Abstract
Purpose
To investigate the association of genetic and environmental factors, and their interactions in Korean patients with exudative age-related macular degeneration (AMD).
Methods
A total of 314 robustly characterized exudative AMD patients, including 111 PCV (polypoidal choroidal vasculopathy) and 154 typical choroidal neovascularization (CNV), and 395 control subjects without any evidence of AMD were enrolled. Full ophthalmologic examinations including fluorescein angiography (FA), indocyanine green angiography (ICG) and optical coherence tomography (OCT) were done, according to which patients were divided into either PCV or typical CNV. Standardized questionnaires were used to collect information regarding underlying systemic diseases, dietary habits, smoking history and body mass index (BMI). A total of 86 SNPs from 31 candidate genes were analyzed. Genotype association and logistic regression analyses were done and stepwise regression models to best predict disease for each AMD subtype were constructed.
Results
Age, spherical equivalent, myopia, and ever smoking were associated with exudative AMD. Age, hypertension, hyperlipidemia, spherical equivalent, and myopia were risk factors for typical CNV, while increased education and ever smoking were significantly associated with PCV (p<.05 for all). Four SNPs, ARMS2/HTRA1 rs10490924, rs11200638, and rs2736911, and CFH rs800292, showed association with exudative AMD. Two of these SNPs, ARMS2/HTRA1 rs10490924 and rs11200638, showed significant association with typical CNV and PCV specifically. There were no significant interactions between environmental and genetic factors. The most predictive disease model for exudative AMD included age, spherical equivalent, smoking, CFH rs800292, and ARMS2 rs10490924 while that for typical CNV included age, hyperlipidemia, spherical equivalent, and ARMS2 rs10490924. Smoking, spherical equivalent, and ARMS2 rs10490924 were the most predictive variables for PCV. When comparing PCV cases to CNV cases, age, BMI, and education were the most predictive risk factors of PCV.
Conclusions
Only one locus, the ARMS2/HTRA1 was a significant genetic risk factor for Korean exudative AMD, including its subtypes, PCV and typical CNV. Stepwise regression revealed that CFH was important to risk of exudative AMD in general but not to any specific subtype. While increased education was a unique risk factor to PCV when compared to CNV, this association was independent of refractive error in this homogenous population from South Korea. No significant interactions between environmental and genetic risk factors were observed.
Introduction
Age-related macular degeneration (AMD) is characterized by progressive degeneration leading to the loss of retinal pigment epithelial cells and subsequent photoreceptor loss, resulting in irreversible central visual field defect. The development and severity of complex diseases such as AMD is known to be influenced by a number of factors. The high prevalence of AMD in the elderly e.g., those over 60 years of age, indicates that genetic, environmental factors as well as their likely interactions are involved in the pathogenesis.[1,2] Although the largest genome-wide association study (GWAS) meta-analysis and replication to date has confirmed many loci and demonstrated several new loci associated with AMD, the two genetic loci contributing the greatest risk to AMD are complement factor H (CFH) (1q32) and age-related maculopathy susceptibility 2 (ARMS2)/Htra serine peptidase 1 (HTRA1) (10q26).[2] Among epidemiological factors, the most consistent and strongest reported one is cigarette smoking.[1,3,4] Moreover it has been shown that cigarette smoking interacts with variants in ARMS2 to amplify the risk of AMD in Caucasians.[5]
Polypoidal choroidal vasculopathy (PCV), which is characterized by inner choroidal vascular network of vessels ending in aneurysmal bulge or outward projection, demonstrates similar clinical manifestations to exudative AMD, but whether it is a subtype of AMD or a distinct disease entity remains controversial.[6,7] PCV is more prevalent in the Asian population with reports showing 40–55% of Japanese exudative AMD, 25% of newly diagnosed Chinese AMD, and 31.7% of Korean exudative AMD patients are PCV.[6,8–10] Numerous studies have examined the correlation between established genetic and environmental risk factors for AMD with PCV, such as CFH, ARMS2/HTRA1 genes, and smoking history, and found significant association.[11–13] A recent meta-analysis also confirmed similarities in genetic risk factors between AMD and PCV, even for the previously inconsistently replicated CFH Y402H variant (rs1061170).[14]
Due to the complex disease nature of AMD and PCV, there have been previous reports examining the differential effects of environmental factors, namely smoking, on known genetic risk factors.[5,15,16] However, comprehensive studies focusing on gene-environment interactions for PCV and non-PCV typical choroidal neovascularization (CNV) are scarce in past literature.[15] Hence, this study was performed to investigate the association of genetic and environmental factors and their interaction with Korean exudative AMD patients, especially its subtypes, typical CNV and PCV, to subsequently assess the effect of gene-environment interaction on the pathogenesis of typical CNV and PCV.
Methods
Study design
This study was approved by the institutional review board of Seoul National University Bundang Hospital (SNUBH). Written informed consent was obtained from all subjects before participation in the study.
Patient and control subjects
This study was a case-control study evaluating the genetic and environmental factors of AMD. Exudative AMD patients were recruited from the SNUBH retina clinic from July 2008 to October 2010. All patients underwent comprehensive ophthalmological evaluation, including measurement of best-corrected visual acuity, slit-lamp biomicroscopy, indirect fundus exam, fluorescein angiography (FA), indocyanine green angiography (ICGA, Heidelberg Retina Angiography; Heidelberg Engineering, Heidelberg, Germany), and optical coherence tomography (OCT, Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany). Exudative AMD was diagnosed when there was evidence of choroidal neovascularization associated with nondrusenoid retinal pigment epithelium detachment, serous or hemorrhagic retinal detachment, subretinal hemorrhage, or subretinal exudation.[17] Large geographical atrophy or large drusen without the presence of choroidal neovascularization (CNV) and any secondary CNVs due to myopic degeneration, angioid streak, idiopathic CNV, ocular histoplasmosis syndrome were excluded.
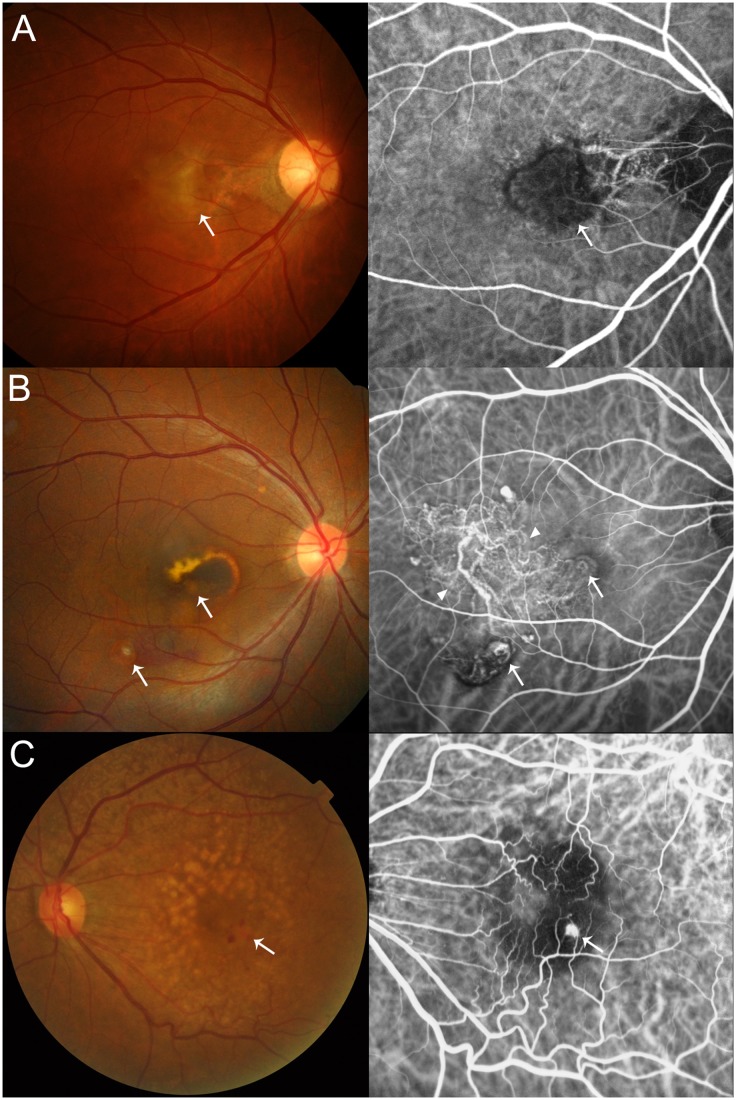
Among the 314 exudative AMD patients recruited, a total of 277 patients underwent ICGA. According to FA, ICGA and OCT findings, this subgroup was divided into three AMD subtypes consisting of typical CNV (n = 157), PCV (n = 112) or retinal angiomatous proliferation (RAP, n = 8) (Fig 1). The typical CNV group was determined by demonstration of choroidal neovascular membrane on FA without any evidence of PCV on ICGA. The PCV group was defined as hyperfluorescent polypoidal choroidal vasculature with branching vascular network on ICGA with concomitant exudation or hemorrhage.[18] The RAP group consisted of cases exhibiting evidence of retinal-retinal or retinal-choroidal anastomosis on ICGA. The 37 patients without ICGA images, RAP patients (n = 8), and typical CNV and PCV patients with missing demographic data (3 patients for typical CNV and 1 patient for PCV) were excluded from the subtype analysis comparing the AMD subtypes, typical CNV and PCV. All diagnoses were made independently by two senior retina specialists (SJW and KYP) and discordant cases were jointly discussed with a third retina specialist (JA).
Fig 1. Representative fundus and angiography images of the three age-related macular degeneration subtypes.
(A) Typical choroidal neovascularization with surrounding subretinal hemorrhage (white arrow) and evident dye leakage (white arrow) on fluorescein angiography. (B) Polypoidal choroidal vasculopathy showing reddish-orange polyp-like structures (white arrows) and branching choroidal vascular network with polypoidal vascular endings (arrowheads). (C) Retinal angiomatous proliferation with multiple drusen, pinpoint subretinal hemorrhage (white arrow) and chorioretinal anastomosis (white arrow) demonstrated on indocyanine green angiography.
For the control group, 273 subjects were recruited from people visiting the SNUBH healthcare center for regular medical checkup and 122 subjects were participants of the Korean Longitudinal Study on Health and Aging (KLoSHA); randomly-sampled community-dwelling elderly Koreans aged 65 years or older.[19] Normal control subjects underwent visual acuity examination, fundus photography and/or OCT to ensure that no intermediate sized drusen, RPE changes, retinal diseases, or glaucoma were present. All study subjects were of Korean descent.
Collection of demographic data
Standardized questionnaires were performed in all patients to collect information regarding age, gender, underlying systemic diseases such as diabetes, hypertension, history of cerebrovascular diseases, and hyperlipidemia, dietary habit, smoking history and body mass index (BMI). Information regarding refractive error was available for a subset of subjects. This included lens status (phakic, pseudophakic, or aphakic), axial length and spherical equivalent. Spherical equivalent (SE, in diopters [D]) was analyzed as the mean of both eyes. When data from only one eye was available, the SE of that eye was used. Myopia was defined as SE ≤ -1 D in at least one eye. Both SE and myopia status were only used when both lenses were phakic. Axial length was analyzed two ways: 1. As the average of both eyes and 2. The right eye (OD) only. According to smoking history, patients were categorized into current, ex- and never smokers. Never smokers were those who had smoked less than 100 cigarettes in the past and ex-smokers had to have quit at least 1 year before the time of examination. An additional sub-analysis categorizing patients into never versus ever smokers was also done.
Genotype analysis
DNA was extracted from leukocytes in the peripheral blood by DNA extraction kit (QIAamp DNA Maxi kit, Qiagen Inc.). A total of 86 SNPs from 31 candidate genes were analyzed (S1 Table). The SNPs were assayed using multiplex PCR with single base extension primers (iPLEX Gold kit and MassARRAY software, Sequenom, San Diego, CA).
Statistical analysis
Baseline clinical information and dietary data were compared between patients and controls using the t-test, χ2 test, or Fisher’s exact test. Genotype data cleaning and analysis was performed using PLINK (http://pngu.mgh.harvard.edu/~purcell/plink/). The SNP data was cleaned by removing SNPs with a low genotyping pass rate (greater than 10% of genotypes missing from the entire cohort) and/or by removing SNPs in those subjects without disease that were not in Hardy Weinberg Equilibrium (HWE p < .0005 (p = 0.05/86 SNPs). Epidemiological variables were tested for their association with disease using logistic regression in SAS (SAS v9.1, Cary, NC: http://www.sas.com/). For the SNP analysis, the minor allele, or less frequent allele, for each SNP was tested for association with disease using the chi square test in PLINK. Correction for multiple testing was performed using two methods: Bonferroni single-step adjusted and FDR BH).[20] Tests for interaction of both genetic and environmental risk factors were performed using interaction terms as well as main effects in the logistic regression model, following the methodology proposed by Keller [21] to control for potential confounders. Specifically, factors that were shown to be significantly associated with each AMD subtype (p < .05) were included in the model along with their corresponding interaction terms. Stepwise logistic regression was performed in order to determine the most significantly associated risk factors. Only those factors shown to be significantly associated with each AMD subtype (p < .05) were included in the stepwise regression model.
Results
A total of 314 exudative AMD patients, consisting of 157 typical CNV and 112 PCV, and 395 control subjects were recruited. Epidemiological and genetic data were available for all recruited subjects. However, based on presence of cataract, history of intraocular surgery, and recruitment at sub-specialty clinics, lens status (n = 481), spherical equivalent (n = 590), and axial length (n = 385) were only available for subsets of individuals. In the univariate analysis of baseline data, exudative AMD patients were significantly older than control subjects (exudative AMD vs controls = 71.1 vs 68.2 years, P<0.001). (Table 1) Regarding smoking history, exudative AMD showed a positive association (ever smoking: exudative AMD vs controls = 54% vs 42%, P = 0.003). For the subgroup analyses comparing PCV and typical CNV, 154 typical CNV and 111 PCV patients were included. PCV patients were significantly younger than typical CNV patients (PCV vs typical CNV = 67.4 vs 72.6 years, P<0.001) and significantly more likely to have smoking history (ever smoking: PCV vs typical CNV = 64% vs 49%, P = 0.018). There were no significant differences in BMI or the presence of systemic diseases between exudative AMD, control and PCV, typical CNV.
Table 1. Distribution of non-genetic variables among studied subjects.
| Exudative AMD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control (N = 395) | Exudative AMD (N = 314) | PCV (N = 111) | Typical CNV (N = 154) | PCV vs. Typical CNV | ||||||
| Variables | N | (%) | N | (%) | P* | N | (%) | N | (%) | P |
| Age (yr) | 68.20±10.13 | 71.1±8.4 | <0.001 | 67.35±7.34 | 72.56±8.10 | <0.001 | ||||
| Male sex | 198 | (50) | 164 | (52) | 0.578 | 61 | (55) | 86 | (56) | 0.886 |
| Smoking | ||||||||||
| (1) Never | 228 | (58) | 145 | (46) | 40 | (36) | 78 | (51) | ||
| Ex- | 128 | (32) | 121 | (39) | 54 | (49) | 53 | (34) | ||
| Current | 39 | (10) | 47 | (15) | 0.007 | 17 | (15) | 23 | (15) | 0.042 |
| (2) Never | 228 | (58) | 145 | (46) | 40 | (36) | 78 | (51) | ||
| Ever | 167 | (42) | 168 | (54) | 0.003 | 71 | (64) | 76 | (49) | 0.018 |
| Education (yr) | ||||||||||
| <9 | 91 | (23) | 70 | (22) | 12 | (11) | 41 | (27) | ||
| <12 | 54 | (14) | 41 | (13) | 12 | (11) | 24 | (16) | ||
| <15 | 122 | (31) | 83 | (27) | 32 | (29) | 38 | (25) | ||
| ≥15 | 128 | (32) | 119 | (38) | 0.423 | 55 | (50) | 51 | (33) | 0.003 |
| BMI (kg/m2) | 23.61±2.96 | 23.47±3.11 | 0.542 | 23.47±2.80 | 23.66±3.37 | 0.638 | ||||
| Diabetes | 87 | (22) | 62 | (20) | 0.462 | 16 | (14) | 28 | (18) | 0.416 |
| Hypertension | 182 | (46) | 164 | (52) | 0.101 | 54 | (49) | 90 | (58) | 0.114 |
| Cerebrovascular accident | 40 | (10) | 43 | (14) | 0.199 | 10 | (9) | 23 | (15) | 0.149 |
| Hyperlipidemia | 82 | (21) | 52 | (17) | 0.134 | 22 | (20) | 21 | (14) | 0.178 |
| Spherical Equivalent (D)° | -0.407±3.13 | 0.581±1.81 | <0.001 | 0.414±1.72 | 0.502±1.90 | 0.737 | ||||
| Myopia° | 36 | (28) | 38 | (17) | 0.014 | 16 | (18) | 31 | (21) | 1.000 |
| Axial Length (OU) | 23.64±1.3 | 23.60±1.1 | 0.756 | 23.57±0.9 | 23.44±1.1 | 0.521 | ||||
| Axial Length (OD) | 23.66±1.3 | 23.58±1.1 | 0.613 | 23.61±0.9 | 23.50±1.1 | 0.310 | ||||
Abbreviations: AMD, age-related macular degeneration; PCV, polypoidal choroidal vasculopathy; CNV, choroidal neovascularization without PCV; BMI, Body Mass Index; D, diopters; OU, oculus uterque (both eyes); OD, oculus dexter (the right eye).
*comparison with controls,
°calculated only in phakic eyes
Of the 86 genotyped SNPs, SNPs CRP rs876538, APP rs11911934, and LIPA rs13500 showed no variation within this cohort and were removed from further analysis. After data cleaning in PLINK, 82 SNPs were tested for association with exudative AMD, typical CNV, PCV, and PCV vs. typical CNV separately among 303 cases and 384 controls. All 82 SNPs were in HWE. After correction for multiple testing, three SNPs in the ARMS2/HTRA1 region (rs10490924, rs11200638, and rs2736911) and CFH rs800292 remained significantly associated with exudative AMD (Table 2). For the other analyses, only ARMS2 rs10490924 and HTRA1 rs11200638 were significantly associated with typical CNV and PCV after correction for multiple testing (Tables 3 and 4). There were no SNPs significantly associated with PCV compared to typical CNV after correcting for multiple testing. Results of the association analysis for all 82 SNPs are listed in S1 Table.
Table 2. Significant Association Results from PLINK comparing Exudative AMD vs. Normal.
| CHR | SNP | BP | A1 | Freq (A) | Freq (U) | A2 | CHISQ | Odds Ratio (95% CI) | UNADJ p | GC p | BONF p | FDR_BH p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | rs800292 | 194908856 | T | 0.290 | 0.401 | C | 18.06 | 0.612 (0.4876–0.7681) | 2.14E-05 | 0.0076 | 0.0018 | 0.0006 |
| 10 | rs2736911 | 124204345 | C | 0.898 | 0.833 | T | 11.77 | 1.755 (1.269–2.427) | 0.0006 | 0.0311 | 0.0493 | 0.0123 |
| 10 | rs10490924 | 124204438 | T | 0.654 | 0.396 | G | 90.05 | 2.881 (2.309–3.595) | 2.32E-21 | 2.52E-09 | 1.91E-19 | 1.91E-19 |
| 10 | rs11200638 | 124210534 | A | 0.655 | 0.402 | G | 86.71 | 2.825 (2.264–3.524) | 1.26E-20 | 4.95E-09 | 1.03E-18 | 5.15E-19 |
SNPs shown above are those that remained significant after correction for multiple testing.
Abbreviations: CHR, chromosome; SNP, Single Nucleotide Polymorphism; BP, base pairs; A1, allele 1; Freq (A), frequency of allele 1 in affecteds; Freq (U) frequency of allele 1 in unaffecteds; A2, allele 2; CHISQ, Chi Square value; C.I., confidence interval; GC, Genomic-control; BONF, Bonferroni single-step adjusted; HOLM, Holm (1979) step-down adjusted; SIDAK SS, Sidak single-step adjusted; SIDAK SD, Sidak step-down adjusted; FDR BH, Benjamini & Hochberg (1995) step-up FDR control), and FDR BY (Benjamini & Yekutieli (2001) step-up FDR control).
Table 3. Significant Association Results from PLINK comparing CNV vs. Normal.
| CHR | SNP | BP | A1 | Freq (A) | Freq (U) | A2 | CHISQ | Odds Ratio (95% CI) | UNADJ p | GC p | BONF p | FDR_BH p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | rs10490924 | 124204438 | T | 0.637 | 0.396 | G | 51.35 | 2.684(2.04–3.532) | 7.73E-13 | 1.48E-04 | 6.34E-11 | 6.34E-11 |
| 10 | rs11200638 | 124210534 | A | 0.637 | 0.402 | G | 48.55 | 2.612 (1.986–3.436) | 3.22E-12 | 2.25E-04 | 2.64E-10 | 1.32E-10 |
SNPs shown above are those that remained significant after correction for multiple testing.
Abbreviations: CHR, chromosome; SNP, Single Nucleotide Polymorphism; BP, base pairs; A1, allele 1; Freq (A), frequency of allele 1 in affecteds; Freq (U) frequency of allele 1 in unaffecteds; A2, allele 2; CHISQ, Chi Square value; C.I., confidence interval; GC, Genomic-control; BONF, Bonferroni single-step adjusted; HOLM, Holm (1979) step-down adjusted; SIDAK SS, Sidak single-step adjusted; SIDAK SD, Sidak step-down adjusted; FDR BH, Benjamini & Hochberg (1995) step-up FDR control), and FDR BY (Benjamini & Yekutieli (2001) step-up FDR control).
Table 4. Significant Association Results from PLINK comparing PCV vs. Normal.
| CHR | SNP | BP | A1 | Freq (A) | Freq (U) | A2 | CHISQ | Odds Ratio (95% CI) | UNADJ p | GC p | BONF p | FDR_BH p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | rs10490924 | 124204438 | T | 0.637 | 0.396 | G | 39.08 | 2.679 (1.955–3.672) | 4.08E-10 | 2.36E-06 | 3.34E-08 | 3.34E-08 |
| 10 | rs11200638 | 124210534 | A | 0.637 | 0.402 | G | 36.91 | 2.607 (1.903–3.572) | 1.24E-09 | 4.50E-06 | 1.01E-07 | 5.06E-08 |
SNPs shown above are those that remained significant after correction for multiple testing.
Abbreviations: CHR, chromosome; SNP, Single Nucleotide Polymorphism; BP, base pairs; A1, allele 1; Freq (A), frequency of allele 1 in affecteds; Freq (U) frequency of allele 1 in unaffecteds; A2, allele 2; CHISQ, Chi Square value; C.I., confidence interval; GC, Genomic-control; BONF, Bonferroni single-step adjusted; HOLM, Holm (1979) step-down adjusted; SIDAK SS, Sidak single-step adjusted; SIDAK SD, Sidak step-down adjusted; FDR BH, Benjamini & Hochberg (1995) step-up FDR control), and FDR BY (Benjamini & Yekutieli (2001) step-up FDR control).
As shown in Table 5, logistic regression analysis showed that age and both smoking measures, but not BMI, were significantly associated with increased risk of exudative AMD when compared to normal (p < .05). For phakic eyes, spherical equivalent was associated with increased risk of exudative AMD while myopia showed a protective effect. For typical CNV, significant epidemiological risk factors were age and hypertension, while hyperlipidemia was shown to be protective of typical CNV when compared to normal. For phakic eyes, spherical equivalent was associated with increased risk of CNV, while myopia showed a protective effect. For PCV, increased education and smoking (both measures) were shown to increase risk of disease when compared to normal subjects. Additionally, in phakic eyes, spherical equivalent was associated with increased risk of PCV. When comparing PCV to typical CNV cases, higher education and ever smoking were shown to increase risk of PCV, while increased age was shown to be protective of PCV when compared to typical CNV cases. Interestingly, no significant associations were seen between AMD or its subtypes and axial length by either measure. No significant statistical interaction was seen between any of the risk factors examined, including smoking and the most commonly associated AMD SNPs in ARMS2/HTRA1 and CFH after controlling for potential confounders (data not shown).
Table 5. Association of non-genetic risk factors using logistic regression.
| Exudative vs. Normal | CNV vs. Normal | PCV vs. Normal | PCV vs. CNV | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Odds Ratio (95% C.I.) | p value | Odds Ratio (95% C.I.) | p value | Odds Ratio (95% C.I.) | p value | Odds Ratio (95% C.I.) | p value |
| Age (years) | 1.034 (1.017–1.051) | 5.25E-05 | 1.049 (1.028–1.071) | 3.76E-06 | 0.99 (0.969–1.012) | 0.3913 | 0.917 (0.886–0.949) | 7.50E-07 |
| BMI (kg/m2) | 0.985 (0.937–1.035) | 0.5420 | 1.005 (0.946–1.068) | 0.8759 | 0.984 (0.915–1.058) | 0.6603 | 0.981 (0.908–1.061) | 0.6378 |
| Cerebrovascular accident | 1.317 (0.834–2.079) | 0.2376 | 1.43 (0.826–2.475) | 0.2013 | 0.811 (0.392–1.675) | 0.5708 | 0.567 (0.258–1.244) | 0.1571 |
| Diabetes | 0.872 (0.605–1.257) | 0.4619 | 0.806 (0.504–1.287) | 0.3662 | 0.588 (0.329–1.051) | 0.0730 | 0.73 (0.375–1.42) | 0.3537 |
| Education | 1.058 (0.93–1.204) | 0.3891 | 0.939 (0.801–1.101) | 0.4355 | 1.475 (1.199–1.816) | 0.0002 | 1.537 (1.224–1.93) | 0.0002 |
| Hypertension | 1.282 (0.952–1.726) | 0.1015 | 1.588 (1.092–2.309) | 0.0154 | 1.085 (0.712–1.651) | 0.7052 | 0.683 (0.419–1.112) | 0.1254 |
| Hyperlipidemia | 0.748 (0.509–1.099) | 0.1396 | 0.584 (0.347–0.983) | 0.0429 | 0.971 (0.578–1.631) | 0.9110 | 1.661 (0.868–3.18) | 0.1254 |
| Female sex | 0.919 (0.683–1.237) | 0.5781 | 0.809 (0.558–1.172) | 0.2624 | 0.84 (0.552–1.28) | 0.4179 | 1.039 (0.638–1.691) | 0.8773 |
| Spherical Equivalent (SE)° | 1.187 (1.078–1.307) | 0.0005 | 1.157 (1.031–1.297) | 0.0128 | 1.145 (1.013–1.295) | 0.0307 | 0.974 (0.834–1.136) | 0.7347 |
| Myopia° | 0.506 (0.301–0.850) | 0.0101 | 0.517 (0.274–0.977) | 0.0421 | 0.553 (0.285–1.073) | 0.0799 | 1.069 (0.510–2.242) | 0.8595 |
| Axial Length (Average) | 0.970 (0.802–1.174) | 0.7551 | 0.904 (0.701–1.166) | 0.4368 | 1.005 (0.756–1.336) | 0.9730 | 1.142 (0.765–1.706) | 0.5167 |
| Axial Length (OD) | 0.952 (0.786–1.153) | 0.6125 | 0.860 (0.659–1.121) | 0.2644 | 1.022 (0.773–1.351) | 0.8802 | 1.232 (0.825–1.840) | 0.3083 |
| Smoking (2 Level) | 1.582 (1.173–2.132) | 0.0026 | 1.297 (0.894–1.882) | 0.1707 | 2.364 (1.533–3.646) | 9.89E-05 | 1.823 (1.11–2.994) | 0.0178 |
| Smoking (3 Level) | 1.408 (1.136–1.745) | 0.0018 | 1.263 (0.97–1.645) | 0.0826 | 1.718 (1.276–2.313) | 0.0004 | 1.345 (0.956–1.891) | 0.0886 |
PCV = polypoidal choroidal vasculopathy, CNV = choroidal neovascularization without PCV, C.I. = confidence interval, BMI = Body Mass Index
°calculated only in phakic eyes
Additionally, a stepwise regression model was constructed for each AMD association using risk factors determined to be significant for each outcome in single factor analysis (p < .05, Tables 6–9). When comparing exudative AMD cases to controls, the most predictive disease model included age, spherical equivalent as measured in phakic eyes only, smoking (Current/Ex/Never), CFH rs8000292, and ARMS2 rs10490924 (Table 6). The most predictive model for typical CNV included age, hyperlipidemia, spherical equivalent as measured in phakic eyes only, and ARMS2 rs10490924 (Table 7). The most predictive model of PCV included smoking (Ever/Never), spherical equivalent as measured in phakic eyes only, and ARMS2 rs10490924 (Table 8). When comparing PCV to CNV cases, age, BMI, and education were the most predictive variables of PCV (Table 9).
Table 6. Final stepwise regression model for Exudative AMD vs. Normal.
| Risk Factor | Exudative AMD vs. Normal | |
|---|---|---|
| Odds Ratio (95% C.I.) | p value | |
| Age | 1.059 (1.027–1.092) | 0.0002 |
| Spherical Equivalent° | 1.198 (1.068–1.344) | 0.0021 |
| Smoking3 | 1.528 (1.044–2.236) | 0.0289 |
| CFH rs800292 (add) | 0.567 (0.393–0.818) | 0.0024 |
| ARMS2 rs10490924 (add) | 2.664 (1.881–3.772) | 3.39E-08 |
Final stepwise regression models were constructed using risk factors that were shown to be significant in single factor analysis (p < .05).
Abbreviations: C.I., confidence interval; Smoking3, Current/Ex/Never smoking; add, additive genetic model.
°calculated only in phakic eyes
Table 9. Final stepwise regression model for PCV vs. CNV.
| Risk Factor | PCV vs. CNV | |
|---|---|---|
| Odds Ratio (95% C.I.) | p value | |
| Age | 0.914 (0.880–0.949) | 2.65E-06 |
| BMI | 0.891 (0.812–0.979) | 0.0159 |
| Education | 1.457 (1.134–1.872) | 0.0032 |
Final stepwise regression models were constructed using risk factors that were shown to be significant in single factor analysis (p < .05).
Abbreviations: C.I., confidence interval; BMI, body mass index.
Table 7. Final stepwise regression model for CNV vs. Normal.
| Risk Factor | CNV vs. Normal | |
|---|---|---|
| Odds Ratio (95% C.I.) | p value | |
| Age | 1.075 (1.038–1.114) | 6.82E-05 |
| Hyperlipidemia | 0.405 (0.191–0.859) | 0.0185 |
| Spherical Equivalent° | 1.188 (1.037–1.361) | 0.0128 |
| ARMS rs10490924 (add) | 2.527 (1.674–3.814) | 1.03E-05 |
Final stepwise regression models were constructed using risk factors that were shown to be significant in single factor analysis (p < .05).
Abbreviations: C.I., confidence interval; add, additive genetic model.
°calculated only in phakic eyes
Table 8. Final stepwise regression model for PCV vs. Normal.
| Risk Factor | PCV vs. Normal | |
|---|---|---|
| Odds Ratio (95% C.I.) | p value | |
| Smoking2 | 2.460 (1.359–4.453) | 0.0030 |
| Spherical Equivalent° | 1.187 (1.033–1.364) | 0.0156 |
| ARMS2 rs10490924 (add) | 2.382 (1.549–3.664) | 7.79E-05 |
Final stepwise regression models were constructed using risk factors that were shown to be significant in single factor analysis (p < .05).
Abbreviations: C.I., confidence interval; Smoking2, Ever/Never smoking; add, additive genetic model.
°calculated only in phakic eyes
Discussion
This is the first study to investigate the association of environmental factors and numerous candidate gene SNPs and their interactions in a relatively large number of Korean AMD patients. Two SNPs, ARMS2/HTRA1 rs10490924 and rs11200638, were significantly associated with exudative AMD and its subtypes, typical CNV and PCV. Age, smoking, hypertension, hyperlipidemia, spherical equivalent (phakic eyes only), and education were significant environmental factors for Korean AMD, while there were no statistically significant interactions between genetic and environmental risk factors affecting risk of AMD.
The ARMS2/HTRA1 genes have been widely reported as the major susceptibility genes for AMD in both Caucasian and Asian ethnicities.[2,22] As for CFH, which was the first reported risk gene for Caucasian AMD, there have been controversies surrounding its association with Asian AMD owing to the low frequency of the risk allele in the well-recognized Y402H (rs1061170) variant in Asians.[23–27] Subsequent meta-analyses have shown that this is not the case, with both ARMS2/HTRA1 and CFH gene being significantly associated with AMD in Asians, as well as its subtype, PCV.[28,29] In our Korean cohort, the ARMS2/HTRA1 rs10490924 and rs11200638 SNPs were significant risk factors for exudative AMD as well as its subtypes typical CNV and PCV. Like Chen et al., who also studied CFH variants in Asians,[28] we found association with CFH rs800292 and exudative AMD, and not CFH Y402H (rs1061170). These SNPs are independent signals, i.e. not in high LD (r2 = 4, data not shown) and show different direction of effect. The lack of significance between CFH rs800292 and the specific disease subtypes is likely due to the sample size, while the lack of significance of the CFH Y402H variant (rs1061170) in this cohort is likely due to the sample size and the low MAF. The risk allele of Y402H, C, was only found at 7.9% in exudative cases and 9% in controls in this cohort of Koreans, while Caucasians have shown the risk allele to be as frequent as 35%.[30] Meta-analyses increasing sample size to gain adequate statistical power have shown statistically significant differences.[29]
Among environmental factors, age, smoking, hypertension, hyperlipidemia, spherical equivalent, and education were associated with AMD. Most of these factors have already been identified as risk factors for AMD.[31,32] A recent study analyzing data from the Korean National Health and Nutrition Examination survey, a large-scale population-based cross-sectional survey, also reported age and smoking to be associated with late AMD in Koreans.[33] While age was significantly different between our exudative cases and controls, the average age of all subjects was greater than that at which AMD is commonly diagnosed, 50 years, limiting the concern of our controls developing AMD.[34] Age was also included in the stepwise regression models to control for confounding effects. Additionally, of interest, education was found to increase the risk of disease in the PCV subtype when compared to CNV subtypes, which could not be explained by refractive error. Past studies have identified higher education as a protective factor for developing AMD and the reason for the inverse finding in our Korean cohort is difficult to explain as different levels of education may be associated with numerous other factors the association of which may not have been assessed in this study.[17,35,36]
Other notable findings include the protective effect of hyperlipidemia (for typical CNV), diabetes and BMI (for PCV) in single factor analysis. Of these findings, hyperlipidemia and BMI remained important predictors of CNV and PCV, respectively, in stepwise regression. Whether these systemic factors are actually associated with AMD have already been disputed in the past.[37,38] When systemic risk factors for CNV and PCV were compared, CNV was associated with higher prevalence of diabetes compared to PCV.[39,40] The apparent negative association of obesity with AMD was recently reported in Koreans and maybe a distinct feature of Korean AMD.[33] Further larger size population studies will be required to validate our findings.
As for the interaction between smoking and genetic risk factors in AMD, some studies conducted in Caucasians, Japanese and Koreans have advocated the presence of a significant interaction between smoking and AMD risk genes, CFH and ARMS2/HTRA1.[5,15,16] However, most of these studies evaluated smoking-genetic interaction with limited variables in isolation rather than use a regression model with all known genetic and environmental risk factors included. In the study by Nakanishi et al, although logistic regression analysis with the variables age, sex, smoking status, CFH, ARMS2 failed to show a significant interaction between smoking and genetic factors, the authors used the synergy index to suggest a joint smoking-genetic effect.[15] Other studies have failed to find a significant interaction between smoking and genetic risk factors.[41,42] We also found no significant interaction of genetic and environmental risk factors in our Korean cohort when controlling for other significant risk factors.
Although the influence of smoking and high-risk genotypes on the risk of AMD in Koreans should be regarded as significant, the absolute risk of developing AMD and exudative AMD is difficult to estimate accurately in samples collected in a tertiary hospital. Also, our study did not have sufficient statistical power due to the number of patients enrolled and hence well-designed large population-based prospective studies are necessary to reveal the exact interaction of smoking and susceptible genotypes in Koreans. The validity of our result depends on the extent to which our case-control dataset represents the population-based samples of AMD patients and controls. As many clinical parameters such as smoking and education are obtained by interviews, there is a potential for recall bias. Additionally, due to the nature of the recruitment of this study, details of refractive error were not available for the entire cohort examined; therefore, these novel findings should be validated. Future studies should include obtaining refractive error data, specifically spherical equivalent, for study as we have shown it to be an important risk factor in AMD and its subtypes.
In conclusion, variants ARMS2/HTRA1 rs10490924 and rs11200638 are significant genetic risk factors for Korean exudative AMD and its subtypes CNV and PCV. Age, smoking, hyperlipidemia, spherical equivalent, and education are important environmental factors whilst there was no significant smoking-gene interaction in our Korean cohort.
Supporting Information
Table a shows the complete association results for all SNPs tested with exudative AMD. Table b shows the complete SNP associations with CNV. Table c shows the complete SNP associations with PCV and Table d shows the complete SNP associations between PCV and CNV.
(DOC)
Data Availability
Data have been deposited to Figshare (http://dx.doi.org/10.6084/m9.figshare.1420565).
Funding Statement
This study was supported by the Seoul National University Bundang Hospital Research Fund (Grant No. 03-2009-008), National Research Foundation of Korea (NRF) grants funded by the Ministry of Education, Science, and Technology (2009-0072603, 2012R1A1A2008943), an unrestricted grant from Research to Prevent Blindness (http://www.rpbusa.org/rpb/) to the Department of Ophthalmology and Visual Sciences – Moran Eye Center, and the ALSAM Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Deangelis MM, Silveira AC, Carr EA, Kim IK (2011) Genetics of age-related macular degeneration: current concepts, future directions. Semin Ophthalmol 26: 77–93. 10.3109/08820538.2011.577129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fritsche LG, Chen W, Schu M, Yaspan BL, Yu Y, Thorleifsson G, et al. (2013) Seven new loci associated with age-related macular degeneration. Nat Genet 45: 433–439, 439e1–e2. 10.1038/ng.2578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Swaroop A, Chew EY, Rickman CB, Abecasis GR (2009) Unraveling a multifactorial late-onset disease: from genetic susceptibility to disease mechanisms for age-related macular degeneration. Annu Rev Genomics Hum Genet 10: 19–43. 10.1146/annurev.genom.9.081307.164350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gorin MB (2012) Genetic insights into age-related macular degeneration: controversies addressing risk, causality, and therapeutics. Mol Aspects Med 33: 467–486. 10.1016/j.mam.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schmidt S, Hauser MA, Scott WK, Postel EA, Agarwal A, Gallins P, et al. (2006) Cigarette smoking strongly modifies the association of LOC387715 and age-related macular degeneration. Am J Hum Genet 78: 852–864. 10.1086/503822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mori K, Horie-Inoue K, Gehlbach PL, Takita H, Kabasawa S, Kawasaki I, et al. (2010) Phenotype and genotype characteristics of age-related macular degeneration in a Japanese population. Ophthalmology 117: 928–938. 10.1016/j.ophtha.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 7. Singerman LJ, Brucker AJ, Jampol LM, Lim JI, Rosenfeld P, Schachat AP, et al. (2005) Neovascular age-related macular degeneration: roundtable. Retina (Philadelphia, Pa) 25: S1–S22. [DOI] [PubMed] [Google Scholar]
- 8. Maruko I, Iida T, Saito M, Nagayama D, Saito K (2007) Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol 144: 15–22. 10.1016/j.ajo.2007.03.047 [DOI] [PubMed] [Google Scholar]
- 9. Liu Y, Wen F, Huang S, Luo G, Yan H, Sun Z, et al. (2007) Subtype lesions of neovascular age-related macular degeneration in Chinese patients. Graefes Arch Clin Exp Ophthalmol 245: 1441–1445. 10.1007/s00417-007-0575-8 [DOI] [PubMed] [Google Scholar]
- 10. Park KH, Song SJ, Lee WK, Yoon HS, Koh HJ, Kim CG, et al. (2010) The Results of Nation-Wide Registry of Age-related Macular Degeneration in Korea. Journal of the Korean Ophthalmological Society 51: 516 10.3341/jkos.2010.51.4.516 [DOI] [Google Scholar]
- 11. Kondo N, Honda S, Kuno S, Negi A (2009) Coding variant I62V in the complement factor H gene is strongly associated with polypoidal choroidal vasculopathy. Ophthalmology 116: 304–310. 10.1016/j.ophtha.2008.11.011 [DOI] [PubMed] [Google Scholar]
- 12. Gotoh N, Nakanishi H, Hayashi H, Yamada R, Otani A, Tsujikawa A, et al. (2009) ARMS2 (LOC387715) variants in Japanese patients with exudative age-related macular degeneration and polypoidal choroidal vasculopathy. Am J Ophthalmol 147: 1037–1041, 1041.e1–2. 10.1016/j.ajo.2008.12.036 [DOI] [PubMed] [Google Scholar]
- 13. Kabasawa S, Mori K, Horie-Inoue K, Gehlbach PL, Inoue S, Awata T, et al. (2011) Associations of cigarette smoking but not serum fatty acids with age-related macular degeneration in a Japanese population. Ophthalmology 118: 1082–1088. 10.1016/j.ophtha.2010.10.012 [DOI] [PubMed] [Google Scholar]
- 14. Chen H, Liu K, Chen LJ, Hou P, Chen W, Pang CP, et al. (2012) Genetic associations in polypoidal choroidal vasculopathy: a systematic review and meta-analysis. Mol Vis 18: 816–829. [PMC free article] [PubMed] [Google Scholar]
- 15. Nakanishi H, Yamashiro K, Yamada R, Gotoh N, Hayashi H, Nakata I, et al. (2010) Joint effect of cigarette smoking and CFH and LOC387715/HTRA1 polymorphisms on polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci 51: 6183–6187. 10.1167/iovs.09-4948 [DOI] [PubMed] [Google Scholar]
- 16. Lee SJ, Kim NR, Chin HS (2010) LOC387715/HTRA1 polymorphisms, smoking and combined effects on exudative age-related macular degeneration in a Korean population. Clin Experiment Ophthalmol 38: 698–704. 10.1111/j.1442-9071.2010.02316.x [DOI] [PubMed] [Google Scholar]
- 17. Age-Related Eye Disease Study Research Group (2000) Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report Number 3. Ophthalmology 107: 2224–2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Imamura Y, Engelbert M, Iida T, Freund KB, Yannuzzi LA (2010) Polypoidal choroidal vasculopathy: a review. Surv Ophthalmol 55: 501–515. 10.1016/j.survophthal.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 19. Jhoo JH, Kim KW, Huh Y, Lee SB, Park JH, Lee JJ, et al. (2008) Prevalence of dementia and its subtypes in an elderly urban korean population: results from the Korean Longitudinal Study on Health And Aging (KLoSHA). Dement Geriatr Cogn Disord 26: 270–276. 10.1159/000160960 [DOI] [PubMed] [Google Scholar]
- 20. Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological) 57: 289–300. [Google Scholar]
- 21. Keller MC (2014) Gene × environment interaction studies have not properly controlled for potential confounders: the problem and the (simple) solution. Biol Psychiatry 75: 18–24. 10.1016/j.biopsych.2013.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Arakawa S, Takahashi A, Ashikawa K, Hosono N, Aoi T, Yasuda M, et al. (2011) Genome-wide association study identifies two susceptibility loci for exudative age-related macular degeneration in the Japanese population. Nat Genet 43: 1001–1004. 10.1038/ng.938 [DOI] [PubMed] [Google Scholar]
- 23. Klein RJ, Zeiss C, Chew EY, Tsai J- Y, Sackler RS, Haynes C, et al. (2005) Complement factor H polymorphism in age-related macular degeneration. Science 308: 385–389. 10.1126/science.1109557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P, et al. (2005) Complement factor H variant increases the risk of age-related macular degeneration. Science 308: 419–421. 10.1126/science.1110359 [DOI] [PubMed] [Google Scholar]
- 25. Edwards AO, Ritter R 3rd, Abel KJ, Manning A, Panhuysen C, Farrer LA. (2005) Complement factor H polymorphism and age-related macular degeneration. Science 308: 421–424. 10.1126/science.1110189 [DOI] [PubMed] [Google Scholar]
- 26. Gotoh N, Yamada R, Hiratani H, Renault V, Kuroiwa S, Monet M, et al. (2006) No association between complement factor H gene polymorphism and exudative age-related macular degeneration in Japanese. Hum Genet 120: 139–143. 10.1007/s00439-006-0187-0 [DOI] [PubMed] [Google Scholar]
- 27. Kim NR, Kang JH, Kwon OW, Lee SJ, Oh JH, Chin HS. (2008) Association between complement factor H gene polymorphisms and neovascular age-related macular degeneration in Koreans. Invest Ophthalmol Vis Sci 49: 2071–2076. 10.1167/iovs.07-1195 [DOI] [PubMed] [Google Scholar]
- 28. Chen LJ, Liu DTL, Tam POS, Chan WM, Liu K, Chong KKL, et al. (2006) Association of complement factor H polymorphisms with exudative age-related macular degeneration. Mol Vis 12: 1536–1542. [PubMed] [Google Scholar]
- 29. Kondo N, Bessho H, Honda S, Negi A (2011) Complement factor H Y402H variant and risk of age-related macular degeneration in Asians: a systematic review and meta-analysis. Ophthalmology 118: 339–344. 10.1016/j.ophtha.2010.06.040 [DOI] [PubMed] [Google Scholar]
- 30. Thakkinstian A, Han P, McEvoy M, Smith W, Hoh J, Magnusson K, et al. (2006) Systematic review and meta-analysis of the association between complement factor H Y402H polymorphisms and age-related macular degeneration. Hum Mol Genet 15: 2784–2790. 10.1093/hmg/ddl220 [DOI] [PubMed] [Google Scholar]
- 31. Tomany SC, Wang JJ, Van Leeuwen R, Klein R, Mitchell P, Vingerling JR, et al. (2004) Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology 111: 1280–1287. 10.1016/j.ophtha.2003.11.010 [DOI] [PubMed] [Google Scholar]
- 32. Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY (2012) Age-related macular degeneration. Lancet 379: 1728–1738. 10.1016/S0140-6736(12)60282-7 [DOI] [PubMed] [Google Scholar]
- 33. Park SJ, Lee JH, Woo SJ, Ahn J, Shin JP, Song SJ, et al. (2014) Age-related macular degeneration: prevalence and risk factors from Korean National Health and Nutrition Examination Survey, 2008 through 2011. Ophthalmology 121: 1756–1765. 10.1016/j.ophtha.2014.03.022 [DOI] [PubMed] [Google Scholar]
- 34. Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. (1995) An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol 39: 367–374. [DOI] [PubMed] [Google Scholar]
- 35. Seddon JM, Reynolds R, Maller J, Fagerness JA, Daly MJ, Rosner B. (2009) Prediction model for prevalence and incidence of advanced age-related macular degeneration based on genetic, demographic, and environmental variables. Invest Ophthalmol Vis Sci 50: 2044–2053. 10.1167/iovs.08-3064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ristau T, Ersoy L, Hahn M, den Hollander AI, Kirchhof B, Liakopoulos S, et al. (2014) Nongenetic risk factors for neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 55: 5228–5232. 10.1167/iovs.14-14299 [DOI] [PubMed] [Google Scholar]
- 37. Klein R, Klein BEK, Tomany SC, Cruickshanks KJ (2003) The association of cardiovascular disease with the long-term incidence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology 110: 1273–1280. 10.1016/S0161-6420(03)00599-2 [DOI] [PubMed] [Google Scholar]
- 38. Tan JSL, Mitchell P, Smith W, Wang JJ (2007) Cardiovascular risk factors and the long-term incidence of age-related macular degeneration: the Blue Mountains Eye Study. Ophthalmology 114: 1143–1150. 10.1016/j.ophtha.2006.09.033 [DOI] [PubMed] [Google Scholar]
- 39. Ueta T, Obata R, Inoue Y, Iriyama A, Takahashi H, Yamaguchi T, et al. (2009) Background comparison of typical age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology 116: 2400–2406. 10.1016/j.ophtha.2009.06.013 [DOI] [PubMed] [Google Scholar]
- 40. Sakurada Y, Yoneyama S, Imasawa M, Iijima H (2013) Systemic risk factors associated with polypoidal choroidal vasculopathy and neovascular age-related macular degeneration. Retina (Philadelphia, Pa) 33: 841–845. [DOI] [PubMed] [Google Scholar]
- 41. DeAngelis MM, Ji F, Kim IK, Adams S, Capone A Jr, Ott J, et al. (2007) Cigarette smoking, CFH, APOE, ELOVL4, and risk of neovascular age-related macular degeneration. Arch Ophthalmol 125: 49–54. 10.1001/archopht.125.1.49 [DOI] [PubMed] [Google Scholar]
- 42. Conley YP, Jakobsdottir J, Mah T, Weeks DE, Klein R, Kuller L, et al. (2006) CFH, ELOVL4, PLEKHA1 and LOC387715 genes and susceptibility to age-related maculopathy: AREDS and CHS cohorts and meta-analyses. Hum Mol Genet 15: 3206–3218. 10.1093/hmg/ddl396 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table a shows the complete association results for all SNPs tested with exudative AMD. Table b shows the complete SNP associations with CNV. Table c shows the complete SNP associations with PCV and Table d shows the complete SNP associations between PCV and CNV.
(DOC)
Data Availability Statement
Data have been deposited to Figshare (http://dx.doi.org/10.6084/m9.figshare.1420565).