Abstract
Background:
Hip fracture is the most common serious injury of older people. The UK National Hip Fracture Database (NHFD) was launched in 2007 as a national collaborative, clinician-led audit initiative to improve the quality of hip fracture care, but has not yet been externally evaluated.
Methods:
We used routinely collected data on 471,590 older people (aged 60 years and older) admitted with a hip fracture to National Health Service (NHS) hospitals in England between 2003 and 2011. The main variables of interest were the use of early surgery (on day of admission, or day after) and mortality at 30 days from admission. We compared time trends in the periods 2003–2007 and 2007–2011 (before and after the launch of the NHFD), using Poisson regression models to adjust for demographic changes.
Findings:
The number of hospitals participating in the NHFD increased from 11 in 2007 to 175 in 2011. From 2007 to 2011, the rate of early surgery increased from 54.5% to 71.3%, whereas the rate had remained stable over the period 2003–2007. Thirty-day mortality fell from 10.9% to 8.5%, compared with a small reduction from 11.5% to 10.9% previously. The annual relative reduction in adjusted 30-day mortality was 1.8% per year in the period 2003–2007, compared with 7.6% per year over 2007–2011 (P<0.001 for the difference).
Interpretation:
The launch of a national clinician-led audit initiative was associated with substantial improvements in care and survival of older people with hip fracture in England.
Key Words: hip fracture, clinician-led audit, quality improvement, administrative hospital data, English National Health Service
Hip fracture is the most common serious injury of older people. Coexisting frailty and medical comorbidities are common. In the United States, there are approximately 250,000 cases a year among older people (65 years and older),1 whereas the UK figure is around 70,000.2 As populations age, these numbers are likely to increase,3 as will numbers occurring in older and frailer people.4 Mortality following hip fracture is high. Historically, in the United Kingdom, around 10% of people die within 30 days. Around one in 10 suffer loss of home, and continuing pain and loss of mobility are common.5 Around a third die within a year, which is twice the mortality rate as in the general population of the same age.6,7
Hip fracture care is costly, with inconsistent quality and patient outcomes.8 Annual medical costs are $12 billion in the United States,9 and nearly $3 billion (£1.7 billion) in the United Kingdom including social care costs.10 Early surgery, dedicated medical care, and rehabilitation following hip fracture can improve outcomes and reduce mortality as well as decrease costs.8,11,12 The importance of coordinated multidisciplinary care is well recognized,13 but its adoption varies widely between and within countries.14,15
The National Hip Fracture Database (NHFD) initiative was conceived in 2004 as a clinician-led collaboration between the British Orthopaedic Association (BOA) and the British Geriatrics Society (BGS), professional associations that cover England, Wales, and Northern Ireland.16 It was launched in 2007 with the explicit aim of improving hip fracture care using the synergy of clinical standards, audit, and feedback. A multidisciplinary team worked to produce a consensus set of 6 national clinical standards for hip fracture care: prompt admission to orthopedic care, surgery within 48 hours, the prevention of pressure ulcers, access to acute orthogeriatric care, assessment for bone protection therapy, and falls assessment. These standards were published by the BOA/BGS, alongside clinical guidance, as The Care of Patients with Fragility Fracture in 2007.17
The NHFD initiative involves much more than data collection. It provides clinical teams in individual participating hospitals with continuous web-based feedback on their case mix, care and outcomes, and on their compliance with the 6 national clinical standards. It provides a telephone helpline, an informative website, and regional multidisciplinary meetings to support local clinical leadership and encourage sharing of good practice. From 2010, annual national reports have allowed public comparison of findings between participating hospitals and the results demonstrate successive improvements in audited standards of care.2
Although the self-reporting of improvements in care and outcomes by large-scale clinical audits is encouraging, a more rigorous external evaluation of their impact is necessary but methodologically challenging.18 However, an opportunity for such an evaluation has arisen in England, where all NHS hospitals that provide trauma care now participate in the NHFD initiative.
This paper uses external data from the years 2003–2011 to evaluate the impact of the NHFD since its launch in 2007 by comparing national time trends in rates of early surgery and mortality in 2003–2007 with those in 2007–2011.
METHODS
Intervention: The BOA/BGS NHFD Initiative
The intervention, referred to in this study as the NHFD initiative, consists of the BOA/BGS national clinical standards, data collection, and feedback, together with NHFD-led activities to support regional and national sharing of good clinical practice and encourage local implementation at hospitals.
We describe the increase in individual hospital participation in the NHFD over the years 2007–2011, with participation defined by the start of regular submission of hospital audit data to the national database (http://www.nhfd.co.uk/20/hipfractureR.nsf/ResourceDisplay).
Patient Cohort
For this external evaluation, we used an anonymized extract of patient records from routinely collected administrative hospital data, the Hospital Episode Statistics (HES),19 which covers all admissions to NHS hospitals in England. HES data were linked to the Office for National Statistics’ database of all registered deaths in England.20 The HES database contains records for each episode of care under the care of a physician and, if patients were transferred between physicians, multiple records for single patients arise. To avoid duplicate reporting and to document the entire period of NHS care, we merged episodes of care using an anonymized patient identifier. Patients’ diagnoses in HES are coded using International Classification of Diseases, 10th revision, and surgical procedures are coded using the classification of surgical operations from the UK Office for Population Censuses and Surveys (OPCS), version 4.
Records were extracted for patients aged 60 or over with an emergency (unplanned) hospital admission to an NHS hospital with a fractured neck of femur between January 1, 2003 and December 31, 2011. A diagnosis of fractured neck of femur was identified using the International Classification of Diseases, 10th revision codes S72.0 (Fracture of Neck of Femur), S72.1 (Pertrochanteric Fracture), and S72.2 (Subtrochanteric Fracture). Up to 14 diagnosis fields were searched for the first episode of the hospital admission. The final sample included 471,590 people treated for an index hip fracture in English NHS hospitals. Subsequent hip fractures were excluded.
Processes of Care and Mortality
The quality of care was measured in 2 ways: whether patients underwent surgery; and whether patients had early surgery, defined as surgery either on the day of or the day after admission to hospital. Patients who had hip fracture surgery were identified in HES using OPCS codes for primary open or closed reduction and internal or external fixation (OPCS codes: W19, W20, W22, W24), hemiarthroplasty involving prosthetic replacement of head of femur (codes: W46–W48), and total hip replacement (codes: W37–W39; W93–W95). Analysis of early surgery was restricted to patients who had surgery (N=423,365).
Mortality was calculated at 30, 90, and 365 days from the day of hospital admission for all patients, including those who did not have surgery. We used the date of death from the Office for National Statistics death register, which is highly accurate.20
Statistical Analysis: Comparison of Time Trends in 2003–2007 versus 2007–2011
Analyses are presented for 2 main variables of interest; the number of early procedures and the number of deaths within 30 days from admission. We summarized this information over 3-month intervals starting from January 2003 for each sex and age category (60–69 years; 70–79 years; 80–89 years; and 90 years or older).
Poisson regression models were fitted for each variable to compare time trends in the 2 time periods 2003–2007 and 2007–2011, with the final calendar quarter of 2007 representing the end of the first time period and the start of the second. The log rate of each variable was fitted as a linear function of continuous time, with an interaction term to test for a change in slope. We adjusted for sex and age category plus their interaction, and for known seasonal variation (dummy indicators for calendar quarter, with January–March as the reference).21 We tested for effects of residual autocorrelation by including lagged values of the deviance residuals for each age-sex group.22 Models were estimated via maximum likelihood using Stata 13.1.
Results are presented as annual rate ratios with 95% confidence intervals (CIs) for the 2 time periods 2003–2007 and 2007–2011. P values are from Wald tests for change in time trend across the 2 periods. Absolute reductions in 30-day mortality are expressed in percentage points calculated from model predictions that were weighted to the age and sex distribution of the sample over the entire study period.
RESULTS
Hospital Participation in the NHFD
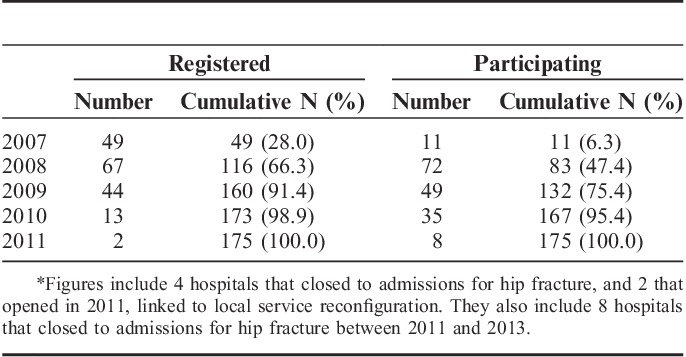
The number of hospitals registered with the NHFD increased from 49 in 2007 to 116 in 2008 and 160 in 2009. All 175 hospitals providing trauma care in England were registered by 2011. The number of hospitals that submitted data to the NHFD rose from 11 in 2007, 83 in 2008 to 132 in 2009, and all hospitals contributed data by 2011 (Table 1).
TABLE 1.
Hospital Registration and Participation in the National Hip Fracture Database by Year among NHS Hospitals in England Between 2007 and 2011*
National Trends in Care and Mortality after Hip Fracture
Over the whole study period 2003–2011, the percentage of patients who underwent hip fracture surgery remained stable before 2007, and then increased from 89.6% in 2007 to 91.7% in 2011. Of patients who had surgery, the percentage having early surgery increased from 54.5% in 2007 to 71.3% in 2011, whereas the rate had remained fairly stable over the period 2003–2007 (Table 2). Thirty-day mortality fell from 10.9% to 8.5% over the period 2007–2011, compared with a small reduction from 11.5% to 10.9% over the 4 preceding years. In addition, greater reductions in 90-day and 365-day mortality were observed after 2007.
TABLE 2.
Description of Average Characteristics, Care, and Mortality in 471,590 Patients Admitted to Hospital with Hip Fracture between 2003 and 2011 in the English NHS
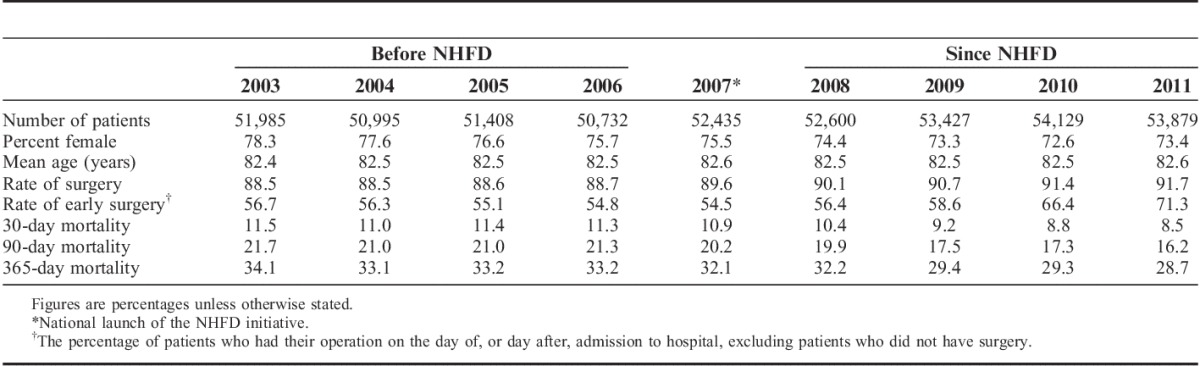
These improvements in care and survival occurred in the context of a gradual rise in hip fracture admissions in England, from 51,985 in 2003 to 53,879 in 2011. The age composition of the hip fracture population remained stable, with an average age of 82.5 years, and around a fifth of patients aged 90 years or older (Table 2). However, the proportion of men, for whom the mortality rate is approximately double that for women, rose from a fifth to a quarter.
There was evidence of autocorrelation in rates of early surgery from one time-point (3-month interval) to the next, but no evidence of autocorrelation in the mortality time series. Adjustment for residual autocorrelation did not affect the estimated time trends presented below.
Impact of NHFD Initiative on Rates of Early Surgery
Table 3 shows average annual changes in rates of early surgery in the periods 2003–2007 versus 2007–2011, adjusted for changes in the age and sex composition of the hip fracture population. On average, over the period 2003–2007, there was a relative annual decrease of 1.3% per year in the proportion of patients having early surgery (adjusted rate ratio (RR) 0.987; 95% CI, 0.985–0.990). This compares to an annual increase of 8.0% per year over the period 2007–2011 (adjusted RR 1.080; 95% CI, 1.077–1.084).
TABLE 3.
Comparison of Average Annual Changes in Rates of Early Surgery and 30-day Mortality before and since National Launch of NHFD in September 2007 (n=471,590 Patients)

Impact of NHFD Initiative on 30-day Mortality
There was a relative reduction of 1.8% per year over the period 2003–2007 (adjusted RR 0.982; 95% CI, 0.975–0.988). This rose to 7.6% per year over the period 2007–2011 (adjusted RR 0.924; 95% CI, 0.916–0.932, P value for their difference <0.001). The absolute reduction over the period 2007–2011 was 2.9%, compared with a small decrease of 1.0% over the period 2003–2007 (Fig. 1).
FIGURE 1.
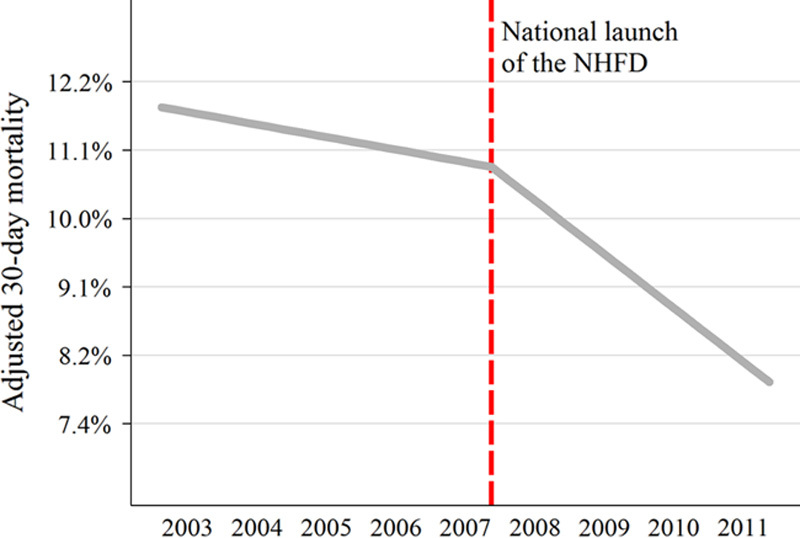
Time trends in 30-day mortality in the periods 2003–2007 and 2007–2011. Y axis is on log scale, with labels on natural scale. Time is measured in 3-month intervals.
DISCUSSION
Main Findings
This external evaluation of the NHFD initiative, a national clinician-led initiative to improve hip fracture care, demonstrates substantial improvements in hospital performance and patient survival following its launch in 2007 and its expansion over the study period. The proportion of patients having early surgery increased only after 2007. Adjusted 30-day mortality fell in relative terms by 7.6% per year in the period 2007–2011, compared with just 1.8% per year over 2003–2007.
Study Strengths and Weaknesses
We used routinely collected hospital data from HES, which has the advantage of containing records for all patients treated in all NHS hospitals in England, with records available for care over several years before and after the NHFD's launch in England. Our sample included all patients admitted to an English NHS hospital with a hip fracture over the study period.
There are limitations arising from the use of routinely collected data. These include the quality and scope of the data. We addressed both in a previous study comparing diagnostic and procedure coding in HES and NHFD,23 confirming the accuracy of diagnostic coding of hip fracture, a major and also a well-defined injury. We limited the analysis strictly to care processes that can be accurately measured using administrative data (i.e. the use and timing of surgery). Clearly, improvements in other less well-documented aspects of care will have contributed to the observed improvements in survival, for example, increasing orthogeriatrician involvement in acute hip fracture care, including preoperative assessments that facilitated early surgery.
We decided not to adjust for comorbidity because of concerns about the possible effect of growing emphasis on the documentation of comorbidity over time in HES.24 A large local clinical database, with consistently detailed documentation over time, suggests a real increase in the prevalence of comorbidities.25 Thus, our estimates may understate improvements in survival attributable to better care in a more challenging population.
Our statistical models were based on the assumptions that time trends in the log rates of variables were linear. We checked this assumption by testing the significance of adding a quadratic term for time to the model using data from 2003–2007, and found that it was nonsignificant both for early surgery (P=0.43) and for 30-day mortality (P=0.16).
Other concurrent national policies could have contributed to the effects that we observe, such as the work of the NHS Institute for Innovation and Improvement.26,27 The introduction of financial incentives under the Best Practice Tariff (BPT) scheme in April 2010, which extended the BOA/BGS clinical standards to include orthogeriatrician participation within 72 hours and surgery within 36 hours, appears to have contributed to a sharp increase in rates of early surgery in 2010–2011.28 However, the decrease in mortality was observed from 2007, before BPT was introduced, coinciding with increasing rates of preoperative geriatrician assessment between 2007 and 2009.2
Implications
The decrease in 90-day mortality was greater in absolute terms than the decrease in 30-day mortality over the period 2007–2011, and similar in magnitude to the decrease in 365-day mortality. This result suggests that better acute hip fracture care reduces mortality within the first 90 days and that this reduction is maintained at 1 year. Importantly, this shows that early mortality was not simply deferred; improved longer-term survival is sustained. This is consistent with evidence that between 17% and 32% of deaths after hip fracture are potentially avoidable.29 However, with around 20% of our sample aged 90 or older, an irreducible 1-year mortality should also be recognized.
The NHFD initiative started with a multidisciplinary meeting in 2004 and evolved as a collaborative nation-wide initiative rather than a pre-determined top-down program. It drew on the work of the Swedish Rikshoft and the Scottish Hip Fracture Audit, as well as on recent advances in web-based technology to support national clinical audit. It used the combination of clinical standards, data collection, and feedback to support hospital clinical teams in their efforts to improve hip fracture care. It is important to recognize the impact of these wider aspects of the initiative, not only in achieving improved care and survival, but in functioning as a broadly based quality improvement initiative.
The NHFD's impact resulted from the use of clinical standards and audit to raise awareness of hip fracture care and the potential for its improvement. In particular, and in marked contrast to feedback via annual reports, continuous web-based feedback enabled clinical teams to scrutinize the care they provided over time, to identify problems and set about solving them, and to monitor the effects of this on care and outcomes.
This wider use of the audit to prompt and monitor initiatives to improve clinical care and service structure by individual hospitals was shared in regional meetings and documented in NHFD annual reports, thus spreading knowledge of good practice in audit and change. For example, clinicians and managers in 2 hospitals in North East England launched a quality improvement initiative in 2009, partly prompted by national benchmarking that revealed an above-average mortality rate in 1 hospital. The care pathway and patients' experiences were reviewed and local targets were set to reduce waiting times for surgery, and provide additional support with nutrition. Progress was monitored locally using new user-defined fields alongside the standard data collected by NHFD. Over the subsequent 18 months, 30-day mortality fell sharply, and patient and carer satisfaction was high.30
The NHFD initiative was deliberately structured to achieve its prime goal of improving quality and outcomes in hip fracture care. A small central implementation group was established with a strong clinical focus and worked to support the best use of audit as widely as possible. During the period of this study, 2 project coordinators provided a telephone helpline, ran data quality workshops for hospital audit staff, and organized regular regional NHFD meetings bringing together multidisciplinary teams to share national developments and local good practice. As a result, the coordinators developed strong and extensive personal contacts with participants. A website for NHFD was developed, and included a database of hip fracture literature, case studies of good practice, model business cases and job descriptions: all of use in facilitating effective participation.
It is impossible to disentangle the synergistic effects of these activities in an evaluation of the NHFD initiative, but the general effectiveness of augmenting clinical audit with measures to help hospitals to use data for improving services has been demonstrated in other contexts.31 It is likely that the improvements in care and survival demonstrated are attributable, at least in part, to the fact that the NHFD initiative, as a large-scale, comprehensive, and supportive national quality improvement initiative, succeeded in creating “a critical mass of enthusiasm and expertise in hip fracture care.”32
Research in Context
Improvements in audited care and outcomes documented by many large-scale clinical audits, including the NHFD, are readily available.2,33 However as they are essentially self-reporting, they are lacking in objectivity.
The objective evaluation of large-scale quality improvement initiatives matters because they are recognized as important, useful, sometimes transformative, and also costly. However, major methodological challenges arise in their evaluation because of their scale and complexity.18
In theory at least, cluster randomization at the hospital level might be considered to evaluate the impact of initiatives to support quality improvement. In practice, this would raise problems in terms of cost, delay, and lengthy time to produce an effect. More seriously, this approach would be at odds with the culture of clinical leadership, local ownership, and sharing of knowledge and good practice that large-scale initiatives seek to promote, and upon which their success arguably depends. The limitations of the randomised controlled trials in more complex contexts are increasingly recognized.34
The present study addresses the challenge of objective evaluation of a major national clinical audit by being the first to use time trends in external national data extending from well before the audit’s launch and through a subsequent rise to national coverage. It demonstrates the possible contribution of a large-scale audit to improved care and survival, shows clearly that these improvements did not merely represent a continuation of already existing trends, and contributes to a small but necessary set of rigorous observational studies that attempt to evaluate large-scale complex improvement initiatives.35
Unanswered Question for Future Research
One of the key developments in hip fracture care in England has been the increasing contribution of orthogeriatrics, an expanding subspecialty within geriatric medicine.36,37 A further rise in orthogeriatrician involvement followed its specification as a BOA/BGS care standard, audited via the NHFD and later under the BPT financial incentive scheme. More detailed work is needed on the impact on patient care of individual hospital participation, the development of orthogeriatrician participation and the effectiveness of different forms of collaborative orthogeriatric and surgical care as the NHFD evolved. An economic evaluation of the impact of the NHFD initiative would also be useful to determine its cost-effectiveness, which could influence the adoption of such programs internationally.
CONCLUSIONS
This evaluation of the impact in England of the NHFD, a national initiative to improve hip fracture care, suggests that it has prompted improvements in hospital care leading to substantial and sustained improvements in survival. Previous work has demonstrated an increase in survival after hip fracture at national level in England since 2001.38 This work now shows that most of this reflects the impact since 2007 of the NHFD.
ACKNOWLEDGMENTS
We thank Lynn Copley for providing the required HES data extract. We thank the NHFD team, in particular, Andy Williams, Tim Bunning, and Chris Boulton, for advice and help accessing the NHFD information on audit participation. We thank other colleagues for useful discussions about the work, in particular: Antony Johansen, Kate Walker, Roz Stanley, Angelina Taylor, Mike Reed, Andy Chaplain, Andrew Hutchings, Philippa Thorpe, Ged Hughes, Celia Gregson and Mick Peake. We also thank our two reviewers.
Footnotes
Hospital episode statistics were made available by the NHS Health and Social Care Information Centre (Copyright© 2012, reused with the permission of The Health and Social Care Information Centre. All rights reserved).
J.N. is funded by a Post-Doctoral Fellowship award from the National Institute for Health Research. This report describes independent research arising from a Post-Doctoral Fellowship supported by the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
The project does not require NHS Research Ethics Committee approval because it involves secondary analysis of anonymised data. The project meets the requirements of the Office for National Statistics (ONS) for release of mortality data under Section 42(4) of the Statistics and Registration Service Act 2007 as amended by Section 287 of the Health and Social Care Act 2012.
R.W., C.C., and F.P. were funded as members of the NHFD implementation group; J.N. was formerly and C.T. and D.C. are currently commissioned by the Royal College of Physicians to analyze data for the NHFD annual reports as part of the Falls and Fragility Fractures Audit Programme (FFFAP). R.W. is clinical lead for orthopedic surgery on the NHFD. C.C. was a clinical lead for geriatric medicine on the National Hip Fracture Database (NHFD) from 2004 to 2013. F.P. was the project coordinator on the NHFD from 2009 to 2013. The remaining authors declare no conflict of interest.
REFERENCES
- 1.Center for Disease Control and Prevention, National Center for Health Statistics. Figure for hip fracture admissions of older people (≥65 years). Available at: http://205.207.175.93/hdi/ReportFolders/ReportFolders.aspx?IF_ActivePath=P,18. Accessed March 27, 2015.
- 2.Johansen AW, Wakeman R, Boulton C, et al. The National Hip Fracture Database National Report 2013. Available at: http://www.nhfd.co.uk/. Accessed December 8, 2014.
- 3.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. [DOI] [PubMed] [Google Scholar]
- 4.DuGoff EH, Canudas-Romo V, Buttorf C, et al. Multiple chronic conditions and life expectancy. A life table analysis. Med Care. 2014;51:688–694. [DOI] [PubMed] [Google Scholar]
- 5.Parker M, Johansen A. Hip fracture. Clinical review. BMJ. 2006;333:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98: database study. BMJ. 2003;327:771–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Office for National Statistics. Deaths Registrations Summary Tables, England and Wales-2011. Available at: http://www.ons.gov.uk/ons/rel/vsob1/death-reg-sum-tables/index.html. Accessed February 22, 2015.
- 8.Kates SL, Blake D, Bingham K, et al. Comparison of an organized geriatric fracture program to United States Government data. Geriatr Orthop Surg Rehabil. 2010;1:15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burge RT, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. JBMR. 2007;22:465–475. [DOI] [PubMed] [Google Scholar]
- 10.Burge RT, Worley D, Johansen A, et al. The cost of osteoporotic fractures in the UK: projections for 2000-2020. J Med Econ. 2001;4:51–62. [Google Scholar]
- 11.Bukata S, DiGiovanni BF, Friedman SM, et al. A guide to improving the care of patients with fragility fractures. Geriatr Orthop Surg Rehabil. 2011;2:5–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. CMG46: management of hip fracture in adults. NICE, 2012. Available at: http://www.nice.org.uk/guidance/cg124/resources/cg124-hip-fracture-full-guideline2. Accessed December 19, 2014.
- 13.Hung WW, Egol K, Zuckerman JD, et al. Hip fracture management. Tailoring care for the older patient. JAMA. 2012;307:2185–2194. [DOI] [PubMed] [Google Scholar]
- 14.Kates SL, O’Malley N, Friedman SM, et al. Barriers to implementation of an organized geriatric fracture program. Geriatr Orthop Surg Rehabil. 2012;3:8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sunol R, Wagner C, Arah OA, et al. Evidence-based organization and patient safety strategies in European hospitals. Int J Qual Health Care. 2014;26:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahota O, Currie C. Hip fracture care: all change. Age Ageing. 2008;37:128–129. [DOI] [PubMed] [Google Scholar]
- 17.British Orthopaedic Association, British Geriatrics Society. The Care of Patients with Fragility Fracture: British Orthopaedic Association; 2007. Available at: http://www.bgs.org.uk/pdf_cms/pubs/Blue%20Book%20on%20fragility%20fracture%20care.pdf. Accessed March 27, 2015.
- 18.Ovretveit J, Gustafson D. Evaluation of quality improvement programmes. BMJ Qual Saf. 2002;11:270–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Health and Social Care Information Centre. Hospital Episode Statistics: HES User Guide, 2010. Available at: http://www.hscic.gov.uk/hes. Accessed December 19, 2014.
- 20.The Information Centre. A guide to linked HES-ONS mortality data. 2011. Available at: http://www.hscic.gov.uk/article/2677/Linked-HESONS-mortality-data. Accessed December 19, 2014.
- 21.Crawford JR, Parker MJ. Seasonal variation of proximal femoral fractures in the United Kingdom. Injury. 2003;34:223–225. [DOI] [PubMed] [Google Scholar]
- 22.Bhaskaran K, Gasparrini A, Hajat S, et al. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42:1187–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neuburger J, Cromwell D. Estimating case-ascertainment and length of acute/post-acute hospital stay for patients with a hip fracture. Analysis of information from the National Hip Fracture Database and Hospital Episode Statistics. Available at: http://www.nhfd.co.uk/20/hipfractureR.nsf/ResourceDisplay. Accessed December 19, 2014.
- 24.Burns EM, Rigby E, Mamidanna R, et al. Systematic review of discharge coding accuracy. J Public Health (Oxf). 2012;34:138–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baker PN, Salar O, Ollivere BJ, et al. Evolution of the hip fracture population: time to consider the future? A retrospective observational analysis. BMJ Open. 2015;4:e004405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliver D. Development of services for older patients with falls and fractures in England: successes, failures, lessons and controversies. Arch Gerontol Geriatr. 2009;49:S7–S12. [DOI] [PubMed] [Google Scholar]
- 27.NHS Institute for Innovation and Improvement. Focus on: Fractured Neck of Femur. 2006 Available at:http://www.institute.nhs.uk/images/documents/Quality_and_value/Focus_On/DVQ_path_fracturefemurPROOF_Nov.pdf. Accessed May 20, 2015
- 28.Audit Commission. Best practice tariffs and their impact. Available at: http://www.audit-commission.gov.uk/2012/11/best-practice-tariffs-and-their-impact/. Accessed December 19, 2014.
- 29.Kanis JA, Oden A, Johnell O, et al. The components of excess mortality after hip fracture. Bone. 2003;32:468–473. [DOI] [PubMed] [Google Scholar]
- 30.Reed M. on behalf of HIPQIP steering group. Hip Fracture Quality Improvement Programme (HIPQIP). Northumbria Healthcare NHS Foundation Trust. 2011. Available at: http://www.nhfd.co.uk/20/hipfractureR.nsf/xsp/.ibmmodres/domino/OpenAttachment/20/hipfracturer.nsf/85EB9341D2540EEA802579ED0038C942/Attachment/HIPQIP%20-%20Update%20on%20progress%20-%20one%20year%20on%20Report.pdf. Accessed December 19, 2014.
- 31.Peterson A, Carlhed R, Lindahl B, et al. Improving guideline adherence through intensive quality improvement and the use of a national quality register in Sweden for acute myocardial infarction. Qual Manag Health Care. 2007;16:25–37. [DOI] [PubMed] [Google Scholar]
- 32.Currie C, Partridge M, Plant F, et al. The National Hip Fracture Database National Report 2011. Available at: http://www.nhfd.co.uk/. Accessed December 21, 2014.
- 33.Larsson S, Lawyer P, Garellick G, et al. Use of 13 disease registries in 5 countries demonstrates the potential to use outcome data to improve health care’s value. Health Aff. 2012;31:220–227. [DOI] [PubMed] [Google Scholar]
- 34.Berwick DM. The science of improvement. JAMA. 2008;299:1182–1184. [DOI] [PubMed] [Google Scholar]
- 35.Hutchings A, Durand MA, Grieve R, et al. Evaluation of the modernisation of adult critical care services in England: time series and cost-effectiveness analysis. BMJ. 2009;399:b4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wakeman R, Sheard PD, Jenner GH. Ortho-geriatric liaison—the missing link? J Bone Joint Surg [Br]. 2004;86-B:636–638. [DOI] [PubMed] [Google Scholar]
- 37.Johansen A. The future of ortho-geriatrics. Age Ageing. 2010;39:664–665. [DOI] [PubMed] [Google Scholar]
- 38.Smith P, Ariti C, Bardsley M. Focus on hip fracture. Trends in emergency admissions for fractured neck of femur, 2001 to 2011. The Health Foundation/Nuffield Trust, 2013. http://www.nuffieldtrust.org.uk/sites/files/nuffield/publication/131010_focus-on-hip-fracture.pdf. [Google Scholar]


