Abstract
Objective:
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, the distinction between nonsuicidal self-injury (NSSI) and suicidal behaviour disorder is highlighted in the section Conditions for Further Study. Diagnostic criteria classify NSSI and suicidal behaviour disorder as distinct disorders, with the latter including suicide attempt (SA). This study examined the prevalence and correlates of NSSI in emergency department (ED) settings and compared them to SA.
Methods:
Data came from adult referrals to psychiatric services in 2 EDs between January 2009 and June 2011 (n = 5336). NSSI was compared with SA, as well as no suicidal behaviour, across a broad range of demographic and diagnostic correlates.
Results:
NSSI was more highly associated with female sex, childhood abuse, anxiety disorders, major depressive disorder (MDD), aggression and impulsivity, age under 45, and substance use disorders (SUDs), compared with presentations without suicidal behaviour. Comparing NSSI and SA, no differences were observed on sex, age, history of child abuse, or presence of anxiety or SUDs. Recent life stressors (OR 1.44; 95% CI 1.05 to 1.99), active suicidal ideation (OR 8.84; 95% CI 5.26 to 14.85), MDD (OR 3.05; 95% CI 2.23 to 4.17), previous psychiatric care or SA (OR 1.89; 95% CI 1.36 to 2.64), and single marital status (OR 1.63; 95% CI 1.20 to 2.22) contributed to a higher SA rate. Among people with NSSI, 83.7% presented only once to an ED. Among people who presented multiple times, only 18.2% re-presented with NSSI.
Conclusions:
NSSI is associated with early life adversity and psychiatric comorbidity. Most people present only once to ED services, and self-harm presentations seemed to change over time. Future studies should continue to clarify whether NSSI and SA have distinct risk profiles.
Keywords: self-injurious behaviour, suicide attempts, mental disorders, suicide risk
Abstract
Objectif :
Dans le Manuel diagnostique et statistique des troubles mentaux, 5e édition, la distinction entre automutilation non suicidaire (AMNS) et trouble de comportement suicidaire est présentée à la section Affections demandant plus d’étude. Les critères diagnostiques classent l’AMNS et le trouble de comportement suicidaire comme étant distincts, le deuxième incluant la tentative de suicide (TS). Cette étude examinait la prévalence et les corrélats de l’AMNS dans le contexte d’un service d’urgence (SU) et les a comparés avec les TS.
Méthodes :
Les données proviennent d’adultes adressés aux services psychiatriques de 2 SU entre janvier 2009 et juin 2011 (n = 5336). L’AMNS a été comparée avec les TS, et avec le comportement non suicidaire, dans unevaste gamme de corrélats démographiques et diagnostiques.
Résultats :
L’AMNS était associée de façon plus marquée avec le sexe féminin, les mauvais traitements dans l’enfance, les troubles anxieux, le trouble dépressif majeur (TDM), l’agressivité et l’impulsivité, un âge inférieur à 45 ans, et les troubles liés à l’utilisation de substances (TUS), comparativement aux présentations sans comportement suicidaire. En comparant AMNS et TS, aucune différence n’a été observée selon l’âge, le sexe, les antécédents de mauvais traitements dans l’enfance, ou la présence d’anxiété ou de TUS. Les récents stresseurs de la vie (RC 1,44; IC à 95 % 1,05 à 1,99), l’idéation suicidaire active (RC 8,84; IC à 95 % 5,26 à 14,85), le TDM (RC 3,05; IC à 95 % 2,23 à 4,17), les soins psychiatriques antérieurs ou une TS (RC 1,89; IC à 95 % 1,36 à 2,64), et la situation de célibataire (RC 1,63; IC à 95 % 1,20 à 2,22) contribuaient à un taux de TS plus élevé. Chez les personnes pratiquant l’AMNS, 83,7 % ne se sont présentées qu’une fois à un SU. Chez celles qui se sont présentées plusieurs fois, seulement 18,2 % se sont présentées de nouveau avec l’AMNS.
Conclusions :
L’AMNS est associée avec l’adversité de début de vie et la comorbidité psychiatrique. La plupart des gens ne se présentent qu’une fois à un SU, et les présentations d’automutilation semblaient changer avec le temps. De futures études devraient continuer de déterminer si l’AMNS et les TS ont des profils de risque distincts.
Nonsuicidal self-injury is “the direct, deliberate destruction of one’s own body tissue in the absence of intent to die.”1, p 78 With the recent release of DSM-5, the distinction between NSSI and SA is highlighted in the section entitled Conditions for Further Study. Diagnostic criteria are laid out for both NSSI and suicidal behaviour disorder as separate and distinct disorders, with the latter including SA. In contrast, a recent editorial2 argued that suicidal behaviour and NSSI are not so distinct. With strong arguments, both for and against NSSI as a distinct category, both sides have advocated for more research to clarify the distinction or non-distinction between NSSI and SA.2,3
Previous research has shown that NSSI is associated with numerous risk factors and correlates, including: SUDs, childhood sexual abuse, MDD, SA, and completed suicide.4–8 Interestingly, several studies demonstrate an association between NSSI and suicidal behaviour. In a sample of offspring of parents with a DSM-IV mood disorder, Cox et al5 found in multivariate models that a diagnosis of depression, greater aggression, depressive symptoms, and suicidal ideation were the strongest correlates of NSSI. They also examined the correlates of NSSI longitudinally and found similar results. The strongest predictors of future NSSI were a diagnosis of current MDD, suicidal ideation at the time point closest to the NSSI, and younger age.4 Further, they found that a history of NSSI predicted future SA and that SA after baseline predicted future NSSI.
People who engage in NSSI are also more likely to have alcohol and drug use disorders, compared with those who do not engage in self-harm.9,10 In addition, childhood sexual abuse has been found to be a risk factor for self-harm, including NSSI.11–13 Nock and Kessler10 directly compared the correlates and risk factors of NSSI and SA in an American nationally representative sample. They found that a major depressive episode, drug abuse and dependence, conduct disorder, antisocial personality disorder, simple phobias, having more than 3 mental disorders, a history of multiple incidents of sexual molestation, and a history of physical assault were more strongly associated with SA than with NSSI.
Clinical Implications
NSSI is associated with early life adversity and psychiatric comorbidity.
SAs, compared with NSSIs, are associated with having an organized plan or serious attempt, lacking social support, having experienced an acute stressor, and having active and passive suicidal ideation.
Most people with NSSI present only once to ED services, and, when people with NSSI present multiple times to ED services, their reason for presentation changes over time.
Limitations
We were unable to draw conclusions about risk for completed suicide.
Our study had a cross-sectional design.
Assessments were based on clinical interview, not on standardized diagnostic tests.
Only 2 hospitals in the Winnipeg area were covered in our study, thus excluding presentations to other hospitals.
Taken together, these findings suggest that NSSI is associated with numerous correlates and risk factors, including: psychiatric comorbidity, suicidal ideation and behaviour, and childhood adversity. Unfortunately, one of the major limitations in the literature is that there are few studies that have looked at the correlates and risk factors of NSSI, compared with SA, among adults. The literature in this area has been limited by small samples and mostly cross-sectional designs. While previous research has shown that NSSI is associated with psychiatric comorbidity, suicidal ideation and behaviour, and childhood adversity, it is unknown whether these correlates and risk factors are more strongly associated with NSSI or SA. It is also of interest to examine whether people with NSSI are likely to repeat this behaviour, or engage in other types of self-harm, as a way of examining the stability of the proposed diagnosis over time. Existing data strongly suggest that SA and suicidal ideation are common among people who engage in NSSI.4,8,14–16 Teasing apart the unique correlates and risk factors of NSSI and SA has major implications for clinical practice and public health initiatives. Bridging these gaps is important to better inform the study and treatment of self-harm behaviour.
The purpose of our study is to examine the correlates and risk factors for NSSI and SA using a sample (n = 5336) comprised of all consecutive adults who were assessed by psychiatric services in the EDs of the 2 largest tertiary care hospitals in Manitoba. Our study will not directly test DSM-5 classifications of NSSI and suicidal behaviour disorder, but instead will classify single presentations based on the intent of self-harm. The current research has 2 objectives. The first objective is to compare the correlates and risk factors of NSSI and SA among adults who present to ED services. Our hypothesis is that SA will be more strongly associated with depression, anxiety disorders, and a history of child abuse, compared with NSSI. The second objective is to determine whether people with NSSI are likely to repeat this behaviour or engage in other types of self-harm behaviour or suicidal ideation. Our hypothesis is that people who engage in NSSI will also engage in other forms of self-harm behaviour, including SA and suicidal ideation, rather than an exclusive pattern of repetitive NSSI.
Methods
Data for this study came from the SAFE database. The SAFE database is comprised of consecutive adults who are assessed by psychiatric services in the EDs of the 2 largest tertiary care hospitals in Manitoba. The SAFE also included the CL psychiatry service. The CL psychiatry service targeted people who were admitted to the hospital and bypassed psychiatric consultation in the ED. The study period was 2.5 years, from January 1, 2009, to June 30, 2011, for the EDs and from January 1, 2009, to June 30, 2010, for the CL psychiatry service.
Study Population
The study population included consecutive referrals to psychiatric services during the study period (n = 5336). There were no exclusionary criteria.
Assessment of the patients were conducted by psychiatry residents and medical students in training, supervised by attending staff psychiatrists. The assessment included a review of the presenting problem, demographic information, psychiatric conditions, medical history, social and development issues, as well as information on any current treatment or previous contact with mental health professionals. The physician then completed the SAFE, which included the C-CASA17 to classify suicidal behaviour. The C-CASA is a standardized suicidal rating system developed by Posner et al.17 The C-CASA is the suicide-related event assessment instrument endorsed by the US Food and Drug Administration and has been adopted in subsequent studies.18–22 The C-CASA classifies self-harm behaviour into 8 mutually exclusive categories: completed suicide; SA; preparatory acts toward imminent suicidal behaviour; suicidal ideation; SIB, no suicidal intent; other, no self-harm; SIB, suicidal intent unknown; and, not enough information. C-CASA ratings have been found to be highly reliable (intraclass correlation coefficient = 0.89). 17
For the purpose of our study, the C-CASA definitions we are interested in are SA and NSSI. SA, as defined by the C-CASA, is as follows:
a potentially self-injurious behavior, associated with at least some intent to die, as a result of the act. Evidence that the individual intended to kill him/herself, at least to some degree, can be explicit or inferred from the behavior or circumstance. A suicide attempt may or may not result in actual injury.17, p 1037
NSSI is as follows:
self-injurious behavior associated with no intent to die. The behavior is intended purely for other reasons, either to relieve distress (often referred to as “self-mutilation,” e.g., superficial cuts or scratches, hitting/banding, or burns) or to effect change in others or the environment.17, p 1037
The following variables were assessed at the baseline presentation: demographics (sex, age [under 45 and over 45], and marital status), psychiatric disorders (MDD, SUDs, anxiety disorders, and psychotic disorders), childhood adversity (presence of child abuse), suicidality (passive suicidal ideation, active suicidal ideation, previous attempts or psychiatric care, and organized plan or serious attempt), and other correlates (presence of an acute stressor, aggression or impulsivity, access to firearms, social support lacking, and chronic pain or physical illness).
Statistical Analysis
Using PASW Statistics for Windows, version 18.0 (SPSS Inc, Chicago, IL, 2009), we generated descriptive prevalence rates for people with NSSI and with no self-harm or suicidal ideation for each of the variables at baseline and conducted binary logistic regressions to investigate if NSSI was more likely to be associated with psychiatric comorbidity (for example, MDD), suicidality (for example, suicidal ideation), and early life adversity (for example, child abuse), compared with no self-harm or suicidal ideation. These models were also run using the same dependent variables but instead comparing people with NSSI to those with SA. Next, descriptive statistics were used to determine the number of presentations to ED services among the entire population and among those with NSSI. Finally, among people with NSSI who present multiple times to ED services, descriptive statistics were used to determine the reasons for presentation (that is, another NSSI, SA, or suicidal ideation).
Ethical Approval
Informed written consent was not obtained from study subjects, as permitted under section 24(3)c of the Personal Health Information Act. The study was approved by the Human Research Ethics Board at the University of Manitoba.
Results
During the course of a 2.5-year period, there were 5336 presentations to ED services and to the CL psychiatry service. Among these, 44.6% (n = 2380) had presentations that did not feature suicidal ideation or self-harm. NSSI accounted for 4.3% (n = 230) of presentations to ED services or the CL psychiatry service. SA were featured in 14% (n = 749) of presentations. Among the 4028 people who presented to ED services, 80% (n = 3225) had a single presentation to ED services or the CL psychiatry service, 13% (n = 522) presented twice to ED services or the CL psychiatry service, and 7.1% (n = 281) of the sample had 3 or more presentations.
Table 1 shows the psychological and psychosocial correlates of the entire SAFE database sample. Most of the sample was male, less than 45 years old, and had single marital status. The sample also has a high prevalence of psychiatric disorders, previous SA or psychiatric care, and suicidal ideation.
Table 1.
Descriptive prevalence rates of demographic and psychiatric correlates in the Suicide Assessment Form in Emergency Psychiatry database sample, N = 5336
| Demographic | n (%) |
|---|---|
| Sex, male | 2764 (51.8) |
| Age, <19 or >45 years | 2207 (41.4) |
| Single marital status | 3410 (63.9) |
| Childhood adversity | |
| Childhood sexual or physical abuse | 911 (17.1) |
| Psychiatric disorders | |
| Anxiety disorders | 1144 (21.4) |
| Depressive disorders | 2348 (44.0) |
| Substance use disorders | 2360 (44.2) |
| Psychotic disorders | 1885 (35.3) |
| Suicidality | |
| Passive suicidal ideation | 1517 (28.4) |
| Active suicidal ideation | 1157 (21.7) |
| Previous attempts or psychiatric care | 3683 (69.0) |
| Organized plan or serious attempt | 819 (15.3) |
| Other correlates | |
| Acute stressor | 2534 (47.5) |
| Aggression or impulsivity | 2474 (46.4) |
| Social support lacking | 1968 (36.9) |
| Chronic pain or physical illness | 1422 (26.6) |
| Access to firearms | 130 (2.4) |
Table 2 displays the relation at baseline between type of presentation and the various psychological and psychosocial baseline measures. People who presented with NSSI, compared with no self-harm or suicidal ideation, had the following demographics: they were less likely to be male (OR 0.65; 95% CI 0.50 to 0.86, P < 0.01), they were less likely to be over the age of 45 years (OR 0.54; 95% CI 0.40 to 0.73, P < 0.001), and they were less likely to have single marital status (OR 0.73; 95% CI 0.55 to 0.97, P < 0.05). They were also more likely to have been physically or sexually abused as a child (OR 2.73; 95% CI 1.84 to 4.06, P < 0.001). Regarding psychiatric disorders, people who presented with NSSI, compared with no self-harm or suicidal ideation, were more likely to suffer from an anxiety disorder (OR 1.65; 95% CI 1.19 to 2.30, P < 0.01), MDD (OR 2.47; 95% CI 1.85 to 3.30, P < 0.001), and a SUD (OR 2.64; 95% CI 1.99 to 3.52, P < 0.001). However, they were less likely to suffer from a psychotic disorder (OR 0.18; 95% CI 0.13 to 0.26, P < 0.001).
Table 2.
Correlates of NSSI, compared with SAs, among tertiary care emergency department patients
| Total sample | No SH or SI N= 2380 (44.6%) n (%) | NSSI n = 230 (4.3%) n (%) | SA N= 749 (14.0%) n (%) | NSSI, compared with no SH or SI (reference) OR (95% CI) | P | SA, compared with no SH or SI OR (95% CI) | P | SA, compared with NSSI OR (95% CI) | P |
|---|---|---|---|---|---|---|---|---|---|
| Demographic | |||||||||
| Sex, female | 1065 (44.8) | 126 (55.3) | 418 (56.0) | 0.65 (0.50 to 0.86)a | 0.64 (0.54 to 0.76)a | 0.98 (0.73 to 1.32) | |||
| Male (reference) | 1306 (55.0) | 101 (44.3) | 328 (44.0) | 0.002 | <0.001 | 0.95 | |||
| Age <19 or >45 years | 1094 (48.2) | 73 (33.5) | 282 (39.0) | 0.54 (0.40 to 0.73)a | <0.001 | 0.69 (0.58 to 0.82)a | <0.001 | 1.27 (0.92 to 1.75) | <0.001 |
| Single marital status | 1440 (63.8) | 125 (56.3) | 488 (67.8) | 0.73 (0.55 to 0.97)a | 0.03 | 1.19 (1.00 to 1.43) | 0.05 | 1.63 (1.20 to 2.22)a | 0.002 |
| Childhood adversity | |||||||||
| Childhood sexual or physical abuse | 216 (24.8) | 55 (47.4) | 171 (47.4) | 2.73 (1.84 to 4.06)a | <0.001 | 2.73 (2.11 to 3.53)a | <0.001 | 1.00 (0.66 to 1.52) | 0.99 |
| Psychiatric disorders | |||||||||
| Anxiety disorder | 360 (21.0) | 58 (30.5) | 170 (29.4) | 1.65 (1.19 to 2.30)a | 0.003 | 1.57 (1.27 to 1.94)a | <0.001 | 0.95 (0.66 to 1.36) | 0.77 |
| Depression | 470 (22.3) | 90 (41.5) | 491 (68.4) | 2.47 (1.85 to 3.30)a | <0.001 | 7.54 (6.25 to 9.10)a | <0.001 | 3.05 (2.23 to 4.17)a | <0.001 |
| Substance abuse | 783 (36.9) | 133 (60.7) | 430 (60.6) | 2.64 (1.99 to 3.52)a | <0.001 | 2.62 (2.20 to 3.12)a | <0.001 | 0.99 (0.73 to 1.35) | 0.96 |
| Psychosis | 1224 (54.5) | 39 (17.7) | 90 (12.9) | 0.18 (0.13 to 0.26)a | <0.001 | 0.12 (0.10 to 0.16)a | <0.001 | 0.69 (0.46 to 1.04) | 0.08 |
| Suicidality | |||||||||
| Passive suicidal ideation | 127 (6.3) | 47 (22.2) | 402 (58.1) | 4.2 (2.90 to 6.09)a | <0.001 | 20.46 (16.18 to 25.87a | <0.001 | 4.87 (3.40 to 6.96)a | <0.001 |
| Active suicidal ideation | 13 (0.6) | 17 (8.1) | 299 (43.7) | 13.78 (6.59 to 28.79)a | <0.001 | 121.77 (69.15 to 214.44)a | <0.001 | 8.84 (5.26 to 14.85)a | <0.001 |
| Previous attempts or psychiatric care | 1399 (62.5) | 151 (67.1) | 576 (79.4) | 1.23 (0.92 to 1.64) | 0.17 | 2.32 (1.90 to 2.84)a | <0.001 | 1.89 (1.36 to 2.64)a | <0.001 |
| Organized plan or serious attempt | 10 (0.5) | 13 (6.0) | 417 (57.6) | 13.83 (5.99 to 31.94)a | <0.001 | 291.9 (154.15 to 552.74)a | <0.001 | 21.11 (11.82 to 37.69)a | <.001 |
| Other correlates | |||||||||
| Acute stressor | 759 (39.3) | 131 (61.8) | 476 (70.0) | 2.5 (1.87 to 3.35)a | <0.001 | 3.61 (3.00 to 4.35)a | <0.001 | 1.44 (1.05 to 1.99)a | 0.03 |
| Aggression or impulsivity | 920 (44.1) | 145 (68.1) | 442 (64.4) | 2.7 (2.00 to 3.65)a | <0.001 | 2.3 (1.93 to 2.75)a | <0.001 | 0.85 (0.62 to 1.18) | 0.34 |
| Social support lacking | 712 (32.9) | 74 (33.8) | 315 (45.2) | 1.04 (0.78 to 1.40) | 1.69 (1.42 to 2.01)a | <0.001 | 1.62 (1.18 to 2.22)a | 0.003 | |
| Chronic pain and physical illness | 655 (29.7) | 51 (23.6) | 201 (28.8) | 0.73 (0.53 to 1.02) | 0.06 | 0.96 (0.80 to 1.16) | 0.66 | 1.31 (0.92 to 1.87) | 0.14 |
| Access to firearms | 21 (1.6) | 6 (4.2) | 25 (5.4) | 2.64 (1.05 to 6.66)a | 0.04 | 3.41 (1.89 to 6.16)a | <0.001 | 1.29 (0.52 to 3.21) | 0.58 |
Statistically significant findings
NSSI = nonsuicidal self-injury; SA = suicide attempt; SH = self-harm; SI = suicidal ideation
People with NSSI also had a higher likelihood of suicidality, compared with those who presented with no self-harm or suicidal ideation. They were more likely to have passive suicidal ideation (OR 4.20; 95% CI 2.90 to 6.09, P < 0.001), active suicidal ideation (OR 13.78; 95% CI 6.59 to 28.79, P < 0.001), and have an organized plan or serious attempt (OR 13.83; 95% CI 5.99 to 31.94, P < 0.001). Other correlates of NSSI and no self-harm or suicidal ideation included having an acute stressor (OR 2.50; 95% CI 1.87 to 3.35, P < 0.001), aggression or impulsivity (OR 2.70; 95% CI 2.00 to 3.65, P < 0.001), and having access to firearms (OR 2.64; 95% CI 1.05 to 6.66, P < 0.05).
When comparing NSSI to SA, people with SA were more likely to have single marital status (OR 1.63; 95% CI 1.20 to 2.22, P < 0.01), MDD (OR 3.05; 95% CI 2.23 to 4.17, P < 0.001), passive suicidal ideation (OR 4.87; 95% CI 3.40 to 6.96, P < 0.001), active suicidal ideation (OR 8.84; 95% CI 5.26 to 14.85, P < 0.001), an organized plan or made a serious attempt (OR 21.11; 95% CI 11.82 to 37.69, P < 0.001), and previous SA or psychiatric care (OR 1.89; 95% CI 1.36 to 2.64, P < 0.001). Other significant correlates of SA, compared with NSSI, included experiencing an acute stressor (OR 1.44; 95% CI 1.05 to 1.99, P < 0.05) and lacking social support (OR 1.62; 95% CI 1.18 to 2.22, P < 0.001).
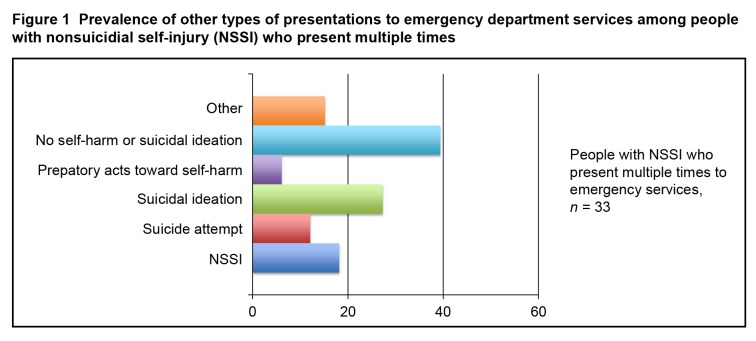
Figure 1 illustrates the other types of presentations to ED services among people with NSSI who present multiple times. The majority of people with NSSI (83.7%) present only once to ED services, while only 16.3% present multiple times. Further, self-harm presentations seemed to change over time. Among multiple presenters with NSSI, 18.2% present with repeat NSSI, 12.1% present with SA, 27.3% present with suicidal ideation, 6.1% present with preparatory acts toward self-harm, 39.4% present with no self-harm or suicidal ideation, and 15.2% present for other reasons.
Figure 1.
Prevalence of other types of presentations to emergency department services among people with nonsuicidial self-injury (NSSI) who present multiple times
Discussion
Three novel findings emerged from our study. First, consistent with previous research, NSSI was found to be associated with early life adversity and psychiatric comorbidity. Second, SA and NSSI differed on several correlates, particularly those related to suicidal ideation and behaviour, but they also had some similarities. Finally, most people with NSSI present only once to ED services and their self-harm presentations seemed to change over time. These findings have important clinical implications in the risk assessment of people who present to ED services with NSSI, and may help to better inform the study and treatment of self-harm behaviour.
This is the first study to examine the correlates and risk factors of NSSI, compared with SA, among adults in an ED sample. The finding that people who present to ED services with NSSI are more likely to have experienced early life adversity and have psychiatric comorbidity than people who present with no self-harm or suicidal ideation is consistent with the current literature. Previous research has found that NSSI is associated with childhood physical and sexual abuse,12,13 having an anxiety disorder,10,23 depression,4,5,10 SUD,9,10 aggression,5 and suicidal ideation.4,5 However, the only study that directly compared the correlates of SA and NSSI was that of Nock and Kessler.10
Consistent with the findings of Nock and Kessler,10 we found numerous similar correlates between SA and NSSI. We found that people who present with NSSI and those with SA were equally likely to have childhood physical and sexual abuse, aggression, an anxiety disorder, and a SUD. Similarly, Nock and Kessler10 found that all anxiety disorders (except simple phobia), alcohol use disorders, and physical abuse were equally likely to occur regardless of intent of self-harm.10
However, Nock and Kessler did find that drug use disorders and multiple incidents of sexual molestation were more strongly associated with SA. These differences in findings may be because Nock and Kessler10 examined specific types of SUDs and child abuse, while our study examined more broad categories of SUDs and child abuse.10
Regarding correlates more strongly associated with SA than NSSI, both our study and that of Nock and Kessler10 found a higher likelihood of MDD among people with SA, compared with NSSI.10 Further, Nock and Kessler10 found that higher comorbidity10 (3 or more mental disorders) was more strongly associated with SA than NSSI. Although, we did not examine the amount of comorbid disorders per se, we found that SA was more strongly associated with having a previous attempt or psychiatric care. Perhaps both studies are tapping into similar constructs of severity where people who have a higher amount of comorbidity also are likely to have previous psychiatric care.
Additional analyses also seem to suggest that the SA group tends to have a more worrisome profile than the NSSI group. We found that people who presented with SA were more likely to have an organized plan or serious attempt, lack social support, have experienced an acute stressor, and have active and passive suicidal ideation, compared with those who present with NSSI. Previous work also supports the view that SA is more strongly associated with suicidal ideation and death by suicide than NSSI. Prior research has demonstrated that SA, where the person intended to die, is a stronger risk factor for future death by suicide, compared with NSSI.24–28
Finally, our study found that most people with NSSI present only once to ED services and that self-harm presentations seemed to change over time. The prevalence of multiple presentations to ED services was 16.4% (n = 33) among people who presented with NSSI and 20% (n = 803) among the entire sample of those presenting to ED services. These numbers are consistent with previous studies done in the United Kingdom that have found the prevalence of representations with self-harm to the same general hospital within a year of between 15% and 25%.24,29 However, these studies did not classify the intent of the self-harm as either SA or NSSI; therefore, the prevalence of re-presentations among people with NSSI is unknown. These findings have important clinical implications in the risk assessment and treatment of people who present to ED services with NSSI. It is also important that treatment providers not trivialize the presentation of NSSI. For example, people who present with superficial forearm lacerations may historically be considered less at risk for future suicidal outcomes than people presenting with SAs. Education to psychiatrists and ED staff should reflect that these people have many similarities with people who are suicidal, and may well indeed engage in more lethal acts in the near future. Service provision should mirror this as well, providing comprehensive outpatient psychiatric support for this at-risk group. Future research is needed to determine what specific interventions would be most effective at preventing future self-harm and suicide.
Further, we found that, among people with NSSI who present multiple times to ED services, their other types of presentations vary. For example, only 18.2% included a repeat presentation with NSSI. The finding that presentations of self-harm vary over time, and that people with NSSI present to ED services with concerns other than additional NSSI, contributes further to the findings of previous studies. Other research has shown that methods and motivations for self-harm change over time, and that many different motivations may occur in the same episode.30–33 In addition, Cox et al5 in a longitudinal study, found that a history of NSSI predicted future SA, and that SA after baseline predicted future NSSI. Similarly, other studies have found that people who frequently engage in NSSI are more likely to attempt suicide.8,14,16 Taken together, this line of research supports the argument that the intent of self-harm behaviour varies over time, and that perhaps people who engage in NSSI and people who engage in SA are not 2 distinct populations.
Our study used C-CASA definitions of NSSI and SA, rather than the DSM-5 Section III definitions of NSSI and suicidal behaviour disorder. Where C-CASA and DSM-5 differ is that C-CASA only describes one event of self-harm, while DSM-5 requires at least 5 incidences of NSSI in the past year. Further, DSM-5 goes into more detail when describing the incidents of self-harm than C-CASA. However, the C-CASA definitions of NSSI and SA are also similar to DSM-5 definitions of NSSI and suicidal behaviour disorder. They both describe the intent of the self-harm. Both DSM-5 and C-CASA have criteria where the person must intend to die from the act of self-harm to be classified as SA. Similarly, both DSM-5 and C-CASA include criteria for NSSI where the self-harm was intended for other reasons, such as to relieve distress or to effect change in others or the environment. Part of the motivation for creating standardized definitions for NSSI and SA in both the DSM-5 and C-CASA stem from a long history of self-harm terms that mean different things to different people. Numerous terms have existed over the years, including deliberate self-harm, self-mutilation, suicidal gesture, and parasuicide, among others. It is difficult to comment on how older classifications mesh with DSM-5 and C-CASA definitions of NSSI and SA, as previous terms differed in meaning depending on the study. The study and classification of SIB continues to be controversial. The DSM has proposed a subclassification of self-harm depending on intent, whereas other groups advocate for the use of the broader term self-harm, regardless of intent, to encompass both NSSI and SA. Our study aims to contribute clinical findings that may inform this debate around nomenclature.
The current findings should be interpreted within the context of certain limitations. The first limitation is that we were unable to draw conclusions about the risk for completed suicide among people who presented with NSSI and SA. A second limitation of our study is its cross-sectional design, because we are unable to make inferences about the temporality of correlates and self-harm behaviour. Future research can address this limitation by using a longitudinal design. The third limitation of our study is that, although the 2 tertiary care hospitals in Manitoba receive the most ED presentations with self-harm, it is possible that some people may have presented to another hospital. A fourth limitation is that our study did not directly evaluate DSM-5 definitions of NSSI and suicidal behaviour disorder. The fifth limitation is that the SAFE database does not contain information on personality disorders. Future studies should examine the influence of personality disorders on NSSI and SA in addition to other mental disorders. A final limitation is that, although physicians conducted the psychiatric assessments, the diagnoses generated were not based on standardized structured clinical interviews, rather they were based on a standard psychiatric interview conducted by psychiatric residents at ED services.
Conclusion
Our study, together with previous research, supports the finding that NSSI is associated with early life adversity and psychiatric comorbidity. Our study further extends this finding to conclude that SA appears to have the more worrisome profile, compared with NSSI. In addition, it appears that most people with NSSI present only once to ED services and that, when those with NSSI present multiple times to ED services, their reason for presentation changes over time. These findings emphasize that the type of self-harm that people engage in is not fixed and that the same people may engage in both SA and NSSI. Although it appears as though people who engage in SA are more likely to have negative correlates than those who engage in NSSI, future research is needed to clarify whether these groups are truly distinct.
Acknowledgments
The authors acknowledge Daniel Palitsky, Cara Katz, and Will Husarewycz, in the Department of Psychiatry, University of Manitoba, for data entry and management; Morgan Rathwell, in the Department of Psychology, The University of Western Ontario, London, Ontario, for assistance with manuscript preparation; and the residents, in the Department of Psychiatry at the University of Manitoba, for their help with data collection.
The Suicide Assessment Form for Emergency Psychiatry (commonly referred to as SAFE) database is part of a research program at the University of Manitoba in the Department of Psychiatry. The database is the property of the University of Manitoba and resides within the Laboratory of the Manitoba Population Mental Health Research Group. Requests for access should be sent to the corresponding author, Dr Bolton.
Preparation of this article was supported by a Canadian Institutes of Health Research (CIHR) Frederick Banting and Charles Best Doctoral Award, and a Manitoba Graduate Scholarship (Hayley Chartrand), a University of Manitoba Graduate Fellowship (Joanna Bhaskaran), a CIHR New Investigator Award and Manitoba Health Research Council (MHRC) Establishment Award (Dr Bolton), and an MHRC Chair Award (Dr Sareen).
Abbreviations
- C-CASA
Columbia Classification Algorithm of Suicide Assessment
- CL
consultation-liaison
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ED
emergency department
- MDD
major depressive disorder
- NSSI
nonsuicidal self-injury
- SA
suicide attempt
- SAFE
Suicide Assessment Form in Emergency Psychiatry
- SIB
self-injurious behaviour
- SUD
substance use disorder
Footnotes
An abridged version of these results was presented at the 2013 Conference of the Canadian Association of Suicide Prevention. Winnipeg, MB; the 2012 Conference of the Canadian Psychiatric Association, Montreal, QC; and the 2012 Annual Scientific Symposium of the Canadian Academy of Psychiatric Epidemiology, Montreal, QC.
References
- 1.Nock MK. Why do people hurt themselves?: new insights into the nature and functions of self-injury. Curr Dir Psychol Sci. 2009;18(2):78–83. doi: 10.1111/j.1467-8721.2009.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kapur N, Cooper J, O’Connor RC, et al. Non-suicidal self-injury v attempted suicide: new diagnosis or false dichotomy? Br J Psychiatry. 2013;202(5):326–328. doi: 10.1192/bjp.bp.112.116111. [DOI] [PubMed] [Google Scholar]
- 3.Nock MK. Self-injury. Annu Rev Clin Psychol. 2010;6:339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- 4.Cox LJ, Stanley BH, Melhem NM, et al. A longitudinal study of nonsuicidal self-injury in offspring at high risk for mood disorder. J Clin Psychiatry. 2012;73(06):821–828. doi: 10.4088/JCP.11m07250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox LJ, Stanley BH, Melhem NM, et al. Familial and individual correlates of nonsuicidal self-injury in the offspring of mood-disordered parents. J Clin Psychiatry. 2012;73(6):813–820. doi: 10.4088/JCP.11m07196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joyce PR, Light KJ, Rowe SL, et al. Self-mutilation and suicide attempts: relationships to bipolar disorder, borderline personality disorder, temperament and character. Aust N Z J Psychiatry. 2010;44(3):250–257. doi: 10.3109/00048670903487159. [DOI] [PubMed] [Google Scholar]
- 7.Parker G, Malhi G, Mitchell P, et al. Self-harming in depressed patients: pattern analysis. Aust N Z J Psychiatry. 2005;39(10):899–906. doi: 10.1080/j.1440-1614.2005.01662.x. [DOI] [PubMed] [Google Scholar]
- 8.Sansone RA, Songer DA, Sellbom M. The relationship between suicide attempts and low-lethal self-harm behavior among psychiatric inpatients. J Psychiatr Pract. 2006;12(3):148–152. doi: 10.1097/00131746-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Herpertz S. Self-injurious behaviour. Psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatr Scand. 1995;91(1):57–68. doi: 10.1111/j.1600-0447.1995.tb09743.x. [DOI] [PubMed] [Google Scholar]
- 10.Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115(3):616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- 11.Romans SE, Martin JL, Anderson JC, et al. Factors that mediate between child sexual abuse and adult psychological outcome. Psychol Med. 1995;25(1):127–142. doi: 10.1017/s0033291700028154. [DOI] [PubMed] [Google Scholar]
- 12.Gladstone GL, Parker GB, Mitchell PB, et al. Implications of childhood trauma for depressed women: an analysis of pathways from childhood sexual abuse to deliberate self-harm and revictimization. Am J Psychiatry. 2004;161(8):1417–1425. doi: 10.1176/appi.ajp.161.8.1417. [DOI] [PubMed] [Google Scholar]
- 13.Boxer P. Variations in risk and treatment factors among adolescents engaging in different types of deliberate self-harm in an inpatient sample. J Clin Child Adolesc Psychol. 2010;39(4):470–480. doi: 10.1080/15374416.2010.486302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cuellar J, Curry TR. The prevalence and comorbidity between delinquency, drug abuse, suicide attempts, physical and sexual abuse, and self-mutilation among delinquent Hispanic females. Hisp J Behav Sci. 2007;29(1):68–82. [Google Scholar]
- 15.Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychol Med. 2011;41(9):1981–1986. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- 16.Mangnall J, Yurkovich E. A literature review of deliberate self-harm. Perspect Psychiatr Care. 2008;44(3):175–184. doi: 10.1111/j.1744-6163.2008.00172.x. [DOI] [PubMed] [Google Scholar]
- 17.Posner K, Oquendo MA, Gould M, et al. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Department of Health and Human Services. Food and Drug Administration (FDA) Center for Drug Evaluation and Research (CDER) Guidance for industry. Suicidal ideation and behavior: prospective assessment of occurrence in clinical trials. Rockville (MD): FDA CDER; 2012. Aug, [revision 1]. Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM225130.pdf. [Google Scholar]
- 19.Bushe CJ, Savill NC. Suicide related events and attention deficit hyperactivity disorder treatments in children and adolescents: a meta-analysis of atomoxetine and methylphenidate comparator clinical trials. Child Adolesc Psychiatry Ment Health. 2013;7(1):19. doi: 10.1186/1753-2000-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emslie G, Kratochvil C, Vitiello B, et al. Treatment for Adolescents with Depression Study (TADS): safety results. J Am Acad Child Adolesc Psychiatry. 2006;45(12):1440–1455. doi: 10.1097/01.chi.0000240840.63737.1d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer RE, Salzman C, Youngstrom EA, et al. Suicidality and risk of suicide—definition, drug safety concerns, and a necessary target for drug development: a brief report. J Clin Psychiatry. 2010;71(8):1040–1046. doi: 10.4088/JCP.10cs06070ablu. [DOI] [PubMed] [Google Scholar]
- 22.Redden L, Pritchett Y, Robieson W, et al. Suicidality and divalproex sodium: analysis of controlled studies in multiple indications. Ann Gen Psychiatry. 2011;10(1):1. doi: 10.1186/1744-859X-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chartrand H, Sareen J, Toews M, et al. Suicide attempts versus nonsuicidal self-injury among individuals with anxiety disorders in a nationally representative sample. Depress Anxiety. 2012;29(3):172–179. doi: 10.1002/da.20882. [DOI] [PubMed] [Google Scholar]
- 24.Hawton K, Harriss L, Hall S, et al. Deliberate self-harm in Oxford, 1990–2000: a time of change in patient characteristics. Psychol Med. 2003;33(6):987–995. doi: 10.1017/s0033291703007943. [DOI] [PubMed] [Google Scholar]
- 25.Hjelmeland H. Verbally expressed intentions of parasuicide: II. Prediction of fatal and nonfatal repetition. Crisis. 1996;17(1):10–14. doi: 10.1027/0227-5910.17.1.10. [DOI] [PubMed] [Google Scholar]
- 26.Ostamo A, Lönnqvist J, Heinonen S, et al. Epidemiology of parasuicides in Finland. Psychiatr Fenn. 1991;22:181–189. [Google Scholar]
- 27.Lönnqvist J, Ostamo A. Suicide following the first suicide attempt: a five-year follow-up using a survival analysis. Psychiatr Fenn. 1992;22:179–179. [Google Scholar]
- 28.Owens D, Wood C, Greenwood DC, et al. Mortality and suicide after non-fatal self-poisoning: 16-year outcome study. Br J Psychiatry. 2005;187(5):470–475. doi: 10.1192/bjp.187.5.470. [DOI] [PubMed] [Google Scholar]
- 29.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 30.Lilley R, Owens D, Horrocks J, et al. Hospital care and repetition following self-harm: multicentre comparison of self-poisoning and self-injury. Br J Psychiatry. 2008;192(6):440–445. doi: 10.1192/bjp.bp.107.043380. [DOI] [PubMed] [Google Scholar]
- 31.Scoliers G, Portzky G, Madge N, et al. Reasons for adolescent deliberate self-harm: a cry of pain and/or a cry for help? Findings from the Child and Adolescent Self-harm in Europe (CASE) study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(8):601–607. doi: 10.1007/s00127-008-0469-z. [DOI] [PubMed] [Google Scholar]
- 32.Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354–358. doi: 10.1192/bjp.bp.109.070219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper J, Hunter C, Owen-Smith A, et al. “Well it’s like someone at the other end cares about you.” A qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm. Gen Hosp Psychiatry. 2011;33(2):166–176. doi: 10.1016/j.genhosppsych.2011.01.009. [DOI] [PubMed] [Google Scholar]