Abstract
The restorative management of tooth surface loss is highlighted through the presentation of two advanced cases of dental erosion. On presentation, the causes of the dental erosion in both patients had been previously diagnosed and stopped. The first patient was a 67 year old with intrinsic erosion and an element of attrition where a multidisciplinary approach was used. The other, a 17 year old patient with extrinsic erosion managed via adhesive restorations. Adhesive techniques are a relatively simple, effective and conservative method for the treatment of dental erosion. The two treatment modalities (conventional versus contemporary) are compared and discussed.
Keywords: Tooth surface loss, Erosion, Full mouth rehabilitation, GORD
Introduction
Tooth surface loss (TSL) is becoming an increasingly common problem as more patients retain their teeth for longer and consume more acidic foods and beverages. The aetiology is usually multifactorial encompassing attrition, abrasion and erosion [1–3]. The prevalence of dental erosion, presented in the two cases here, is now reported in all age groups [4]. Dental erosion is the loss of mineralised tooth structure (enamel and subsequently dentine) by frequent presence of acidic agents [5]. Erosion can be either extrinsic or intrinsic in origin. Extrinsic sources of acid include carbonated drinks and fresh fruit juices. Gastric juice is the main intrinsic factor [6]. There are a number of intrinsic causes for dental erosion that include gastro-oesophageal reflux disease (GORD), eating disorders and pregnancy morning sickness. GORD is a relatively common gastrointestinal disorder in Western society [7]. It has been found that gastric juice had a greater potential per unit time for erosion than a carbonated drink [8]. The refluxed material may reach the cervical oesophagus, pharynx and oral cavity [9]. A number of studies have shown a strong association between GORD and dental erosion [9, 10]. Enamel dissolution occurs at a critical pH of 5.5 [11–13]. Gastric acid has a pH < 2 which is more acidic than the critical pH of enamel, and demineralization can occur.
There is evidence which suggests that erosion can potentiate damaging effects of dental attrition in certain situations [14]. Damage can be so severe that it can progress to pulpal exposure. In vitro studies indicate that dental attrition in an erosive environment (low pH) will result in greater enamel–enamel breakdown, when subjected to the same force, compared to that in a neutral environment (water/saline) [15]. The pH value required for this is associated with that of acid regurgitation of patients with gastric reflux (pH 1.2) [16]. When the enamel is exposed to a less acidic erosive agent such as acetic acid (pH 3.0), the relative enamel breakdown during attrition is significantly less [17].
There are 4 reported groups at risk of dental erosion [18]. These are adolescent males due to their large consumption of acidic beverages, adolescent females suffering from bulimia, patients with GORD and elderly patients suffering from xerostomia and taking medication affecting salivary flow. If a patient fits into a risk group, it is crucial to determine the aetiology of the erosion [19]. With intrinsic erosion, TSL is generally present on the palatal aspects of the maxillary tooth and occlusal and buccal surfaces of the mandibular teeth. In extrinsic erosion, TSL is mainly on the labial surface of anterior teeth and buccal and occlusal surfaces of the mandibular posterior teeth.
The treatment of patients with dental erosion ranges from preventative to fixed prosthodontic management [20]. The multifactorial nature of the disease creates complex treatment challenges. Long term success is affected by the patient’s oral environment and how diet, medication and lifestyle modify the oral cavity [21]. New techniques and advances in micromechanical adhesion have enabled less invasive, more conservative options particularly in younger patients [22]. The use of direct and indirect resin composite restorations for the treatment of younger adults and adolescents is often a preferred option [23]. The earlier the erosion is detected, the sooner preventative strategies can be put in place along with simple restorations. In the more advanced cases, treatment involving a full mouth reconstruction may be the only option.
Two cases are presented here, both fit into a risk group. One, in a 67 year old male with a history of GORD resulting in dental erosion together with attrition. The other a 17 year old male with a history of carbonated drink consumption exhibiting severe erosion particularly affecting his upper anterior teeth.
Case Reports
Case 1
A 67 year old, male patient, complaining of progressive wear of his teeth which had deteriorated over the last 15 years was referred to the Restorative Department of a dental teaching hospital. He was concerned about the appearance of his teeth and generalized sensitivity. Clinical examination revealed severe TSL affecting the majority of his teeth. The patient exhibited a class III incisor relationship as he was posturing forward due to the severe TSL. Initial photographs (Fig. 1a–d) as well as radiographs (Fig. 2a, b) were taken. He had normal bone levels and there was no tenderness or crepitus at either temporomandibular joint. The patient reported a history of excessive alcohol intake (beer) between 120 and 140 units/week with symptoms of GORD for several years. He required antacids and ranitidine for relief of these symptoms. The diagnosis of GORD had been confirmed by a Gastroenterologist. The patient had reduced his alcohol consumption 10 years earlier and on presentation his intake was reduced to 18 units/week. He had lost weight, his symptoms of GORD disappeared and he no longer required medication. The patient’s general dental practitioner had monitored his wear condition for several years however, the patient was unhappy with the appearance of his teeth.
Fig. 1.
a Pre-operative buccal view. b Pre-operative maxillary occlusal view. c Pre-operative mandibular occlusal view. d Initial smile line
Fig. 2.
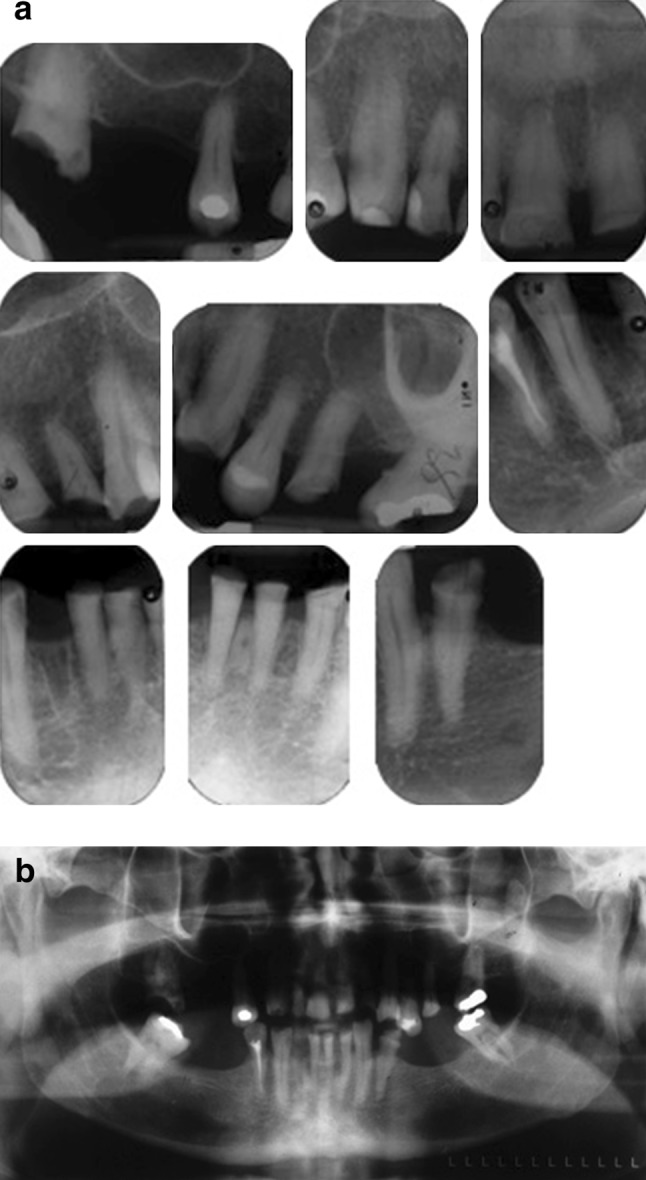
a Periapical radiographs. b Odontopantomogram
A diagnosis of TSL, which appeared to have an erosive origin, with superimposed attrition due to night time parafunction was made. Some teeth were affected by TSL more than others and several teeth had over erupted. In order to conserve as much tooth tissue as possible, it was decided to provide a combination of direct (composites) and indirect (metal ceramic and full gold crowns) restorations at an increased occlusal vertical dimension (OVD). The treatment was carried out over two phases.
Phase I: Diagnostic
Preoperative impressions of both arches were made using irreversible hydrocolloid material. Pre-contact jaw registration was recorded on the retruded arc of closure using moyco extra-hard beauty wax reinforced with aluminium foil. A set of study casts were set up in the retruded contact position (RCP) and a diagnostic wax up made (Fig. 3). Vacuum formed matrices, for use in fabrication of chair side provisional restorations, were also made using duplicate wax ups.
Fig. 3.

Diagnostic wax up
Phase 2: Restorative Treatment
Elective endodontic treatment was carried out on the 22 as a post and core were needed for the tooth. Crown lengthening was carried out on the 24 and 25. Periapicals of the 24 and 25 revealed moderate bone loss and therefore only soft tissue (about 4–5 mm) was removed on the buccal and palatal aspects of the teeth (Fig. 4). The soft tissues were allowed to heal over a period of 3 months. On the review appointment, protemp (Protemp ™ Temporization material, 3 M ESPE) temporaries were made over existing teeth to help visualize the final result. The patient was happy with the appearance and the increased OVD appeared satisfactory (Fig. 5).
Fig. 4.

Soft tissue surgery 24, 25
Fig. 5.

Protemp “try-in”
In order to establish occlusal holding stops, the laboratory made matrices were used to provide direct composites on 17, 13, 23, 27, 34, 43, 44 at the increased OVD planned on the diagnostic wax up. The 22 was prepared for a post and core. On a subsequent visit, the 22 post and core was fitted and the 12, 11, 21, 22, 32, 31, 41 prepared for metal ceramic crowns. The 43 was prepared for a fixed metal ceramic cantilever bridge to replace the 42. Maxillary and mandibular full arch addition cured silicone impressions, facebow and interocclusal records were made. Subsequently, anterior laboratory made provisional crowns were fitted (Fig. 6). The occlusion was checked and RCP and ICP were coincident and only minor adjustments were made to the occlusion. After a period of 2 months, the final metal ceramic crowns were cemented on the 12, 11, 21, 22, 33, 32, 31, 41, 42, 43 using Rely X™ (Dental Cement Products, 3 M ESPE Dental Products). Metal ceramic crown preparations were carried out on the 24, 25 and the crowns were subsequently fitted.
Fig. 6.

Anterior laboratory made provisional restorations
Buccal composites were built up on the 13 and 14. Composite build ups were also carried out on 23, 34 and 44. Finally the 17, 27, 37 and 47 were prepared for full gold crowns and subsequently fitted (Fig. 7a, b). The patient was fitted with a stabilization splint to wear at night and was very happy with the final result (Fig. 8a, b). Figure 9 shows the patient at his 2 year review. He did not report any problems and was wearing his stabilization splint as was evidenced by occlusal wear on the splint.
Fig. 7.

a Post-operative maxillary occlusal view. b Post-operative mandibular occlusal view
Fig. 8.

a, b Post-operative right and left lateral views respectively
Fig. 9.

Buccal views at 2 year review
Case 2
A 17 year old patient, also referred to a teaching hospital, was complaining of the appearance of his anterior teeth due to erosion from a history of excessive intake of carbonated drinks (Coca Cola). On presentation, he had completely stopped his intake of carbonated drinks over the previous 12 months. Prior to that, however, he consumed at least one litre of carbonated drinks per day. He presented with severe wear of his upper teeth (Fig. 10) together with wear affecting the occlusal surfaces of his posterior teeth. He had excellent oral hygiene and in addition to brushing with a fluoride toothpaste twice daily, he was also using a fluoride mouth rinse.
Fig. 10.

Pre-operative buccal view
A wax up was produced from study models in RCP (RCP and ICP were coincident). From the wax up, anterior restorations were fabricated from protemp (Fig. 11) and tried in the mouth. This helped to determine the amount of opening required for the case. The patient was happy with the general appearance. With the fabricated temporaries in place, an addition cured silicone bite registration material (Futar D Bite Registration material, Kettenbach LP) was placed in between the posterior teeth which acted as silicone indices (Fig. 12).
Fig. 11.

Protemp “try-in”
Fig. 12.

Silicone indices in place increasing the OVD
The first stage of the treatment was the fabrication of resin bonded crowns on 13, 12, 11, 21, 22, 23. Minimal preparations were required on the anterior teeth due to the extent of the TSL. A maxillary addition cured silicone impression was made along with a face-bow record. The silicone indices were sent to the laboratory to replicate the opening determined by the wax up. Following bonding of the anterior crowns (Caliber R Esthetic Resin Cement, Dentsply International), minimal preparations were done (establishing a finish line only) on the 15, 14, 24, 25, 35, 34, 44, 45 for ceramic onlays. The 17, 16, 26, 27 were prepared for gold caps. On a subsequent visit the ceramic onlays were bonded into place (Caliber R Esthetic Resin Cement, Dentsply International) along with the gold caps (Panavia ™ F 2.0, Dental Dual-Cured Adhesive Resin Cement, Kuraray America, Inc.). The patient was very happy with the final outcome (Fig. 13a, c).
Fig. 13.

a Post-operative buccal view. b Post-operative maxillary occlusal view. c Post-operative mandibular occlusal view
Discussion
Management of TSL ranges from prevention to full mouth rehabilitation. The decision on treatment modality depends on the severity of the TSL on presentation. The two cases presented here show late presentation of dental erosion. Although both patients had a history of dental erosion, the erosion was, however, no longer active in both cases. Before operative treatment commences, it is important that the cause of the erosion is known and preferably stopped.
There are a number of approaches that can be followed in the treatment of tooth wear cases. These will depend largely on clinical crown heights available and interocclusal space present [23]. When wear is diagnosed early, preventative measures can be employed without the need for intervention. In severe cases, such as the two presented here, the main difficulties encountered in providing crowns are the reduced clinical height and the lack of interocclusal space available for restorations. These two features were present in both patients and the damage to their dentition was particularly apparent in the anterior maxillary quadrant; often found in dental erosion cases [24].
The 67 year old patient reported a history of GORD. Dental erosion has been found in over 90 % of patients suffering from excessive alcohol intake [10]. In this case as well as the intrinsic dental erosion there would have also been an element of extrinsic erosion as beer has a pH of about 3. He exhibited a loss of occlusal vertical dimension (OVD) and appeared over closed. He had an occlusal plane discrepancy. There were a number of super erupted teeth which further complicated the treatment as these teeth caused occlusal interferences. By increasing the OVD needed to restore function and aesthetics, it also eliminated the occlusal interferences. The restorative material selected to cement the crowns was resin modified glass ionomer as it has relatively good acidic resistance and is not technique sensitive [25]. Adhesive techniques using composite resin material were used to restore a number of teeth which exhibited less severe wear. This was deemed to be the most conservative option and avoided removal of excessive tooth structure.
The 17 year old patient had a history of carbonated drink consumption which he had given up 1 year earlier. The frequency of soft drink consumption is a strong risk factor in the development of dental erosion [26]. There was no loss in his OVD due to dental alveolar compensation. A full mouth rehabilitation was necessary as there was evidence of TSL on his anterior and posterior teeth. All his teeth needed protecting from further TSL and therefore a Dahl approach was deemed inappropriate. An ‘adhesive’ full mouth rehabilitation was provided in this case at an increased OVD. Minimal tooth preparations were made and all margins were kept in enamel. In this way, the patient’s tooth structure was protected and the pulp was not compromised. Conventional crown preparation in a young patient may sometimes result in pulp exposure. For this patient, composite resin was used to cement the anterior and premolar restorations. Composite resin cements have a high acidic resistance and strong bond strength [27]. The patient’s aesthetic requirements were satisfied. The appearance of dentine bonded restorations is superior to that of conventional metal ceramic crowns. Additionally, dentine bonded restorations do not appear to cause darkening of the gingival margins as in the case with metal ceramic crowns.
Satisfactory results were obtained in both cases and the patients were very happy with the final outcomes. Clearly an adhesive dentistry approach is less destructive to tooth tissue and should be used wherever possible, especially in young patients exhibiting dental erosion with no evidence of parafunction. There have been a number of case reports [28, 29] dealing with adhesive restorations in the treatment of dental erosion. There is, however, a dearth of long term clinical trials on the success of full mouth adhesive reconstructions [30]. In spite of the limited number of clinical trials, the treatment provided for the 17 year old patient was deemed most appropriate and it does not preclude him from future maintenance with conventional crowns. A combination of direct adhesive restorations and indirect metal ceramic crowns were provided for the 67 year old patient as he had evidence of erosion as well as attrition. There are many studies which have reported the long term outcome of full mouth rehabilitation with conventional metal crowns [31, 32].
References
- 1.Milosevic A. Toothwear: aetiology and Presentation. Dent Update. 1998;25(1):6–11. [PubMed] [Google Scholar]
- 2.Verrett RG. Analyzing the etiology of an extremely worn dentition. J Prosthodont. 2001;10(4):224–233. doi: 10.1111/j.1532-849X.2001.00224.x. [DOI] [PubMed] [Google Scholar]
- 3.Amaechia BT, Highamb SM. Dental erosion: possible approaches to prevention and control. J Dent. 2005;33(3):243–252. doi: 10.1016/j.jdent.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Grippo JO. Abfractions: a new classification of hard dental tissue lesions. J Esthet Dent. 1991;3:14–19. doi: 10.1111/j.1708-8240.1991.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 5.Gugmore CR, Rock WP. The prevalence of tooth erosion in 12-year old children. Br Dent J. 2004;196:279–282. doi: 10.1038/sj.bdj.4811040. [DOI] [PubMed] [Google Scholar]
- 6.Bartlett DW, Coward PY. Comparison of the erosive potential of gastric juice and a carbonated drink in vitro. J Oral Rehabil. 2001;28:1045–1047. doi: 10.1046/j.1365-2842.2001.00780.x. [DOI] [PubMed] [Google Scholar]
- 7.Dent JE, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54(5):710–717. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Roekel NB. Gastroesophageal reflux disease, tooth erosion and prosthodontic rehabilitation: a clinical report. J Prosthodont. 2003;12(4):255–259. doi: 10.1016/S1059-941X(03)00104-9. [DOI] [PubMed] [Google Scholar]
- 9.Bartlett DW, Evans DF, Anggiansah A, Smith BG. A Study of the Association between gastro-oesophageal reflux and palatal dental erosion. Br Dent J. 1996;181:125–131. doi: 10.1038/sj.bdj.4809187. [DOI] [PubMed] [Google Scholar]
- 10.Robb ND, Smith BGN. Prevalence of pathologic tooth wear in patients with chronic alcoholism. Br Dent J. 1990;169:367–369. doi: 10.1038/sj.bdj.4807386. [DOI] [PubMed] [Google Scholar]
- 11.Zero DT. Etiology of dental erosion–extrinsic factors. Eur J Oral Sci. 1996;104(2):162–177. doi: 10.1111/j.1600-0722.1996.tb00065.x. [DOI] [PubMed] [Google Scholar]
- 12.Birkhead D. Sugar content, acidity and effect on plaque pH of fruit juices, fruit drinks, carbonated beverages and sports drinks. Caries Res. 1984;18:120–127. doi: 10.1159/000260759. [DOI] [PubMed] [Google Scholar]
- 13.Seow WK, Thong KM. Erosive effects of common beverages on extracted premolar teeth. Aust Dent J. 2005;50(3):173–178. doi: 10.1111/j.1834-7819.2005.tb00357.x. [DOI] [PubMed] [Google Scholar]
- 14.Addy M, Shellis RP. Interaction between attrition, abrasion, and erosion in tooth wear. Monogr Oral Sci. 2006;20:17–31. doi: 10.1159/000093348. [DOI] [PubMed] [Google Scholar]
- 15.Kaidonis JA, Richards LC, et al. Wear of human enamel: a quantitative in vitro assessment. J Dent Res. 1998;77(12):1983–1990. doi: 10.1177/00220345980770120601. [DOI] [PubMed] [Google Scholar]
- 16.Mahoney EK, Kilpatrick NM. Dental erosion: part 1. Aetiology and prevalence of dental erosion. NZ Dent J. 2003;99(2):33–41. [PubMed] [Google Scholar]
- 17.Wang X, Lussi A. Assessment and management of dental erosion. Dent Clin North Am. 2010;54(3):565–578. doi: 10.1016/j.cden.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Harpenau LA, Noble WH, Kao RT. Diagnosis and management of dental wear. J Calif Dent Assoc. 2011;39(4):225–231. [PubMed] [Google Scholar]
- 19.Curtis DA, Jayaneetti J, Chu R, Staninec M. Decision-making in the management of the patient with dental erosion. J Calif Dent Assoc. 2011;39(4):259–265. [PubMed] [Google Scholar]
- 20.Shaw L, Smith AJ. Dental erosion-the problem and some practical solutions. Br Dent J. 1999;186(3):115–118. doi: 10.1038/sj.bdj.4800037. [DOI] [PubMed] [Google Scholar]
- 21.Meyers IA. Diagnosis and management of the worn dentition: risk management and pre-restorative strategies for the oral dental environment. Ann R Australas Coll Dent Surg. 2008;19:27–30. [PubMed] [Google Scholar]
- 22.Al-Salehi SK, Dooley K, Harris IR. Restoring function and aesthetics in a patient previously treated for amelogenesis imperfecta. Eur J Prosthodont Restor Dent. 2008;17(4):170–176. [PubMed] [Google Scholar]
- 23.Abduo J, Lyons K. Clinical considerations for increasing occlusal vertical dimension: a review. Aust Dent J. 2012;57(1):2–10. doi: 10.1111/j.1834-7819.2011.01640.x. [DOI] [PubMed] [Google Scholar]
- 24.Vailati F, Belser UC. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 1. Eur J Esthet Dent. 2008;3(1):30–44. [PubMed] [Google Scholar]
- 25.Honorio HM, Rios D, Francisconi LF, Magalhaes AC, Machado MA, Buzalaf MA. Effect of prolonged erosive pH cycling on different restorative materials. J Oral Rehabil. 2008;35:947–953. doi: 10.1111/j.1365-2842.2008.01856.x. [DOI] [PubMed] [Google Scholar]
- 26.Jensdottir T, Arnadottir IB, Thorsdottir I, Bardow A, Gudmundsson K, Theodors A, Holbrook WP. Relationship between dental erosion, soft drink consumption, and gastroesophageal reflux among Icelanders. Clin Oral Investig. 2004;8:91–96. doi: 10.1007/s00784-003-0252-1. [DOI] [PubMed] [Google Scholar]
- 27.Shabanian M, Richards LC. In vitro wear rates of materials under different loads and varying pH. J Prosthet Dent. 2002;87:650–656. doi: 10.1067/mpr.2002.125609. [DOI] [PubMed] [Google Scholar]
- 28.Guldag MU, Buyukkaplan US, Yetkin AYZ, Katirci G. A multidisciplinary approach to dental erosion. A case report. Eur J Dent. 2008;2:110–114. [PMC free article] [PubMed] [Google Scholar]
- 29.Vailati F, Vaglio G, Belser UC. Full mouth minimally invasive adhesive rehabilitation to treat severe dental erosion: a case report. J Adhes Dent. 2012;14(1):83–92. doi: 10.3290/j.jad.a21852. [DOI] [PubMed] [Google Scholar]
- 30.Attin T, Filli T, Imfled C, Schmidlin PR. Composite vertical bite reconstruction in eroded dentitions after 5.5 years: a case series. J Oral Rehabil. 2012;39(1):73–79. doi: 10.1111/j.1365-2842.2011.02240.x. [DOI] [PubMed] [Google Scholar]
- 31.Van Nieuwenhuysen JP, D’hoore W, Carvalho J, Quist V. Long-term evaluation of extensive restorations in permanent teeth. J Dent. 2003;31:395–405. doi: 10.1016/S0300-5712(03)00084-8. [DOI] [PubMed] [Google Scholar]
- 32.Valderhaug J. A 15 year clinical evaluation of fixed prosthodontics. Acta Odontol Scand. 1991;49:35–40. doi: 10.3109/00016359109041138. [DOI] [PubMed] [Google Scholar]



