Abstract
The rehabilitation of medically compromised elderly patients with long span partially edentulous arches has been a tremendous challenge for dentists. Proper dental management requires a commitment to provide the best treatment despite the compromised oral conditions. The aim of this paper is to describe the prosthetic rehabilitation of an elderly patient who presented with chief complaints of gagging sensation while using upper denture, loose upper and lower dentures and difficulty in eating food. Patient was rehabilitated using removable partial denture with semi-rigid attachments in the maxillary arch and telescopic prosthesis in the mandibular arch. Use of semi precision attachments helped in increasing the retentive ability of the maxillary prosthesis, even in the presence of only few abutments. Fabrication of a telescopic denture is a technique sensitive procedure but it offers advantages like bilateral splinting effect in long span partially edentulous arches, reduced effective crown–root ratio, maintenance of proprioception and transfer of forces along the long axis of the abutments. Although the management was complex but it improved patient’s esthetics, oral function and social confidence.
Keywords: Multiple missing teeth, Fixed removable prosthesis, Telescopic prosthesis, Semi-precision attachment
Introduction
Partial edentulism is defined as the absence of some but not all of the natural teeth in a dental arch. The management of long span partially edentulous arches in medically compromised elderly patients is a daunting task. Although the management is complex but the rewards can be satisfying [1]. Various treatment modalities are available for replacement of multiple missing teeth such as fixed partial denture, Implants supported dentures, removable cast partial dentures, over dentures, telescopic prosthesis and different attachments etc., but there are certain limitations to each of these.
In many clinical situations, periodontal status and location and position of remaining teeth is such that it precludes the use of fixed partial dentures [2]. Implant supported dentures can be fabricated in such cases, but adequate width and height of bone at the prospective implant site is a primary requisite along with other factors like absence of any local or systemic risk factor and good financial status of the patient [3].
Implants and other current innovations do not make telescopic retainer obsolete; on the contrary, they can enhance each other and expand the range of viable treatment alternatives. Telescopic retainers provide a modality of treatment that can facilitate maintenance and enhance the survival of natural abutments and also provide additional option for the restoration of a partially edentulous mouth [4–7]. Therefore telescopic prosthesis provides a high degree of intraoral comfort and long term viability.
Intracoronal and extracoronal attachments may be used in treatment of long span partially edentulous arches requiring removable partial dentures. Use of a precision attachment provides advantages like better retention, esthetics, patient comfort, maintainable periodontal health and longevity of abutment teeth [8–10]. The present report describes oral rehabilitation using removable partial denture with semi-rigid attachment in maxillary arch and telescopic prosthesis in mandibular arch, in a geriatric patient having history of breast carcinoma and high gag reflex.
Outline of the Case
A 65-year-old partially-dentate female patient reported with chief complaints of looseness of upper and lower partial dentures, gagging sensation with the use of upper denture which led to difficulty in chewing food. Medical history revealed that the patient had undergone surgery followed by chemotherapy and radiotherapy for treating breast cancer 3 years ago. Dental history revealed that patient had removable partial dentures but she was not using them as they were loose and she felt gagging sensation whenever she tried to wear them.
Extra oral examination revealed concave facial profile with reduced vertical facial height, poor tone of the facial tissues, thin and short upper lip and reduced lip support (Fig. 1a).
Fig. 1.
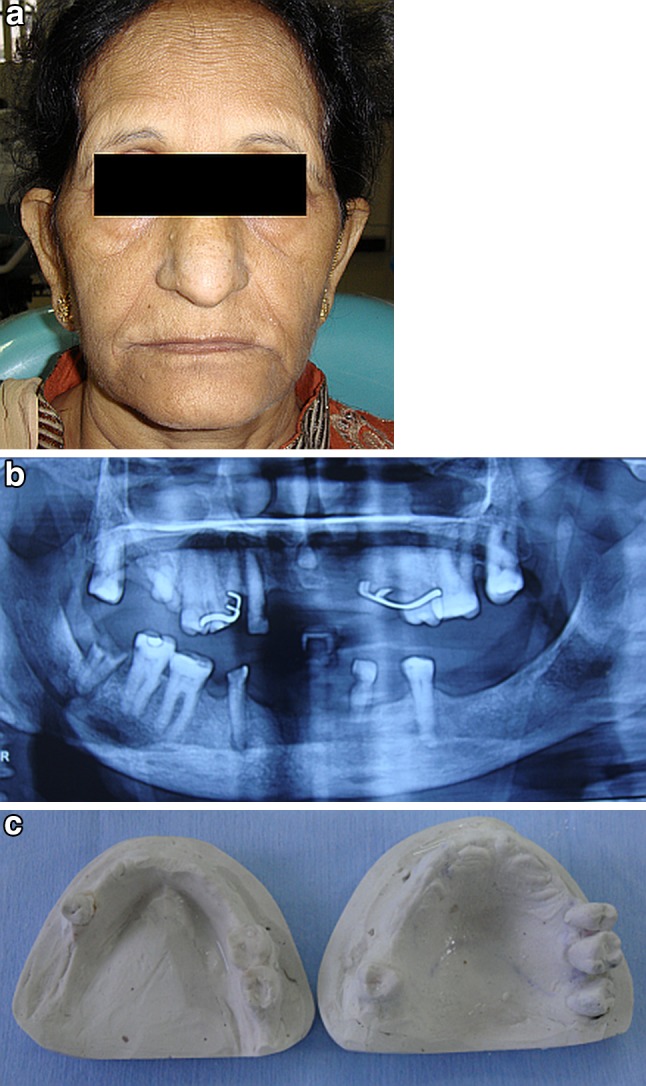
a Pre-treatment extra oral view. b Pre-treatment panorex view. c Diagnostic casts
Intraoral examination: 15, 16, 17, 18, 25, 26, 28, 32, 35, 44, 46, 47 and 48 were present. Teeth 15, 16, 32 were mobile. 17, 44, 48 were root stumps and 35, 47 were carious (FDI tooth numbering system).
Examination of old prosthesis revealed that both maxillary and mandibular partial dentures were not retentive and maxillary prosthesis had full palatal coverage.
Radiographic examination revealed only 18, 25, 26, 35, 46 and 47 had good quality of supporting bone and continuous lamina dura (Fig. 1b). Remaining teeth and root stumps had poor quality of supporting bone.
Preprosthetic Phase
Teeth with guarded prognosis (15, 16 and 32) and root stumps (17, 44, and 48) were extracted and amalgam restoration was done in 35 and 47. Teeth 18, 25, 26 and 28 were left in maxillary arch (Kennedy’s class IV) and 35, 46 and 47 were left in mandibular arch (Kennedy’s class II mod I).
Treatment Executed
Treatment option that appeared most suitable to restore this case was removable partial prosthesis with semi-rigid attachment in the maxillary arch and telescopic removable prosthesis for mandibular arch.
Fabrication Procedure
Maxillary and mandibular diagnostic impressions were made with irreversible hydrocolloid (Zelgan, Dentsply India Ltd.) and casts were poured with type III gypsum product (Fig. 1c). Occlusal rims were fabricated and adjusted according to the phonetics and esthetics. Vertical dimension was assessed by using physiological and mechanical methods. Maxillary and mandibular casts were mounted on a semi adjustable articulator (Whip Mix Corporation 361 Farmington Ave. Louisville, KY USA) with the help of facebow (Quick mount facebow) and centric relation record. Artificial resin teeth were set following the landmarks for establishing occlusal plane. The wax up was done on the abutments also to develop a bilateral balanced occlusion.
In the maxillary arch, teeth were prepared for fabrication of metal ceramic crowns. Left maxillary third molar was not prepared due to inaccessibility in that region as it was bucally tilted. Mandibular teeth were prepared for the fabrication of telescopic copings.
Impression of prepared abutments was made with putty reline technique and was poured in type IV die stone (Kalrock, Kalabhai Karson Pvt Ltd., Mumbai, India). Maxillary cast was mounted with the help of face bow record and mandibular cast was mounted in centric relation. Then, the wax patterns for telescopic copings in the mandibular arch were fabricated with cut back technique to achieve 0.5–1 mm wide shoulder. These copings were surveyed to achieve near parallel axial walls. Maxillary copings were fabricated and the male components of semirigid precision attachments (BeGo precision elements Ancora Profile rod attachment dimensions: bar length 6 mm, head diameter 1.75 mm, Germany) were attached to copings with the help of surveyor to achieve parallelism. These wax patterns were invested and casted in Ni–Cr alloy (Bellabond plus, BeGo, Germany).
Cast metal copings were finished and surveyed again to check parallelism. Porcelain was applied on maxillary copings against the mandibular trial denture. After required adjustments, crowns and copings were polished and cemented with Glass Ionomer cement (3 M ESPE, Ketac™ Cem Easymix, Bangalore, India) (Fig. 2).
Fig. 2.

Cemented metal copings
Maxillary and mandibular final impressions were made with dual impression technique. This helped to record the complete border extensions of the residual ridge within the physiological limits and to record the anatomic details of the metal copings. Master casts were obtained.
Fabrication of Overlay Metal Framework for Mandibular Teeth
After surveying, wax up for framework was done on the refractory mandibular cast. The design of the framework included a lingual bar placed 3 mm away from the marginal gingiva and overlay copings on 35, 46 and 47 (Fig. 3a). The pattern was invested using phosphate bonded investment (Wirovest BeGo, Germany) and casted using Co–Cr alloy (Bellabond plus BeGo, Germany). Framework try-in was done to verify its fit (Fig. 3b). Porcelain application was done on the overlay copings according to the diagnostic wax up.
Fig. 3.
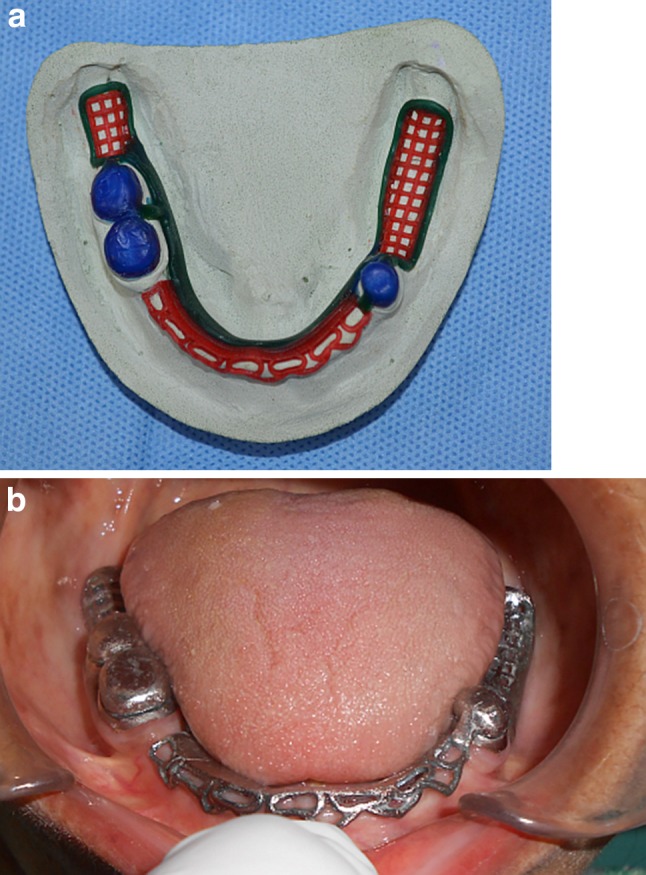
a Wax pattern on refractory cast. b Metal framework try- in
Try-in and Delivery of Maxillary and Mandibular Removable Prosthesis
Master casts were mounted on semi adjustable articulator with the help of facebow and centric relation record. Artificial resin teeth were set following the established occlusal plane. Try-in was taken in the patient’s mouth to verify fit, esthetics and to take patient’s consent before acrylization of the final prosthesis (Fig. 4a, b).
Fig. 4.

a Try-in (Right lateral view). b Try-in (Left lateral view)
Finally, after curing, remounting, finishing and polishing, female component was attached to the maxillary denture with self-cured tooth coloured acrylic resin. Maxillary and mandibular dentures were delivered to the patient after occlusal adjustments (Fig. 5a, b, c).
Fig. 5.
a Final maxillary prosthesis (occlusal view). b Final mandibular prosthesis (occlusal view). c Final prosthesis
Post Insertion Instructions and Recall
Post insertion instructions were given to the patient that included maintenance of meticulous oral hygiene and she was put on a six month follow up regimen. At each follow up visit, patient was evaluated for effectiveness of oral hygiene, retention and stability of the prosthesis.
Discussion
In the present case, rehabilitation was done with telescopic removable prosthesis in mandibular arch and removable partial prosthesis with semi-rigid attachment in the maxillary arch. Fixed dental prosthesis was not thought to be a good option for this particular case as it would have resulted in excessive forces on the remaining teeth. Cast partial denture was also excluded as number and distribution of the remaining teeth were not suitable to provide the desired amount of direct and indirect retention. Further, the patient’s unwillingness for any surgical procedure ruled out the option of implant supported prosthesis too.
The Glossary of Prosthodontic Terms defines a telescopic crown as “an artificial crown constructed to fit over a coping (framework). The coping can be another crown, a bar, or any other suitable rigid support for the dental prosthesis [11]. The telescopic unit, serving as anchorage in removable dental restorations, is based on a double crown design. The primary coping protects the abutment tooth from caries and thermal irritations and provides the basic element for retention and stabilization of the outer part. The secondary crown, being an integral part of the removable superstructure serves as a unit and it anchors the rest of the dentition [12, 13]. Telescopic crowns provide dental restorations with many of the advantages of both fixed and removable prostheses [14–18]. Yalisove and Dietz showed that in telescopic crown-sleeve-coping restorations, the effective crown-to-root ratio is reduced at the point where the telescopic over crown rotates. Inclusion of weak abutments is also possible, because the loss of a weak abutment does not compromise the entire prosthesis [19]. Telescopic dentures provide bilateral splinting effect in long span partially edentulous arches. Removability of superstructure enables the use of pink base material to replace lost bone and restore the soft tissue, achieving a more aesthetic appearance. By removing the over prosthesis, the gingival tissues are easily accessible around the entire marginal circumference of the abutment thus permitting easy home care and oral hygiene. Hence, patient can maintain good periodontal health around abutments. Also, the overdenture maintains teeth as a part of residual ridge. This gives the patient a denture that has far more support than any conventional appliance. Instead of soft movable mucous membrane, the denture literally sits on teeth ‘pilings’, enabling the denture to withstand a much greater occlusal load without movement [4, 20]. In addition to this, reduction of lateral stress on abutments by using telescopic retainer has been well documented. Pezzoli et al. [21] evaluated load transmission in distal extention partial dentures and found that telescopic retainers “produced less stress in the edentulous region and transmits loads more equally to the abutments”.
On the other hand, the application of the double crowns requires considerable clinical skill and experience. In the past, telescopic retainers were perceived as having disadvantages of increased bulk, expensive and complex laboratory procedures which contribute to the high cost of treatment.These obstacles are not significant any more, as new light cure resin materials, bonding techniques that allow these resin materials to be bonded directly to the metal crown frames, and less expensive casting alloys have substantially removed the difficulty in this modality of treatment [22].
Retention of the maxillary denture is one of the most important concerns for the patients as it affects their function as well as social confidence. But this was difficult to achieve in our case because of few remaining teeth to act as abutments. Therefore, extracoronal attachments were used to enhance the retention of maxillary partial denture as they offer different path of insertion from the pull of muscles and the action of tongue and gravity [8–10].
Such prosthesis leads to cross arch load transfer and thus leads to better prosthesis stabilization. As compared to conventional clasp retained partial denture, it is less liable to fracture, less bulky, provides better retention and stability, aesthetics and leads to less food stagnation [9]. Crown contour is better achieved in the gingival area with laboratory fabricated precision attachment. All these factors lead to elevated psychological acceptance by the patients.
On the other hand, use of these attachments have some disadvantages like added cost because of complex laboratory and clinical procedure, wearing of attachment components and cooperation and manual dexterity are essentially required from the patient.
Therefore, thorough and insightful treatment planning, a sound knowledge base, practical experience and reliable technical support must be available in order to be successful with this type of prosthesis.
Summary
A medically compromised elderly patient with long span partially edentulous arches was rehabilitated with the help of fixed removable type of telescopic prosthesis in mandibular arch and removable partial prosthesis with semi-rigid attachments in the maxillary arch. Although the treatment was complex but it improved patient’s aesthetics, oral function and social confidence. Periodic follow ups and meticulous prosthesis maintenance by the patient will hold the key for the ultimate success of this type of rehabilitation.
Acknowledgments
Financial support
None.
Contributor Information
Bhavita Wadhwa, Phone: +91-9971465152, Email: drbhavitamds@gmail.com.
Veena Jain, Phone: +91-9868187441, Email: jainveena1@gmail.com.
Gunjan Pruthi, Email: gunjan_prostho@yahoo.co.in.
References
- 1.Eichner K. Recent knowledge gained from long-term observations in the field of prosthodontics. Int Dent J. 1984;34:35–40. [PubMed] [Google Scholar]
- 2.Ante IH. The fundamental principles, design and construction of crown and bridge prosthesis. Dent Items Interest. 1928;1:215–232. [Google Scholar]
- 3.Misch CE. Dental implant prosthetics. 2. St Louis: Elsevier Mosby; 2005. p. 207. [Google Scholar]
- 4.Breitman JB, Nakamura S, Freedman AL, Yalisove IL. Telescopic retainer: an old or new solution? A second chance to have a normal dental function. J Prosthodont. 2012;21:79–83. doi: 10.1111/j.1532-849X.2011.00797.x. [DOI] [PubMed] [Google Scholar]
- 5.Swoope CC. Prosthetic considerations in tooth removal. Dent Clin North Am. 1969;13:857–870. [PubMed] [Google Scholar]
- 6.Atwood DA. Some clinical factors related to rate of resorption of the residual ridges. J Prosthet Dent. 1962;12:446–450. doi: 10.1016/0022-3913(62)90125-7. [DOI] [PubMed] [Google Scholar]
- 7.Gershkoff A. The subperiosteal unilateral implant as a distal abutment and as a support to the periodontally involved teeth. Dent Clin North Am. 1970;14:95–102. [PubMed] [Google Scholar]
- 8.Preiskel HW. Precision attachments in dentistry. 3. St Louis: CV Mosby Co; 1979. p. 171. [Google Scholar]
- 9.Wang CH, Lee HE, Du JK, Igarashi Y. Connecting rigidities of various precision attachments compared with a conical crown retained telescope. Kaohsiung J Med Sci. 2005;21:22–28. doi: 10.1016/S1607-551X(09)70272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phoneix RD, Cagna, Defreest CF (2008) Stewart’s clinical removable partial prosthodontics, 4th edn. Quintessence publishing Co Inc, Hanover Park, USA, pp 501–508
- 11.The glossary of prosthodontics terms (2005) J Prosthet Dent 94:10-92 [DOI] [PubMed]
- 12.Langer A. Telescope retainers and their clinical application. J Prosthet Dent. 1980;44:516–522. doi: 10.1016/0022-3913(80)90070-0. [DOI] [PubMed] [Google Scholar]
- 13.Berman H, Lusting P. Primary substructure and removable telescope superstructure in denture reconstruction. J Prosthet Dent. 1960;10:724–732. doi: 10.1016/0022-3913(60)90254-7. [DOI] [Google Scholar]
- 14.Schweitzer JM, Schweitzer RD, Schweitzer J. The telescoped complete denture. A research report at the clinical level. J Prosthet Dent. 1971;26:357–372. doi: 10.1016/0022-3913(71)90167-3. [DOI] [PubMed] [Google Scholar]
- 15.Miller PA. Complete dentures supported by natural teeth. J Prosthet Dent. 1958;8:924–928. doi: 10.1016/0022-3913(58)90122-7. [DOI] [PubMed] [Google Scholar]
- 16.Weaver JD. Telescopic copings in restorative dentistry. J Prosthet Dent. 1989;61:429–433. doi: 10.1016/0022-3913(89)90008-5. [DOI] [PubMed] [Google Scholar]
- 17.Perel ML. Telescope denture. J Prosthet Dent. 1973;29:151–156. doi: 10.1016/0022-3913(73)90107-8. [DOI] [PubMed] [Google Scholar]
- 18.Isaacson GO. Telescope crown retainer for removable partial denture. J Prosthet Dent. 1969;22:436–448. doi: 10.1016/0022-3913(69)90211-X. [DOI] [PubMed] [Google Scholar]
- 19.Yalisove IL, Dietz JR. Telescopic prosthetic therapy. Philadelphia: George F Stickley Co; 1977. p. 11. [Google Scholar]
- 20.DeFranco RL. Overdentures. In: Winkler S, editor. Essentials of complete denture prosthodontics. 2. St. Louis, USA: Ishiyaku EuroAmerica Inc.; 2000. pp. 384–385. [Google Scholar]
- 21.Pezzoli M, Rossetto M, Calderale PM. Evaluation of load transmission of distal-extension removal partial dentures using reflection photoelasticity. J Prosthet Dent. 1986;56:325–327. doi: 10.1016/0022-3913(86)90015-6. [DOI] [PubMed] [Google Scholar]
- 22.Weigl P, Hahn L, Lauer HC. Advanced biomaterials used for a new telescopic retainer for removable dentures. J Biomed Mater Res. 2000;53:320–336. doi: 10.1002/1097-4636(2000)53:4<320::AID-JBM6>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]



