Abstract
Introduction
Pulmonary spindle cell carcinoma (SpCC) is a rare subtype of non-small-cell lung cancer (NSCLC) and, in general, is chemoresistance.
Case
A sixty-five year-old male patient with metastatic pulmonary SpCC was initially treated with cisplatin and docetaxel, but his disease progressed. Then, he received a combination chemotherapy with carboplatin and nab-PTX followed by maintenanced chemotherapy with nab-PTX. Fluorodeoxyglucose (FDG) positron-emission CT revealed a substantial decrease of FDG accumulation in the primary tumor, and the response continued for more than 7 months.
Discussion
Preclinical models suggested that nab-PTX may reach the tumor microenvironment more efficiently than solvent-based paclitaxel (sb-PTX) and be preferentially taken up by cancer cells. Considering that there is no effective treatment for patients with pulmonary SpCC, nab-PTX may merit further investigation in patients with pulmonary SpCC.
Keywords: Pulmonary sarcomatoid carcinoma, Spindle cell carcinoma, Nab-PTX
Introduction
Pulmonary sarcomatoid carcinoma (PSC) is defined as a poorly differentiated non-small-cell lung cancer (NSCLC) containing sarcoma or a sarcoma-like component. Pulmonary spindle cell carcinoma (SpCC) is a rare subgroup of PSC comprised only of spindle cells. In general, SpCC is chemoresistance, and a few cases with poor outcome have been reported in an advanced stage.
Nanoparticle albumin-bound paclitaxel (nab-PTX) is an albumin-bound, 130 nm particle form of paclitaxel that exhibits a higher activity and lower toxicity than solvent-based paclitaxel (sb-PTX). In a previous phase III study comparing nab-PTX with sb-PTX in combination with cabboplatin, nab-PTX demonstrated significantly better response rate and less neuropathy than sb-PTX in advanced NSCLC [1].
Here, we described a case of pulmonary SpCC, refractory to cisplatin plus docetaxel, but which responded to subsequent treatment with carboplatin plus nab-PTX.
Case
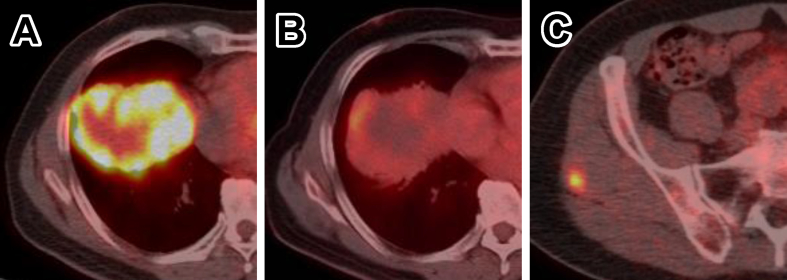
A 65-year-old never-smoking male presented with progressing right hypochondrial pain. Contrast-enhanced computed tomography (CT) revealed a 74-mm irregular tumor in the right lower lobe with diaphragm invasion (Fig. 1A). Fluorodeoxyglucose (FDG) positron-emission CT demonstrated marked FDG accumulation in the marginal region of the lung tumor and solitary nodule-shaped accumulations in pleura, liver, and the right gluteal muscles (Fig. 2A and C).
Fig. 1.
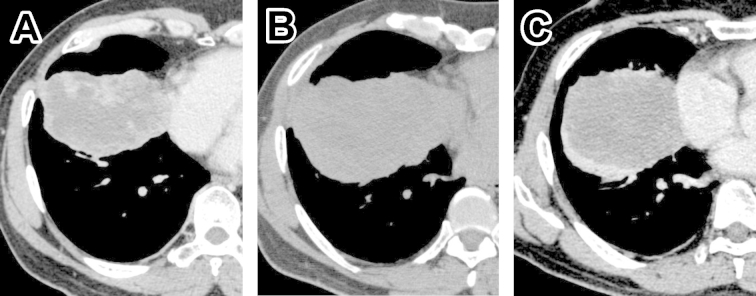
Imaging findings in chest computed tomography (CT). (A) Contrast-enhanced CT showing a 74-mm irregular tumor in the right lower lobe with diaphragm invasion. (B) Plane CT showing a 111-mm tumor after 1 cycle of cisplatin plus docetaxel treatment. (C) Contrast-enhanced CT showing an 83-mm tumor after 2 cycles of carboplatin with albumin-bound paclitaxel.
Fig. 2.
Fluorodeoxyglucose (FDG) positron-emission computed tomography findings at diagnosis and at 8 weeks after treatment initiation. (A) Marked accumulation of FDG in a marginal region of the lung tumor and low accumulation in the center of the tumor. (B) Low accumulation in the lung tumor after 2 cycles of carboplatin with albumin-bound paclitaxel. (C) Nodule-shaped accumulation in left gluteal muscles at diagnosis.
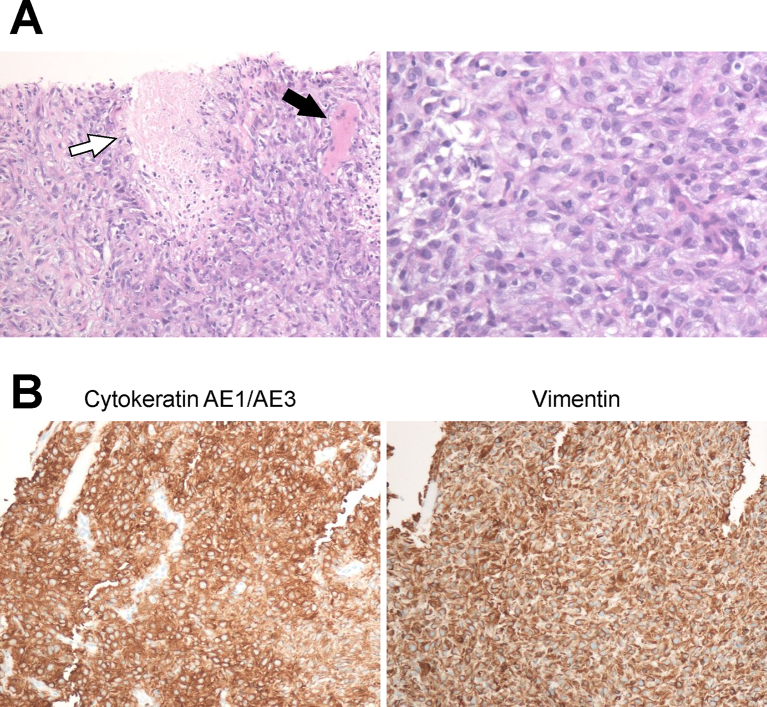
Ultrasound-guided needle biopsy of the nodule in the gluteal muscle was performed to avoid an unnecessary biopsy because massive necrosis was suspected in the lung tumor. Histologically, the nodule consisted only of spindle-shaped malignant cells with invasion to skeletal muscles and clustered necrotic foci (Fig. 3A). Neither tubular formation nor squamous differentiation was identified.
Fig. 3.
Histopathological findings of the nodule obtained from left gluteal muscle. (A) Low-power (left) and high-power (right) images of a hematoxylin and eosin-stained section showing the tumor comprised only of spindle-shaped malignant cells with clustered necrotic regions (white arrow) and invasion to skeletal muscles (black arrow). (B) Immunohistochemical analysis showing diffuse cytokeratin AE1/AE3 (left) and vimentin (right) positivity.
Immunohistochemical analysis demonstrated that the tumor cells were diffusely positive for cytokeratin AE1/AE3 and vimentin (Fig. 3B), and negative for S-100, p63, synaptophysin, and thyroid transcription factor 1 (TTF-1). The patient was diagnosed with spindle cell carcinoma (SpCC) of the lung based on the World Health Organization (WHO) criteria.1 The clinical stage was IV (cT4N1M1b).
First-line chemotherapy with cisplatin and docetaxel was started, but disease progression (Fig. 1B) and grade 2 creatinine elevation were observed after 1 cycle. Subsequently, chemotherapy with carboplatin and nab-PTX was started. CT taken after 2 cycles of chemotherapy demonstrated a reduction of tumor size (Fig. 1C), and FDG-PET revealed a substantial decrease of FDG accumulation in the primary tumor (Fig. 2B). The patient received 4 cycles of the combination therapy followed by 4 cycles of continued maintenance therapy with nab-PTX, and is now alive 9 months from the diagnosis with the maintenance of stable disease for 7 months.
Discussion
In the current WHO histological classification of lung tumors, PSC is defined as a poorly differentiated NSCLC containing sarcoma or a sarcoma-like component. Pulmonary SpCC is a subgroup of PSC comprised only of spindle cells [2]. In terms of advanced or recurrent pulmonary SpCC, a few cases have been reported, with a poor outcome [3,4]. To our knowledge, this is the first case of successful treatment of pulmonary SpCC at an advanced stage.
A retrospective cohort of 97 patients with advanced or recurrent PSC receiving conventional chemotherapy showed better progression-free survival (PFS) in some patients receiving a platinum plus gemcitabine or sb-PTX regimen, although most patients presented a poor outcome (median PFS: 2.0 months) [5]. As described in this report, interestingly, nab-PTX was effective in a patient refractory to docetaxel.
Although sb-PTX has often been selected for the treatment of PSC, nab-PTX must take the place of sb-PTX in future considering that nab-PTX has obvious superiority in both efficacy and toxicity in patients with NSCLC [1]. Preclinical models suggested that nab-PTX may reach the tumor microenvironment more efficiently than sb-PTX and be preferentially taken up by cancer cells [6].
As a limitation to this work, we could not completely demonstrate that the whole tumor was comprised only of spindle cells, since the obtained sample was just a part of the whole tumor. In previous reports, however, an SpCC diagnosis was described as being given based on biopsy samples [3,4].
In conclusion, we have presented a case of PSC, probably pulmonary SpCC, refractory to cisplatin plus docetaxel, but which responded to subsequent treatment with carboplatin plus nab-PTX. Considering that there is no effective treatment for patients with PSC, including pulmonary SpCC, nab-PTX may merit further investigation in this rare but extremely aggressive disease.
References
- 1.Socinski M.A., Bondarenko I., Karaseva N.A., Makhson A.M., Vynnychenko I., Okamoto I. Weekly nab-paclitaxel in combination with carboplatin versus solvent-based paclitaxel plus carboplatin as first-line therapy in patients with advanced non-small-cell lung cancer: final results of a phase III trial. J Clin Oncol. 2012;30:2055–2062. doi: 10.1200/JCO.2011.39.5848. [DOI] [PubMed] [Google Scholar]
- 2.Travis WD, Colby TV, Corrin B, Shimosato Y, and Brambilla E. Histological Typing of lung and Pleural tumors, 3rd ed.; World Health Organization International Histological Classification of Tumours.
- 3.Terada T. Spindle cell carcinoma of the lung: frequency, clinical features, and immunohistochemical studies of three cases. Respir Med CME. 2010;3:241–245. [Google Scholar]
- 4.Misumida N., Sanda R., Ota A., Kato M., Takagi Y., Yagi A. A case of rapidly progressing lung spindle cell carcinoma presenting as pancoast syndrome. Nihon Kokyuki Gakkai Zasshi. 2009;47:865–869. [PubMed] [Google Scholar]
- 5.Vieira T., Girard N., Ung M., Monnet I., Cazes A., Bonnette P. Efficacy of first-line chemotherapy in patients with advanced lung sarcomatoid carcinoma. J Thorac Oncol. 2013;8:1574–1577. doi: 10.1097/01.JTO.0000437008.00554.90. [DOI] [PubMed] [Google Scholar]
- 6.Desai N., Trieu V., Yao Z., Louie L., Ci S., Yang A. Increased antitumor activity, intratumor paclitaxel concentrations, and endothelial cell transport of cremophor-free, albumin-bound paclitaxel, ABI-007, compared with cremophor-based paclitaxel. Clin Cancer Res. 2006;12:1317–1324. doi: 10.1158/1078-0432.CCR-05-1634. [DOI] [PubMed] [Google Scholar]