Abstract
The present clinical report describes the prosthodontic management for a patient with uncontrolled bleeding and diabetes mellitus treated with a maxillary complete denture and a mandibular partial fixed dental prosthesis designed to interface with a removable cast framework partial denture retained by 2 ERA attachments. This approach was undertaken to improve both retention and stability of the distal extension Kennedy Class I removable partial denture. The rehabilitation provided better anterior esthetics than if treated with a conventional clasp retained removable partial denture, by employing a simple, practical design and offering a significant biomechanical advantages, restoring both oral health and function. Thus, this treatment modality, involving an ERA system and transfixation in fixed crowns, is an effective treatment and can be indicated as a clinical alternative for edentulous and partially edentulous patients with systemic disorders or for patients in economic situations that might preclude implant-based rehabilitation.
Keywords: Removable prosthetics, Health status, Dental abutments, Dental benefits, Dental clasps
Introduction
Dental implants associated with removable partial dentures have been used with satisfactory results in the dental treatment of patients with extensive tooth loss [1]. However, the use of implants is not always affordable for many patients [2, 3]. In these situations, removable partial dentures (RPDs) constitute a feasible option. RPDs are recommended for public health service clinics where costs must be considered, mainly in those situations in which implants are not indicated [4, 5], such as in individuals with poor general health status that contraindicates the use of implants or any type of surgery [2, 3]. In such situations, patients often would prefer not showing the anterior buccal clasps of RPDs.
RPDs can be retained and stabilized with a variety of attachments instead of RPD clasps. Extracoronal resilient attachments (ERAs) have demonstrated appropriate mechanical resilience, retention and stability [6]. The main advantage of ERA attachments, when compared with conventional clasp retained removable prostheses, are their esthetics, by eliminating the use of buccal/facial clasps of the RPDs thereby making the retentive design of the prosthesis invisible. In addition, when compared to implant-supported prostheses, removable partial dentures retained by ERAs have lower costs and a shorter time span for fabrication [7]. Thus, the present clinical case report describes the fabrication technique for a cast framework RPD retained by ERA attachments, interfaced with a partial fixed dental prosthesis, to provide for stability, retention and improved esthetics for a patient with compromised health.
Outline of the Case
A 55-year-old male with poor general health status presented to the Meridional Study Center in Uningá, Brazil, with the primary complaint of a lack of esthetics and poor masticatory function. The clinical examination revealed a need for both maxillary and mandibular arch rehabilitation (Fig. 1).
Fig. 1.
Intraoral view of the patient with (a) and without the prosthesis (b), mandibular occlusal view (c), maxillary occlusal view (d)
The medical and dental histories were reviewed and discussed with the patient. The patient had a history of bleeding because of type II diabetes mellitus; therefore, implant therapy was excluded due to the risk of post-surgical complications.
The intraoral examination revealed that the mandibular right molar presented with a clinically acceptable amalgam restoration, while the remaining mandibular anterior incisors all presented with carious lesions. Radiographic examination (Fig. 2) of these mandibular remaining anterior teeth demonstrated periapical radiolucencies, necessitating endodontic treatment, then posts and cores and full coverage indirect restorations. The residual root of the mandibular right premolar was recommended for extraction.
Fig. 2.
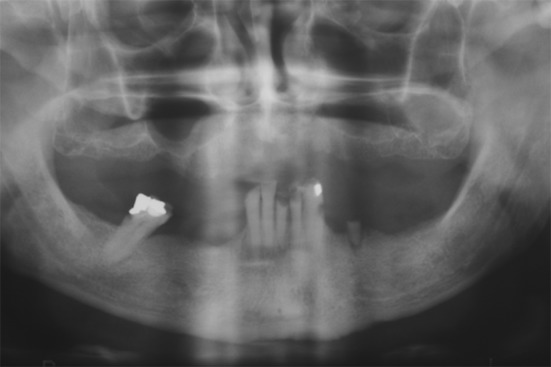
Initial radiograph
Several treatment options were offered to the patient, and the difficulty of obtaining adequate retention, stability, and esthetics with an anterior buccal clasps for a mandibular RPD was also considered. For this reason, a new complete maxillary denture and a mandibular RPD with an ERA attachment partial fixed dental prosthesis was the chosen as the treatment of choice.
The mandibular anterior incisors were prepared with round end diamond burs (KG Sorensen, Cotia, Brazil) to prepare them to receive metal ceramic crowns. The left canine and lateral incisor and right lateral and central incisors were selected to be splinted and serve as abutment teeth for the RPD. Provisional acrylic resin crowns were fabricated for the mandibular anterior teeth, and a provisional removable partial denture was created for the interim replacement of the missing posterior teeth. Preliminary maxillary and mandibular impressions were obtained with irreversible hydrocolloid (Hydrogum; Zermach, Italy) and a definited cast of the tooth preparations was fabricated in type III gypsum (Microstone; Whip Mix Corp, Louisville, KY). The wax-up of the metallic structure for the fixed prostheses was prepared. The matrix for each ERA attachment (SternGold Implamed; SP, Brazil) was appropriately positioned allowing for adequate tissue clearance and vertical space for the patrix/housing, framework and overlying replacement tooth (Fig. 3). The crowns were splinted for better distribution of the occlusal loading of the posterior teeth on the removable partial denture that was transmitted to the natural endodontically treated anterior tooth abutments via the ERA attachments.
Fig. 3.

Wax-up of the metallic structure: female ERA attachment on the left and right sides. Crowns positioned in the remaining mandibular anterior teeth, already milled and with transfixation in the lingual surface. Thin black arrows the transfixation; thick black arrows female ERA attachment; white arrows the milling
Next, the try-in of the metallic structure was evaluated, and the ERA attachment presented 4 mm of vertical height observed between the ridge crest and occlusal plane. In addition, it was placed at an appropriate distance from the supporting tissues to allow for hygiene and for appropriate interocclusal distance to involve the ERA attachment/metal housing, the artificial teeth and the acrylic resin of the denture base. The milling and the transfixation (channels) on the lingual surface of the fixed metal crowns were also evaluated (Fig. 4).
Fig. 4.
Bucco-lingual position of the ERA attachment in the center of the teeth. The metallic structure was tried-in and adjusted. The ERA attachment components were positioned with 4 mm of vertical height
After applying the ceramic, hygiene space was again evaluated, and esthetic, phonetic and functional evaluations of the (full contour wax trial set up of the) partial fixed dental prosthesis and maxillary complete denture were conducted. Cementation was not performed at this time [8]. The next step was to clinically evaluate the partial fixed dental prosthesis and the metallic framework of the RPD (Remanium GM 380; Dentaurum, Pforzhein, Germany) at the same time. The proper fitting of the removable framework was evaluated in the milled areas of the partial fixed dental prosthesis (Fig. 5). Cementation of a partial fixed dental prosthesis is an important critical step because slightly incorrect positioning of the crowns can result in improper fitting of the removable partial denture to the ERA attachments, causing premature loss of retention or possible need to re-index the patrix housing to be aligned properly with the ultimate position of the post cementation orientation of the matrix on the fixed restorations; therefore, both the crowns and the removable framework had to be inserted and cemented simultaneously. A self-adhesive resin cement (RelyX U100; 3M ESPE, St. Paul, MN) was used, and the crowns were kept in position with gentle digital pressure until cement overflow. The excess cement was carefully removed, and a recommendation was given to the patient not to remove the partial denture during the first 24 h following cementation, to prevent crown dislodgement.
Fig. 5.

Occlusal view of the metal framework. The mandibular incisor crowns were milled to allow a proper fitting of the removable framework
The laboratory inserted a black (an ERA laboratory processing) component (SternGold Implamed; SP, Brazil) to maintain the space necessary for the mpatrix ERA attachment during polymerization. The black component was then replaced with a white least retentive ERA patrix, after 1 week of clinical service to guarantee perfect interface of the prosthesis to the teeth and soft tissues. Next, clinical evaluation of the fixed prostheses, including the matrix and matrix for the ERA attachments, with the white retentive component was conducted at this time, as well as obtaining the patient’s opinion regarding the rehabilitation (Figs. 6, 7).
Fig. 6.
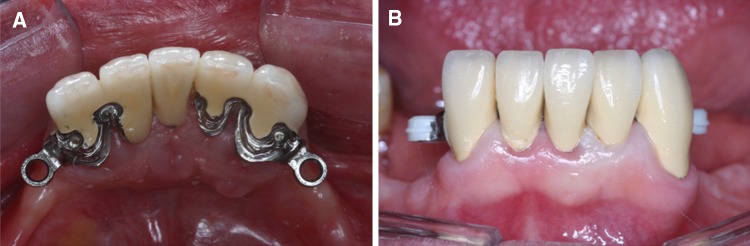
Fixed prostheses including the female ERA attachment (a) and male ERA attachment with white nylon retentive component (b)
Fig. 7.

Final facial view
Discussion
Different treatment options should be offered to patients, considering local and systemic factors such as the patient’s general health status, local risk factors, total treatment cost and time, status of remaining teeth as well as their periodontal support and bone health [2–5, 9].
The present clinical report described a treatment option for which surgical management was deemed contraindicated. Rehabilitation with an RPD, without clasps instead using ERA attachments, and with splinted crowns on all but one the remaining mandibular anterior teeth, milled and transfixed in metal on the lingual surface, could be an option for patients with blood disorders or poor bone condition, for whom the surgical placement of implants is contraindicated. This technique is innovative since the distribution of load between abutment teeth and resiliency of the tissue overlying the residual edentulous ridge is balanced because the transfixation on the lingual surface of the fixed metal is not rigid. The removable partial denture only fits into of the fixed partial denture without overloading the system. Moreover, the resilience of this system provides stress release because significant rotation of the attachment is allowed, thus reducing the load concentrated on the RDP and teeth and making it suitable for patients with inadequate periodontal status [6, 10, 11].
The ERA system includes retention elements in 4 colors representing levels of resiliency. The white component provides the least retention; however, it is the most widely used component because its retention is sufficient to retain the RPD [11, 12], and for this reason, this component was selected for the case presented. If after a period of time, the prosthesis requires increased retention, the component could be changed using a less resilient replacement patrix. Fortunately, in this case, 1 year after the first evaluation, no maintenance was required, and the same component was kept in place after 3 years of follow-up. Long-term studies have shown better clinical performance of RPDs retained with attachments, compared to RPDs retained with clasps [10, 13]. After the completion of treatment for this patient with a 3-year follow-up appointment (Fig. 8), the quality and durability of the attachments (Fig. 9), adequate retention and stability, preservation of the abutment teeth demonstrating reasonable periodontal support and patient satisfaction, reported together, can be considered indicators of success [14–16]. It is important to emphasize that the patient’s ability to masticate was improved, which is strongly dependent on the maxillary and mandibular removable prostheses’ stability and retention contributing to positively influencing oral health-related quality of life [17, 18]. Adaptation to the adjacent tissues, the quality of the underlying bone, good occlusal design and the number and location of the remaining teeth, as well as the prosthesis design, are good predictors of stability [19].
Fig. 8.

Removable partial denture and complete maxillary denture in position after 3-year follow-up
Fig. 9.

Male ERA attachment in the removable partial denture after 3-year follow-up
The main advantage of RPDs retained with resilient attachments is reduction of the incidence of occlusal load on mandibular anterior teeth that present with poor bone height as a result of the dissipation of stress on the abutment’s adjacent teeth to the alveolar ridge [11]. In addition, milled crowns direct forces in a more axial direction, and the transfixation of the fixed crowns provides considerable stability and durability, not requiring adjustments [6].
This system presents a low failure rate, but it is important to note that when there is a loss of retention, it is necessary to replace the resilient matrix. An oral self-care program that includes the use of fluoridated toothpaste, effective biofilm removal and regular check-ups is mandatory [19].
Conclusion
Thus, this treatment modality, involving an ERA system and transfixation in fixed crowns, is an effective treatment and can be indicated as a clinical alternative for edentulous and partially edentulous patients with systemic disorders or for patients in economic situations that might preclude implant-based rehabilitation.
References
- 1.Hobkirk JA, Abdel-Latif HH, Howlett J, Welfare R, Moles DR. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-stabilized complete mandibular dentures: a case–control study (part 2) Int J Prosthodont. 2009;22:13–19. [PubMed] [Google Scholar]
- 2.Hwang D, Wang HL. Medical contraindications to implant therapy: part I: absolute contraindications. Implant Dent. 2006;15:353–360. doi: 10.1097/01.id.0000247855.75691.03. [DOI] [PubMed] [Google Scholar]
- 3.Hwang D, Wang HL. Medical contraindications to implant therapy: part II: relative contraindications. Implant Dent. 2007;16:13–23. doi: 10.1097/ID.0b013e31803276c8. [DOI] [PubMed] [Google Scholar]
- 4.Bornstein MM, Cionca N, Mombelli A. Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implant. 2009;24:12–27. [PubMed] [Google Scholar]
- 5.Martin W, Lewis E, Nicol A. Local risk factors for implant therapy. Int J Oral Maxillofac Implant. 2009;24:28–38. [PubMed] [Google Scholar]
- 6.Becerra G, McEntee MA. Classification of precision attachments. J Prosthet Dent. 1987;3:322–327. doi: 10.1016/0022-3913(87)90049-7. [DOI] [PubMed] [Google Scholar]
- 7.Davidoff SR, Davis RP. The ERA implant-supported overdenture. Compend Contin Educ Dent. 1995;16:512–516. [PubMed] [Google Scholar]
- 8.Marafie Y, Nelson SK. Retention of an extracoronal resilient at attachment. J Prosthet Dent. 2008;99:412–413. doi: 10.1016/S0022-3913(08)60094-3. [DOI] [PubMed] [Google Scholar]
- 9.Brennan DS, Spencer AJ. Longitudinal comparison of factors influencing choice of dental treatment by private general practitioners. Aust Dent J. 2006;51:117–123. doi: 10.1111/j.1834-7819.2006.tb00414.x. [DOI] [PubMed] [Google Scholar]
- 10.Owall B. Precision attachment retained removable partial dentures: part 1. Technical long term study. Int J Prosthodont. 1991;4:249–257. [PubMed] [Google Scholar]
- 11.Wang H, Zhang Y, Yao D, Chen J. Effects of rigid and nonrigid extracoronal attachments on supporting tissues in extension base partial removable dental prostheses: a nonlinear finite element study. J Prosthet Dent. 2011;105:338–346. doi: 10.1016/S0022-3913(11)60066-8. [DOI] [PubMed] [Google Scholar]
- 12.Chen IC, Brudvik JS, Mancl LA, Rubenstein JE, Chitswe K, Raigrodski AJ. Freedom of rotation of selected overdenture attachments: an in vitro study. J Prosthet Dent. 2011;106:78–86. doi: 10.1016/S0022-3913(11)60099-1. [DOI] [PubMed] [Google Scholar]
- 13.Owall B. Precision attachment-retained removable partial dentures: part 2. Long-term study of ball attachments. Int J Prosthodont. 1995;8:21–28. [PubMed] [Google Scholar]
- 14.Mollov ND, Lindauer SJ, Best AM, Shroff B, Tufekci E. Patient attitudes toward retention and perceptions of treatment success. Angle Orthod. 2010;80:468–473. doi: 10.2319/102109-594.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maia NG, Normando D, Maia FA, Ferreira MA, Do Socorro Costa Feitosa Alves M. Factors associated with long-term patient satisfaction. Angle Orthod. 2010;80:1155–1158. doi: 10.2319/120909-708.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brennan M, Houston F, O’Sullivan M, O’Connell B. Patient satisfaction and oral health-related quality of life outcomes of implant overdentures and fixed complete dentures. Int J Oral Maxillofac Implant. 2010;25:791–800. [PubMed] [Google Scholar]
- 17.Gilbert GH, Meng X, Duncan RP, Shelton BJ. Incidence of tooth loss and prosthodontic dental care: effect on chewing difficulty onset, a component of oral health-related quality of life. J Am Geriatr Soc. 2004;52:880–885. doi: 10.1111/j.1532-5415.2004.52253.x. [DOI] [PubMed] [Google Scholar]
- 18.Inoue M, John MT, Tsukasaki H, Furuyama C, Baba K. Denture quality has a minimal effect on health-related quality of life in patients with removable dentures. J Oral Rehabil. 2011;38:818–826. doi: 10.1111/j.1365-2842.2011.02222.x. [DOI] [PubMed] [Google Scholar]
- 19.Ettinger RL, Qian F. Abutment tooth loss in patients with overdentures. J Am Dent Assoc. 2004;135:736–739. doi: 10.14219/jada.archive.2004.0300. [DOI] [PubMed] [Google Scholar]




