Abstract
Acetaminophen (APAP) is a widely used analgesic and antipyretic drug. Generally, the therapeutic dose of APAP is clinically safe, however, high doses of APAP can cause acute liver and kidney injury. Therefore, the majority of previous studies have focussed on elucidating the mechanisms of APAP-induced hepatotoxicity and nephrotoxicity, in addition to examining ways to treat these conditions in clinical cases. However, few studies have reported APAP-induced intoxication in human stem cells. Stem cells are important in cell proliferation, differentiation and repair during human development, particularly during fetal and child development. At present, whether APAP causes cytotoxic effects in human stem cells remains to be elucidated, therefore, the present study aimed to investigate the cellular effects of APAP treatment in human stem cells. The results of the present study revealed that high-dose APAP induced more marked cytotoxic effects in human mesenchymal stem cells (hMSCs) than in renal tubular cells. In addition, increased levels of hydrogen peroxide (H2O2), phosphorylation of c-Jun N-terminal kinase and p38, and activation of caspase-9/-3 cascade were observed in the APAP-treated hMSCs. By contrast, antioxidants, including vitamin C reduced APAP-induced augmentations in H2O2 levels, but did not inhibit the APAP-induced cytotoxic effects in the hMSCs. These results suggested that high doses of APAP may cause serious damage towards hMSCs.
Keywords: acetaminophen, c-Jun N-terminal kinase, caspase, human mesenchymal stem cells
Introduction
Acetaminophen (APAP) is commonly used as an analgesic and antipyretic agent (1–3), and is considered safe at therapeutic doses (4). It is readily available, and high doses of APAP may be provided to patients over a short time-period. However, APAP is the most common drug to cause clinical hepatotoxicity and nephrotoxicity in several countries (5–7). A number of studies have demonstrated that high-dose APAP (10–15 g) causes serious damage to liver and renal cells (8,9). High-dose APAP can increase the levels of reactive oxygen species (ROS), thus increasing cellular oxidative stress and causing liver and renal injury (10–12). Therefore, several studies have examined the ability of antioxidants to target high-dose APAP-induced liver and renal damage through the reduction of cellular ROS levels and oxidative stress (13–16). At present, N-acetylcysteine (NAC), an antioxidant, has been used to treat APAP-induced hepatotoxicity and nephrotoxicity in emergency cases (17–19).
In order to improve the understanding of the mechanisms underlying APAP-induced toxicity, several animal and cell models have been developed for hepatotoxic and nephrotoxic investigations. In general, high-dose APAP (>5 mM) is used to induce cell death in renal and liver cell models (20–26), and high-dose APAP (300–2,500 mg/kg) is used to induce liver and kidney damage in animal models (27–31). These studies have observed that APAP can stimulate apoptotic or necrotic death pathway activation in different cell models (24,31,32). In addition, several cellular effects and signals are stimulated in high-dose APAP-treated cells, including increased levels of ROS and oxidative stress, decreased levels of glutathione, induction of the mitogen-activated protein kinase (MAPK) signaling pathway and activation of caspase cascades (21,25,26,31,33–36).
High-dose APAP-induced clinical intoxication is predominantly found in liver and renal cells; therefore, the majority of previous studies have focussed on the mechanisms underlying high-dose APAP-triggered liver and renal injury (17,37,38). Furthermore, certain studies have indicated that APAP can exhibit antitumor activities in certain tumor types, including breast cancer, liver cancer and neuroblastoma (26,39–43). These studies also demonstrated that APAP-induced cell death is linked to nuclear factor-κB, the B-cell lymphoma 2 family or glycogen synthase kinase-3 in different tumor cells.
At present, with the exception of liver, renal and tumor cells, almost no cellular effects have been reported in other human cells following APAP therapy (10,12,39–43). Therefore, whether APAP causes toxic cellular effects in other human cells remains to be elucidated. APAP can freely cross the placenta (44,45); thus, high-dose APAP can cause cellular damage in maternal as well as fetal liver cells. In addition, several previous studies have suggested that stem cells are critical during fetal development (46–48). However, whether APAP can induce toxic cellular effects in stem cells during fetal development remains to be elucidated. APAP-induced cellular effects in human stem cells have not been reported previously, therefore, the aim of the present study was to investigate the cellular responses of APAP-treated human stem cells.
Based on the above-mentioned studies, the aim of our study was to determine the cytotoxic effects of APAP on human mesenchymal stem cells (hMSCs). Furthermore, the ROS levels (H2O2 and O2−) and the role of caspase death pathways and MAPK signaling pathways were also determined in the APAP-treated hMSCs.
Materials and methods
Chemicals
Caspase-3, caspase-8, caspase-9, cleaved caspase-3, cleaved caspase-8 and cleaved caspase-9 monoclonal antibodies were purchased from Cell Signaling Technology, Inc. (Danvers, MA, USA). Extracellular-signal-regulated kinase (ERK), p38, JNK, phosphorylated (p)-p38, p-ERK and p-JNK monoclonal antibodies were purchased from BD Transduction Laboratories (San Diego, CA, USA). Secondary mouse anti-human antibody was purchased from GE Healthcare (Piscataway, NJ, USA). Tubulin monoclonal antibody, luminol, lucigenin, vitamin C and Hoechst 33342 were purchased from Sigma-Aldrich (St. Louis, MO, USA). The 3-(4,5-dimethylthiazol-2-yl)-2,5-di-phenyltetrazolium bromide (MTT) kits were purchased from Bio Basic, Inc. (Markham, ON, Canada). Fetal bovine serum, Dulbecco’s modified Eagle’s medium (DMEM), DMEM-low glucose (DMEM-LG), non-essential amino acid L-glutamine and penicillin/streptomycin were obtained from GE Healthcare Life Sciences (Logan, UT, USA).
Cells and cell cultures
The NRK-52E rat renal tubular cells were obtained from Bioresource Collection and Research Center (Hsinchu, Taiwan). The hMSCs (Bioresources Collection and Research Center, Hsin Chu, Taiwan) were cultured in DMEM-LG supplemented with 10% fetal bovine serum, 2 mM L-glutamine, 100 IU/ml penicillin/streptomycin and 0.1 mM non-essential amino acids. The NRK-52E cells were cultured in DMEM supplemented with 10% fetal bovine serum, 2 mM L-glutamine, 100 IU/ml penicillin/streptomycin, and 0.1 mM non-essential amino acids. The two cell lines were maintained in a humidified 37°C incubator containing 5% carbon dioxide.
Cell survival rate assay
The survival rates of the NRK-52E and hMSCs were determined using MTT assay kits, as described in a previous study (26). Briefly, 1,500 cells were cultured in each well of 96-well plates at 37°C. After 24 h, the cells were divided into control and experimental groups and the cell survival rates were examined for 4 days. Each day, 100 μl MTT (0.005 g/ml in PBS) were added to each well, according to the manufacturer’s instructions. After 3 h incubation at 37°C, the absorbance (570 nm) was measured under a multi-well enzyme-linked immunosorbent assay reader (SpectraMax Paradigm Multi-Mode Microplate Reader; Molecular Devices, Sunnyvale, CA, USA). The cell survival rate was determined using the following formula: A570 experimental group / A570 control group × 100%.
Observation of nuclear condensation
The examine the presence of apoptotic cells exhibiting nuclear condensation, a Hoechst 33342 staining method was used (26,49). The cells (approximately 104) in the control group and experimental group were treated with 10 μg/ml Hoechst 33342 for 5 min. Nuclear condensation was observed under an Olympus BX61 fluorescent microscope (excitation, 352 nm; emission, 450 nm; Olympus Corporation, Tokyo, Japan).
Sodium dodecyl sulfate (SDS) electrophoresis and western blot analysis
SDS electrophoresis and western blot analysis were performed, according to previous described methods (50,51). Briefly, the cells (approximately 107) were treated with radioimmunoprecipitation assay lysis buffer (50 mM Tris-HCl, 120 mM NaCl, 1 mM EDTA, 1% NP-40, pH 7.5) and centrifuged (16,000 × g) for 10 min at 4°C. The protein was collected from the supernatant layer and the concentration was determined using a BSA Protein Assay Reagent kit (Pierce, Rockford, IL, USA) with a DU-530 spectrophotometer (OD562 nm; Beckman Coulter, Inc., Brea, CA, USA). Equal quantities of protein (60 μg) were separated on a SDS-polyacrylamide gel (13.3%) using GHE320 Mini-STD Vertical Gel Electrophoresis Tank and transferred onto a polyvinylidene difluoride membrane (Millipore, Billerica, MA, USA). The membranes were blocked with 5% milk for 2 h at 25°C and then washed with phosphate-buffered saline (PBS). The membranes were incubated with 5% milk containing the primary antibodies (1:500) for 2 h at 25°C. The membranes were then washed with PBS buffer and treated with secondary antibodies (1:2,000) for 1 h at 25°C. Finally, the proteins were detected using 400 μl Western Lightning Chemiluminescence Reagent Plus (PerkinElmer, Inc., Waltham, MA, USA).
Determination of oxygen (O2−) and H2O2 levels
The levels of O2− and H2O2 were examined using a lucigenin-amplified chemiluminescence technique, as previously described (52,53). Briefly, to determine the levels of H2O2, 200 μl of the sample (containing 8,000 cells) was treated with 0.2 mmol/l luminol solution (100 μl), followed by examination using a chemiluminescence analyzing system (CLA-FS1; Tohoku Electronic Industrial Co., Ltd., Sendai, Miyagi, Japan). Similarly, to determine the levels of O2−, 200 μl of the sample (containing 8,000 cells) was treated with 0.1 mmol/l of the lucigenin solution (500 μl), followed by examination using the CLA-FS1 system.
Statistical analysis
Data were calculated from four independent triplicate experiments and are presented as the means ± standard deviation. Statistical differences between 2 groups were analyzed using the Student’s t-test. A P-value <0.05 was considered to indicate a statistically significant difference.
Results
APAP decreases the survival of kidney tubular epithelial cells and hMSCs
Previous studies have demonstrated that high-dose APAP (> 5 mM) can decrease the cell survival rate of liver and kidney cells (20–26). Similar to these studies, the present study revealed that high-dose APAP (7.94 mM) reduced cell survival in the NRK-52E kidney tubular epithelial cells (Fig. 1A). Until now, the cytotoxic effects of APAP treatment in human stem cells have not been investigated. The present study is the first, to be best of our knowledge, to demonstrate that high-dose APAP reduced the survival rate of hMSCs (Fig. 1B). The results following low-dose APAP treatment (0.794 mM) revealed no significant cytotoxic effects in the NRK-52E cells or the hMSCs (Fig. 1). The survival rates following high-dose APAP therapy between the NRK-52E cells and hMSCs were also compared. The survival rate on day 3 was ~60% in the APAP-treated NRK-52E cells (Fig. 1A) and ~30% in the APAP-treated hMSCs (Fig. 1B). Therefore, high-dose APAP exerted a more marked cytotoxic effect in the hMSCs, compared with the NRK-52E cells. These findings indicated that APAP induced more damage in the stem cells than in the kidney cells.
Figure 1.
Cell survival rates following treatment with APAP. (A) NRK-52E cells were treated with 7.94 mM (high-dose) and 0.794 mM APAP. (B) hMSCs were treated with 7.94 mM (high-dose) and 0.794 mM APAP. The survival rate was lower in the 7.94 mM APAP-treated hMSCs, compared with the 7.94 mM APAP-treated NRK-52E cells. Data was calculated from four independent experiments and is presented as the means ± standard deviation. The statistical differences between 7.94 mM-treated and 0.794 mM-treated group were analyzed by the Student’s t-test. *P<0.05. APAP, acetaminophen; hMSC, human mesenchymal stem cell.
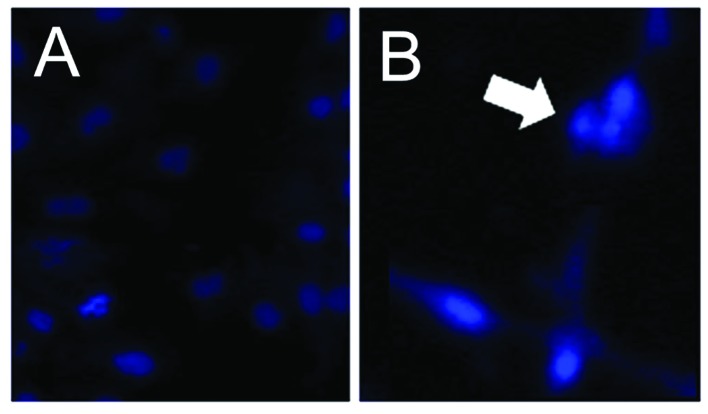
High-dose APAP induces apoptosis and activates the caspase-9/-3 cascade in hMSCs
The present study subsequently examined whether the apoptotic death pathway is involved in hMSC death following high-dose APAP treatment. Upon examination of the nuclear morphology, nuclear condensation, an apoptotic feature (26,54), was identified in the APAP-treated hMSCs (Fig. 2). Thus, the results demonstrated that high-dose APAP induced apoptosis in the hMSCs. Caspase activation triggers apoptosis (49,55). Two major caspase signaling pathways are associated with the apoptosis-caspase-9/-3 and caspase-8/-3 cascades (26,56). Cleaved caspase-3, -8 and -9 were observed following 3 days of APAP treatment using western blot analysis. As shown in Fig. 3, the levels of cleaved caspase-3 and -9 were increased in the high-dose APAP-treated hMSCs (Fig. 3A, lane 3 and Fig. 3C, lane 3); however, the levels of cleaved caspase-8 were unchanged (Fig. 3B). Therefore, these results suggested that high-dose APAP stimulated apoptosis in the hMSCs via the caspase-9/-3 signaling pathway.
Figure 2.
Nuclear condensation. (A) Control group. (B) APAP-treated group. hMSCs were treated with 7.94 mM APAP for 2 days, nuclear condensation (white arrow) was observed in the APAP-treated cells under a phase-contrast microscope at magnifications of x400. APAP, acetaminophen; hMSC, human mesenchymal stem cell.
Figure 3.
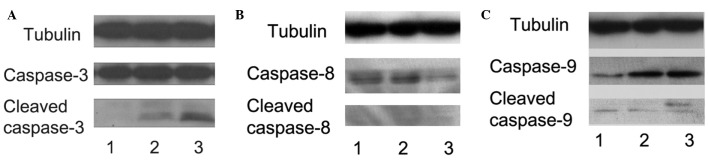
Western blot analysis to determine caspase activation. The activities of (A) caspase-3, (B) caspase-8 and (C) caspase-9 were analyzed on day 3 in the control (lane 1), 0.794 mM APAP-treated (lane 2) and 7.94 mM APAP-treated (lane 3) cells. Ceaved caspase-3 and cleaved caspase-9 were markedly increased in the 7.94 mM APAP-treated cells. APAP, acetaminophen; hMSC, human mesenchymal stem cell.
APAP induces the phosphorylation of JNK and p38 in hMSCs
APAP can induce liver injury via the MAPK signaling pathways (57,58). In the present study, whether APAP also activates the MAPK signaling pathways in hMSCs was examined. JNK, p38 and ERK belong to the MAPK family (59,60). Therefore, the phosphorylation levels of JNK, p38 and ERK were examined using western blot analysis in the present study. As shown in Fig. 4, the levels of p- JNK and p-p38 were increased in the high-dose APAP-treated cells (Fig. 4B, lane 3), compared with the control group (Fig. 4B, lane 1). However, ERK phosphorylation was not observed in the APAP-treated cells (Fig. 4B). These experimental results suggested that APAP activated the JNK/p38 MAPK signaling pathways, but not the ERK MAPK signaling pathway, in the hMSCs.
Figure 4.
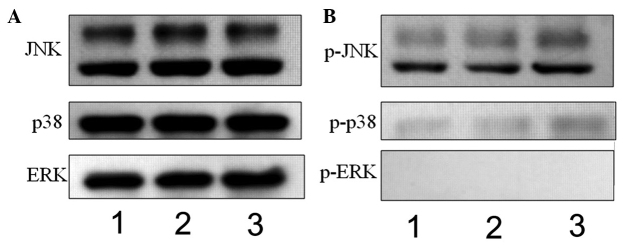
Western blot analysis to determine the expression of mitogen-activated protein kinases, (JNK, p38 and ERK) and their phosphorylation. (A) JNK, p38 and ERK, and (B) p-JNK, p-p38 and p-ERK were observed at 30 min in the control (lane 1), 0.794 mM APAP-treated (lane 2) and 7.94 mM APAP-treated (lane 3) cells. The levels of p-JNK and p-p38 were increased in the 7.94 mM APAP-treated cells. JNK, c-Jun N-terminal kinase; ERK, extracellular signal-regulated kinase; p-, phosphorylated; APAP, acetaminophen.
APAP stimulates increases in H2O2 levels in hMSCs
Previous studies have demonstrated that APAP can induce increases in ROS levels (61,62). In addition, a previous study reported that augmentations in H2O2 levels are found in APAP-treated kidney cells (26). O2− and H2O2 belong to the ROS family and are normally present in living cells, therefore, the levels of O2− and H2O2 were examined in the present study. As shown in Fig. 5, the O2− levels remained constant (Fig. 5A), whereas increases in H2O2 were found in the APAP-treated hMSCs (Fig. 5B), whereas. Therefore, the APAP-induced augmentation of ROS was associated with H2O2, but not O2−, in the hMSCs.
Figure 5.
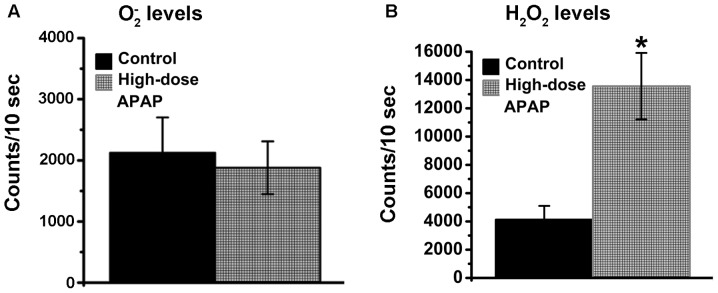
O2− and H2O2 levels. (A) O2− levels were determined in the control and high-dose APAP-treated cells. (B) H2O2 levels were determined in the control and high-dose APAP-treated cells. The levels of O2− and H2O2 levels were measured following 1 h treatment. Data were analyzed from four independent experiments and are presented as the means ± standard deviation. *P<0.05, compared to the control group. O2−, oxygen; H2O2 hydrogen peroxide; APAP, acetaminophen.
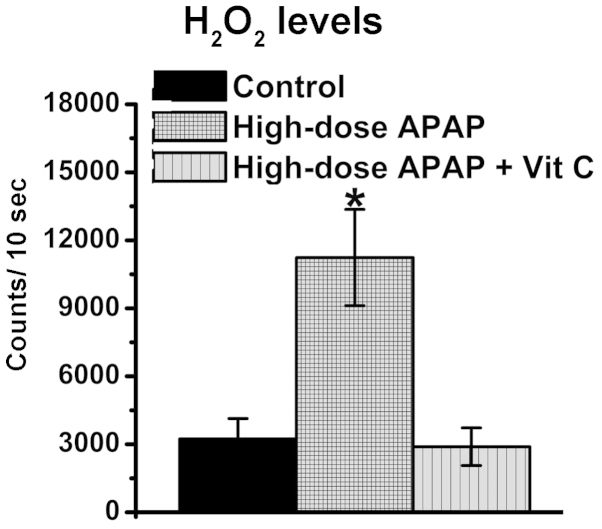
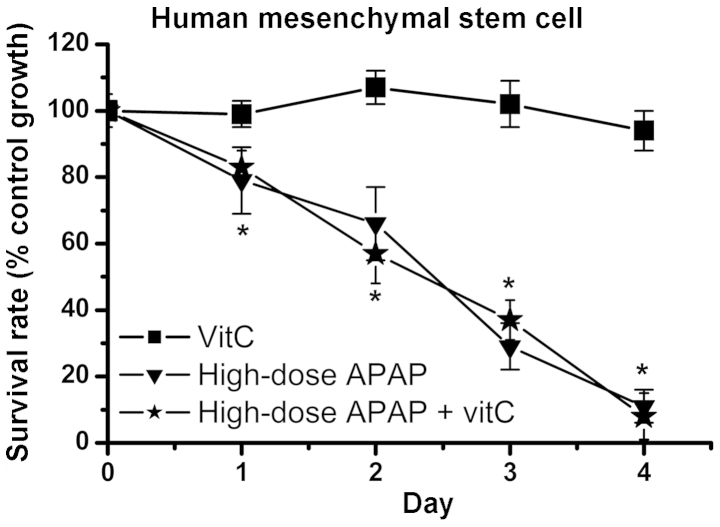
Vitamin C reduces APAP-induced increases in H2O2 levels, but does not inhibit APAP-induced cytotoxicity in hMSCs
APAP can stimulate elevations in ROS levels causing cellular oxidative stress, which results in hepatotoxicity and nephrotoxicity (16,63). Therefore, several antioxidant drugs that prevent APAP-induced cellular damage have been investigated (64–68). Vitamin C, an antioxidant, was used to inhibit the cytotoxic effects of APAP in the hMSCs in the present study. The resulting data revealed that vitamin C effectively reduced the increases in H2O2 levels (Fig. 6). Therefore, vitamin C had an antioxidative function in decreasing cellular oxidative stress. Subsequently, whether vitamin C inhibited APAP-induced cytotoxicity in the hMSCs was determined. As shown in Fig. 7, cell survival rates were markedly decreased in the high-dose APAP-treated group and high-dose APAP + vitamin C-treated group, compared to the control group. These findings indicated that inhibition of the increases in H2O2 did not prevent APAP-induced cytotoxicity in the hMSCs.
Figure 6.
H2O2 levels. The levels of H2O2 levels were determined in the control, high-dose APAP-treated and high-dose APAP + 0.5 mM vit C-treated cells. The levels of H2O2 were measured after 1 h treatment. Data were analyzed from four independent experiments and are presented as the means ± standard deviation.*P<0.05, compared to the control group. H2O2 hydrogen peroxide; APAP, acetaminophen; vit C, vitamin C.
Figure 7.
Cell survival rates. The hMSCs were treated with 0.5 mM vit C, high-dose APAP, and high-dose APAP +0.5 mM vit C-treated cells. No significant difference in survival rates were observed between the APAP-treated and APAP + vit C-treated cells. Data were calculated from four independent experiments and are presented as the means ± standard deviation.*P<0.05, compared to vitamin C alone group; both APAP group and APAP plus vitamin C group have significant difference. hMSC, human mesenchymal stem cell; APAP, acetaminophen; vit C, vitamin C.
The present study was the first, to the best of our knowledge, to demonstrate that high-dose APAP reduced the survival rate of hMSCs, induced the JNK/p38 MAPK signaling pathways and activated the caspase-9/-3 apoptotic death pathway. In addition, the inhibition of increases in the levels of H2O2 did not rescue the cell survival rate following APAP treatment.
Discussion
APAP is regarded a safe medicine applied widely to treat pain and fever in clinical cases (69–71). However, high-dose APAP can cause clinical hepatotoxicity and nephrotoxicity (5–7). Previous studies have demonstrated that APAP has antitumor effects in various types of cancer, including liver cancer, breast cancer and neuroblastoma (26,39,43). These studies indicated that APAP can induce cytotoxicity in liver, renal and tumor cells. Therefore, the majority of studies investigating APAP-induced cytotoxic mechanisms have focused on renal, liver and tumor cells (26,39,43,58,62,72,73). The present study was the first, to the best of our knowledge, to demonstrate that APAP also induces cytotoxicity in hMSCs, suggesting APAP not only triggers clinical hepatotoxicity and nephrotoxicity, but it is also harmful to stem cells. Notably, as shown in Fig. 1, the present study demonstrated that APAP exerts a more marked cytotoxic effect in hMSCs than in renal tubular cells. Stem cells are important in fetal development, and stem cell dysfunction may be harmful to fetus growth. In addition, previous studies have demonstrated that APAP can cross the placenta (44,45). Therefore, the results of the present study suggested the requirement for caution when treating pregnant females with APAP for pain and fever.
The activation of apoptosis and necrosis have been found in liver and renal cells following APAP treatment in different animal and cell models (31,32). The majority of studies have reported that APAP-induced apoptotic death in liver and renal cells is associated with caspase-3 activation (74–76). There are two major caspase cascades, caspase-9/-3 and caspase-8/-3 cascades (26,54,55). The caspase-9/-3 cascade is linked to mitochondrial dysfunction and the caspase-8/-3 casecade is associated with death receptor signal transduction. APAP-induced liver and renal injury has been observed to trigger the caspase-9/-3 pathway (11,77). In addition, activation of the caspase-9/-3 cascade is also found in APAP-treated hepatoma cells (26). In the present study, the data revealed that APAP activated caspase-9 and -3 signaling in the hMSCs but did not activate caspase-8 (Fig. 3). Taken together, these studies indicated that mitochondrial damage is an important factor that results in cell death in renal cells, liver cells, hepatoma cells and stem cells following APAP treatment.
The MAPK signaling pathways undergo three major phosphorylation reactions: ERK, JNK and p38 phosphorylation (59,60). Previous studies have demonstrated that APAP can induce acute liver injury via the JNK and ERK phosphorylation signaling pathways (57,58). A previous study found that APAP-induced liver damage not only activates JNK and ERK phosphorylation, but also induces p38 phosphorylation in mouse models (78), although the common signaling pathways are the ERK and JNK phosphorylation pathways. In the present study, JNK and p38 phosphorylation were observed in the APAP-treated hMSCs, however, ERK phosphorylation was not observed (Fig. 4). The observation of ERK phosphorylation in the APAP-treated liver cells, but not in the stem cells remains to be elucidated and requires investigation in the future.
Previous studies have demonstrated that high-dose APAP-induced hepatotoxicity and nephrotoxicity are associated with increases in ROS levels (25,79–81). Severalantioxidants against APAP-induced cytotoxicity have been investigated, including green tea, honey, tofu and NAC (13,80,82–85). O2− and H2O2 belong to the ROS family and are produced by the electron transport chain. O2− can be removed by superoxide dismutase, and H2O2 can be removed by glutathione system (19,26,85). NAC, a precursor for glutathione synthesis, can effectively reduce H2O2 levels and has been applied as a treatment method for APAP-induced hepatotoxicity and nephrotoxicity in clinical cases (17–19). The levels of O2− and H2O2 can be determined in APAP-treated stem cells. The present study demonstrated that APAP stimulated increases in the levels of H2O2, but not O2−, in human stem cells. This result is similar to a previous study, in which only increases in H2O2 levels were found in APAP-treated Hep3B cells (26). In addition, the present study further demonstrated that vitamin C effectively reduced APAP-induced elevations in H2O2, but does not inhibit APAP-induced cytotoxicity, in human cells. This result indicated that there are unknown cellular effects, in addition to augmentations in the levels of ROS, resulting in APAP-induced cytotoxicity in human stem cells. The present study demonstrated that antioxidants agents prevented APAP-induced damage in liver and renal cells, but not in stem cells.
In conclusion, this study was the first, to the best of our knowledge, to demonstrate that APAP induced the p38/JNK MAPK signaling pathway, activated the caspase-9/-3 cascade and decreased survival rate in human stem cells. The present study also revealed that APAP-induced cytotoxic effects were more marked in stem cells than in renal cells, and antioxidants did not prevent stem cell damage following APAP treatment.
Acknowledgments
This study was supported in part by the Ministry of Science and Technology (MOST103 2320-B-039-052-MY3), the National Health Research Institutes (NHRI-EX102-10245BI) and the Taipei Tzu Chi Hospital (TCRD-TPE-102-26 and TCRD-TPE-103-48).
References
- 1.Cuzzolin L, Antonucci R, Fanos V. Paracetamol (acetaminophen) efficacy and safety in the newborn. Curr Drug Metab. 2013;14:178–185. [PubMed] [Google Scholar]
- 2.Klotz U. Paracetamol (acetaminophen) - a popular and widely used nonopioid analgesic. Drug Res. 2012;62:355–359. doi: 10.1055/s-0032-1321785. [DOI] [PubMed] [Google Scholar]
- 3.Section on Clinical Pharmacology Therapeutics, Committee on Drugs. Sullivan JE, Farrar HC. Fever and antipyretic use in children. Pediatrics. 2011;127:580–587. doi: 10.1542/peds.2010-3852. [DOI] [PubMed] [Google Scholar]
- 4.Rumack BH. Acetaminophen misconceptions. Hepatology. 2004;40:10–15. doi: 10.1002/hep.20300. [DOI] [PubMed] [Google Scholar]
- 5.Hawton K, Bergen H, Simkin S, et al. Impact of different pack sizes of paracetamol in the United Kingdom and Ireland on intentional overdoses: a comparative study. BMC Public Health. 2011;11:460. doi: 10.1186/1471-2458-11-460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawton K, Townsend E, Deeks J, et al. Effects of legislation restricting pack sizes of paracetamol and salicylate on self poisoning in the United Kingdom: before and after study. BMJ. 2001;322:1203–1207. doi: 10.1136/bmj.322.7296.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly FF, Fountain JS, Murray L, Graudins A, Buckley NA, Panel of Australian and New Zealand clinical toxicologists Guidelines for the management of paracetamol poisoning in Australia and New Zealand - explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. Med J Aust. 2008;188:296–301. doi: 10.5694/j.1326-5377.2008.tb01625.x. [DOI] [PubMed] [Google Scholar]
- 8.Young RJ. Dextropropoxyphene overdosage. Pharmacological considerations and clinical management. Drugs. 1983;26:70–79. doi: 10.2165/00003495-198326010-00004. [DOI] [PubMed] [Google Scholar]
- 9.Simkin S, Hawton K, Kapur N, Gunnell D. What can be done to reduce mortality from paracetamol overdoses? A patient interview study. QJM. 2012;105:41–51. doi: 10.1093/qjmed/hcr135. [DOI] [PubMed] [Google Scholar]
- 10.McGill MR, Li F, Sharpe MR, et al. Circulating acylcarnitines as biomarkers of mitochondrial dysfunction after acetaminophen overdose in mice and humans. Arch Toxicol. 2014;88:391–401. doi: 10.1007/s00204-013-1118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghosh J, Das J, Manna P, Sil PC. Acetaminophen induced renal injury via oxidative stress and TNF-alpha production: therapeutic potential of arjunolic acid. Toxicology. 2010;268:8–18. doi: 10.1016/j.tox.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Chandrasekaran VR, Wan CH, Liu LL, Hsu DZ, Liu MY. Effect of sesame oil against acetaminophen-induced acute oxidative hepatic damage in rats. Shock. 2008;30:217–221. doi: 10.1097/shk.0b013e318160dd6b. [DOI] [PubMed] [Google Scholar]
- 13.Galal RM, Zaki HF, Seif El-Nasr MM, Agha AM. Potential protective effect of honey against paracetamol-induced hepatotoxicity. Arch Iran Med. 2012;15:674–680. [PubMed] [Google Scholar]
- 14.Abdul Hamid Z, Budin SB, Wen Jie N, Hamid A, Husain K, Mohamed J. Nephroprotective effects of Zingiber zerumbet Smith ethyl acetate extract against paracetamol-induced nephrotoxicity and oxidative stress in rats. J Zhejiang Univ Sci B. 2012;13:176–185. doi: 10.1631/jzus.B1100133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kheradpezhouh E, Panjehshahin MR, Miri R, et al. Curcumin protects rats against acetaminophen-induced hepatorenal damages and shows synergistic activity with N-acetyl cysteine. Eur J Pharmacol. 2010;628:274–281. doi: 10.1016/j.ejphar.2009.11.027. [DOI] [PubMed] [Google Scholar]
- 16.Anoush M, Eghbal MA, Fathiazad F, Hamzeiy H, Kouzehkonani NS. The protective effects of garlic extract against acetaminophen-induced oxidative stress and glutathione depletion. Pak J Biol Sci. 2009;12:765–771. doi: 10.3923/pjbs.2009.765.771. [DOI] [PubMed] [Google Scholar]
- 17.Mehrpour O, Shadnia S, Sanaei-Zadeh H. Late extensive intravenous administration of N-acetylcysteine can reverse hepatic failure in acetaminophen overdose. Hum Exp Toxicol. 2011;30:51–54. doi: 10.1177/0960327110366182. [DOI] [PubMed] [Google Scholar]
- 18.Blackford MG, Felter T, Gothard MD, Reed MD. Assessment of the clinical use of intravenous and oral N-acetylcysteine in the treatment of acute acetaminophen poisoning in children: a retrospective review. Clin Ther. 2011;33:1322–1330. doi: 10.1016/j.clinthera.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Tsai CL, Chang WT, Weng TI, Fang CC, Walson PD. A patient-tailored N-acetylcysteine protocol for acute acetaminophen intoxication. Clin Ther. 2005;27:336–341. doi: 10.1016/j.clinthera.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Amaral SS, Oliveira AG, Marques PE, et al. Altered responsiveness to extracellular ATP enhances acetaminophen hepatotoxicity. Cell Commun Signal. 2013;11:10. doi: 10.1186/1478-811X-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Badmann A, Langsch S, Keogh A, Brunner T, Kaufmann T, Corazza N. TRAIL enhances paracetamol-induced liver sinusoidal endothelial cell death in a Bim- and Bid-dependent manner. Cell Death Dis. 2012;3:e447. doi: 10.1038/cddis.2012.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Badmann A, Keough A, Kaufmann T, Bouillet P, Brunner T, Corazza N. Role of TRAIL and the pro-apoptotic Bcl-2 homolog Bim in acetaminophen-induced liver damage. Cell Death Dis. 2011;2:e171. doi: 10.1038/cddis.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGill MR, Yan HM, Ramachandran A, Murray GJ, Rollins DE, Jaeschke H. HepaRG cells: a human model to study mechanisms of acetaminophen hepatotoxicity. Hepatology. 2011;53:974–982. doi: 10.1002/hep.24132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao X, Cong X, Zheng L, Xu L, Yin L, Peng J. Dioscin, a natural steroid saponin, shows remarkable protective effect against acetaminophen-induced liver damage in vitro and in vivo. Toxicol Lett. 2012;214:69–80. doi: 10.1016/j.toxlet.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Mobasher MA, Gonzalez-Rodriguez A, Santamaria B, et al. Protein tyrosine phosphatase 1B modulates GSK3β/Nrf2 and IGFIR signaling pathways in acetaminophen-induced hepatotoxicity. Cell Death Dis. 2013;4:e626. doi: 10.1038/cddis.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu YL, Yiang GT, Chou PL, et al. Dual role of acetaminophen in promoting hepatoma cell apoptosis and kidney fibroblast proliferation. Mol Med Rep. 2014;9:2077–2084. doi: 10.3892/mmr.2014.2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gopi KS, Reddy AG, Jyothi K, Kumar BA. Acetaminophen-induced hepato- and nephrotoxicity and amelioration by silymarin and Terminalia chebula in rats. Toxicol Int. 2010;17:64–66. doi: 10.4103/0971-6580.72672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abdel-Zaher AO, Abdel-Hady RH, Mahmoud MM, Farrag MM. The potential protective role of alpha-lipoic acid against acetaminophen-induced hepatic and renal damage. Toxicology. 2008;243:261–270. doi: 10.1016/j.tox.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Cermik H, Taslipinar MY, Aydin I, et al. The relationship between N-acetylcysteine, hyperbaric oxygen, and inflammation in a rat model of acetaminophen-induced nephrotoxicity. Inflammation. 2013;36:1145–1152. doi: 10.1007/s10753-013-9649-4. [DOI] [PubMed] [Google Scholar]
- 30.Ucar F, Taslipinar MY, Alp BF, et al. The effects of N-acetylcysteine and ozone therapy on oxidative stress and inflammation in acetaminophen-induced nephrotoxicity model. Ren Fail. 2013;35:640–647. doi: 10.3109/0886022X.2013.780530. [DOI] [PubMed] [Google Scholar]
- 31.Liang YL, Zhang ZH, Liu XJ, et al. Melatonin protects against apoptosis-inducing factor (AIF)-dependent cell death during acetaminophen-induced acute liver failure. PLoS One. 2012;7:e51911. doi: 10.1371/journal.pone.0051911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramachandran A, McGill MR, Xie Y, Ni HM, Ding WX, Jaeschke H. Receptor interacting protein kinase 3 is a critical early mediator of acetaminophen-induced hepatocyte necrosis in mice. Hepatology. 2013;58:2099–2108. doi: 10.1002/hep.26547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmad ST, Arjumand W, Nafees S, et al. Hesperidin alleviates acetaminophen induced toxicity in Wistar rats by abrogation of oxidative stress, apoptosis and inflammation. Toxicol Lett. 2012;208:149–161. doi: 10.1016/j.toxlet.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 34.Inkielewicz-Stepniak I, Knap N. Effect of exposure to fluoride and acetaminophen on oxidative/nitrosative status of liver and kidney in male and female rats. Pharmacol Rep. 2012;64:902–911. doi: 10.1016/S1734-1140(12)70885-X. [DOI] [PubMed] [Google Scholar]
- 35.Slitt AM, Dominick PK, Roberts JC, Cohen SD. Effect of ribose cysteine pretreatment on hepatic and renal acetaminophen metabolite formation and glutathione depletion. Basic Clin Pharmacol Toxicol. 2005;96:487–494. doi: 10.1111/j.1742-7843.2005.pto_96613.x. [DOI] [PubMed] [Google Scholar]
- 36.Yousef MI, Omar SA, El-Guendi MI, Abdelmegid LA. Potential protective effects of quercetin and curcumin on paracetamol-induced histological changes, oxidative stress, impaired liver and kidney functions and haematotoxicity in rat. Food Chem Toxicol. 2010;48:3246–3261. doi: 10.1016/j.fct.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 37.De-Giorgio F, Lodise M, Chiarotti M, d’Aloja E, Carbone A, Valerio L. Possible fatal acetaminophen intoxication with atypical clinical presentation. J Forensic Sci. 2013;58:1397–1400. doi: 10.1111/1556-4029.12205. [DOI] [PubMed] [Google Scholar]
- 38.Brusilow SW, Cooper AJ. Encephalopathy in acute liver failure resulting from acetaminophen intoxication: new observations with potential therapy. Crit Care Med. 2011;39:2550–2553. doi: 10.1097/CCM.0b013e31822572fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Posadas I, Santos P, Cena V. Acetaminophen induces human neuroblastoma cell death through NFKB activation. PLoS One. 2012;7:e50160. doi: 10.1371/journal.pone.0050160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Posadas I, Vellecco V, Santos P, Prieto-Lloret J, Cena V. Acetaminophen potentiates staurosporine-induced death in a human neuroblastoma cell line. Br J Pharmacol. 2007;150:577–585. doi: 10.1038/sj.bjp.0706993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jaeschke H. Comments on ‘glycogen synthase kinase-3 mediates acetaminophen-induced apoptosis in human hepatoma cells’. J Pharmacol Exp Ther. 2005;314:1401–1402. doi: 10.1124/jpet.105.089821. author reply 1403–1404. [DOI] [PubMed] [Google Scholar]
- 42.Macanas-Pirard P, Yaacob NS, Lee PC, Holder JC, Hinton RH, Kass GE. Glycogen synthase kinase-3 mediates acetaminophen-induced apoptosis in human hepatoma cells. J Pharmacol Exp Ther. 2005;313:780–789. doi: 10.1124/jpet.104.081364. [DOI] [PubMed] [Google Scholar]
- 43.Bilir A, Guneri AD, Altinoz MA. Acetaminophen and DMSO modulate growth and gemcitabine cytotoxicity in FM3A breast cancer cells in vitro. Neoplasma. 2004;51:460–464. [PubMed] [Google Scholar]
- 44.Thiele K, Kessler T, Arck P, Erhardt A, Tiegs G. Acetaminophen and pregnancy: short- and long-term consequences for mother and child. J Reprod Immunol. 2013;97:128–139. doi: 10.1016/j.jri.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 45.Wilkes JM, Clark LE, Herrera JL. Acetaminophen overdose in pregnancy. South MedJ. 2005;98:1118–1122. doi: 10.1097/01.smj.0000184792.15407.51. [DOI] [PubMed] [Google Scholar]
- 46.Tsunekawa Y, Kikkawa T, Osumi N. Asymmetric inheritance of Cyclin D2 maintains proliferative neural stem/progenitor cells: A critical event in brain development and evolution. Dev Growth Differ. 2014;56:349–357. doi: 10.1111/dgd.12135. [DOI] [PubMed] [Google Scholar]
- 47.Di Bernardo J, Maiden MM, Jiang G, Hershenson MB, Kunisaki SM. Paracrine regulation of fetal lung morphogenesis using human placenta-derived mesenchymal stromal cells. J Surg Res. 2014;190:255–263. doi: 10.1016/j.jss.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 48.Dambrot C, Buermans HP, Varga E, et al. Strategies for rapidly mapping proviral integration sites and assessing cardiogenic potential of nascent human induced pluripotent stem cell clones. Exp Cell Res. 2014;327:297–306. doi: 10.1016/j.yexcr.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 49.Yiang GT, Chen YH, Chou PL, Chang WJ, Wei CW, Yu YL. The NS3 protease and helicase domains of Japanese encephalitis virus trigger cell death via caspase-dependent and -independent pathways. Mol Med Rep. 2013;7:826–830. doi: 10.3892/mmr.2013.1261. [DOI] [PubMed] [Google Scholar]
- 50.Yu YL, Su KJ, Chen CJ, et al. Synergistic anti-tumor activity of isochaihulactone and paclitaxel on human lung cancer cells. J Cell Physiol. 2012;227:213–222. doi: 10.1002/jcp.22719. [DOI] [PubMed] [Google Scholar]
- 51.Wei CW, Hu CC, Tang CH, Lee MC, Wang JJ. Induction of differentiation rescues HL-60 cells from Rana catesbeiana ribonuclease-induced cell death. FEBS Lett. 2002;531:421–426. doi: 10.1016/S0014-5793(02)03577-9. [DOI] [PubMed] [Google Scholar]
- 52.Chen KH, Li PC, Lin WH, Chien CT, Low BH. Depression by a green tea extract of alcohol-induced oxidative stress and lipogenesis in rat liver. Biosci Biotechnol Biochem. 2011;75:1668–1676. doi: 10.1271/bbb.110163. [DOI] [PubMed] [Google Scholar]
- 53.Lin BR, Yu CJ, Chen WC, et al. Green tea extract supplement reduces D-galactosamine-induced acute liver injury by inhibition of apoptotic and proinflammatory signaling. J Biomed Sci. 2009;16:35. doi: 10.1186/1423-0127-16-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yiang GT, Yu YL, Chou PL, et al. The cytotoxic protein can induce autophagocytosis in addition to apoptosis in MCF-7 human breast cancer cells. In Vivo. 2012;26:403–409. [PubMed] [Google Scholar]
- 55.Yiang GT, Yu YL, Hu SC, Chen MH, Wang JJ, Wei CW. PKC and MEK pathways inhibit caspase-9/-3-mediated cytotoxicity in differentiated cells. FEBS Lett. 2008;582:881–885. doi: 10.1016/j.febslet.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 56.Tang CH, Hu CC, Wei CW, Wang JJ. Synergism of Rana catesbeiana ribonuclease and IFN-gamma triggers distinct death machineries in different human cancer cells. FEBS Lett. 2005;579:265–270. doi: 10.1016/j.febslet.2004.11.086. [DOI] [PubMed] [Google Scholar]
- 57.Wang AY, Lian LH, Jiang YZ, Wu YL, Nan JX. Gentiana manshurica Kitagawa prevents acetaminophen-induced acute hepatic injury in mice via inhibiting JNK/ERK MAPK pathway. World J Gastroenterol. 2010;16:384–391. doi: 10.3748/wjg.v16.i3.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Win S, Than TA, Han D, Petrovic LM, Kaplowitz N. c-Jun N-terminal kinase (JNK)-dependent acute liver injury from acetaminophen or tumor necrosis factor (TNF) requires mitochondrial Sab protein expression in mice. J Biol Chem. 2011;286:35071–35078. doi: 10.1074/jbc.M111.276089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen JY, Zhang L, Zhang H, Su L, Qin LP. Triggering of p38 MAPK and JNK signaling is important for oleanolic acid-induced apoptosis via the mitochondrial death pathway in hypertrophic scar fibroblasts. Phytother Res. 2014;28:1468–1478. doi: 10.1002/ptr.5150. [DOI] [PubMed] [Google Scholar]
- 60.Liu X, Ye F, Xiong H, et al. IL-1β upregulates IL-8 production in human Müller cells through activation of the p38 MAPK and ERK1/2 signaling pathways. Inflammation. 2014;37:1486–1495. doi: 10.1007/s10753-014-9874-5. [DOI] [PubMed] [Google Scholar]
- 61.Levanon D, Manov I, Iancu TC. Qualitative and quantitative analysis of the effects of acetaminophen and N-acetylcysteine on the surface morphology of Hep3B hepatoma cells in vitro. Ultrastruct Pathol. 2004;28:3–14. [PubMed] [Google Scholar]
- 62.Manov I, Hirsh M, Iancu TC. Acetaminophen hepatotoxicity and mechanisms of its protection by N-acetylcysteine: a study of Hep3B cells. Exp Toxicol Pathol. 2002;53:489–500. doi: 10.1078/0940-2993-00215. [DOI] [PubMed] [Google Scholar]
- 63.Kumari A, Kakkar P. Lupeol protects against acetaminophen-induced oxidative stress and cell death in rat primary hepatocytes. Food Chem Toxicol. 2012;50:1781–1789. doi: 10.1016/j.fct.2012.02.042. [DOI] [PubMed] [Google Scholar]
- 64.Okokon JE, Nwafor PA, Charles U, Dar A, Choudhary MI. Antioxidative burst and hepatoprotective effects of ethanol root extract of Hippocratea africana against paracetamol-induced liver injury. Pharm Biol. 2013;51:872–880. doi: 10.3109/13880209.2013.768273. [DOI] [PubMed] [Google Scholar]
- 65.Lee NH, Seo CS, Lee HY, et al. Hepatoprotective and antioxidative activities of Cornus officinalis against acetaminophen-induced hepatotoxicity in mice. Evid Based Complement Alternat Med. 2012;2012:804924. doi: 10.1155/2012/804924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Olaleye MT, Akinmoladun AC, Ogunboye AA, Akindahunsi AA. Antioxidant activity and hepatoprotective property of leaf extracts of Boerhaavia diffusa Linn against acetaminophen-induced liver damage in rats. Food Chem Toxicol. 2010;48:2200–2205. doi: 10.1016/j.fct.2010.05.047. [DOI] [PubMed] [Google Scholar]
- 67.Nkosi CZ, Opoku AR, Terblanche SE. In vitro antioxidative activity of pumpkin seed (Cucurbita pepo) protein isolate and its in vivo effect on alanine transaminase and aspartate transaminase in acetaminophen-induced liver injury in low protein fed rats. Phytother Res. 2006;20:780–783. doi: 10.1002/ptr.1958. [DOI] [PubMed] [Google Scholar]
- 68.Bhattacharjee R, Sil PC. The protein fraction of Phyllanthus niruri plays a protective role against acetaminophen induced hepatic disorder via its antioxidant properties. Phytother Res. 2006;20:595–601. doi: 10.1002/ptr.1933. [DOI] [PubMed] [Google Scholar]
- 69.Needleman SM. Safety of rapid intravenous of infusion acetaminophen. Proc (Bayl Univ Med Cent) 2013;26:235–238. doi: 10.1080/08998280.2013.11928969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Engstrom Ruud L, Wilhelms DB, Eskilsson A, et al. Acetaminophen reduces lipopolysaccharide-induced fever by inhibiting cyclooxygenase-2. Neuropharmacology. 2013;71:124–129. doi: 10.1016/j.neuropharm.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 71.Zuppa AF, Hammer GB, Barrett JS, et al. Safety and population pharmacokinetic analysis of intravenous acetaminophen in neonates, infants, children, and adolescents with pain or fever. J Pediatr Pharmacol Ther. 2011;16:246–261. doi: 10.5863/1551-6776-16.4.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Boulares AH, Zoltoski AJ, Stoica BA, Cuvillier O, Smulson ME. Acetaminophen induces a caspase-dependent and Bcl-XL sensitive apoptosis in human hepatoma cells and lymphocytes. Pharmacol Toxicol. 2002;90:38–50. doi: 10.1034/j.1600-0773.2002.900108.x. [DOI] [PubMed] [Google Scholar]
- 73.Ghanizadeh A. Acetaminophen may mediate oxidative stress and neurotoxicity in autism. Med Hypotheses. 2012;78:351. doi: 10.1016/j.mehy.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 74.Wang C, Blough ER, Arvapalli R, et al. Metabolic syndrome-induced tubulointerstitial injury: role of oxidative stress and preventive effects of acetaminophen. Free Radic Biol Med. 2013;65:1417–1426. doi: 10.1016/j.freeradbiomed.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 75.Fouad AA, Al-Mulhim AS, Jresat I, Gomaa W. Therapeutic role of telmisartan against acetaminophen hepatotoxicity in mice. Eur J Pharmacol. 2012;693:64–71. doi: 10.1016/j.ejphar.2012.07.049. [DOI] [PubMed] [Google Scholar]
- 76.Choi J, Park KH, Kim SZ, Shin JH, Jang SI. The ameliorative effects of L-2-oxothiazolidine-4-carboxylate on acetaminophen-induced hepatotoxicity in mice. Molecules. 2013;18:3467–3478. doi: 10.3390/molecules18033467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kumari A, Kakkar P. Lupeol prevents acetaminophen-induced in vivo hepatotoxicity by altering the Bax/Bcl-2 and oxidative stress-mediated mitochondrial signaling cascade. Life Sci. 2012;90:561–570. doi: 10.1016/j.lfs.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 78.Ji L, Jiang P, Lu B, Sheng Y, Wang X, Wang Z. Chlorogenic acid, a dietary polyphenol, protects acetaminophen-induced liver injury and its mechanism. J Nutr Biochem. 2013;24:1911–1919. doi: 10.1016/j.jnutbio.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 79.Nafisi S, Heidari R, Ghaffarzadeh M, et al. Cytoprotective effects of silafibrate, a newly-synthesised siliconated derivative of clofibrate, against acetaminophen-induced toxicity in isolated rat hepatocytes. Arh Hig Rada Toksikol. 2014;65:169–178. doi: 10.2478/10004-1254-65-2014-2434. [DOI] [PubMed] [Google Scholar]
- 80.Colle D, Arantes LP, Gubert P, et al. Antioxidant properties of Taraxacum officinaleleaf extract are involved in the protective effect against hepatoxicity induced by acetaminophen in mice. J Med Food. 2012;15:549–556. doi: 10.1089/jmf.2011.0282. [DOI] [PubMed] [Google Scholar]
- 81.Zhao YL, Zhou GD, Yang HB, et al. Rhein protects against acetaminophen-induced hepatic and renal toxicity. Food Chem Toxicol. 2011;49:1705–1710. doi: 10.1016/j.fct.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 82.Lu Y, Sun J, Petrova K, et al. Metabolomics evaluation of the effects of green tea extract on acetaminophen-induced hepatotoxicity in mice. Food Chem Toxicol. 2013;62:707–721. doi: 10.1016/j.fct.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 83.Yakubu N, Oboh G, Olalekan AA. Antioxidant and hepatoprotective properties of tofu (curdle soymilk) against acetaminophen-induced liver damage in rats. Biotechnol Res Int. 2013;2013:230142. doi: 10.1155/2013/230142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Prescott LF, Park J, Ballantyne A, Adriaenssens P, Proudfoot AT. Treatment of paracetamol (acetaminophen) poisoning with N-acetylcysteine. Lancet. 1977;2:432–434. doi: 10.1016/S0140-6736(77)90612-2. [DOI] [PubMed] [Google Scholar]
- 85.Allameh A, Vansoun EY, Zarghi A. Role of glutathione conjugation in protection of weanling rat liver against acetaminophen-induced hepatotoxicity. Mech Ageing Dev. 1997;95:71–79. doi: 10.1016/S0047-6374(97)01862-9. [DOI] [PubMed] [Google Scholar]