Abstract
The purposes of this study were to develop a Social Cognitive Theory (SCT)-based, Structured Hip Fracture Prevention Website (TSW) for older adults and conduct a preliminary evaluation of its effectiveness. The TSW is comprised of learning modules and a moderated discussion board. A total of 245 older adults recruited from two websites and a newspaper advertisement were randomized into the TSW and the Conventional Websites (CW) groups. Outcomes included (1) knowledge (hip fractures and osteoporosis), (2) self-efficacy and outcome expectations, and (3) calcium intake and exercise, and were assessed at baseline, end-of-treatment ([EOT], 2 weeks), and follow-up (3 months). Both groups showed significant improvement in most outcomes. For calcium intake, only the TSW group showed improvement. None of the group and time interactions were significant. The TSW group, however, was more satisfied with the intervention. The discussion board usage was significantly correlated with outcome gains. Despite several limitations, the findings showed some preliminary effectiveness of web-based health interventions for older adults and the use of a TSW as a sustainable web structure for online health behavior change interventions.
Keywords: Social Cognitive Theory-based online intervention, Older adults, Internet, Health promotion, Hip fracture prevention
Each year in the United States, approximately 340,000 older adults experience hip fractures,1 and an estimated 18% to 33% die within one year of the fracture.2,3 Extensive research efforts have been undertaken to identify causes and effective management of hip fractures. Factors that contribute to hip fractures among older adults include low bone density (e.g., osteoporosis), falls/a lack of environmental safety, and multimedication usage.4-7 Prior research findings indicate that hip fractures can be prevented by using a multimodal approach, including dietary intervention (eg, calcium consumption), exercise, medication, environmental management, and screening tests.4,6,7 Unfortunately, many older adults are unaware of the serious impact of or preventive interventions for hip fractures until they experience one.4,7 With the rapidly increasing number of older adult online users and their interest in health, the web can be an appropriate medium to provide older individuals with this important health information. In particular, the web has unique opportunities for older adults, such as being able to learn about health topics at their convenience.8-10
According to a 2004 Pew Internet study,11 22% of Americans age 65 or older (about 8 million) use the Internet, and 66% of them perform online searches for health information. It is expected that by 2010, 70% of older adults will be online.12 Recently, the numbers of health-related websites have significantly increased.13-16 Some of these sites include information related to hip fracture prevention (eg, fall prevention or osteoporosis). However, the topics vary by site and those are not designed to deliver effective education on hip fracture prevention to older adult population. In general, older adults have unique web usability issues due to psychomotor and cognitive changes, and many of them have learned to use the web to do simple searches. These individuals therefore have some difficulty in finding and synthesizing specific health information from multiple websites. The amount of information available online could also be overwhelming to them.9,17,18
In this developmental and planning grant project (R21 AG026013, National Institute on Aging), we developed an innovative Social Cognitive Theory (SCT)-based Structured hip fracture prevention Website (TSW) and conducted a preliminary evaluation of its effectiveness. As a preliminary study, we conducted a randomized controlled trial (RCT) using a short-term (2-week) intervention period. (Based on the findings, our next phase of research will use a longer-term theory-based intervention to assess its long-term impact on health behaviors.) The interventions were focused on improving older adults’ health behaviors to prevent hip fractures. The effects of the TSW, which used (1) structured web learning modules and (2) moderated discussion boards, were assessed compared to those of the Conventional hip fracture prevention Website (CW) that included only learning modules, without the discussion board. The CW included the same number of modules and learning objectives. The CW, however, was comprised of lists of hyperlinks to other relevant, pre-selected websites instead of the structured abstracted content.
The outcomes included: (1) knowledge (hip fractures and osteoporosis) gains; (2) self-efficacy (calcium intake, exercise, and web-based learning); (3) outcome expectations (calcium intake, exercise); and (4) the use of preventive hip fracture behaviors (dietary calcium intake and exercise). Specifically, we hypothesized that: (1) participants in both groups would improve significantly over the study period with respect to knowledge, self-efficacy, and outcome expectations and the use of hip fracture prevention behaviors; and (2) participants in the TSW group would exhibit significantly greater gains on these outcome variables than participants who were given access to the conventional websites.
A Theory-Driven, Structured Hip Fracture Prevention Website for Older Adults
Numerous health websites have been developed to provide health information to the public.13-16 Few studies, however, have been conducted to investigate effective methods to package and deliver online health information to improve the health outcomes of specific populations.
In our study, we developed the TSW in accordance with the SCT (ie, self-efficacy and outcome expectations theory) because they are proven to be effective in changing individuals’ health behaviors.19-21 In the SCT,22-24 a person's belief in his/her ability to carry out a behavior (self-efficacy) and in its benefit (outcome expectations) promote the person's health behaviors. Efficacy beliefs can be enhanced through the following mechanisms: (1) enactive mastery experience (ie, through ones’ prior successful accomplishments); (2) vicarious experiences (ie, through modeling others’ successful performances); (3) verbal persuasion (ie, through verbal encouragement); and (4) improvement in physiological and emotional states (eg, pain relief or reduction of stress and negative mood). The TSW provided these four mechanisms using web-based learning modules and moderated discussion boards. For instance, in the web modules, the individual's mastery experiences for taking calcium and performing exercise was facilitated through instructions for setting personal goals, keeping track of health behaviors using diaries, and stressing the importance of rewarding oneself upon meeting goals. On our discussion board, the moderator followed up on participants’ ongoing health behaviors using specific discussion questions. Vicarious experiences and social modeling were provided using demonstration video clips and pictures as well as testimonials. The learning modules also included various techniques and information to alleviate pain or stress. On the discussion board, participants shared their own strategies to maintain better physical and emotional states.
Methods
Design
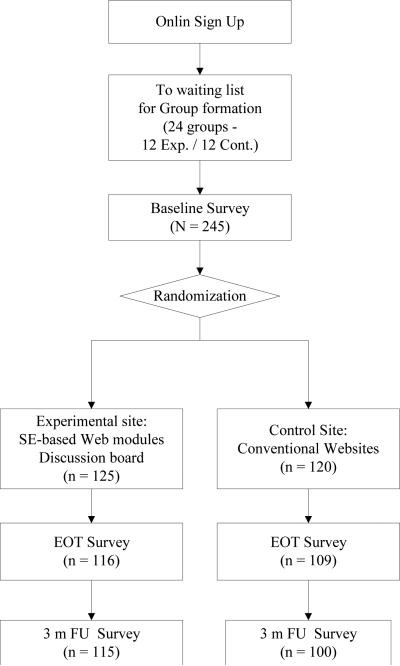
This was a randomized controlled trial (RCT) using a two-group comparison design with repeated measures (baseline, EOT, and 3-months follow-up). Approximately 20 participants in each cohort were randomly assigned to one of the two groups (TSW and CW) with participants within each cohort beginning the interventions simultaneously. (Figure 1 summarizes the overview of the trial.)
Figure 1.
Overview of the study.
Sample/Settings/Recruitment
Upon approval from the University of Maryland Institutional Review Board (UMIRB), 245 participants were recruited online from SeniorNet (http://www.seniornet.org) and Baltimore Times Online (http://www.btimes.com) as well as through advertisements in the Baltimore Times newspaper (print version) between September 2006 and January 2007. The sample size was based upon a power analysis employing effect sizes emanating from prior studies.25,26 SeniorNet, a leading older adult online community with 30,000 members nationwide, provides older adults with education for and access to computer technologies. The Baltimore Times, a weekly newspaper distributed primarily to the African-American community in Maryland, maintainsBaltimore Times Online. This newspaper site was selected in an effort to include more minority participants.
Participants were eligible if they (1) were age 55 years or older; (2) had access to the Internet/e-mail (at home, public libraries, work places, etc); (3) could use the Internet/e-mail independently; (4) resided in a community setting in the United States; and (5) could read and write English. Participants were excluded if they had a hip fracture prior to the study and/or wereparticipating in any other studies on falls, osteoporosis, and/or nutrition. A total of 245 older adults participated in the study. Table 1 summarizes general demographics of the participants. The majority of the participants were female (n = 192, 78.4%) and White (n = 223, 91.0%), with a mean age of 69.3 ± 7.7 years. The majority (n = 212, 85.5%) had some college or higher education. The average years of web experience was 10.0 ± 5.2, and their average web use per week was 13.1 ± 12.8 hours. Participants’ overall age, education level and computer experience were similar to those of SeniorNet members (data from SeniorNet, 2006).
Table 1.
Baseline Differences in Demographic Variables
| Variable | Total Sample (%) | TSW (%) | CW (%) | p |
|---|---|---|---|---|
| Gender | ||||
| Male | 53 (21.6%) | 19 (15.2%) | 34 (28.3%) | .013 |
| Female | 192 (78.4%) | 106 (84.8%) | 86 (77.7%) | |
| Age | ||||
| <65 | 69 (28.2%) | 35 (28.0%) | 34 (28.3%) | .685 |
| 65-74 | 102 (41.6%) | 55 (44.0%) | 47 (39.2%) | |
| ≥75 | 74 (30.2%) | 35 (28.0%) | 39 (32.5%) | |
| Ethnicity | ||||
| White | 223 (91.0%) | 112 (89.6%) | 111(92.5%) | .547 |
| African American | 18 (7.3%) | 10 (8.0%) | 8 (6.7%) | |
| Others | 4 (1.6 %) | 3 (2.4%) | 1 (0.8%) | |
| Education | ||||
| HS or Below | 33 (13.5% | 15 (12.0%) | 18 (15.0%) | .818 |
| Some College/ College Degree | 148 (58.4%) | 79 (63.2%) | 68 (57.5%) | |
| Graduate Degree | 64 (26.1%) | 31 (24.8%) | 33 (27.5%) | |
| WEB Experience | ||||
| <5 years | 31 (12.8%) | 18 (14.4%) | 13 (11.0%) | .583 |
| 5-10 Years | 120 (49.4%) | 63 (50.4%) | 57 (48.3%) | |
| >10 Years | 92 (37.9%) | 44 (35.2%) | 48 (40.7%) |
A brief description of the study, the eligibility criteria, and a hyperlink to the secure study website were posted on SeniorNet and Baltimore Times Online. The same information was also included in the monthly SeniorNet online newsletter and the weekly Baltimore Times newspaper. The eligibility screening and consent processes were completed online. A toll-free phone number was available on the study website for any questions. Individuals who completed the consent process were contacted via phone within 48 hours and placed on a waiting list until a cohort of approximately 20 (10 in each group) was recruited. The waiting period was no longer than two weeks throughout the study. Selected participant demographic information (eg, gender, age, history of hip fractures, etc.) was validated during the initial telephone contact.
Interventions
The project website included the TSW, CW, and online surveys. Usability tests were conducted for all three sections.
Theory-based structured HFP website (TSW)
The majority of the following TSW learning modules was developed in a previous study25: Osteoporosis, Falls and Hip Fractures, Dietary / Supplementary Calcium Intake, and Exercise. For this study, the content of the learning modules was reviewed and by an expert panel including a geriatrician, a geriatric nurse practitioner, a dietician and an exercise physiologist. The content was updated and expanded as recommended by the experts. The reading level of the modules was maintained between 6th and 8th grades. The modules were developed emphasizing the benefits of the specific preventive health behaviors and to strengthen older adults’ beliefs about their ability to engage in such behaviors. The modules included text material, video, audio, and self-assessment quizzes using an older adult–friendly format. Transcripts were provided for all audio and video clips for users whose computers were not equipped with playing videos or audios. If the video clips included specific demonstrations, animated pictures were also included as an alternative method. Each module took about 20 to 30 minutes to complete, and participants were encouraged to complete two modules per week.
On the TSW, the discussion boards were moderated by the project manager (PM), who is a registered nurse (RN), using an SCT-based approach. Each week, two behavior-oriented discussion questions (one question per module) were posted (e.g., for the exercise module, “...If you set goals for exercise, which goals did you set for yourself this week? Were you able to meet them? Are there any strategies that help you to keep exercising?”). Participants were encouraged to post their responses and/or questions at least twice per week. The PM carefully monitored the discussions and, if necessary, consulted appropriate experts (eg, geriatric nurse practitioner, geriatrician, orthopedic surgeon). Participants who did not use the discussion board were queried about their lack of use during routine Help Desk follow-ups.
Conventional HFP Websites (CW)
The participants assigned to the CW also completed four learning modules, without the discussion boards. The learning objectives, topics and the web design of the CW were similar to those in the TSW. The content of the CW, however, consisted of hyperlinks to selected relevant health websites for learning objectives instead structured content. Participants were encouraged to achieve learning objectives by exploring the recommended websites for 20 to 30 minutes per module and to complete two modules per week.
Development and maintenance of the study's website and web surveys
A secure web server at the investigators’ university was used for the project. Participants’ web activities (eg, the participant's ID and login time) were monitored using WebTrends® logging software. The web pages were developed using Macromedia Dreamweaver® and Flash MX.®27 The discussion board was developed using the Yabb® program.28 The websites were developed to be older adult friendly following the National Institute on Aging guidelines29 and other prior findings.9,17,18,30 The web surveys were developed using the Remark survey program®.31 Usability of the websites was tested by a usability expert and 10 older adult online users. The websites then were refined based on these findings.
Procedures
When approximately 20 participants were available on the waiting list, they were contacted and given user IDs, passwords, and the URL for the study's website. The first week was allocated for the completion of the baseline survey. Upon completion, participants were randomized to either the TSW or the CW by the study's biostatistician using SPSS Version 15.0. The PM then contacted each participant via e-mail and provided his/her user ID and password. When participants logged into the website, they saw only the intervention assigned to them. The TSW group participants used their user ID as an alias for the discussion board. The Help Desk was available via e-mail and a toll-free phone number weekdays from 8 a.m. to 5 p.m. EST.
After the 2-week intervention period, participants were contacted via e-mail and/or telephone (per their preference) to complete the web-based EOT survey. The web modules were unavailable during the survey period. Most participants completed the survey within one week. Only 24 surveys over the entire study period had to be mailed due to specific issues, including computer/Internet issues (e.g., winter storm), travel, or health conditions. Once the EOT survey was completed, the modules were available again for the next three months (volunteer use only). At the end of the first and the second month after completion of the EOT survey, participants received an e-mail containing a brief thank-you note and information about the due date for the 3-month follow-up survey. At the end of the 3rd month, participants were contacted for the follow-up survey. Upon completion of all three surveys, a check for $40 was mailed to the participants in appreciation of the time they spent on the study.
Measures
Table 2 summarizes measures for the main outcomes and web usability, as well as their assessment points. All outcome measures, except web-based learning self-efficacy, were assessed at baseline, EOT, and 3 months. Self-efficacy for web-based learning was assessed at EOT and 3-month follow-up only because findings from our preliminary studies showed that most older adults were unfamiliar with “web-based learning” and did not have a clear idea about what it was. Usability of websites was also assessed at EOT and 3-month follow-up (after using the sites).
Table 2.
Assessment Points for Main Outcome Measures and Web Usability
| Measures | Baseline | EOT | 3 months |
|---|---|---|---|
| Knowledge: Osteoporosis, Hip fractures | X | X | X |
| Self-Efficacy: Dietary calcium intake, Exercise | X | X | X |
| Self-Efficacy: Web-based learning | X | X | |
| Behavioral change: Dietary calcium intake, Exercise | X | X | X |
| Perceived Web usability | X | X |
Knowledge (exercise, calcium intake, and hip fracture)
The original Osteoporosis Knowledge Test (OKT)32 includes 2 subscales: a 16-item Exercise Scale and a 17-item Calcium Scale. Prior findings reported acceptable internal consistency (KR-20) of the two subscales (α = .69 and .72, respectively). In this study, the calculated alpha coefficients were .74 and .76, respectively.33 Both scales were sufficiently sensitive to detect statistically significant baseline to EOT and baseline to follow-up changes.
Hip fracture knowledge was examined using the 8-item Hip Fractures Knowledge Test (HFKT), which was developed based on the content of the learning module. Stability of the measure was demonstrated in a prior study employing older adults (Pearson's r = .62, p <.001).30
Self-efficacy
Self-efficacy for calcium intake was assessed using a subscale of the Osteoporosis Self-Efficacy Scale (OSE-Calcium).34,35 The original measure includes 11 items with a visual analog scale (VAS, 0-100 mm). In this study, the scale was changed to a 0-10 point Likert scale because a VAS is difficult to administer on the web due to varying computer screen sizes. Prior studies suggested appropriate reliability of the OSE-Calcium (α = .93) and criterion-related validity using self-reported calcium intake.34 Our study also showed some evidence of internal consistency (α =.94), as well as sensitivity to change (p < .001).
Exercise self-efficacy was assessed using the Self-Efficacy for Exercise scale (SEE), a 9-item measure on an 11-point scale ranging from 0 to 10.36 Reliability of the scale was evidenced by squared multiple correlation coefficients (.38 - .76) using structural equation modeling (SEM). Validity of the measure was supported using a hypothesis testing approach.36 Validity coefficients using SEM (all estimates ≥ .81) provided further evidence of validity. Our study also showed evidence of reliability (α = .93).
Self-efficacy for web-based learning was assessed using the Web-Based Learning Self-Efficacy Measure (WBLSEM), an 11-item measure on a 10-point Likert scale.30 The reliability and validity of the WBLSEM were examined in a study employing 33 older adults.30 The calculated alpha coefficient was 0.9, and the measure was stable over time (r = .8, p < .001). The construct validity was examined using the contrasted groups approach.
Outcome expectations
Outcome expectations of calcium intake were assessed using the 6-item Calcium Benefit subscale of the Osteoporosis Health Belief Scale (OHBS).37,32 The scale uses a 5-point Likert scale, and the findings from our study showed evidence of internal consistency (α = .82). Other studies37 reported criterion-related validity of the measure.
Outcome expectations for exercise were assessed using the 9-item Outcome Expectations for Exercise Scale (OEE).38,39 The scale also uses a 5-point Likert scale, and calculated alpha in our study was .82. Validity of the measure was evidenced by the confirmatory factor analysis in prior studies (validity coefficients: .69 −.87 and model fit).38,39
Calcium intake behavior
Dietary calcium intake was assessed using a 22-item measure derived from the Block-National Cancer Institute Health Habits and History Questionnaire (HHHQ).40 The tool assesses both frequency (9-point scales: “never” - “every day”) and portions (3- point scales: small, medium, large). Dietary calcium intakes are calculated using the Diet History Questionnaire database developed by the National Cancer Institute.41 Evidence of concurrent validity was reported using estimates of calcium and vitamin D intakes derived from the 7-day food diary and the short screening instrument (r = .66 and .72, respectively, p < .001).40 The tool was also successfully used in our study as evidenced by sufficient sensitivity to detect significant changes over time. Calculated stability coefficient (r = .56) in our prior study yielded a potentially underestimated value because of the presence of interventions occurring between the two assessment points.
Exercise behavior was measured using the exercise dimension (6 items) of the Yale Physical Activity Survey (YPAS).42 The original 27-item YPAS includes five categories of common groups of work, exercise, and recreational activities performed during a typical week. The measure was stable over time (r = .63, p < .001)42 and has been validated against several physiological variables.42,43 The measure was successfully used in our study. Calculated stability coefficient (r = .59) in our prior study, however, was potentially underestimated due to the same issue discussed in the calcium intake measure.
Descriptive measures
Perceived web usability was assessed using the 12-item Perceived Health Website Usability Questionnaire (PHWUQ).44 The PHWUQ, using a 7-point Likert scale, assesses three dimensions of usability: satisfaction, ease of use, and usefulness. Prior findings supported appropriate reliability (α ranging from .64 to .93) of the measure as well as its validity as indicated by a hypothesis testing (correlation of the scores of the PHWUQ and the results from the heuristic evaluation by usability experts).44 Individuals’ web and discussion board usage were assessed using frequency. In this study, the calculated alpha of the PHWUQ ranged from .85 to .94.
Analyses
Baseline demographic and computer experience differences between the two intervention groups (TSW vs. CW) were assessed via independent sample t-tests for continuous variables and chi-square analyses for categorical variables. Website differences were assessed via a series of mixed linear model analyses in which baseline, EOT, and follow-up assessments were represented as repeated measures and the two treatment groups constituted a between subjects (fixed effect) factor. This analytic model possesses the dual advantages of being robust to many of the assumptions governing the use of general linear models and permits the use of repeated measures employing different numbers of observations. A one-way General Linear Model Analysis of Variance [GLM ANOVA] was employed for the variable self-efficacy for web-based learning because no baseline assessment was performed for this variable. Log10 transformations were used for significantly skewed outcome variables. Data imputation procedures were not necessary because of the low attrition (8.2% at EOT and 11.8% at 3-months) and missing data (< 2%) rates.
To assess the impact of the discussion board use upon outcomes for TSW participants, frequency of usage (ie, message postings) was correlated with EOT and follow-up outcome scores. Covariates were modeled for each outcome variable but failed to consistently meet the a priori set criterion of a covariate-dependent variable relationship of ≥ 0.20. Additionally, subgroup analyses were performed for age, gender, frequency of website usage, and racial group by adding each variable to the overall model as a second between subjects factor. User satisfaction differences between the two websites were assessed via one-way Analysis of Covariance (ANCOVA). Qualitative data, including discussion board postings, Help Desk follow-ups, and e-mail comments, were analyzed using content analysis.45
Results
Baseline demographic and computer experience data and differences between the two intervention groups are presented in Table 1. The TSW group had a slightly higher percentage of females than the CW group (p = .013), but no other statistically significant baseline demographic or computer experience differences were found. Baseline differences between the two groups on outcome variables are presented in Table 3 which indicated that the TSW exceeded CW participants on both outcome expectancy for exercise (p = .04) and initial exercise behavior itself (p = .01). However these differences did not affect the interaction effect between the groups and time points when differences in outcome changes were assessed. During the intervention period, participants accessed the websites overall an average of 4.6 times (ranging from 1 to 15 times). TSW participants averaged 5.6 ± 3.8 visits as compared to 3.5 ± 2.4 visits for CW participants (p < .001). The TSW group showed a 7.1% drop-out rate at 3 months as compared to a 9.2% for the CW group.
Table 3.
Baseline Differences on Outcome Variables
| Variable (range) | Total Sample (SD) | TSW (SD) | CW (SD) | p |
|---|---|---|---|---|
| Knowledge | ||||
| Hip Fracture (0 – 8) | 6.4 (1.4) | 6.5 (1.4) | 6.4 (1.4) | 0.65 |
| Osteoporosis-Calcium (1-16) | 12.0 (3.2) | 11.8 (3.5) | 12.2 (3.0) | 0.25 |
| Osteoporosis-Exercise (1-16) | 10.5 (3.1) | 10.4 (3.3) | 10.6 (2.9) | 0.57 |
| Self-Efficacy | ||||
| Calcium (6 – 60) | 48.4 (11.1) | 48.7 (11.1) | 48.0 (11.1) | 0.66 |
| Exercise (0 – 90) | 54.9 (22.6) | 56.5 (24.3) | 53.2 (20.7) | 0.27 |
| Outcome Expectations | ||||
| Calcium (6 – 30) | 22.4 (3.5) | 22.4 (3.6) | 22.3 (3.5) | 0.74 |
| Exercise (9 – 45) | 36.6 (7.2) | 37.6 (7.0) | 35.7 (7.2) | 0.04 |
| Behavior | ||||
| Calcium (mg) | 1026.5 (675.1) | 974.5 (599.9) | 1087.0 (751.8) | 0.23 |
| Exercise (minutes) | 1038.2 (1207.1) | 1235.0 (1476.3) | 807.1 (723.7) | 0.01 |
Hypotheses Testing
Within-group changes over time
The first hypothesis predicted that participants exposed to either of the web interventions would improve significantly on study outcomes over the study period. As shown in Table 4, this hypothesis was generally supported for knowledge as well as calcium self-efficacy and outcome expectancy. Only TSW participants’ calcium intake showed improvement from baseline to both EOT and follow-up. No significant changes, however, were observed for either group with respect to exercise self-efficacy or exercise behavior.
Table 4.
Group Differences in EOT and Follow-Up Changes from Baseline
| TSW | CW | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcomesa | BL - EOT δ | p | BL – FU Δ | p | BL - EOT Δ | p | BL – FU Δ | p |
| Knowledge | ||||||||
| Hip Fractureb | 1.1 (1.4) | < .001 | 0.1 (1.5) | .032 | 1.3 (1.2) | < .001 | 0.2 (1.3) | .084 |
| Osteoporosis-Calciumb | 2.6 (2.8) | < .001 | 2.3 (3.0) | < .001 | 2.1 (2.3) | < .001 | 1.7 (2.2) | < .001 |
| Osteoporosis-Exercise.b | 2.6 (2.6) | < .001 | 2.3 (2.9) | < .001 | 1.9 (2.2) | < .001 | 1.7 (2.6) | < .001 |
| Self-Efficacy | ||||||||
| Calciumb | 2.7 (2.9) | .004 | 2.5 (10.4) | .012 | 3.3 (10.0) | .001 | 3.9 (11.0) | .001 |
| Exercise | −2.1 (20.9) | .287 | −10.8 (17.3) | .647 | 2.0 (21.5) | .345 | 3.5 (18.7) | .062 |
| Outcome Expectations | ||||||||
| Calciumb | 1.4 (2.9) | < .001 | 1.6 (3.2) | < .001 | 1.2 (2.9) | < .001 | 1.6 (3.0) | < .001 |
| Exerciseb | 0.6 (6.3) | .343 | 1.1 (6.3) | .071 | 2.4 (7.0) | < .001 | 2.2 (7.1) | .003 |
| Behavior | ||||||||
| Calciumc | 154.2 (578.0) | .005 | 168.5 (640.3) | .006 | −7.6 (677.5) | .913 | 13.3 (615.0) | .832 |
| Exercise | −100.6 (1354.6) | .457 | −55.6 (1341.7) | .672 | 73.0 (699.5) | .318 | 120.2 (630.5) | .072 |
* Web-based learning self-efficacy outcome was not included in this table because the data were collected at two points only; BL - Baseline; FU – 3-month follow-up
None of the Treatment × Time interactions approached statistical significance
Time main effect, p < .001
Time main effect, p = .026.
Outcome gains between groups over time
The second hypothesis predicted that the TSW group participants would exhibit significantly greater gains in outcome improvement than the CW group participants. The findings did not show significant differences in outcome gains between the two groups over the two-week study period (Table 4).
At the end of the treatment, the CW (mean = 69.8 ± 12.8) participants exhibited significantly greater self-efficacy for using the site than TSW participants (M = 66.0 ± 16.0) ( p = .03). The TSW participants, however, were significantly more satisfied with their experience with the web intervention (M = 72.9 ± 8.1) than their CW counterparts (M = 69.4 ± 11.8) (p = .045).
Effects of the discussion board and subgroup analyses
Within the TSW group, frequent use of the discussion board was significantly correlated with improvement in EOT self-efficacy for web-based learning and exercise and EOT and follow-up osteoporosis knowledge, calcium consumption, and exercise. Four subgroup analyses were performed involving age, gender, frequency of website usage, and racial subgroup (African-American vs. White and others). There was no trend for any of the four variables to interact with the type of website with respect to changes in the outcomes.
Discussion
Participants in both the TSW and CW improved on most outcomes, which suggests that web-based health interventions can be successfully used to improve the health knowledge and certain health behaviors of older adults. There were, however, no significant changes in exercise self-efficacy or exercise behavior. Although further studies are needed, these results could have been attributed to several limitations in this preliminary study, such as the brief intervention period to change individuals’ exercise behaviors. Furthermore, this study was conducted from September to January, and cold winter weather and holiday seasonal activities could have interrupted their regular exercise practices.46 Further studies are needed using a longer study period and including specific strategies to overcome challenges with severe weather and holidays.
In this study, while the TSW group showed significant improvement in calcium intake behavior over the study period, none of the between group improvements occurring during the study period were statistically significant. A few factors must be taken into consideration in interpreting these findings. In this preliminary study, the amount of structured health information available on the TSW modules during the two week study period was limited. Conversely, the CW included a list of selected credible health websites relevant to the learning objectives instead of structured content, and participants were encouraged to explore those sites during the study protocol. Considering many participants’ relatively high web competency (71.1% perceived themselves as competent web users in their age group) and high education level (85.5% reported some college or higher education), inclusion of selected relevant external health websites in addition to the structured content could have been beneficial to participants. Consequently, a no treatment or wait list control would have provided a more appropriate test of the TSW's specific efficacy.
Some other findings also provided the research team with important information about the amount and presentation of health information in developing and delivering theory-based online health intervention. For instance, online learning modules need to meet each older adult's varying degree of health information needs. A combination of the TSW and CW structure therefore could be an effective approach to present online learning modules intended to improve health behaviors.
The structure of the TSW demonstrated several strengths in implementing an SCT-based online health intervention. Particularly, within the TSW group, the discussion board usage and the outcomes were significantly correlated. The themes that emerged from the discussion postings (e.g., goal settings and follow-ups, encouragement, role modeling, method to relieve discomfort) were consistent with SCT.45 Many participants served as role models and many provided verbal encouragement for each other. (A manuscript with detailed qualitative findings is under review.) These findings are particularly encouraging considering that most participants had no experience in using an online discussion board but successfully learned to use the program within the 2-week intervention period. Furthermore, the TSW participants were significantly more satisfied with their experience with the web program and had a lower drop-out rate (7.1%) than the CW group (9.2%). The short time period (2 weeks) for learning new technology, however, could have contributed to the TSW group's lower self-efficacy for web-based learning than its counterpart. Although further studies are needed, the findings suggest that the TSW structure could be a more sustainable method to deliver longer-term online health interventions than the CW structure.
Conclusion
With rapidly growing technology and its popularity among older adults, there is tremendous opportunity to improve the health behaviors of increasing numbers of older adult online users using web-based interventions. In this exploratory study, we developed an innovative, SCT-based hip fracture prevention website for older adults and tested its preliminary effects on health outcomes. The findings suggest that older adults can benefit from web-based health interventions that promote health behaviors. Furthermore, the SCT-based approach used in this study showed excellent potential for use in more sustainable longer-term online health promotion interventions (ie, high user satisfaction and significant correlation between the discussion board usage and the outcomes). More research must be conducted to test the long-term effects of longer-term interventions using this approach. This study also has several implications for current health informatics practice and research. The advancement and increasing popularity of the Internet presents a great opportunity to use this technology as a medium to disseminate health promotion interventions. This opportunity can be maximized through collaboration among clinicians, researchers, and information technology experts. Health care informaticians are uniquely positioned to drive this effort. Furthermore, effective utilization of technology-based interventions must be incorporated in healthcare education.
Acknowledgments
This study was supported by Grant R21 AG026013 from the National Institute on Aging.
Contributor Information
Eun-Shim Nahm, University of Maryland School of Nursing 655 W. Lombard St, Suite 455 C Baltimore, MD 21201.
Bausell Barker, University of Maryland School of Nursing.
Barbara Resnick, University of Maryland School of Nursing.
Barbara Covington, University of Maryland School of Nursing.
Jay Magaziner, University of Maryland School of Nursing
Patricia Flatley Brennan, University of Wisconsin-Madison.
References
- 1.Thacker SB, Branche C. Reducing Falls and Resulting Hip Fractures Among Older Women. Mortality and Morbidity Weekly Report. 2000;49(RR02):1–12. [PubMed] [Google Scholar]
- 2.Pitto RP. The mortality and social prognosis of hip fractures: A prospective multifactorial study. International Orthopaedics. 1994;18:109–113. doi: 10.1007/BF02484420. [DOI] [PubMed] [Google Scholar]
- 3.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. American Journal of Epidemiology. 2003;157(11):1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 4.New Zealand Guidelines Group [February 27, 2009];Prevention of hip fracture amongst people aged 65 years and over. Available at: http://www.nzgg.org.nz/guidelines/0006/hip_Fracture_Prevention_Fulltext.pdf.
- 5.Rubinstein L. Hip protectors: A breakthrough in fracture prevention. The New England Journal of Medicine. 2000;343(21):1562–1563. doi: 10.1056/NEJM200011233432109. [DOI] [PubMed] [Google Scholar]
- 6.Marks R, Allegrante JP, Ronald MacKenzie C, Lane JM. Hip fractures among the elderly: causes, consequences and control. Ageing Research Reviews. 2003;2(1):57–93. doi: 10.1016/s1568-1637(02)00045-4. [DOI] [PubMed] [Google Scholar]
- 7.Gourlay M, Richy F, Reginster JY. Strategies for the prevention of hip fracture. American Journal of Medicine. 2003;115(4):309–317. doi: 10.1016/s0002-9343(03)00371-1. [DOI] [PubMed] [Google Scholar]
- 8.Nahm ES, Resnick B. Homebound older adults’ experiences with the Internet and e-mail. Computers in Nursing. 2001;19(6):257–263. [PubMed] [Google Scholar]
- 9.Echt KV. Designing Web-based health information for older adults: visual considerations and design directives. In: Morrell RW, editor. Older Adults, Health Information, and the World Wide Web. Lawrence Erlbaum; Mahwah, NJ: 2002. pp. 61–87. [Google Scholar]
- 10.Hendrix CC. Computer use among elderly people. Computers in Nursing. 2000;18(2):62–68. [PubMed] [Google Scholar]
- 11.Fox S. Older Americans and the Internet. [February 27, 2009];Pew Internet & American Life Project. Available at: http://www.pewinternet.org/reports/toc.asp?Report=117.
- 12.Riddle C. [February 27, 2009];e-Health for managed Medicaid & Medicare: Senior's use of the Internet. Available at: http://www.conferenceland.com/nmhccriddle.ppt#9.
- 13.Agency for Healthcare Research and Quality Guide to clinical preventive services. [February 27, 2009];Recommendations of the U.S. preventive services task force. 2006 Available at: http://www.ahrq.gov/clinic/pocketgd.htm.
- 14.National Institute on Aging & National Library of Medicine [February 27, 2009];NIHSeniorHealth.gov. Available at: http://nihseniorhealth.gov/.
- 15.National Osteoporosis Foundation [February 27, 2009];Prevention. Available at: http://www.nof.org/prevention/index.htm.
- 16.The National Library of Medicine [September 20, 2008];MedlinePlus. Available at: www.Medlineplus.gov.
- 17.Morrell RW, Dailey SR, Feldman C, Mayhorn CB, Echt KV. Older adults and information technology: A compendium of scientific research and web site accessibility guidelines. National Institute on Aging; Washington, D. C.: 2001. [Google Scholar]
- 18.Nahm E-S, Preece J, Resnick B, Mills ME. Usability of health Web sites for older adults: A preliminary study. CIN: Computers, Informatics. 2004;22:326–334. 343. doi: 10.1097/00024665-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 19.McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Preventive Medicine. 2003;37(2):110–118. doi: 10.1016/s0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 20.Resnick B. The Impact of self-efficacy and outcome expectations on functional status in older adults. Topics in Geriatric Rehabilitation. 2002;17(4):1–10. [Google Scholar]
- 21.Schnoll R, Zimmerman BJ. Self-regulation training enhances dietary self-efficacy and dietary fiber consumption. Journal of the American Dietetic Association. 2001;101(9):1006–1011. doi: 10.1016/S0002-8223(01)00249-8. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Self-efficacy: The Exercise of Control. Freeman; New York: 1997a. [Google Scholar]
- 23.Bandura A. Self-efficacy in Changing Societies. Cambridge University Press; New York: 1997b. [Google Scholar]
- 24.Bandura A. Health promotion from the perspective of social cognitive theory. Psychological and Health. 1998;13:623–649. [Google Scholar]
- 25.Nahm E-S, Resnick B, Covington B. Development of theory-based, online health learning modules for older adults: Lessons learned. CIN: Computers, Informatics, Nursing. 2006;24(5):261–268. doi: 10.1097/00024665-200609000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Napolitano MA, Fotheringham M, Tate D, et al. Evaluation of an Internet-based Physical Activity intervention: A preliminary investigation. Annals of Behavioral Medicine. 2003;25(2):92–99. doi: 10.1207/S15324796ABM2502_04. [DOI] [PubMed] [Google Scholar]
- 27.Macromedia Inc. [December 20, 2007];Macromedia Studio 8. Available at: http://www.adobe.com/macromedia/proom/pr/2005/studio8_ships.html.
- 28.Yabb [February 27, 2009];Yabb 2.0. Available at: http://www.yabbforum.com/.
- 29.The National Institute on Aging and the National Library of Medicine [February 27, 2009];Making your web site senior friendly. Available at: http://www.nlm.nih.gov/pubs/checklist.pdf.
- 30.Nahm E-S, Resnick B. Development and Pilot-Testing of the Web-Based Learning Self-Efficacy Scale (WBLSES) for Older Adults.. Paper presented at: The Gerontological Society of America's 59th Annual Scientific Meeting; Dallas, TX.. 2006. [Google Scholar]
- 31.Gravic Inc. Remark Web Survey Software. Gravic, Inc.; [February 27, 2009]. Available at: http://www.gravic.com/remark/websurvey/. [Google Scholar]
- 32.Kim KK, Horan ML, Gendler P, Patel MK. Development and evaluation of the Osteoporosis Health Belief Scale. Research in Nursing & Health. 1991;14(2):155–163. doi: 10.1002/nur.4770140210. [DOI] [PubMed] [Google Scholar]
- 33.Redman BK. Measurement tools in patient education. 2nd ed. Springer Publishing; New York, NY: 2003. [Google Scholar]
- 34.Horan ML, Kim KK, Gendler P, Froman RD, Patel MD. Development and evaluation of the Osteoporosis Self-Efficacy Scale. Research in Nursing & Health. 1998;21(5):395–403. doi: 10.1002/(sici)1098-240x(199810)21:5<395::aid-nur3>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 35.Wallace LS. Osteoporosis prevention in college women: application of the expanded health belief model. American Journal of Health Behavior. 2002;26(3):163–172. doi: 10.5993/ajhb.26.3.1. [DOI] [PubMed] [Google Scholar]
- 36.Resnick B, Jenkins LS. Testing the reliability and validity of the Self-Efficacy for Exercise scale. Nursing Research. 2000;49(3):154–159. doi: 10.1097/00006199-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Kim KK, Horan M, Gendler P, Patel M. Osteoporosis health belief, self-efficacy, and knowledge test. In: Redman BK, editor. Measurement tools In Patient Education. 2nd ed. Springer; New York, NY: 2003. pp. 364–377. [Google Scholar]
- 38.Resnick B, Zimmerman S, Orwig D, Furstenberg AL, Magaziner J. Model testing for reliability and validity of the Outcome Expectations for Exercise Scale. Nursing Research. 2001;50(5):293–299. doi: 10.1097/00006199-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Resnick B. Testing the effect of the WALC intervention on exercise adherence in older adults. Journal of Gerontological Nursing. 2002;28(6):40–49. doi: 10.3928/0098-9134-20020601-10. [DOI] [PubMed] [Google Scholar]
- 40.Blalock SJ, Norton LL, Patel RA, Cabral K, Thomas CL. Development and assessment of a short instrument for assessing dietary intakes of calcium and vitamin D. Journal of the American Pharmacists Association. 2003;43(6):685–693. doi: 10.1331/154434503322642615. [DOI] [PubMed] [Google Scholar]
- 41.National Cancer Institute [September 3, 2008];Diet History Questionnaire: Current Database File. Available at: http://riskfactor.cancer.gov/DHQ/database/current.html.
- 42.Dipietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Medicine and Science in Sports and Exercise. 1993;25(5):628–642. [PubMed] [Google Scholar]
- 43.Pescatello L, DiPietro L, Fargo A, Ostfeld A, Nadel E. The impact of physical activity and physical fitness on health indicators among older adults. Journal of Aging Physical Activity. 1994;2(1):2–13. [Google Scholar]
- 44.Nahm E-S, Resnick B, Mills ME. Development and pilot-testing of the perceived health Web site usability questionnaire (PHWSUQ) for older adults. Studies in Health Technology and Informatics. 2006;122:38–43. [PubMed] [Google Scholar]
- 45.Nahm ES, Resnick B, Brothemakle B. Use of discussion boards in a social cognitive theory-based hip fracture prevention website for older adults.. Paper presented at: Southern Nursing Research Society; Baltimore, MD.. February 11-14, 2009. [Google Scholar]
- 46.Strauss-Blasche G, Reithofer B, Schobersberger W, Ekmekcioglu C, Marktl W. Effect of vacation on health: moderating factors of vacation outcome. Journal of Travel Medicine. 2005;12:94–101. doi: 10.2310/7060.2005.12206. [DOI] [PubMed] [Google Scholar]