 10 | 47 | 29 |
| 6 | F | 10 | 6 | 15 | 8 | 12 | 8 | 29 | 12 | 66 | 34 |
| 7 | M | 14 | 8 | 13 | 8 | 12 | 10 | 26 | 17 | 65 | 43 |
| 8 | M | 13 | 5 | 17 | 10 | 12 | 8 | 22 | 10 | 64 | 33 |
| 9 | F | 14 | 9 | 16 | 8 | 12 | 10 | 24 | 13 | 66 | 40 |
| 10 | M | 13 | 6 | 15 | 7 | 10 | 8 | 25 | 10 | 63 | 31 |
| 11 | F | 14 | 7 | 18 | 8 | 12 | 8 | 30 | 11 | 74 | 34 |
| 12 | F | 11 | 5 | 17 | 8 | 14 | 8 | 30 | 9 | 72 | 30 |
| 13 | F | 10 | 5 | 15 | 8 | 10 | 8 | 21 | 11 | 56 | 32 |
| 14 | F | 13 | 6 | 18 | 7 | 10 | 8 | 26 | 11 | 67 | 32 |
| 15 | F | 14 | 7 | 17 | 9 | 10 | 8 | 27 | 12 | 68 | 36 |
| 16 | F | 14 | 5 | 17 | 9 | 14 | 8 | 32 | 12 | 77 | 34 |
| 17 | F | 10 | 5 | 19 | 9 | 10 | 8 | 27 | 11 | 66 | 33 |
| Mean | 12.47 | 6.12 | 16.35 | 8.47 | 11.59 | 8.24 | 25.88 | 12.18 | 66.29 | 35.35 |
Table 3.
Paired sample statistics.
| Mean | Std. deviation | Std. error mean | Sig. (2-tailed) | ||
|---|---|---|---|---|---|
| Pair 1 | D1 preoperative | 12.4706 | 2.03463 | .49347 | 0.000 |
| D1 postoperative | 6.1176 | 1.21873 | .29558 | ||
| Pair 2 | D2 preoperative | 16.3529 | 1.69341 | .41071 | 0.000 |
| D2 postoperative | 8.4706 | 1.00733 | .24431 | ||
| Pair 3 | D3 preoperative | 11.5882 | 1.69775 | .41176 | 0.000 |
| D3 postoperative | 8.2353 | 1.20049 | .29116 | ||
| Pair 4 | D4 preoperative | 25.8824 | 3.95099 | .95825 | 0.000 |
| D4 postoperative | 12.1765 | 2.96301 | .71863 | ||
| Pair 5 | OQLQ preoperative | 66.2941 | 7.33796 | 1.77972 | 0.000 |
| OQLQ postoperative | 35.3529 | 5.26713 | 1.27747 | ||
Figure 1.
A graph showing the mean values of all the four domains of the questionnaire and the overall QOLQ with its significance.
4. Discussion
In recent times, people have directed great care towards their appearance and how it can affect their careers, relationships, self-confidence, and, generally, quality of life. WHO defines Quality of Life as individuals Z perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. It is a broad ranging concept affected in a complex way by the person’s physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment. (Tabrizi et al., 2014). The impacts of dentofacial deformities on people’s emotional and social lives have been a focus of research for a long time (Cunningham et al., 2000; Garvill et al., 1992; Hatch et al., 1998). Dentofacial deformity has long been expected to affect quality of life, which should be improved after orthognathic surgery. Among the most effective instruments for the measurement of this process is the OQLQ, developed through precise testing, rather than using more comprehensive instruments that cover more than one causative factor. (Cunningham et al., 2000, 2002; Lee et al., 2007; Younossi et al., 1999).
The results of the present study showed a highly significant degree of overall improvement in patients’ quality of life after orthognathic surgery, in agreement with previous findings (Choi et al., 2010; Kavin et al., 2012; Rustemeyer and Gregersen, 2012; Soh and Narayanan, 2013; Tabrizi et al., 2014). Mean scores were higher in our study than in that conducted by Lee et al. (2007) using the Chinese version of the 22-item OQLQ. This difference may be explained by the degree of preoperative discrepancy [>5 mm in our patients, not reported by Lee et al. (2007)] and/or by differences in culture and the ability of the translated instruments to suitably express patients’ feelings and perspectives. We used preoperative discrepancy >5 mm as an inclusion criterion because we believe that greater discrepancy is associated with greater psychological trauma, and to avoid dilution and biasing of scores due to sample heterogeneity.
Previous researchers (Kavin et al., 2012; Murphy et al., 2011; Rustemeyer and Gregersen, 2012) have reported that the greatest differences in preoperative and postoperative OQLQ scores were in the facial aesthetics domain. In our study, the difference in the social aspects domain was greatest, followed by those in the facial aesthetics and oral function domains. Psychosocial responses may differ considerably among cultures. Jensen (1978) and Kiyak et al. (1985) mentioned the importance of conformity between orthognathic surgery and social acceptance regarding culture-specific aims and values, which may explain the high social aspects scores in the present study. Given the conservative and intimate nature of Saudi society, we believe that all of its members, especially women, are keenly attuned to others’ opinions about and acceptance of their appearance and behaviour.
The awareness of dentofacial anomalies domain showed the smallest difference between mean preoperative and postoperative scores in this study, in line with the finding of Taylor et al. (2009) that malocclusion and its orthodontic treatment had little effect on general quality of life in an adolescent sample. The author can explain the similarity in the present study results with the results of Taylor et al., 2009 as a result to the young age of our patients in its average. The study limitation includes the limited number of patients as we included only the patients treated by the author team as a result we think that further studies are needed on a bigger sample size.
5. Conclusion
-
-
In conclusion, the present study showed highly significant improvement in Saudi patients’ quality of life following orthognathic surgery. This improvement was evident in all four OQLQ domains. The social aspects domain was shown to be more important for patients than were facial aesthetics and oral function.
-
-
OQLQ was found to be an efficient instrument for the evaluation of quality of life of the patients in its Arabic translated version.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgements
The author would like to thank the College of Dentistry Research Center, King Saud University for their support during conduction of this research.
Footnotes
Peer review under responsibility of King Saud University.
References
- Atchison, K.A. The general oral health assessment index. In: Slade GD, editor. Measuring oral health and quality of life. North Carolina: University of North Carolina; 1997. Quoted from Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Community Dent Oral Epidemiol 2002; 30: 81–90. [DOI] [PubMed]
- Choi W.S., Lee S., McGrath C., Samman N. Change in quality of life after combined orthodontic-surgical treatment of dentofacial deformities. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010;109:46–51. doi: 10.1016/j.tripleo.2009.08.019. [DOI] [PubMed] [Google Scholar]
- Cunningham S.J., Garratt A.M., Hunt N.P. Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Commun. Dent. Oral Epidemiol. 2002;30:81–90. doi: 10.1034/j.1600-0528.2002.300201.x. [DOI] [PubMed] [Google Scholar]
- Cunningham S.J., Garratt A.M., Hunt N.P. Development of a condition-specific quality of life measure for patients with dentofacial deformity: I. Reliability of the instrument. Commun Dent Oral Epidemiol. 2000;28:195–201. doi: 10.1034/j.1600-0528.2000.280305.x. [DOI] [PubMed] [Google Scholar]
- Cushing A.M., Sheiham A., Maizels J. Developing sociodental indicators – the social impact of dental disease. Community Dent. Health. 1986;3:3–17. [PubMed] [Google Scholar]
- Garratt A.M., Ruta D.A., Abdalla M.I., Russell I.T. Responsiveness of the SF-36 and a condition-specific measure of health for patients with varicose veins. Qual. Life Res. 1996;5:1–12. doi: 10.1007/BF00434744. [DOI] [PubMed] [Google Scholar]
- Garvill J., Garvill H., Kahnberg K.E., Lundgren S. Psychological factors in orthognathic surgery. J. Craniomaxillofac. Surg. 1992;20:28–33. doi: 10.1016/s1010-5182(05)80193-3. [DOI] [PubMed] [Google Scholar]
- Hatch J.P., Rugh J.D., Clark G.M., Keeling S.D., Tiner B.D., Bays R.A. Health-related quality of life following orthognathic surgery. Int. J. Adult Orthodon. Orthognath. Surg. 1998;13:67–77. [PubMed] [Google Scholar]
- Jensen S.H. The psychosocial dimensions of oral and maxillofacial surgery: a critical review of the literature. J. Oral. Surg. 1978;36:447–453. [PubMed] [Google Scholar]
- Kavin T., Jagadesan A.G., Venkataraman S.S. Changes in quality of life and impact on patients’ perception of esthetics after orthognathic surgery. J. Pharm. Bioallied. Sci. 2012;4:S290–S293. doi: 10.4103/0975-7406.100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiyak H.A., McNeill R.W., West R.A. The emotional impact of orthognathic surgery and conventional orthodontics. Am. J. Orthod. 1985;88:224–234. doi: 10.1016/s0002-9416(85)90217-9. [DOI] [PubMed] [Google Scholar]
- Lee S., McGrath C., Samman N. Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. Int. J. Oral Maxillofac. Surg. 2007;36:488–492. doi: 10.1016/j.ijom.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Marques L.S., Ramos-Jorge M.L., Paiva S.M., Pordeusb I.A. Malocclusion: esthetic impact and quality of life among Brazilian schoolchildren. Am. J. Orthod. Dentofacial Orthop. 2006;129:424–427. doi: 10.1016/j.ajodo.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Murphy C., Kearns G., Sleeman D., Cronin M., Allen P.F. The clinical relevance of orthognathic surgery on quality of life. Int. J. Oral Maxillofac. Surg. 2011;40:926–930. doi: 10.1016/j.ijom.2011.04.001. [DOI] [PubMed] [Google Scholar]
- Ong M.A.D. Spectrum of dentofacial deformities. Ann. Acad. Med. Sing. 2004;33:239–242. [PubMed] [Google Scholar]
- Rustemeyer J., Gregersen J. Quality of life in orthognathic surgery patients: postsurgical improvements in aesthetics and self-confidence. J. Craniomaxillofac. Surg. 2012;40:400–404. doi: 10.1016/j.jcms.2011.07.009. [DOI] [PubMed] [Google Scholar]
- Sadek, H., Salem, G., 2007. Psychological aspects of orthognathic surgery and its effect on quality of life in Egyptian patients. La Revue de Santé de la Méditerranée orientale 13(1) [PubMed]
- Slade G.D. Derivation and validation of a short-form oral health impact profile. Commun. Dent. Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- Soh C.L., Narayanan V. Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery-a systematic review. Int. J. Oral Maxillofac. Surg. 2013;42:974–980. doi: 10.1016/j.ijom.2013.03.023. [DOI] [PubMed] [Google Scholar]
- Taylor K.R., Kiyak A., Huang G.J., Greenlee G.M., Jolley C.J., King G.J. Effects of malocclusion and its treatment on the quality of life of adolescents. Am. J. Orthod. Dentofacial Orthop. 2009;136:382–392. doi: 10.1016/j.ajodo.2008.04.022. [DOI] [PubMed] [Google Scholar]
- Tabrizi R., Rezaii A., Golkari A., Ahrari F. The impact of orthognathic surgery on oral health-related quality of life. J. Dent. Mater. Technol. 2014;3(1):23–27. [Google Scholar]
- Ware J.E. Measuring patients’ views: the optimum outcome measure. Br. Med. J. 1993;306:1429–1430. doi: 10.1136/bmj.306.6890.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younossi Z.M., Guyatt G., Kiwi M., Boparai N., King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45:295–300. doi: 10.1136/gut.45.2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]