Abstract
The tripartite model of fear posits that the fear response entails three loosely coupled components: subjective distress, behavioral avoidance, and physiological arousal. The concept of synchrony vs. desynchrony describes the degree to which changes in the activation of these components vary together (synchrony), independently, or inversely (both forms of desynchrony) over time. The present study assessed synchronony-desynchrony and its relationship to treatment outcome in a sample of 98 children with specific phobias both prior to and 1 week after receiving one-session treatment, a 3 hour cognitive-behavioral intervention. The results suggest an overall pattern of desynchronous change whereby youth improved on behavioral avoidance and subjective distress following treatment, but their level of cardiovascular reactivity remained stable. However, we found evidence that synchronous change on the behavioral avoidance and subjective distress components was related to better treatment outcome, whereas desynchronous change on these components was related to poorer treatment outcome. These findings suggest that a fuller understanding of the three response systems and their interrelations in phobic youth may assist us in the assessment and treatment of these disorders, potentially leading to a more person-centered approach and eventually to enhanced treatment outcomes.
Keywords: synchrony, desynchrony, tripartite model of fear, specific phobias, children and adolescents, treatment outcome
Lang (1967) describes three components of the fear response: subjective distress, behavioral avoidance, and physiological arousal. Synchronous change on these components following treatment of phobic disorders is hypothesized to predict positive outcomes (Hodgson & Rachman, 1974). Desynchrony occurs when the components fail to change in concert, and is thought to predict poorer treatment outcomes. Research in adults is generally consistent with these hypotheses, although it is uncommon for all three components to be assessed simultaneously (Barlow, Mavissakalian, & Schofield, 1980; Michelson & Mavissakalian, 1985; Michelson, Mavissakalian, & Marchione, 1985; Michelson, Mavissakalian, Marchione, Ulrich, Marchione, & Testa, 1990; Vermilyea, Boice, & Barlow, 1984; Mavissakalian, 1987). Despite its potential clinical utility, it is unclear how synchrony-desynchrony might apply to anxious children, and how it relates to treatment outcome in this population. The current study assesses synchrony-desynchrony across all three components, as well as its relationship to treatment outcome, in a sample of youth with specific phobias treated with a cognitive-behavioral intervention.
Synchrony-Desynchrony of the Tripartite Model of Fear
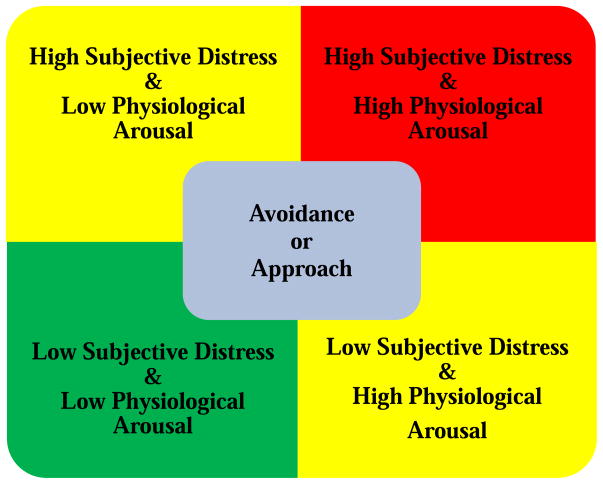
According to Lang’s tripartite model (Lang, 1967, 1979; Lang, Cuthbert, & Bradley, 1998; Lang, Levin, Miller, & Kozak, 1983), fear is comprised of a neural network of three loosely coupled components: subjective distress, behavioral avoidance, and physiological arousal. Although activity in one of these components can activate the remaining components, the extent of “diffusion” is dependent upon the strength of the initiation and the level of fear (Hodgson & Rachman, 1974). In some instances the three components co-vary with one another, and in other instances the components do not respond in concert. In fact, it is possible for any one of the components to be in ascendance while the others lay relatively dormant. An intuitive pattern in the tripartite model is heightened subjective distress, elevated physiological arousal, and avoidance of a feared object or situation; however, others may approach a feared object or situation, even though they experience subjective distress and elevated physiological arousal. All eight combinations of activation of the three components are possible (see Figure 1).
Figure 1.
Possible combinations of activation in the tripartite model of fear.
*Note: Intended for color reproduction on the Web and in black-and-white in print.
Forty years ago, Hodgson and Rachman (1974) described a high correlation among all three components as concordance, and a small correlation among the three components as discordance. Lang and Cuthbert (1984) suggested that concordance among the three response components should be greater in individuals with specific phobias versus other anxiety disorders, since the fear response would likely be heightened in these disorders. While concordance vs. discordance refers to activation patterns in the three components at a single time point, the notion of synchrony vs. desynchrony describes the degree to which changes in the activation of these components vary together (synchrony), independently, or inversely (both forms of desynchrony) over time (Rachman & Hodgson, 1974). For example, treatment of a specific phobia may lead to subsequent changes in all three of the response modalities, or only some of the components while others remain unaffected (Davis & Ollendick, 2005).
The vast majority of research on synchrony-desynchrony has occurred in adults with specific phobias, with more studies showing evidence of desynchrony following treatment (Alpers, Wilhelm, & Roth, 2005; Grey, Sartory, & Rachman, 1979; Hellstrom, Fellenius, & Öst, 1996; Öst, Stridh, & Wolf, 1998; Thomas & Rapp, 1977) than synchrony (Girodo & Henry, 1977; Rentz, Powers, Smits, Cougle, & Telch, 2003). Of note, these studies vary in whether they operationalize synchrony-desynchrony according to changes in only two response systems or all three of the response systems. Studies that incorporate all three components of the fear response consistently demonstrate desynchrony, with the predominant pattern being change in behavioral avoidance and subjective distress, while heart rate remains stable and largely unaffected by treatment (Hellstrom et al., 1996; Öst et al., 1998).
In the child specific phobia literature, the results are more limited. In spider phobic children receiving back-to-back 1.5 hour sessions of in vivo exposure and eye movement desensitization and reprocessing, both distress and avoidance were found to decrease following treatment (Muris, Merkelbach, van Haaften, & Mayer, 1997). Similar synchronous changes in distress and avoidance were found in a large treatment outcome study of children with a range of specific phobias receiving either one-session treatment (OST) or an education support treatment (Blinded for review, 2009). Unfortunately, changes in physiological arousal were not explored in either of these studies. In the only child phobia study to incorporate physiological measures, children with a heterogeneous array of specific phobias were found to decrease from pre- to post-treatment (after receiving either OST alone or OST with a parent present) on avoidance, distress, blood pressure, and heart rate (Öst, Svensson, Hellstrom, & Lindwall, 2001). However, this study did not account for baseline physiological measures, making it impossible to determine if participants responded differently to the phobic stimulus from pre-treatment to-post-treatment, or if their baseline levels of blood pressure and heart rate changed from pre-treatment to post-treatment.
Synchrony-Desynchrony and Treatment Outcome
Hodgson and Rachman (1974) proposed a number of hypotheses with regard to the concept of synchrony-desynchrony, not the least of which was that successful treatment of disorders of fear should involve amelioration, or synchronous change, across all three domains of the tripartite response system. Individuals demonstrating desynchronous change from pre- to post-treatment were proposed to evince inferior treatment outcomes. In the decades following Hodgson and Rachman (1974), researchers have advocated for the collection of data across all three domains of the fear response with the goal of clarifying the link between synchrony-desynchrony and treatment outcome (Davis & Ollendick, 2005; Himaldi, Boice & Barlow, 1985; Michelson, 1984; Silverman & Ollendick, 2005).
Unfortunately, there are no studies to date of synchrony-desynchrony predicting treatment outcome in child phobia samples. In adults, the evidence for and against Hodgson and Rachman’s (1974) hypothesis largely comes from patients with agoraphobia. “Synchronizers” have been found to be less symptomatic than “desynchronizers” at post-treatment, 1 month follow-up, and 3 month follow-up (Michelson & Mavissakalian, 1985; Michelson et al., 1985). Vermilyea et al. (1984) reported a trend for treatment non-response in relation to desynchronous change; however, at 6 month follow-up, the trend disappeared (Craske, Sanderson, & Barlow, 1987). Further, some studies suggest that it is not desynchrony per se, but rather the pattern of desynchrony, that may predict sub-optimal therapeutic outcomes. For example, desynchronous clients with high behavioral avoidance but low heart rate were more likely to be treatment non-responders, whereas subjects with low behavioral avoidance and high heart rate were more likely to be treatment-responders (Mavissakalian, 1987). Finally, the few studies that operationalized synchrony-desynchrony according to all three fear components found evidence that desynchrony was related to poorer outcomes (Michelson et al., 1985; Michelson et al., 1990).
Thus, the adult agoraphobia literature suggests a general relationship between desynchronous change and inferior treatment outcomes (although when only two response systems are assessed, certain patterns of desynchrony might be more pertinent than other patterns). This finding has been replicated in adults with claustrophobia (Alpers & Sell, 2008) and a phobia of flying (Beckham, Vrana, May, Gustafson, & Smith, 1990), with both studies assessing only two indices of the fear response. However, in a case study of two adults with a phobia of heights, Abelson and Curtis (1989) showed continued positive response at 6- and 8-month follow-up, despite both patients showing more change on subjective distress and behavioral avoidance than physiological arousal (measured via heart rate, cortisol, epinephrine and norepinephrine). Given the similar time scale in this and the Craske et al. (1987) paper, it may be that desynchrony is more important in predicting short-term treatment outcome than longer-term follow-up.
Current Study
In summary, the synchrony-desynchrony literature has suffered from a lack of focus on children (particularly as it relates to treatment outcome), and rarely incorporates change in all three components of the tripartite model. The current study aims to address these gaps by assessing synchrony-desychrony among all three components, as well as its relationship to treatment outcome, in a sample of phobic youth treated in two randomized control trials with OST. Davis and Ollendick (2005) note that OST is an intervention uniquely positioned to tackle all three components of the fear response given its incorporation of graduated exposure therapy presented in an intensive format, in vivo exposures, participant modeling, reinforced practice, and direct cognitive challenges through behavioral experiments. However, they also state that while there is evidence suggesting that OST is effective in changing behavioral avoidance and subjective distress, it remains to be examined whether it leads to change in physiological correlates of the fear response. In addition, they acknowledge that the rapid pace of the session could interfere with the time needed for physiological responses to sufficiently habituate. This is similar to the idea put forth by Hodgson and Rachman (1974) that an intervention with high levels of demand will result in desynchronous change because it will take time for subjective distress and/or physiological arousal to catch up with the initial rapid decrease in behavioral avoidance.
Our hypotheses were two-fold. First, based on the literature review showing that desynchronous change is consistently found in adults when all three components of the fear response are assessed (Hellstrom et al., 1996; Öst et al., 1998; Thomas & Rapp, 1977), we predicted desynchronous change from pre- to post-treatment across the whole sample of youth. More specifically, we hypothesized that the physiological arousal component (measured via cardiovascular reactivity) would be the only one to show non-change from pre- to post-treatment, again based on the adult literature, and the review of OST by Davis and Ollendick (2005). Second, based on research with adults, we predicted that a desynchronous pattern of change across all three components would be associated with poorer treatment outcome, while a synchronous pattern of change would be associated with better treatment outcome.
Method
Participants
Children and adolescents (ages 6–15 years) were recruited for two larger phobia treatment outcome studies (Blinded for review, 2009, 2015) through referrals from child mental health services, family medical practices, schools, and newspaper, radio and television advertisements. Study 1 (Blinded for review, 2015) compared standard OST to an education support treatment (EST), while Study 2 (Blinded for review, 2015) compared standard OST to a parent-augmented OST. Inclusion in both studies required participants to meet criteria for a diagnosis of specific phobia, as defined in the DSM-IV-TR (American Psychiatric Association, 2000). As such, the participant had to receive a diagnosis of specific phobia with a clinician severity rating of at least 4 on a 0–8 scale on a semi-structured diagnostic interview (see below). Exclusionary criteria included presence of a pervasive developmental disorder, active suicidal ideation, drug or alcohol abuse, or psychosis. Children with phobias of blood, injection, or injury were also excluded due to their unique physiological profile (see Sarlo, Buodo, Munafo, Palomba, & Stegagno, 2008). Participants were required to discontinue other forms of psychotherapy or medication (anxiolytic or antidepressant) for the duration of their participation in the study.
Children from the larger treatment studies were included in the current study if they received the standard OST and were excluded if they received either EST in Study 1 or parent-augmented OST in Study 2. Specifically, 52 children from Study 1 and 46 children from Study 2 were included. The 98 children included 46 girls (47%) and 52 (53%) boys, with a mean age of 9.07 years (SD = 2.07). Of the youth, 86% were Caucasian, 11% were African American, 2% were Hispanic, and 1% were of other ethnicities. Regarding family structure, 77% of children resided in a two-parent home, 21% resided in a single parent home, and 2% did not report family structure. Mean family income for the combined sample was approximately $81,000 (SD = $71,011, range = $3,000–500,000). Forty (41%) children had animal phobias, including fear of dogs (20), spiders (10), bees (7), snakes (2), and cats (1); 42 (43%) children had natural environment phobias, including fear of the dark/being alone (22), storms (14), heights (3), water (2), and wind (1); and 4 (4%) children had situational phobias, comprised of fear of flying (2), elevators or enclosed spaces (1), and peanuts (1). Finally, 12 (12%) children had phobias that fit into the “other” category, including fear of costumed characters (3), loud noises (4), and other (5).
The reason for referral in all cases was for the treatment of a specific phobia; however, not all participants had a primary specific phobia (i.e., most severe disorder or disorder resulting in the most impairment). Primary diagnoses consisted of specific phobia (79%), generalized anxiety disorder (GAD; 13%), attention-deficit/hyperactivity disorder, combined type (ADHD-C; 7%), and encopresis (1%). The sample was also highly comorbid with 94% having at least one comorbid diagnosis: an additional specific phobia other than the one treated (48%), GAD (20%), social phobia (10%), ADHD-C (3%), separation anxiety disorder (SAD; 3%), obsessive-compulsive disorder (OCD; 3%), enuresis (3%), attention-deficit/hyperactivity disorder, inattentive type (ADHD-I; 2%), post-traumatic stress disorder (PTSD; 1%), and oppositional defiant disorder (ODD; 1%). Finally, 76% of the sample had a tertiary diagnosis: an additional specific phobia (36%), social phobia (15%), GAD (6%), SAD (6%), ODD (5%), ADHD-C (3%), ADHD-I (2%), OCD (2%), and PTSD (1%).
Measures
Anxiety Disorders Interview Schedule for Children (ADIS-C/P; Silverman & Albano, 1996)
The ADIS-C/P is a semi-structured diagnostic interview administered separately to children and parents. It is designed to assess anxiety disorders and other common disorders of childhood (e.g., MDD, ADHD). The ADIS-C/P has demonstrated adequate test-retest reliability for child (ages 7–16, kappas of .61–.80) and parent (kappas of .65–1.00) diagnoses (Silverman, Saavedra, & Pina, 2001). Trained graduate student clinicians conducted the diagnostic interviews for both studies. Following the interview, parent and child clinicians separately assigned clinician severity ratings (CSRs) for each diagnosis on a scale from 0 to 8, with a rating ≥ 4 suggesting a clinical level of impairment, based solely on information obtained during the ADIS interview (i.e., performance on the behavioral approach test described below was not taken into account). All interviews were videotaped: 18 of 90 (20%) from Study 1 and 21 of 83 (25.3%) from Study 2 were coded for reliability. Reliability of parent and child ADIS diagnoses was adequate in both studies (for detailed information, see Blinded for review, 2009 for detailed information, see Blinded for review, 2015). A clinical consensus meeting was then held, led by a licensed clinical psychologist, during which final diagnoses and CSRs were assigned, in order to resolve any discrepancies between parent and child clinician reports. Mean consensus CSR for the treated phobia at pre-treatment was 6.16 (SD = 1.07) on the 0–8 severity scale, reflecting a moderate to severe level of disturbance. Mean consensus CSR dropped to 3.45 (SD = 1.75) at 1 week post-treatment, reflecting subclinical levels of impairment.
Behavioral Approach Test (BAT)
Based largely on BATs designed for children by Öst et al. (2001), BATs were developed for each of the specific phobias in the current study. For most phobia types, the BATs were realistic in that the child was asked to approach a live animal or actual feared object or situation. For example, children with a phobia of dogs were asked to approach and pet a leashed dog on the head for 20 seconds and children fearful of being in the dark were asked to sit alone in a dark room for 5 minutes. The exceptions to this were the BATs for thunderstorms, wind, and flying. For these phobias, children were asked to view videotaped segments of rain, lightning, and thunderstorms (storms); wind and tornadoes (wind); and airplanes (flying) for 5 minutes.
For all BATs, children were escorted to a hallway outside the room in which the BAT was to be administered and were given instructions regarding the task. All children were instructed to do their best but were informed that they could stop the task at any time. The BATs consisted of a series of gradually more difficult steps (ranging from 7 to 12 steps depending on the specific phobia). BATs were ended at the child’s request or when the terminal step was completed. Since some children completed very few steps on the BAT or completed it very rapidly, the actual time in the BAT varied from 30 seconds to 5 minutes. Due to the variability in number of steps on the BATs, percentage of steps completed was used as the measure of behavioral avoidance.
Subjective units of distress ratings
Children were asked to provide ratings of their anxiety utilizing a subjective units of distress scale (SUDS) ranging from 0 to 8 (0 = None, 2 = A Little, 4 = Some, 6 = A Lot, and 8 = Very Much). Ratings were obtained immediately following termination of the BAT, while the child was still in the phobic situation. This was used as the measure of subjective distress.
Interbeat Interval
Prior to the start of the BAT, each child in Study 1 (Blinded for review, 2009) was connected to the Ambulatory Monitoring System v4.4 (AMS; Vrije Universiteit, the Netherlands) to record an electrocardiogram (ECG). Ag-AgCl electrodes were attached to the front torso region according to guidelines set forth in the user manual (Groot, de Geus, & de Vries, 1998). Children in Study 2 (Blinded for review, 2015) each wore a Polar S810i heart rate monitor (Polar HR monitor; Polar Electro Oy, Kempele, Finland). The Polar monitor uses a combined sensor and transmitter that is strapped across the chest with an elastic band. The receiver, which looks like a normal wristwatch, is worn on the non-dominant hand. The sensor detects cardiac electrical impulses and the signal is transmitted to the individual receiver, which calculates the interbeat interval (IBI). The Polar monitor provides results comparable and strongly correlated with an ECG (Gamelin, Berthoin, & Bosquet, 2006). Following connection to the AMS or Polar HR monitor, the child was instructed to sit quietly while watching a 5-minute neutral, non-threatening cartoon video, which allowed for measurement of the child’s baseline cardiac activity. The child then completed the BAT itself.
Our measure of physiological arousal was IBI, an index of cardiovascular reactivity. It was derived from the ECG and Polar HR monitor recordings during baseline and the BATs. IBI is the reciprocal of heart rate, meaning larger IBIs represent slower heart rates. IBI was specifically chosen as the physiological index of arousal because of its relationship with the fear response (Fowles, 1980; Rushen, Passille, & Munksgaard, 1999). Change in IBI from baseline to the completion of the BAT was used as a cardiac chronotropic measure (Berntson, Cacioppo, & Quigley, 1995).
Treatment
Trained graduate student therapists administered OST in both studies, under the supervision of a licensed clinical psychologist. Briefly, OST involved a functional assessment in which the therapist obtained information from the child about precipitating and maintaining factors associated with the specific phobia in order to develop a graduated exposure plan. The child then participated in a 3-hour therapy session in which he or she was gradually exposed to the phobic stimulus (i.e., dogs, costume characters, dark) under controlled conditions. During the session, the therapist assisted the child in challenging anxious cognitions associated with the feared stimulus. Participant modeling and social reinforcement were used throughout the session. Following treatment, the therapist contacted parents weekly for four consecutive weeks to determine how the child was doing; however, no prescribed maintenance program for the child was enacted.
Procedure
As noted, children and parents participated in two larger phobia treatment outcome studies occurring between 2002 and 2012 (Blinded for review, 2009, 2015). As part of the assessment process both prior to and one-week following treatment, children and parents were administered a diagnostic interview and questionnaires, and children participated in the phobia-specific BATs based on information gathered during the interviews.
Institutional Review Board (IRB) approval was acquired for Study 1 and Study 2. Informed consent and assent were obtained from parents and children, respectively. Participants were compensated for their involvement.
Data Analytic Plan
All analyses were conducted using SPSS 22 and the PROCESS macro (Hayes, 2013) was used to probe interactions. Missing values constituted less than 6% of our data, were missing at random (Little’s MCAR test: χ2 = 52.32, df = 49, p = .346), and were estimated using expectation maximization. First, independent-sample t-tests were conducted to compare Study 1 and Study 2 on all variables of interest. There were no significant differences between Study 1 and Study 2 on any measure, and the samples were therefore combined. Second, based on the possibility that developmental level may have an impact on how fear-related symptoms are experienced (Muris, 2005), we examined the relationships between age and all variables of interest. No significant correlations were found and age was therefore not controlled for in any of the analyses.
To test the first hypothesis, pairwise t-tests and Cohen’s Ds were computed to determine if there was significant change from pre- to post-treatment in subjective distress (SUDS), behavioral avoidance (% steps), and cardiovascular reactivity (Δ IBI) during the BAT. Pearson correlations between change scores for each of these tripartite components were then calculated to quantify synchrony (significant correlations) vs. desynchrony (non-significant correlations).
To test the second hypothesis, treatment outcome, quantified as change in CSR from pre- to post-treatment, was regressed onto change in each of the tripartite components, as well as their two-way and three-way interactions. All variables were converted to Z-scores prior to analyses to ensure standardized regression coefficients. These regression models were conducted hierarchically, with the first step of the regression controlling for initial values at pre-treatment, the second step including change scores for each of the tripartite components, and the third and fourth steps including all two-way and three-way interactions, respectively. The significance of the interactions was our formal test of whether synchrony-desynchrony in each pair of the tripartite components (or all three of them, in the case of the three-way interaction) was related to treatment outcome. For example, a significant interaction between change in SUDS and change in % steps would indicate that synchrony-desynchrony between these two components is related to the magnitude of change in CSR following treatment.
Significant interactions were probed using both simple slopes and the Johnson-Neyman technique (Johnson & Neyman, 1936; Preacher, Curran, & Bauer, 2006). For the later, we computed the standardized slope and the 95% confidence intervals for the relationship between change in the focal predictor and change in the outcome variable (CSR) as a function of the moderator variable. This plot allows for the detection of regions of significance (i.e., values of the moderator at which the focal predictor is significantly related to the outcome). The percentage of the sample that fell within this region of significance was also computed.
Results
Our examination of synchrony-desynchrony in the tripartite model of fear began with pairwise t-tests to determine whether subjective distress (SUDS), behavioral avoidance (% steps), and cardiovascular reactivity (Δ IBI) during the BAT significantly changed following treatment (see Table 1). SUDS decreased significantly and % steps increased significantly, but there was no significant change in IBI response during the BAT. The largest effect size was a decrease in SUDS, followed by a modest increase in % steps. A significant reduction in IBI from baseline to BAT was evident at both pre- and post-treatment, but this response was similar in magnitude at both of these time points.
Table 1.
Change in Tripartite Components of Fear from Pre- to Post-treatment
| T1 | T2 | T2 – T1 | t-value | p-value | Cohen’s D | |
|---|---|---|---|---|---|---|
| SUDS | 4.79 (3.00) | 2.38 (2.56) | −2.41 (3.12) | 7.65 | < .001 | −0.86 |
| % Steps | 63.56 (40.08) | 76.06 (32.11) | 12.50 (34.42) | 3.59 | < .001 | 0.34 |
| Δ IBI | −80.21 (68.68) | −81.87 (55.87) | −1.66 (64.62) | −0.26 | .799 | −0.02 |
Note. Standard deviations are shown in parentheses. SUDS = subjective units of distress; % steps = # of steps completed/# steps possible; Δ IBI = change in interbeat interval from baseline to end of BAT; T1 = pre-treatment; T2 = 1 week post-treatment
Next, we conducted our formal test of synchrony-desynchrony by computing change scores for each of the tripartite components and examining each of the three intercorrelations to see if change in one component was related to change in each of the others. Only one of the three intercorrelations was significant, suggesting a predominant pattern of desynchrony among the components. Specifically, a decrease in SUDS following treatment was significantly related to an increase in % steps (r = −.28, p = .005), but change in IBI following treatment was not related to a decrease in SUDS (r =.13, p = .194) or an increase in % steps (r = −.07, p = .508). Since there was no significant change in IBI following treatment, these latter two relationships were not unexpected.
Our last set of analyses addressed the question of whether synchrony-desynchrony in the tripartite model of fear predicted treatment outcome. Change in CSR following treatment (CSR at time 2 – CSR at time 1, so negative values indicate greater change) was regressed onto all main effects, two-way interactions, and the three-way interaction between change in SUDS, % steps, and Δ IBI, while controlling for all values at time 1 (see Table 2). The first step of the regression showed that pretreatment CSR was negatively related to change in CSR following treatment, such that higher initial CSR levels were associated with a more pronounced decrease in CSR following treatment. The second step of the regression included all main effects and showed that change in SUDS following treatment was positively associated with change in CSR following treatment. In addition, the pretreatment SUDS rating from step 1 became significant, indicating that initial levels of subjective distress were positively related to change in CSR, such that higher pretreatment levels of SUDS were associated with a less pronounced decrease in CSR following treatment.
Table 2.
Regression Models of Synchrony-Desynchrony Among Tripartite Components Predicting Treatment Outcome
| Predictors | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | t | p | β | t | p | β | t | P | β | t | p | |
|
|
|
|
|
|||||||||
| CSR T1 | −.23 | −2.15 | .035 | −.33 | −3.28 | .001 | −.38 | −3.84 | <.001 | −.38 | −3.76 | <.001 |
|
|
|
|
|
|||||||||
| SUDS T1 | −.08 | −0.62 | .536 | .45 | 2.88 | .005 | .44 | 2.73 | .008 | .43 | 2.65 | .010 |
|
|
|
|
|
|||||||||
| % Steps T1 | −.13 | −1.08 | .283 | .05 | 0.35 | .724 | .05 | 0.31 | .758 | .04 | 0.25 | .802 |
|
|
|
|
|
|||||||||
| IBI T1 | .12 | 1.07 | .288 | .23 | 1.68 | .096 | .19 | 1.43 | .155 | .20 | 1.47 | .144 |
|
|
|
|
|
|||||||||
| Δ SUDS | - | - | - | .64 | 4.67 | <.001 | .66 | 4.85 | <.001 | .65 | 4.79 | <.001 |
|
|
|
|
|
|||||||||
| Δ % Steps | - | - | - | .07 | 0.55 | .586 | .12 | 0.99 | .327 | .11 | 0.84 | .406 |
|
|
|
|
|
|||||||||
| Δ IBI | - | - | - | .07 | 0.55 | .581 | −.03 | −0.20 | .846 | .00 | −0.01 | .996 |
|
|
|
|
|
|||||||||
| Δ SUDS x Δ Steps | - | - | - | - | - | - | .24 | 2.61 | .011 | .24 | 2.42 | .017 |
|
|
|
|
|
|||||||||
| Δ IBI x Δ SUDS | - | - | - | - | - | - | −.10 | −1.14 | .258 | −.08 | −0.80 | .425 |
|
|
|
|
|
|||||||||
| Δ IBI x Δ Steps | - | - | - | - | - | - | −.18 | −1.84 | .070 | −.14 | −1.07 | .289 |
|
|
|
|
|
|||||||||
| Δ SUDS x IBI x Δ Steps | - | - | - | - | - | - | - | - | - | .04 | 0.37 | .711 |
Note. T1 = pre-treatment; CSR = clinician severity rating; treatment outcome = CSR at post-treatment – CSR at pre-treatment; SUDS = subjective units of distress; % steps = # of steps completed/# steps possible; IBI = change in interbeat interval from baseline to end of BAT; Δ SUDS = SUDS post – SUDS pre-treatment; Δ % Steps = % Steps post – % Steps pre-treatment; Δ IBI = IBI pre – Δ IBI post-treatment
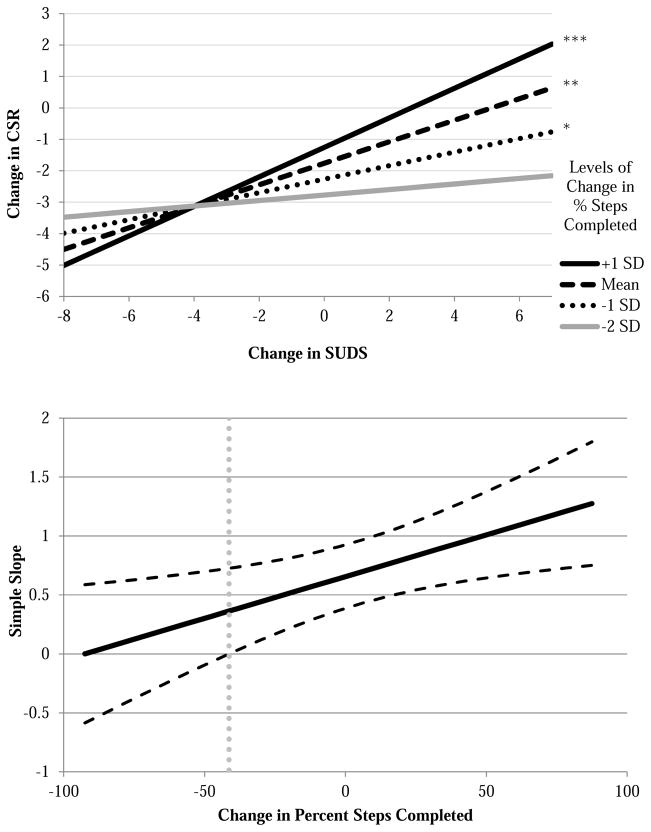
The third regression model included all two-way interactions, which tested whether synchrony-desynchrony in each pair of the tripartite components was related to treatment outcome. The interaction between change in SUDS and change in % steps was the only tripartite pair that significantly predicted change in CSR following treatment. The fourth regression model included the three-way interaction among all tripartite components, which was not significant. In post-hoc probing of the significant two-way interaction, we first set change in SUDS as the predictor and change in % steps as the moderator because the former was directly related to change in CSR . Post-hoc probing of the simple slopes showed that as % steps completed increased, the relationship between change in SUDS and change in CSR became stronger (see top of Figure 2). In other words, synchronous change in SUDS (a decrease) and % steps (an increase) was associated with positive treatment outcome (a decrease in CSR). Conversely, desynchronous change in these components (i.e.., an increase in % steps coupled with an increase in distress) was related to worse treatment outcome. The Johnson-Neyman technique was used to plot the regions of significance (see bottom of Figure 2). It shows that the standardized simple slope of the relationship between change in SUDS and change in CSR was significant at all values above a change in % steps of −41%, which constituted roughly 96% of the sample (see Figure 2). It was only for the small minority of youth who had a very large decrease in % steps that change in SUDS did not relate to treatment outcome.
Figure 2.
Simple slope plots (top) and regions of significance (bottom) for the relationship between change in subjective distress and treatment outcome at various levels of change in percentage of steps completed during the behavioral approach test. The top figure shows the simple slopes for the relationship between change in SUDS (subjective units of distress) and treatment outcome (change in CSR or clinical severity rating) plotted at various standard deviations above and below the mean change in % steps completed. Note: * = p < .05; ** = p < .01; *** = p < .001; SD = standard deviation. The bottom figure shows the standardized simple slope on the y-axis for the relationship between change in SUDS and change in CSR following treatment, plotted against all possible values of change in % steps completed on the x-axis. The black dashed lines represent the upper and lower limit of the 95% confidence intervals surrounding the simple slopes (solid black line) at each level of the moderator, change in % steps. The vertical gray dotted line represents the value of change in % steps at which the lower limit of the confidence interval crosses the zero point and the relationship between change in SUDS and change in CSR becomes significant.
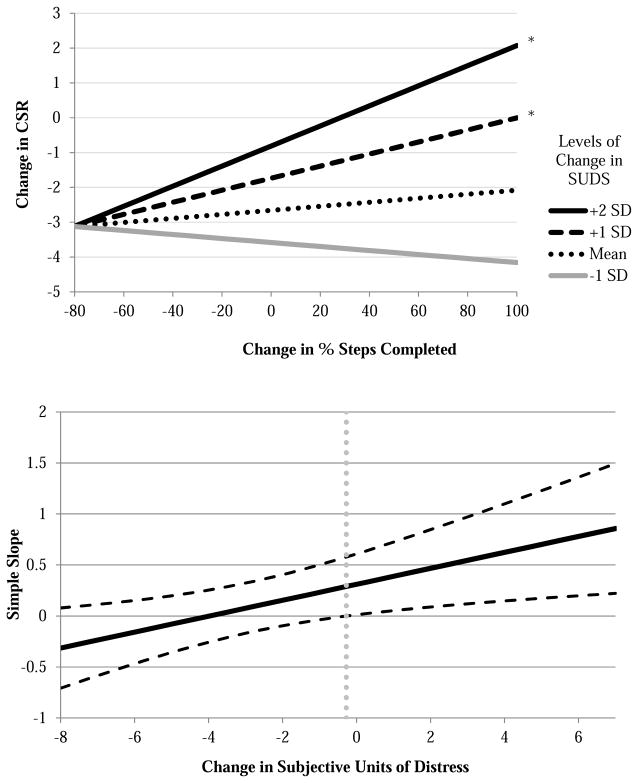
Next, we probed this interaction by setting change in % steps as the predictor and change in SUDS as the moderator. While % steps was not a significant predictor of treatment outcome in the second model, this analysis tested whether % steps was significantly associated with treatment outcome in a subgroup of participants with a certain level of change in SUDS. Post-hoc probing of the simple slopes showed that as SUDS increased following treatment, the relationship between change in % steps and change in CSR became significant (see top of Figure 3). In other words, similar to what is depicted in Figure 2, desynchronous change in SUDS and % steps (an increase in both) was associated with negative treatment outcome (relative increases in CSR). The Johnson-Neyman technique was used to plot the regions of significance (see bottom of Figure 3). It shows that the standardized simple slope of the relationship between change in % steps and change in CSR was significant at all values above a change in SUDS of roughly 0, which constituted approximately 30% of the sample. For the majority of the youth, who decreased in SUDS following treatment, there was no relationship between change in % steps and treatment outcome.
Figure 3.
Simple slope plots (top) and regions of significance (bottom) for the relationship between change in percentage of steps completed and treatment outcome at various levels of change in subjective distress during the behavioral approach test. The top figure shows the simple slopes for the relationship between change in % steps completed and treatment outcome (change in CSR or clinical severity rating) plotted at various standard deviations above and below the mean change in SUDS (subjective units of distress). Note: * = p < .05; SD = standard deviation. The bottom figure shows the standardized simple slope on the y-axis for the relationship between change in % steps completed and change in CSR following treatment, plotted against all possible values of change in SUDS on the x-axis. The black dashed lines represent the upper and lower limit of the 95% confidence intervals surrounding the simple slopes (solid black line) at each level of the moderator, change in SUDS. The vertical gray dotted line represents the value of change in SUDS at which the lower limit of the confidence interval crosses the zero point and the relationship between change in % steps completed and change in CSR becomes significant.
Discussion
Desynchronous Change Following OST
Despite debuting 40 years ago, the field still knows relatively little about how the concept of synchrony-desynchrony applies to clinically phobic youth, or how it relates to treatment outcome in this group. The results of the current study clearly demonstrate desynchronous change from pre- to post-treatment for phobic children treated with OST, lending support to our first hypothesis. More specifically, while these youth were less avoidant and less distressed when confronting their feared stimulus during the BAT at post-treatment, their cardiovascular reaction was consistent in magnitude with pre-treatment levels. Further, change in subjective distress was significantly correlated with change in behavioral avoidance, but neither was related to change in cardiovascular reactivity.
Our finding of overall desynchronous change is consistent with studies in the adult phobia literature that have assessed all three components of the fear response, which also found evidence of desynchronous change from pre- to post-treatment, specifically with heart rate remaining stable (Hellstrom et al., 1996; Öst et al., 1998). Our study replicates these findings in a population of phobic youth, and by taking into account baseline levels of cardiovascular reactivity, overcomes an important limitation in the only other study to assess synchrony-desynchrony in phobic youth on all three components of the fear response (Öst et al., 2001).
Why might phobic children improve on subjective distress and behavioral avoidance, but have consistent cardiovascular reactions when confronting phobic stimuli following OST treatment? First, it could be that the rapid pace of the 3-hour treatment is incompatible with the time needed for cardiovascular responses to sufficiently habituate (Davis & Ollendick, 2005). This is consistent with the assertion of Hodgson and Rachman (1974) that interventions with high levels of demand may result in desynchronous change because it will take time for physiological arousal to “catch up” with an initial rapid decrease in behavioral avoidance. Therefore, we might see evidence of more synchronous change if we looked at the results of a BAT administered at longer-term follow-up. This is in line with findings from adult agoraphobics, for whom there was a greater tendency for desynchrony in the earlier phases of treatment, with a shift to more synchronous change in the later phases (Mavissakalian & Michelson, 1982). On the other hand, because activity in one component can activate the others (Hodgson & Rachman, 1974), persistent physiological arousal could potentially reverse the effects of an intervention over time. In other words, continued activation of this component of the fear response may leave phobic individuals vulnerable to relapse. Studies investigating longer-term outcomes are needed to parse out these possibilities.
Second, it is possible that our demonstrated lack of change in cardiovascular reactivity is due to OST explicitly targeting the subjective and behavioral components of fear, but only implicitly targeting physiology. That is, in OST the therapist carefully assesses the child’s behavioral avoidance (e.g., watches for subtle signs of avoidance and escape) and subjective distress (e.g., asks for SUDS ratings) throughout the session in order to determine when and how to move the exposure forward. He/she does not, on the other hand, directly assess the child’s heart rate before deciding on the next step in the graduated exposure. Therefore, it may be that children are moving on to more difficult exposures before having physiologically habituated to the prior step. Future studies that incorporate real-time physiological data into OST would shed more light on this possibility.
The Relationship Between Synchrony-Desynchrony and Treatment Outcome
A particularly unique contribution of the current study was the investigation of the link between synchrony-desynchrony and treatment outcome in a child phobia sample, the first to our knowledge to do so. Inconsistent with our second hypothesis, we did not find evidence that synchrony-desynchrony on all three components was related to treatment outcome. However, we found that less positive treatment outcome among phobic youth was associated with desynchronous change between the subjective distress and behavioral avoidance components of the tripartite model of fear, whereas synchronous change on these two components was related to improved treatment outcome. These relationships are captured most succinctly in the top portion of Figure 2. The solid line depicts the children who improved the most on % steps (i.e., behavioral avoidance). They also demonstrated the strongest relationship between change in SUDS (i.e., subjective distress) and change in CSR (i.e., treatment outcome). This means that a large decrease in SUDS was coupled with a large decrease in CSR, whereas a relatively smaller decrease (or increase) in SUDS was coupled with a relatively smaller decrease (or increase) in CSR. Children fitting the first profile are clearly “synchronizers:” they improved the most on both behavioral avoidance and subjective distress and had the best treatment outcomes. Children in the latter group would be “desynchronizers:” they also improved on behavioral avoidance, but showed relatively less improvement on subjective distress and had relatively poorer treatment outcomes. The “desynchronizers” are depicted more vividly in Figure 3. For youth who stayed the same or increased in subjective distress following treatment, the more they improved on approach behavior, the worse their outcomes were. It should be noted that 96% of the current sample fit these descriptions. It is only for the 4% of children who had a decrease in % steps of more than 41% that there was no relationship between change in SUDS and change in CSR. Therefore, it is for a very small minority of children that synchrony-desynchrony does not predict treatment outcome.
Why might our study have failed to find support for the hypothesis proposed by Hodgson and Rachman (1974) and echoed by Davis and Ollendick (2005) that successful treatment should involve synchronous change across all three domains of the tripartite response system? In other words, in our sample, why was it that cardiovascular reactivity did not have to change in order for treatment to be successful? It may be that this particular pattern of desynchrony can be explained by the effects of emotion regulation (Cisler et al., 2010). Although children did not change on cardiovascular reactivity from pre- to post-treatment, they may have learned to reappraise physical sensations in a way that was less-threatening (i.e., the treatment taught them that they could successfully cope with the feeling of an increased heart rate when approaching the feared object/situation). This idea was stated early on by Hodgson and Rachman (1974), who asserted that one’s emotional state is the result of both the predominant physiological environment and one’s cognitive appraisal of it. Therefore, desynchrony will be evident if the same physiological state is interpreted differently at two points in time. Future work in this area should include assessment of the use of reappraisal in order to determine the role that this type of emotion regulation strategy might play in the relationship between synchrony-desynchrony and treatment outcome.
Our finding that it is only synchrony-desynchrony between the behavioral avoidance and subjective distress components that predicts treatment outcome has not been previously reported; however, it is broadly consistent with the idea that the pattern of desynchrony may be more important than the presence of desynchrony in the prediction of suboptimal treatment outcomes (Mavissakalian, 1987). In our sample, children who improved the most following OST were those who had the greatest decreases in both subjective distress and behavioral avoidance. It appears that for children, as opposed to adults, these two components are the ones most explicitly tied to improvement following treatment. It could also be that this finding is a direct consequence of the result that overall cardiovascular reactivity did not change in magnitude from pre- to post-treatment, and therefore could not be related to treatment outcome in the current sample. Alternatively, this result could be due to potential overlap between the BAT and CSR. That is, they are both influenced by report of subjective distress and behavioral avoidance. On the other hand, there is evidence that these constructs are fairly independent. Child and parent clinicians assigned CSR ratings completely independent of child’s performance on the BAT, and the BAT was based solely on child report of distress and behavior, whereas the final CSR incorporated both child and parent report. More importantly, additional analyses showed that neither distress nor avoidance on the BAT were correlated with CSR at time 1, and only distress was moderately correlated with CSR at time 2 (r = .43).
Our study is also the first to find that poor treatment outcome in phobic youth is associated with an increase in approach behavior coupled with an increase in distress. This finding is somewhat counter-intuitive, as one would predict that youth who push themselves to be brave despite their distress will do well in a CBT. This may again be an issue of the timing of the second BAT assessment. We propose that while children who increase in approach behavior without simultaneous habituation of distress show concurrent increases in fear, this pattern may lead to improved outcomes over time.
A Person-centered Approach to Assessment and the Evaluation of Treatment Outcome
More generally, the results of our study remind us that Lang (1985) described the three response systems as “loosely coupled” and noted that they may not all be equally activated when an individual is confronted with a phobic stimulus (i.e., discordance). Indeed, not all components of the tripartite model of fear are equally relevant for all phobic individuals (Bergman & Piacentini, 2005) and there may be marked differences in the manifestation of the response systems among various types of specific phobias, as well as individual differences within phobias (Muris, 2005). Of course, if any one system is not activated in the phobic response at pre-treatment, it is impossible for it to ameliorate with treatment. This suggests that concordance-discordance of the three response systems is complexly related to synchrony-desynchrony following treatment, which raises two related questions: 1) how do we define activation in each of the three systems at pre-treatment? And 2) should we alter our definition of synchrony-desynchrony when one or more systems are not activated at pre-treatment, and if so, how? Regarding the former, there are currently no guidelines available for determining how much subjective distress, behavioral avoidance, or physiological arousal must be present in order to indicate that all components of the fear response have been activated. No normative data exist for these systems (see Ollendick, Allen, Benoit, & Cowart, 2011). As a result, in our study, we were simply left with defining any change from pre- to post-treatment as change, and we have no evidence that this change was clinically meaningful or significant (Jacobson & Truax, 1991). Future research will need to establish such parameters before we can explore this notion further.
Regarding the second issue, however activation is defined, we suggest that if any component(s) is not activated at pre-treatment, amelioration of that component is not possible and therefore our definition of synchrony-desynchrony should be altered. For example, if a child reports very low distress, yet exhibits an increase in heart rate and is unable to approach the phobic stimuli, only behavioral avoidance and cardiovascular reactivity would be expected to show synchronous change following treatment. This issue suggests that we need to move to an individualized, person-centered approach to assessment and the evaluation of treatment outcome (see McLeod, Jensen-Doss, & Ollendick, 2013). That is, although desirable to measure all three response systems in assessing the phobic response, only those systems found to be activated (however that is defined) would be used to determine whether synchronous change has occurred following treatment. Furthermore, differences in activation might also be used to tailor the treatment to the individual profile of responding such that treatments would directly address the response systems activated in each individual. Support for this notion was shown by Öst and colleagues (Öst, Jerremalm, & Johansson, 1981; Öst, Johansson, & Jerremalm, 1982), who demonstrated that individuals with phobias who showed relatively greater behavioral avoidance than heart rate reactivity responded better to exposure therapy whereas those individuals showing relatively greater heart rate reactivity did better with applied relaxation techniques. In a somewhat similar vein, Silverman and Kearney (1992) have demonstrated differential treatment effects based on the assessment profile of both phobic and anxious children (what they referred to as “prescriptive treatment”). Of course, not all studies have supported this person-centered assessment approach and whether treatments “matched” to the assessment profile really produce better treatment outcomes awaits systematic inquiry via randomized control studies. However, in the least, our findings of overall desynchronous change and a relationship between synchrony-desynchrony and treatment outcome in phobic youth illustrate the need for more research as to how we define activation of the tripartite components and how we should examine synchrony-desynchrony following treatment.
Limitations
First, there may be disadvantages associated with the BAT as a measure of the phobic response. Although it is a measure that is uniquely capable of simultaneously eliciting the three components of the phobic response under controlled laboratory conditions (Dadds, Rapee, & Barrett, 1994), whether the BAT captures the phobic response as it would be represented in more naturalistic situations remains to be seen (Ollendick et al., 2011). That is, the degree of threat may not be as potent as it would be in naturalistic situations, thus the threat may not be as high as it needs to be in order to produce synchrony over time. There was also considerable variability in the BATs used for the various phobias treated in the current study. For example, the BATs for storms, wind, and flying were not “in vivo,” and therefore may not have activated the fear response as well the BATs that entailed directly confronting the phobic stimuli/situation. Second, we only assessed synchrony-desynchrony in relation to pre-treatment and 1 week post-treatment. Future studies should assess these constructs at longer-term follow-up, especially in light of the hypothesis that it might take time for the other indices to “catch up” with change in behavioral avoidance (Hodgson & Rachman, 1974; Muris, 2005). Further, more than two time points would enable the investigation of a second index of change, which would contribute to a more complete understanding of synchrony-desynchrony in the tripartite model. Third, our study lacks a control group of waitlist children (who would have undergone the same procedures minus the intervention), which limits our ability to parse the effect of time on change in fear indices. Fourth, the phobic youth in our sample were highly comorbid with other disorders and it is unclear what effect this may have had on the fear components of interest. Last, our sample was referred to a specialty clinic, largely Caucasian, medium to high in family income, and from largely intact families. As a result, it is unclear whether our findings related to synchrony-desynchrony would generalize to youth presenting in non-specialty clinics or in community samples, or youth from other ethnicities or family backgrounds.
Conclusion
Despite these limitations, our study used a well-characterized sample of clinically phobic youth, employed a methodologically sound measure of the tripartite model of fear, and used a continuous approach to investigate change in the tripartite model of fear over time (as opposed to using artificial dichotomization to define “synchronizers” and “desynchronizers”). Our findings suggest that desynchrony is common in the early treatment outcome of clinically phobic youth, and that cardiovascular reactivity, in particular, may be resistant to change following treatment with OST. Further, we provide initial evidence that synchronous or desynchronous change in behavioral avoidance and subjective distress may be particularly important in predicting treatment outcome for these youth. These findings are of importance for treatment-seeking youth with specific phobias and they begin to lay the foundation for addressing the issue of synchrony-desynchrony more fully. Our findings suggest that a fuller understanding of the three response systems and their interrelations in youth with specific phobias will be necessary to assist us in the assessment and treatment of these disorders. We believe that such an understanding will lead to a more person-centered approach to assessment and eventually to enhanced treatment outcomes.
Highlights.
Synchrony is when avoidance, distress, and physiological arousal decrease over time.
We examine synchrony in clinically phobic youth following one-session treatment.
Avoidance and distress decreased while cardiovascular reactivity remained stable.
Synchronous change in avoidance and distress was related to better outcomes.
This is the first study to relate synchrony to treatment outcome in phobic youth.
Acknowledgments
Dr. Benoit Allen is supported by an Institutional National Research Service Award from NIMH (MH18269). Funds for the two 5-year projects were provided by R01 MH51308 and R01 MH07477 from the National Institute of Mental Health. Joel Sherrill, Chief of the Psychosocial Treatment Research Program, served as Program Officer. We are grateful for Dr. Sherrill’s guidance and NIMH’s support. We wish to express appreciation to the graduate clinicians and postdoctoral fellows who served as project coordinators, assessors, and/or therapists on these projects over the years. In addition, we extend thanks to the many undergraduate students at Virginia Tech who assisted with data coding, entry, and verification and, in particular, those who helped to manage the projects on a day-to-day basis. Finally, we are grateful to the youth and families who participated in these clinical research trials.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abelson JL, Curtis GC. Cardiac and neuroendocrine responses to exposure therapy in height phobics: Desynchrony within the ‘physiological response system’. Behaviour Research and Therapy. 1989;27:561–567. doi: 10.1016/0005-7967(89)90091-0. [DOI] [PubMed] [Google Scholar]
- Alpers GW, Sell R. And yet they correlate: Psychophysiological activation predicts self-report outcomes of exposure therapy in claustrophobia. Journal of Anxiety Disorders. 2008;22:1101–1109. doi: 10.1016/j.janxdis.2007.11.009. [DOI] [PubMed] [Google Scholar]
- Alpers GW, Wilhelm FH, Roth WT. Psychophysiological assessment during exposure in driving phobic patients. Journal of Abnormal Psychology. 2005;114:126–129. doi: 10.1037/0021-843X.114.1.126. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Beckham JC, Vrana SR, May JG, Gustafson DJ, Smith GR. Emotional processing and fear measurement synchrony as indicators of treatment outcome in fear of flying. Journal of Behavior Therapy and Experimental Psychiatry. 1990;21:153–162. doi: 10.1016/0005-7916(90)90002-3. [DOI] [PubMed] [Google Scholar]
- Bergman RL, Piacentini J. Targeting discrete response channels in the treatment of childhood specific phobia. Clinical Psychology: Science and Practice. 2005;12:166–169. [Google Scholar]
- Berntson GG, Cacioppo JT, Quigley KS. The metrics of cardiac chronotropism: Biometric perspectives. Psychophysiology. 1995;32(2):162–171. doi: 10.1111/j.1469-8986.1995.tb03308.x. [DOI] [PubMed] [Google Scholar]
- Blinded for review. 2015 [Google Scholar]
- Blinded for review. 2009 [Google Scholar]
- Cisler JM, Olatunji BO, Feldner MT, Forsyth JP. Emotion regulation and the anxiety disorders: An integrative review. Journal of Psychopathology and Behavioral Assessment. 2010;32:68–82. doi: 10.1007/s10862-009-9161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Sanderson WC, Barlow DH. How do desynchronous response systems relate to the treatment of agoraphobia: A follow-up evaluation. Behaviour Research and Therapy. 1987;25:117–122. doi: 10.1016/0005-7967(87)90082-9. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Rapee RM, Barrett PM. Behavioral observations. In: Ollendick TH, King NJ, Yule W, editors. International handbook of phobic and anxiety disorders in children and adolescents. New York, NY: Plenum Press; 1994. pp. 349–364. [Google Scholar]
- Davis TE, III, Ollendick TH. A critical review of empirically supported treatments for specific phobias in children: Do efficacious treatments address the components of a phobic response? Clinical Psychology: Science and Practice. 2005;12:144–160. [Google Scholar]
- Fowles DC. The three arousal model: Implications of Gray’s two-factor learning theory for heart rate, electrodermal activity, and psychopathy. Psychophysiology. 1980;17:87–104. doi: 10.1111/j.1469-8986.1980.tb00117.x. [DOI] [PubMed] [Google Scholar]
- Gamelin FX, Berthoin S, Bosquet L. Validity of the polar S810 heart rate monitor to measure R-R intervals at rest. Medicine & Science in Sports & Exercise. 2006;38:887–893. doi: 10.1249/01.mss.0000218135.79476.9c. [DOI] [PubMed] [Google Scholar]
- Girodo M, Henry DR. Cognitive, physiological and behavioural components of anxiety in flooding. Canadian Journal of Behavioural Science. 1976;8:224–231. [Google Scholar]
- Grey S, Sartory G, Rachman S. Synchronous and desynchronous changes during fear reduction. Behaviour Research and Therapy. 1979;17:137–147. doi: 10.1016/0005-7967(79)90022-6. [DOI] [PubMed] [Google Scholar]
- Groot PFC, de Geus EJC, de Vries J. Ambulatory monitoring system. User manual v1.2. Amsterdam, The Netherlands: Vrije Universiteit, Department of Psychophysiology; 1998. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guildford Press; 2013. [Google Scholar]
- Hellstrom K, Fellenius J, Öst LG. One versus five sessions of applied tension in the treatment of blood phobia. Behaviour Research and Therapy. 1996;34:101–112. doi: 10.1016/0005-7967(95)00060-7. [DOI] [PubMed] [Google Scholar]
- Himadi WG, Boice R, Barlow DH. Assessment of agoraphobia: Triple response measurement. Behaviour Research and Therapy. 1985;23:311–323. doi: 10.1016/0005-7967(85)90010-5. [DOI] [PubMed] [Google Scholar]
- Hodgson R, Rachman S. II. Desynchrony in measures of fear. Behaviour Research & Therapy. 1974;12:319–326. doi: 10.1016/0005-7967(74)90006-0. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johnson PO, Neyman J. Tests of certain linear hypotheses and their application to some educational problems. Statistical Research Memoirs. 1936;1:57–93. [Google Scholar]
- Lang PJ. Fear reduction and fear behavior: Problems in treating a construct. In: Shlien JM, editor. Research in psychotherapy. Washington, DC: American Psychological Association; 1967. pp. 332–368. [Google Scholar]
- Lang PJ. A bio-informational theory of emotional imagery. Psychophysiology. 1979;16:495–512. doi: 10.1111/j.1469-8986.1979.tb01511.x. [DOI] [PubMed] [Google Scholar]
- Lang PJ. The cognitive psychophysiology of emotion: Fear and anxiety. In: Tuma AH, Maser JD, editors. Anxiety and the anxiety disorders. Hillsdale, NJ: Lawrence Erlbaum Associates; 1985. pp. 131–170. [Google Scholar]
- Lang PJ, Cuthbert BN. Affective information processing and the assessment of anxiety. Journal of Behavioral Assessment. 1984;6:369–395. doi: 10.1007/BF01321326. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Cuthbert BN, Bradley MM. Measuring emotions in therapy: Imagery, activation, and feeling. Behavior Therapy. 1998;29:655–674. [Google Scholar]
- Lang PJ, Levin DN, Miller GA, Kozak MJ. Fear behavior, fear imagery, and the psychophysiology of emotion: The problem of affective response regulation. Journal of Abnormal Psychology. 1983;92:276–306. doi: 10.1037//0021-843x.92.3.276. [DOI] [PubMed] [Google Scholar]
- Mavissakalian M. Trimodal assessment in agoraphobia research: Further observations on heart rate and synchrony/desynchrony. Journal of Psychopathology and Behavioral Assessment. 1987;9:89–98. [Google Scholar]
- Mavissakalian M, Michelson L. Patterns of psychophysiological change in the treatment of agoraphobia. Behaviour Research and Therapy. 1982;20:347–356. doi: 10.1016/0005-7967(82)90094-8. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Jensen-Doss A, Ollendick TH, editors. Diagnostic and behavioral assessment in children and adolescents: A clinical guide. New York, NY: Guilford Press; 2013. [Google Scholar]
- Michelson L. The role of individual differences, response profiles, and treatment consonance in anxiety disorders. Journal of Behavioral Assessment. 1984;6:349–367. [Google Scholar]
- Michelson L, Mavissakalian M. Psychophysiological outcome of behavioral and pharmacological treatments of agoraphobia. Journal of Consulting and Clinical Psychology. 1985;53:229–236. doi: 10.1037//0022-006x.53.2.229. [DOI] [PubMed] [Google Scholar]
- Michelson L, Mavissakalian M, Marchione K. Cognitive and behavioral treatments of agoraphobia: Clinical, behavioral, and psychophysiological outcomes. Journal of Consulting and Clinical Psychology. 1985;53:913–925. doi: 10.1037//0022-006x.53.6.913. [DOI] [PubMed] [Google Scholar]
- Michelson L, Mavissakalian M, Marchione K, Ulrich RF, Marchione N, Testa S. Psychophysiological outcome of cognitive, behavioral and psychophysiologically-based treatments of agoraphobia. Behaviour Research and Therapy. 1990;28:127–139. doi: 10.1016/0005-7967(90)90025-e. [DOI] [PubMed] [Google Scholar]
- Muris P. Treatment of specific phobia in children: Are all the components of the phobic response of equal importance? Clinical Psychology: Science and Practice. 2005;12:170–173. [Google Scholar]
- Muris P, Merckelbach H, Van Haaften H, Mayer B. Eye movement desensitisation and reprocessing versus exposure in vivo. A single-session crossover study of spider-phobic children. The British Journal of Psychiatry. 1997;171:82–86. doi: 10.1192/bjp.171.1.82. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Allen B, Benoit K, Cowart MJ. The tripartite model of fear in children with specific phobias: Assessing concordance and discordance using the Behavioral Approach Test. Behaviour Research and Therapy. 2011;49:459–465. doi: 10.1016/j.brat.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öst L-G, Jerremalm J, Johansson J. Individual response patterns and the effects of different behavioral methods in the treatment of social phobia. Behaviour Research and Therapy. 1981;19:1–16. doi: 10.1016/0005-7967(81)90107-8. [DOI] [PubMed] [Google Scholar]
- Öst L-G, Johansson J, Jerremalm J. Individual response patterns and the effects of different behavioral methods in the treatment of agoraphobia. Behaviour Research and Therapy. 1982;20:445–460. doi: 10.1016/0005-7967(82)90066-3. [DOI] [PubMed] [Google Scholar]
- Öst LG, Stridh BM, Wolf M. A clinical study of spider phobia: Prediction of outcome after self-help and therapist-directed treatments. Behaviour Research and Therapy. 1998;36:17–35. doi: 10.1016/s0005-7967(97)10018-3. [DOI] [PubMed] [Google Scholar]
- Öst LG, Svensson L, Hellstrom K, Lindwall R. One-session treatment of specific phobias in youths: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2001;69:814–824. [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Rachman S, Hodgson R. I. Synchrony and desynchrony in fear and avoidance. Behaviour Research & Therapy. 1974;12:311–318. doi: 10.1016/0005-7967(74)90005-9. [DOI] [PubMed] [Google Scholar]
- Rentz TO, Powers MB, Smits JA, Cougle JR, Telch MJ. Active-imaginal exposure: Examination of a new behavioral treatment for cynophobia (dog phobia) Behaviour Research and Therapy. 2003;41:1337–1353. doi: 10.1016/s0005-7967(03)00041-x. [DOI] [PubMed] [Google Scholar]
- Rushen J, Passillé AMB, Munksgaard L. Fear of people by cows and effects on milk yield, behavior, and heart rate at milking. Journal of Dairy Science. 1999;82:720–727. doi: 10.3168/jds.S0022-0302(99)75289-6. [DOI] [PubMed] [Google Scholar]
- Sarlo M, Buodo G, Munafo M, Palomba D, Stegagno L. Cardiovascular dynamics in blood phobia: Evidence for a key role of sympathetic activity in vulnerability to syncope. Psychophysiology. 2008;45:1038–1045. doi: 10.1111/j.1469-8986.2008.00713.x. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety disorders interview schedule for DSM-IV: Child and parent versions. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Kearney CA. Listening to our clinical partners: Informing researchers about children’s fears and phobias. Journal of Behavior Therapy and Experimental Psychiatry. 1992;23:71–76. doi: 10.1016/0005-7916(92)90003-2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Thomas MR, Rapp MS. Physiological, behavioural and cognitive changes resulting from flooding in a monosymptomatic phobia. Behaviour Research and Therapy. 1977;15:304–306. doi: 10.1016/0005-7967(77)90027-4. [DOI] [PubMed] [Google Scholar]
- Vermilyea JA, Boice R, Barlow DH. Rachman and Hodgson (1974) a decade later: How do desynchronous response systems relate to the treatment of agoraphobia? Behaviour Research and Therapy. 1984;22:615–621. doi: 10.1016/0005-7967(84)90124-4. [DOI] [PubMed] [Google Scholar]