Abstract
Objective
To examine whether an off-axis elliptical training program reduces pain and improves knee function in individuals with patellofemoral pain (PFP).
Design
Controlled laboratory study, pre-test-post-test.
Setting
University rehabilitation center.
Participants
Twelve adult subjects with PFP.
Interventions
Subjects with PFP completed an exercise program consisting of 18 sessions of lower extremity off-axis training using a custom-made elliptical trainer that allows frontal-plane sliding and transverse-plane pivoting of the footplates.
Main Outcome Measures
Changes in knee pain and function post-training and 6 weeks following training were evaluated using the Knee Injury and Osteoarthritis Outcome Score (KOOS) and International Knee Documentation Committee (IKDC) scores. Lower extremity off-axis control was assessed by pivoting and sliding instability, calculated as the root mean square (RMS) of the footplate pivoting angle and sliding distance during elliptical exercise. Subjects’ single-leg hop distance and proprioception in detecting lower extremity pivoting motion were also evaluated.
Results
Subjects reported significantly greater KOOS and IKDC scores (increased by 12–18 points) and hop distance (increased by 0.2 m) following training. A significant decrease in the pivoting and sliding RMS was also observed following training. Additionally, subjects with PFP demonstrated improved pivoting proprioception when tested under a minimum-weight-bearing position.
Conclusions
An off-axis elliptical training program was effective in enhancing lower extremity neuromuscular control on the frontal and transverse planes, reducing pain and improving knee function in persons with PFP.
Keywords: Rehabilitation, Knee, Lower Extremity, Kinematics
INTRODUCTION
Patellofemoral pain (PFP) is characterized by retropatellar and/or peripatellar pain that is often exacerbated by activities involving prolonged running, squatting, stair climbing, sitting, or kneeling.1,2 A wide range of individuals are affected by PFP, especially females and those who are physically active.3–5 Despite the high incidence, the underlying etiologic factors of PFP have not been fully understood.6,7
One of the most common proposed mechanisms for developing PFP is the maltracking/malalignment of the patellofemoral joint (e.g., lateral displacement and/or lateral tilt of the patella relative to the femoral groove).6,8,9 Patellofemoral maltracking may increase joint stress and lead to subsequent cartilage wear, which would likely irritate pain receptors within the joint.6,10 As such, many interventions focus on correcting patellofemoral pathomechanics.1
Patellofemoral maltracking has been associated with altered frontal and/or transverse-plane kinematics (i.e., off-axis movements) of the lower extremity, such as increased rearfoot eversion, knee valgus, hip adduction and internal rotation.6,11–14 Intervention strategies, including hip muscle strengthening and foot orthoses, have been used for treating PFP in an effort to better control these lower extremity off-axis motions.15–18 Although these interventions have been shown to be somewhat effective,15,16,18 few interventions are currently available to monitor and/or improve the neuromuscular control of the lower extremities to reduce the off-axis movements in functional weight-bearing activities during which PFP occurs.
A robotic off-axis elliptical trainer has been developed to provide neuromuscular training of the lower extremities under a functional weight-bearing elliptical stepping exercise.19–22 Considering that PFP is commonly associated with altered off-axis lower extremity kinematics and loading, an intervention that aims to enhance the off-axis control of the lower extremities in a functional way may be beneficial for people with PFP. Therefore, the purpose of this study was to examine the effects of an off-axis elliptical training program on improving off-axis neuromuscular control of the lower extremities, reducing pain, and improving knee function in individuals with PFP. We hypothesized that 1) following the off-axis elliptical training individuals with PFP would demonstrate improved off-axis control/stability (i.e., decreased pivoting and sliding instability of the legs) while stepping on the elliptical trainer; and 2) individuals with PFP would experience reduced pain and improved knee function post-training.
METHODS
Subjects
Twelve volunteers with PFP participated in the study (3 males and 9 females; age: 38.8±17.5 year; height: 170.3±9.0 cm; mass: 67.8±11.9 kg). Based on our previous pilot study investigating the effects of off-axis training in people with knee injuries,22 it is estimated that a sample size of 12 subjects would reach a power greater than 80% to detect a significant (p=0.05) improvement in the off-axis control post-training. All subjects had clinically diagnosed unilateral (N=4) or bilateral (N=8) PFP for at least the past 6 months. In addition to PFP, subjects reported no current or past lower extremity injuries and receiving no concurrent interventions for PFP during the study. Subjects were allowed to perform their usual daily and sport activities during the study. Subjects were excluded if they had neurologic disorders, current pregnancy, or cardiopulmonary disorders that prevented them from elliptical exercise. Prior to participation, all subjects gave informed consent approved by the institutional review board.
Off-axis elliptical trainer
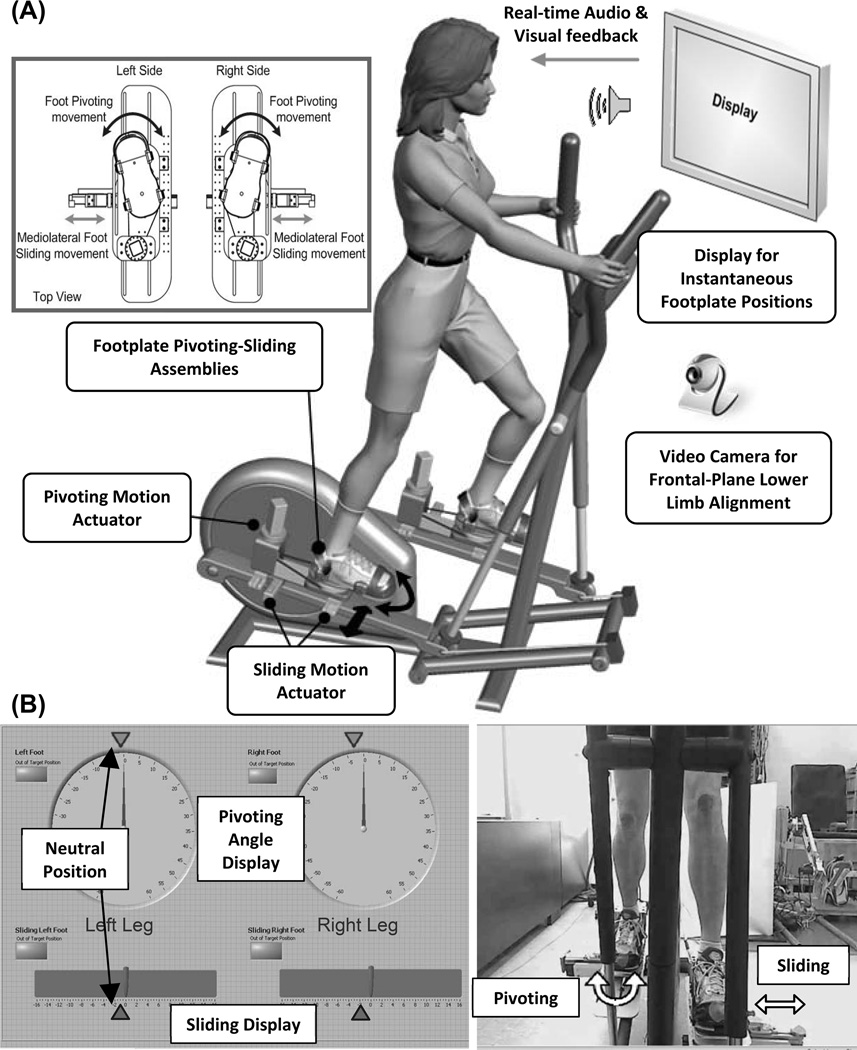
This study involved the use of a custom-made robotic off-axis elliptical trainer with motorized footplates to allow transverse-plane pivoting and frontal-plane sliding of the lower extremities during elliptical exercise.19 Briefly, the traditional footplates of an elliptical trainer were replaced with custom pivoting-sliding assemblies (Figure 1). Each footplate is driven by two servomotors through a cable-driven rotation mechanism for the transverse-plane pivoting and a linear guide for the frontal-plane sliding.19 The maximum sliding force and pivoting toque that could be generated by the motors underneath the footplate are 362 N and 30 Nm, respectively.19 Real-time audiovisual feedback regarding the instantaneous footplate positions (LabVIEW, National Instruments, Austin, TX) was displayed on the computer monitor in front of the subject. A video camera in front of the elliptical trainer provided real-time feedback of the frontal-plane lower limb alignment (Figure 1).
Figure 1.
Design of the robotic off-axis elliptical trainer with motorized footplates that allow transverse-plane pivoting and frontal plane sliding motions of the lower extremities during elliptical exercise (A). Real-time audiovisual feedback regarding the instantaneous footplate pivoting-sliding positions and frontal-plane lower limb alignment was displayed on the computer monitor in front of the subject (B).
The pivoting and sliding mechanisms were servo-controlled digitally (1000 Hz) with 3 different control modes that can be adjusted through a custom-made user-interface program (LabVIEW, National Instruments, Austin, TX): 1) Spring mode; 2) Free mode; and 3) Perturbation mode.19 Under the Spring mode, the footplates behaved like a spring that provides an assistive sliding force and/or pivoting torque to restore footplate positions if the footplates are moving away from the targeted positions. The magnitude of the assistive force/torque was determined by the stiffness of the “footplate spring” and the amount of pivoting angle or sliding distance based on Hooke's law.19 A decrease in the stiffness (i.e., less assistive force/torque) increases the difficulty of controlling the footplates. In the Free mode, the footplates were controlled as backdrivable to simulate a slippery surface. The slipperiness of the footplates could be adjusted through servomotor control to reduce the frictional force/torque inside the motor gears. Under the Perturbation mode, the servomotors underneath the footplates generated a force and/or torque to perturb the footplates.19 An increase in the perturbation force/torque increases the difficulty of controlling the footplates.
Procedures
Subjects went through 3 evaluations: before training, after training, and at follow-up 6 weeks following training. During each evaluation, subjects’ knee pain and function were evaluated using Knee Injury and Osteoarthritis Outcome Score (KOOS) and International Knee Documentation Committee (IKDC) questionnaires.23,24 Subjects also performed a single-leg hop task. They started in a single-leg standing position with the test leg, and hopped forward as far as possible while maintaining balance at landing. The hopping distance from 3 successful trials were measured.
Subjects’ off-axis neuromuscular control was evaluated based on their footplate motions when performing the elliptical exercise with the footplates allowed to pivot freely and with the footplates allowed to slide freely (i.e., Free mode). Before the pre-training evaluation, subjects practiced on the off-axis elliptical trainer to become familiar with the off-axis elliptical tasks. During elliptical testing, subjects placed their hands on the stationary handrails of the elliptical in front of them and performed the free-sliding and free-pivoting task (1 minute each) with a target speed of 30–40 cycles/minute. Subjects were given a one-minute break between tasks. During testing, subjects were instructed to maintain the starting neutral foot positions (the 2nd toe pointing forward), and real-time visual feedback of the footplate positions was provided on the display monitor.
Subjects’ proprioception to detect footplate pivoting motion was also evaluated.19 The right or left footplate was pivoted internally or externally (i.e., 4 possible conditions) by the motors at a constant speed of 1°/s. Each leg was tested under a weight-bearing and minimum-weight-bearing condition (Figure 2). Under the testing position, each foot and each pivoting direction were tested 4 times and thus a total of 16 trials were performed (8 trials/leg). The foot and pivoting direction were determined in a random order. During testing, the subjects closed their eyes, and were instructed to press a hand-held button as soon as they felt the subtle pivoting movement and then identify the direction and leg that was moved by the motors.
Figure 2.
An example of the limb positions for the pivoting proprioception testing. In this example, the left leg (foot in the lowest position) was at the weight-bearing condition in which the subject shifted the weight to the left leg, and the right leg (knee flexed) was at the minimum-weight-bearing condition.
The off-axis elliptical training program consisted of a total of 18 sessions within 6–8 weeks (2–3 sessions/week). During each session, subjects exercised on the off-axis elliptical trainer for 30 minutes with a target speed of 30–40 cycles/minute and with their hands on the stationary handrails of the elliptical. Each session started with a short warm-up and ended with a cool-down period during which the subject performed regular elliptical exercise (i.e., footplates locked). For the rest of each session, subjects received both the pivoting and sliding elliptical training using a combination of the three control modes (Spring, Free, and Perturbation). During training, real-time visual feedback of the footplate positions and frontal-plane leg alignment were provided. Subjects were instructed to maintain a neutral knee alignment (i.e., no varus and valgus) and neutral foot positions by minimizing the pivoting or sliding motion of the footplates.
The difficulty level of the training was gradually increased as the subjects progressed through the program. More specially, subjects started the training with a low difficulty setting (i.e., high stiffness for the Spring mode, high friction for the Free mode, and low force/torque perturbation for the Perturbation mode). Stepping resistance was also applied using the built-in resistance setting of the elliptical trainer (level 1–10 with 10 being the hardest to step). As subjects progressed and demonstrated better control of the off-axis motions, the control setting were adjusted (i.e., decreased stiffness and friction, increased perturbation intensity) to make the training more challenging. The difficulty level and stepping resistance were determined based on subjects’ feedback and tolerance such that the task was challenging to perform, yet the subjects did not experience any discomfort during and following each session.
Data Analysis
The KOOS and IKDC scores were calculated and normalized to 100 % to evaluate the change in knee pain and function post-training.23,24 The score of each of the 5 subscales of the KOOS score (i.e., Pain, Other Symptoms, Function in Daily Living, Function in Sport and Recreation, and Knee Related Quality of Life) was also normalized to 100 % for further analyses.
Lower extremity off-axis instability was quantified by calculating the root mean square (RMS) of the footplate pivoting angle (for the free-pivoting task) and RMS of the sliding distance (for the free-sliding task) during each elliptical cycle. Using this convention, a decreased RMS represents improved off-axis stability. The RMS value was also calculated for the first and second halves of each elliptical cycle, corresponding to the stance and swing phase of a gait cycle, respectively.25 Given that subjects might require several cycles to familiarize with the off-axis tasks, the data from the first 10 cycles were not included for analyses. The pivoting and sliding RMS values from the following 20 cycles were averaged to obtain the representative off-axis control measurements for each subject.
Pivoting proprioception was defined as the angle when the subject first perceived the footplate pivoting movement generated by the motors. The pivoting angles from multiple trials (i.e., 8 trials/leg for each condition) were averaged to represent the pivoting proprioception under the weight-bearing and minimum-weight-bearing condition. For the off-axis instability, proprioception, and single-leg hop distance, the data recorded from the symptomatic legs (for subjects with unilateral PFP) or the more symptomatic legs (for subjects with bilateral PFP) were used in subsequent statistical analyses.
Statistical Analysis
Friedman’s test was used to compare the differences among the 3 time points for the normalized KOOS and IKDC scores (SPSS Version20; IBM, Armonk, NY). If significance was found (P < 0.05), Wilcoxon Signed Rank tests with a modified sequentially rejective Bonferroni adjustment were used for post-hoc pairwise comparisons.26 For the single-leg hop distance, off-axis instability and pivoting proprioception measurements, a one-way ANOVA with repeated measures was used to compare the differences among the 3 time points. Paired-t tests with a modified sequentially rejective Bonferroni adjustment were used for post-hoc pairwise comparisons.26
RESULTS
Knee Pain and Function
Friedman’s tests reached significance for the normalized KOOS and IKDC scores (P<0.001; Table). Post-hoc testing indicated that the normalized KOOS and IKDC scores of the post-training and follow-up conditions were significantly greater than those of the pre-training condition (p<0.025; Table). Post-hoc testing also indicated that the normalized KOOS scores of the follow-up condition were significantly greater than the post-training condition (p<0.05; Table).
TABLE.
Normalized KOOS scores (and each of the 5 subscales), normalized IKDC scores, and single-leg hop distance.
| Pre Training | Post Training | Follow Up | ||
|---|---|---|---|---|
| Total KOOS Score* | 69.2 ± 11.2 | 81.6 ± 11.2† | 87.4 ± 8.6†‡ | |
| Pain* | 69.2 ± 10.5 | 81.3 ± 11.6† | 87.3 ± 8.3†‡ | |
| Other Symptoms* | 70.5 ± 13.2 | 76.8 ± 11.0† | 85.1 ± 14.4†‡ | |
| Function in Daily Living* | 78.6 ± 11.4 | 89.8 ± 10.2† | 95.0 ± 5.9†‡ | |
| Function in Sport* | 52.1 ± 18.0 | 73.3 ± 15.6† | 78.8 ± 20.8† | |
| Knee Related Quality of Life* | 49.0 ± 21.0 | 60.9 ± 20.7† | 70.3 ± 14.4†‡ | |
| IKDC Score* | 59.9 ± 14.2 | 75.0 ± 12.7† | 78.2 ± 13.6† | |
| Single-Leg Hop Distance (m)* | 0.96 ± 0.32 | 1.17 ± 0.38† | 1.16 ± 0.36† | |
Significant main effect (p <0.05) detected in Friedman’s test or one-way ANOVA with repeated measures
Significantly (p <0.025) smaller than the pre-training value
Significantly (p <0.05) smaller than the post-training value
Friedman’s tests also reached significance for each of the 5 KOOS subscales (P≤0.001; Table). For all of the 5 subscales, post-hoc testing indicated that the scores of the post-training and follow-up testing conditions were significantly greater than those of the pre-training condition (p<0.025; Table). Except for the “Function in Sport and Recreation”, post-hoc testing indicated that the scores of the other 4 subscales during the follow-up testing were significantly greater than those of the post-training condition (p<0.05; Table).
ANOVA tests reached significance for the single-leg hop distance (P<0.001; Table). Post-hoc testing indicated that the hop distance of the post-training and follow-up conditions were significantly greater than those of the pre-training condition (p<0.025; Table).
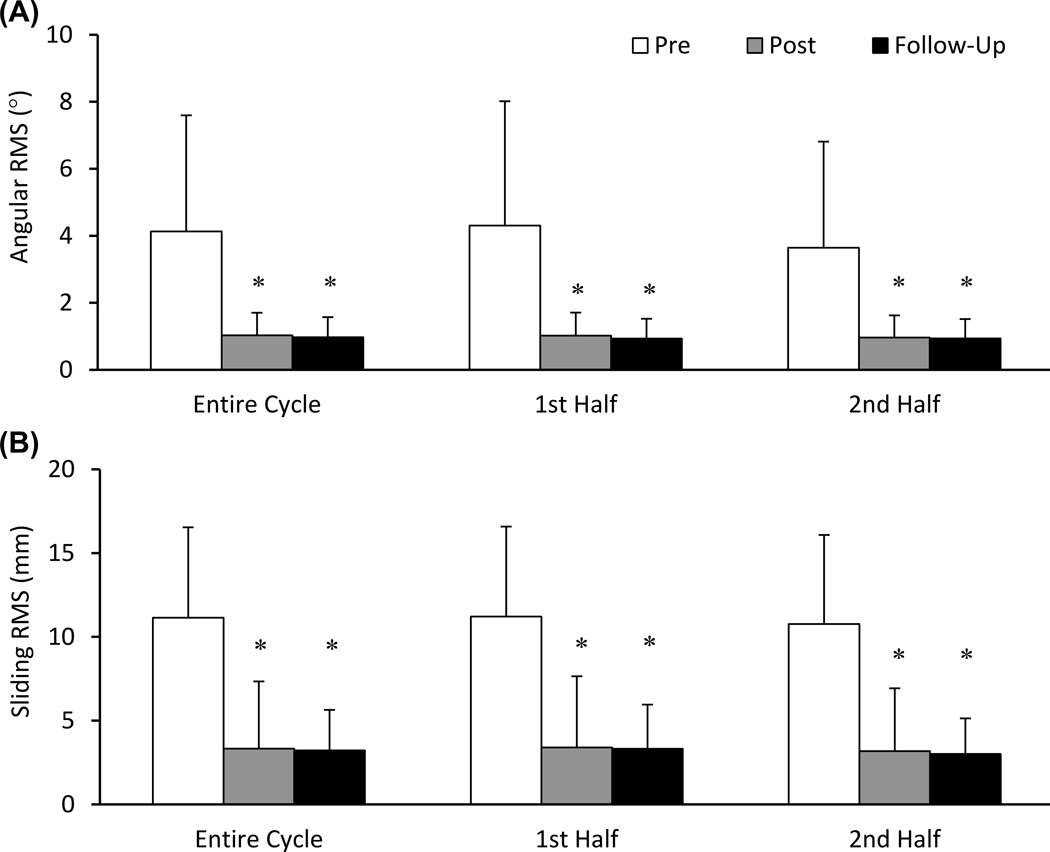
Off-Axis Instability Measurements
ANOVA tests reached significance for the pivoting angular RMS calculated from the entire elliptical cycle as well as the first and second halves of the cycle (P = 0.006, 0.007, and 0.007, respectively; Figure 3). Post-hoc testing indicated that the angular RMS values of the post-training and follow-up conditions were significantly smaller than the pre-training condition (p<0.025; Figure 3). On average, the angular RMS decreased by about 3° post-training (3.1±3.2°, 3.3±3.5°, and 2.7±2.9° for the entire cycle, first and second half, respectively) and remained decreased during follow-up (3.2±3.3°, 3.4±3.6°, and 2.7±3.0° for the entire cycle, first and second half, respectively).
Figure 3.
Angular (A) and sliding (B) RMS values during elliptical exercise (mean ± SD) before and after the completion of the training program. *Significantly less than the pre-training value.
ANOVA tests also reached significance for the RMS of the sliding distance calculated from the entire elliptical cycle as well as the first and second halves of the cycle (P<0.001; Figure 3). Post-hoc testing indicated that the RMS values of the sliding distance during the post-training and follow-up testing conditions were significantly shorter than the pre-training condition (p<0.025; Figure 3). The sliding distance RMS decreased by about 8 mm post-training (7.8±4.1, 7.8±4.0, and 7.6±4.2 mm for the entire cycle, first and second half, respectively) and remained decreased during the follow-up testing (7.9±4.7, 7.9±4.7, and 7.8±4.7 mm for the entire cycle, first and second half, respectively).
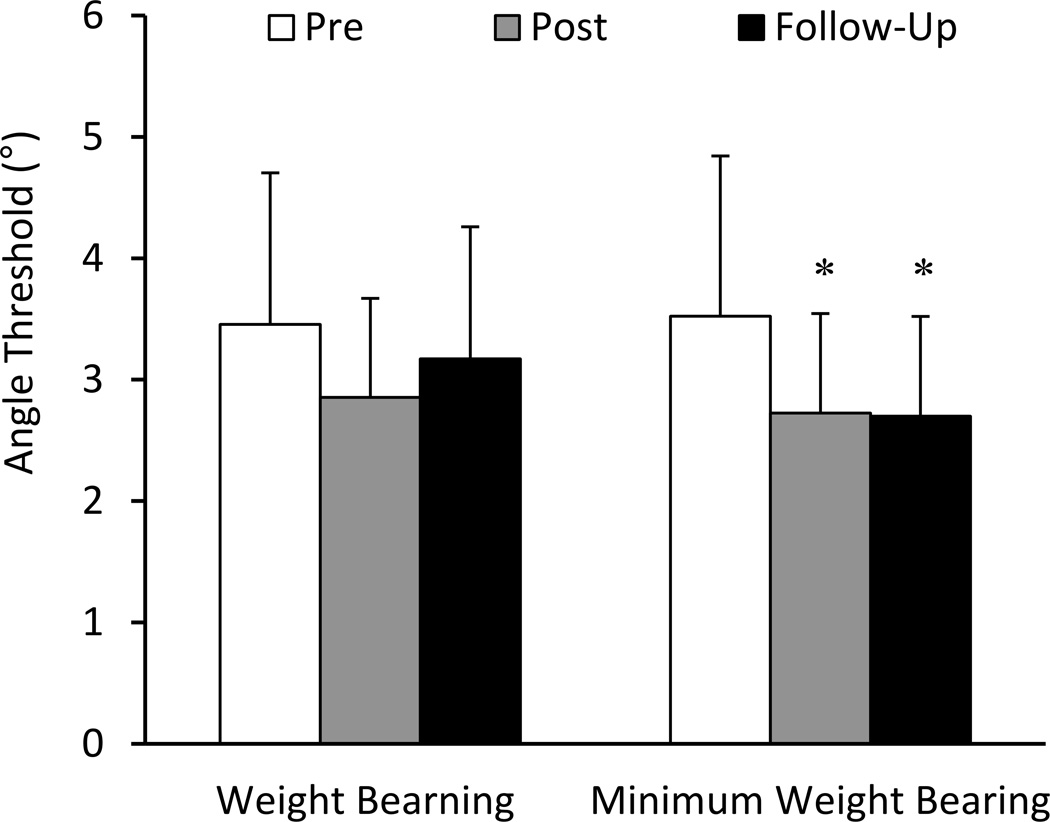
Pivoting Proprioception
ANOVA tests reached significance for the angular proprioceptive thresholds only in the minimum-weight-bearing condition (P=0.024; Figure 4). Post-hoc testing indicated that the angular proprioceptive thresholds of the post-training and follow-up conditions were significantly smaller than those of the pre-training condition (p<0.025; Figure 4). When compared to the pre-training values, the proprioceptive thresholds reduced by 0.8±1.2° post-training and remained decreased by 0.8±1.1° during the follow-up testing.
Figure 4.
Angular proprioceptive threshold to detect lower extremity transverse-plane rotation under weight-bearing and non-weight-bearing conditions (mean ± SD) before and after the completion of the training program. *Significantly less than the pre-training value.
DISCUSSION
The purpose of this study was to examine the effects of an off-axis elliptical training program on enhancing lower-extremity off-axis control and improving knee pain and function in individuals with PFP. To our knowledge, this is the first study that incorporates an exercise intervention to improve the neuromuscular control of the legs in the transverse and frontal planes under a functional weight-bearing activity in persons with PFP. The results supported the hypothesis that individuals with PFP would demonstrate improved off-axis stability, reduced pain and improved knee function following the off-axis elliptical training.
After training, subjects with PFP reported reduced pain and improved knee function as quantified using the KOOS and IKDC scores. Such improvements were maintained for at least 6 weeks post-training. On average, an increase of 12.3±5.8 (post-training) and 18.1±8.2 (follow-up) points in the KOOS as well as 12.1±5.4 (post-training) and 15.9±7.2 (follow-up) points in the IKDC score were observed. Subjects also demonstrated an increase of 23–24% in the hop distance following training, consistent with the significant increase in the “Function in Sport and Recreation” subscale of the KOOS. A minimal clinically important change ranging from 6 to 10 points has been reported when using IKDC or KOOS scores in individuals with knee injuries during a follow-up period of 3–6 months.23,27 While the minimal clinically important change may be influenced by many factors (e.g., symptom severity, injury type, etc.), we feel that the increased KOOS and IKDC scores from our subjects with PFP reflected a meaningful short-term (i.e., 6 weeks) improvement in their knee function and symptoms. However, further investigation is needed to understand the underlying mechanism(s) associated with the improvement in knee pain and function following off-axis elliptical training.
PFP is commonly associated with altered transverse- and/or frontal-plane kinematics of the lower extremities that lead to patellofemoral maltracking and increased joint stress.6,11–14 Following training, subjects with PFP demonstrated an improvement in minimizing the off-axis pivoting and sliding of the lower extremities during elliptical exercise. The improved off-axis control post-training may reduce the excessive lower extremity off-axis motions that are often observed in people with PFP, thereby reducing patellofemoral maltracking and stress. However, kinematics from individual lower extremity joints and patellofemoral joint loading was not estimated in the study. Additionally, while elliptical exercise has been used for gait training given their similarity,25,28 whether the improved off-axis control observed during elliptical exercise can be translated to daily functional activities, such as walking and running, remains unknown.
We also observed improved pivoting proprioception post-training with the test legs in the minimum-weight-bearing condition. On average, the proprioceptive thresholds decreased by about 0.8° following training. Given that the pivoting motion was motorized with a constant speed of 1°/s, a decrease of 0.8° suggests that subjects were about 800 ms faster to detect a passive pivoting motion applied to their legs. Although we expect that this improved proprioception may assist in better lower extremity alignment, whether this improvement represents a meaningful change require further investigations.
The current study was designed as a first step to determine the effects of a novel off-axis elliptical intervention on individuals with PFP. Therefore, several limitations must be acknowledged, and findings from the study must be interpreted carefully. While the sample size (N=12) was determined using a priori power analysis,22 our sample size was relatively small and may have limited the generalizability of our findings to the PFP population. We did not implement a control group. Several previous intervention studies with a control group reported minimum (or negative) changes in knee pain in the control groups.15,29–32 Given these findings and the fact that subjects in this study had PFP for at least 6 months, we feel that the improvement observed was a result of the elliptical training. However, we also did not have a comparison group that only exercised on a regular elliptical trainer. Although elliptical trainers are a common form of exercise and our subjects with PFP reported previous experience of using elliptical trainers, it remains unclear whether the observed improvement can be attributed to the unique off-axis feature in our training.
While we tried to minimize the potential variability by having all subjects tested by the same investigator, our design would not allow for blinding procedures. While we consider that our testing and measurements to be objective, the lack of blinding procedures may have resulted in potential tester bias. We also did not assess the changes in lower extremity kinematics during daily activities, such as walking and running. Finally, we did not implement objective criteria for determining the progression of the training. The difficulty levels of the training program were simply adjusted based on each subject’s tolerance and feedback. Based on our positive findings of off-axis elliptical training, future studies may focus on developing standardized evaluation/assessment criteria to optimize training effects.
CONCLUSIONS
This study demonstrates a novel intervention that provides off-axis training for individuals with PFP to better control the frontal- and transverse-plane motions of the lower extremities under a functional weight-bearing elliptical exercise. Our findings revealed that subjects with PFP experienced reduced pain and improved knee function following the off-axis elliptical intervention. The novel off-axis intervention may be incorporated with other common treatment options currently available for PFP (e.g., muscle strengthening) to augment the effects of musculoskeletal rehabilitation for this population.
Clinical Relevance.
This study provides a novel intervention approach to enhance the control of the frontal- and transverse-plane motions of the lower extremities during functional weight-bearing activities. This novel off-axis elliptical training may be incorporated with other common treatment options currently available for PFP to augment the effects of musculoskeletal rehabilitation for the PFP population.
Acknowledgments
Source of Funding:
The present study was supported in part by the National Institutes of Health, National Science Foundation, and National Institutes on Disability and Rehabilitation Research.
Footnotes
Conflicts of Interest
Two authors, Li-Qun Zhang and Yupeng Ren, hold equity positions in Rehabtek LLC, which received funding from the National Science Foundation in developing the off-axis elliptical trainer used in the study.
REFERENCES
- 1.Davis IS, Powers CM. Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat. J Orthop Sports Phys Ther. 2010;40:A1–A16. doi: 10.2519/jospt.2010.0302. [DOI] [PubMed] [Google Scholar]
- 2.Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Factors associated with patellofemoral pain syndrome: a systematic review. Br J Sports Med. 2013;47:193–206. doi: 10.1136/bjsports-2011-090369. [DOI] [PubMed] [Google Scholar]
- 3.Fredericson M, Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85:234–243. doi: 10.1097/01.phm.0000200390.67408.f0. [DOI] [PubMed] [Google Scholar]
- 4.Boling M, Padua D, Marshall S, et al. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20:725–730. doi: 10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roush JR, Curtis Bay R. Prevalence of anterior knee pain in 18–35 year-old females. Int J Sports Phys Ther. 2012;7:396–401. [PMC free article] [PubMed] [Google Scholar]
- 6.Powers CM, Bolgla LA, Callaghan MJ, et al. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42:A1–A54. doi: 10.2519/jospt.2012.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fulkerson JP. Disorders of the Patellofemoral Joint. 3rd ed. Baltimore: Williams & Wilkins; 1997. p. 365. [Google Scholar]
- 8.Wilson NA, Press JM, Koh JL, et al. In vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral pain. J Bone Joint Surg Am. 2009;91:558–566. doi: 10.2106/JBJS.G.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin F, Makhsous M, Chang AH, et al. In vivo and noninvasive six degrees of freedom patellar tracking during voluntary knee movement. Clin Biomech (Bristol, Avon) 2003;18:401–409. doi: 10.1016/s0268-0033(03)00050-0. [DOI] [PubMed] [Google Scholar]
- 10.Farrokhi S, Keyak JH, Powers CM. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: a finite element analysis study. Osteoarthritis Cartilage. 2011;19:287–294. doi: 10.1016/j.joca.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barton CJ, Levinger P, Crossley KM, et al. The relationship between rearfoot, tibial and hip kinematics in individuals with patellofemoral pain syndrome. Clin Biomech (Bristol, Avon) 2012;27:702–705. doi: 10.1016/j.clinbiomech.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Souza RB, Draper CE, Fredericson M, et al. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40:277–285. doi: 10.2519/jospt.2010.3215. [DOI] [PubMed] [Google Scholar]
- 13.Powers CM, Ward SR, Fredericson M, et al. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33:677–685. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]
- 14.Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech (Bristol, Avon) 2008;23:203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Khayambashi K, Mohammadkhani Z, Ghaznavi K, et al. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42:22–29. doi: 10.2519/jospt.2012.3704. [DOI] [PubMed] [Google Scholar]
- 16.Barton CJ, Menz HB, Crossley KM. Effects of prefabricated foot orthoses on pain and function in individuals with patellofemoral pain syndrome: a cohort study. Phys Ther Sport. 2011;12:70–75. doi: 10.1016/j.ptsp.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Mills K, Blanch P, Dev P, et al. A randomised control trial of short term efficacy of in-shoe foot orthoses compared with a wait and see policy for anterior knee pain and the role of foot mobility. Br J Sports Med. 2012;46:247–252. doi: 10.1136/bjsports-2011-090204. [DOI] [PubMed] [Google Scholar]
- 18.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154–163. doi: 10.1177/0363546510379967. [DOI] [PubMed] [Google Scholar]
- 19.Ren Y, Lee SJ, Park HS, et al. A pivoting elliptical training system for improving pivoting neuromuscular control and rehabilitating musculoskeletal injuries. IEEE Trans Neural Syst Rehabil Eng. 2013;21:860–868. doi: 10.1109/TNSRE.2013.2273874. [DOI] [PubMed] [Google Scholar]
- 20.Lee SJ, Ren Y, Geiger F, et al. Gender differences in offaxis neuromuscular control during stepping under a slippery condition. Euro J Appl Physiol. 2013;113:2857–2866. doi: 10.1007/s00421-013-2727-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee SJ, Ren Y, Chang AH, et al. Effects of Pivoting Neuromuscular Training on Pivoting Control and Proprioception. Med Sci Sports Exercise. doi: 10.1249/MSS.0000000000000249. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee SJ, Ren Y, Geiger F, et al. Offaxis neuromuscular training of knee injuries using an offaxis robotic elliptical trainer. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:2081–2084. doi: 10.1109/IEMBS.2011.6090386. [DOI] [PubMed] [Google Scholar]
- 23.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 25.Burnfield JM, Shu Y, Buster T, et al. Similarity of joint kinematics and muscle demands between elliptical training and walking: implications for practice. Phys Ther. 2010;90:289–305. doi: 10.2522/ptj.20090033. [DOI] [PubMed] [Google Scholar]
- 26.Rom DM. A sequentially rejective test procedure based on a modified Bonferroni inequality. Biometrika. 1990;77:663–665. [Google Scholar]
- 27.Greco NJ, Anderson AF, Mann BJ, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form in comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, modified Cincinnati Knee Rating System, and Short Form 36 in patients with focal articular cartilage defects. Am J Sports Med. 2010;38:891–902. doi: 10.1177/0363546509354163. [DOI] [PubMed] [Google Scholar]
- 28.Damiano DL, Norman T, Stanley CJ, et al. Comparison of elliptical training, stationary cycling, treadmill walking and overground walking. Gait Posture. 2011;34:260–264. doi: 10.1016/j.gaitpost.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Loudon JK, Gajewski B, Goist-Foley HL, et al. The effectiveness of exercise in treating patellofemoral-pain syndrome. J Sport Rehabil. 2004;13:323–342. [Google Scholar]
- 30.Song CY, Lin YF, Wei TC, et al. Surplus value of hip adduction in leg-press exercise in patients with patellofemoral pain syndrome: a randomized controlled trial. Phys Ther. 2009;89:409–418. doi: 10.2522/ptj.20080195. [DOI] [PubMed] [Google Scholar]
- 31.Fukuda TY, Rossetto FM, Magalhaes E, et al. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40:736–742. doi: 10.2519/jospt.2010.3246. [DOI] [PubMed] [Google Scholar]
- 32.Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007;37:155–160. doi: 10.2519/jospt.2007.2433. [DOI] [PubMed] [Google Scholar]