Abstract
Complicated crown fractures are a common outcome of dental trauma. Various treatment options are available for consideration. The preferred choice of treatment though, is determined by multiple factors associated with the nature of trauma itself. This case report highlights the management of a cervical crown fracture by modifying the clinical technique of an existing concept of the “Biologic Post and Core” and integrating it with current advances in adhesive technology, with an intention for preservation and reinforcement of residual tooth structure. The clinical success observed during subsequent patient recall has given reason for optimism in considering the employed method as a possible alternative to address this area of prosthetic concern.
Keywords: Coronal fracture, Biologic foundation restoration, Natural tooth post and core
Introduction
Traumatized anterior teeth require immediate attention in terms of function and aesthetics as there is a social and psychological effect on the patient [1]. Several factors are to be taken into consideration during the management of coronal fractures like the vitality of pulp, extent of fracture, type of injury, the dental structures involved, ability to restore the residual tooth/retrieve the tooth fragment, occlusion and aesthetics, and lastly patient compliance [2]. Even with all the advances in the field of adhesive dentistry, no such restorative material exists that can reproduce the aesthetic and functional needs as well as the natural dentition.
Chosack and Eidelman [3] were the pioneers in the concept of attaching tooth fragments in their natural form over a cast metal post.
In clinical situations where the autogenous bonding of the tooth fragment may not be possible as it may be lost or irreversibly damaged, the possibility of use of fragments obtained by means of extracted teeth, a technique known as homogenous bonding or “Biological Restoration” was first highlighted by Santos and Bianchi [4] in 1991 with successful results.
Ever since several case reports have demonstrated the benefits of the use of natural tooth structure in its entirety or as fragments providing superior aesthetics, natural color and anatomic form, preservation of sound tooth structure, cost effectiveness and elimination of the need for complex restorative materials and techniques [5–10].
This case report presents the successful placement of a natural post and core foundation using a modification of the existing procedures [11] wherein a natural tooth in combination with adhesive techniques was utilized to restore a fractured maxillary canine, where autogenous reattachment of the coronal fragment had previously failed.
Case Report
An 18 year old male patient reported to the Department of Conservative Dentistry and Endodontics with a complaint of a cracked and movable fragment of the left maxillary canine. The patient gave a history of trauma 2 weeks back. He had visited a private dentist who seemed to have reattached the fractured fragment. However the fragment had become mobile and the patient was experiencing pain and sensitivity in the involved tooth.
On clinical examination, the involved tooth showed an oblique complicated crown root fracture extending supragingivally from the palatal side to the buccal aspect deep subgingivally involving the enamel cementum junction. The fractured fragment was separated from the rest of the crown with the coronal fragment still attached to the buccal gingiva. Clinically the pulp was exposed (Fig. 1a).
Fig. 1.
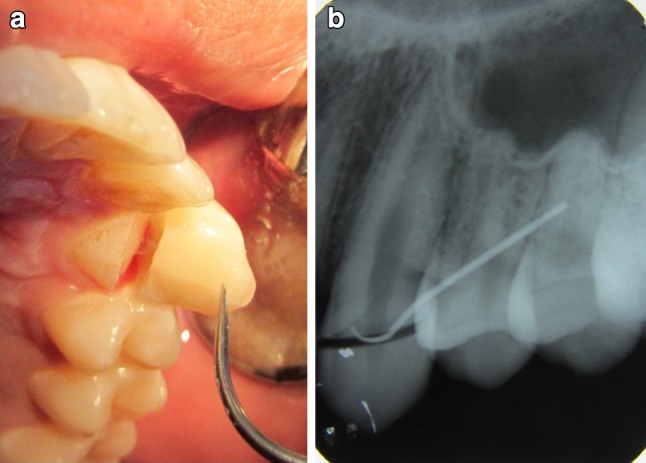
a Pre operative view of fractured maxillary left canine. b Diagnostic radiograph of fractured maxillary left canine
Intraoral periapical radiographic examination confirmed the clinical findings related to the trauma showing a clear oblique fracture line. Slight widening of the apical periodontal ligament space was evident. (Fig. 1 b).Several treatment options of post and core were presented including that of the biologic post core. A written informed consent from the patient was obtained to exercise the option of a biologic post and core. The institutional review board was appraised of the clinical option being planned and an ethical clearance was sought in this regard prior to initiating treatment.
Under local anaesthesia and rubber dam isolation, cleaning and shaping of the root canal followed by obturation with gutta percha and resin sealer (AH Plus, Dentsply, Konstanz, Germany) using the lateral condensation technique was completed. The coronal root canal filling material was removed to the apical one-third of the root.
The residual coronal tooth structure was prepared to receive the biologic post and core. In order to obtain a visual of the internal root canal anatomy of the fractured canine, a direct wax pattern impression of the same was taken only to serve as a three dimensional guide for the root preparation of the donated extracted tooth (Fig. 2a).
Fig. 2.

a Direct Wax pattern compared to Autoclaved donor tooth. b Clinical view of biologic foundation restoration
A freshly extracted tooth, obtained from the Department of Oral and Maxillofacial Surgery Clinic of the same institution, presenting the approximate colour, root form and dimensions of the wax pattern was then selected and stored in 0.1 % thymol solution. The donor tooth belonged to a healthy individual of 20 years of age with no known medical history. Informed consent from the donor patient was obtained. The tooth was extracted for orthodontic reasons. In this case it was a mesiodens. The donor tooth was thoroughly scaled and cleared of all soft tissues and periodontal remnants. The tooth was then autoclaved using the standardised autoclaving procedures of 121 °C, for 30 min as suggested by previous literature [12].
Root canal therapy was carried out with new unused set of burs and files. The tooth was obturated with Gutta percha and resin sealer (AH Plus, Dentsply, Konstanz, Germany) and allowed to set overnight under sterile and humid (37 °C) conditions. The following day the root was shaped minimally to the approximate shape of the wax pattern to function as a natural post using a new crown preparation kit (Shofu Inc, Kyoto, Japan), under constant hydration to avoid breakage and verified with radiograph. There was no opportunity given to the tooth to be in a dehydrated state. The prepared biologic post was cemented using dual cure resin (Fig. 2b) (Calibra, Dentsply Caulk, Milford, DE, USA).
Composite (Ceram X Duo,Dentsply,UK) was used for reconstructing and shaping at the neck of the core to seal any gaps and eliminate minute undercuts (Fig. 3a, b).Due to the low socio economic status of the patient refused an all ceramic crown. A porcelain fused to metal crown preparation was done preserving as much of the coronal tooth structure as possible in order to enable the axial walls of the crown to externally brace the tooth (Fig. 4). Retraction cord (UltraPack #00,Ultradent,Jodan,UT, USA) was placed to displace the gingival tissues followed by an addition silicone impression (Aquasil Ultra, Dentsply, USA).
Fig. 3.
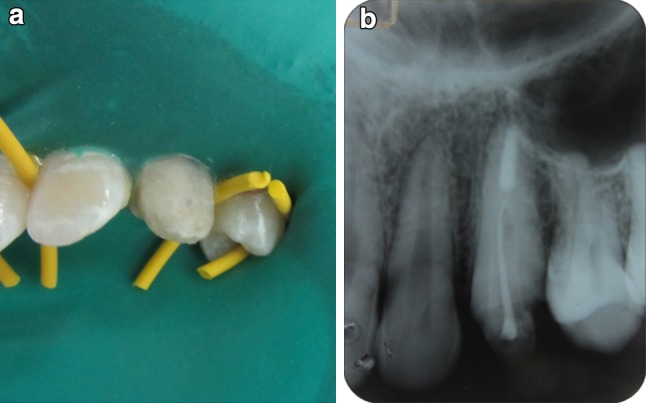
a Clinical view of core build up with composite. b Post cementation radiograph of biologic foundation restoration
Fig. 4.

Clinical view of prepared core
Post operative clinical photographs and radiographs were taken (Fig. 5a–c). 1 year recall radiograph is presented (Fig. 6).
Fig. 5.
a, b, Clinical labial and palatal view of cemented crown. c Radiographic view after crown cementation
Fig. 6.
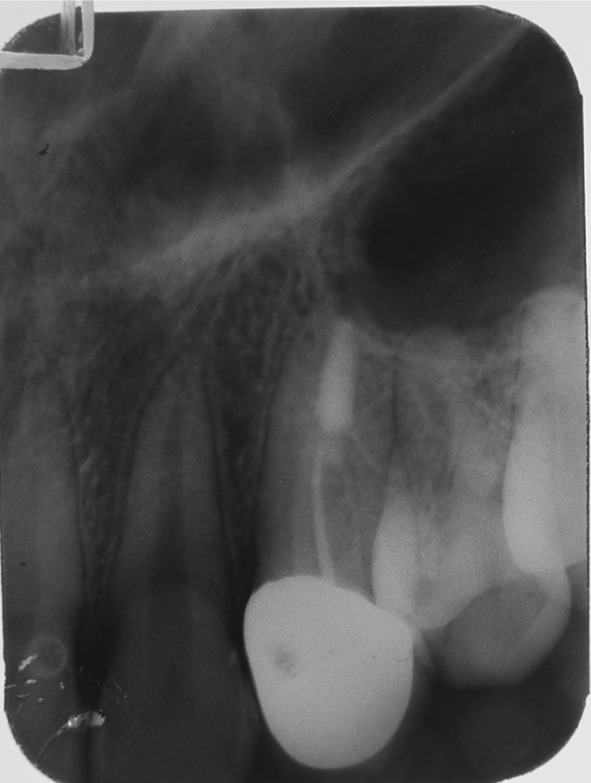
Radiographic view (1 year follow up)
Discussion
The most common type of traumatic injury affecting the permanent dentition is a crown fracture especially in the anterior teeth [13]. In such clinical situations the traditional forms of management range from the more conservative approach of autogenous reattachment of the crown fragment to that of the post and core system. Literature shows that the survival rates for the former are good [2]. However, in this case the reattachment was a failure, The function of a post is to increase the surface area for resistance and retention of the coronal fragment and transmit and distribute occlusal forces to the apical area of the remaining root. However, root fracture is the most common form of failure associated with teeth restored with metal posts due to their lack of resiliency in comparison to tooth structure [14]. Remaining dentin thickness is a critical factor in the resistance of the dentin/root restorative complex during function [15]. Fibre posts are more flexible in comparison to metal posts and result in better stress distribution along the root thereby resulting is lesser failures [16].
In this case report, natural tooth substance or more appropriately, “A biological foundation restoration” has been used as an alternative to the conventional post and core.
Biological restorations both autogenous and homogenous not only mimic the missing part of the oral structures, but are also biofunctional [17]. This concept allows for the preservation of sound tooth structure and provides excellent aesthetics below all ceramic crowns and has low cost [18]. In addition being homogenous in nature, its similarity in elasticity to that of surrounding dentin would allow for a more uniform distribution of stress to the apical region [19–21].
A few reported cases utilizing dentin as a post material have shown successful outcomes [5, 7–10, 19–21]. These claims have been substantiated with in vitro and in vivo studies that concluded that teeth restored with dentin posts exhibited equal or better fracture resistance than those restored with fibre reinforced composite posts [22, 23] and clinical performance of biological post and core and intracanal reinforced composite were comparable [24].
Due to similar bonding structures, the cementing medium creates a type of single unit or a monoblock effect where the materials are compatible with each other [25]. Also since they are made up of the same natural material, they do not cause stress to the dentin in the manner that is observed with synthetic post core systems [19, 20].
In this case the donor tooth was received from a healthy individual of 20 years of age group extracted for orthodontic reasons with no known medical of familial history. The donor tooth was sterilized by steam autoclaving at 121 °C for 30 min at 15 lbs psi as recommended by Kumar et al. [12]. Furthermore this sterilization protocol did not significantly alter the functional characteristics of the teeth with respect to bonding [26, 27].
The preferred material would have been an all ceramic prosthesis. The natural colour and structure of the biological core would add to the highest aesthetics and optimum bonding with enamel as opposed to a synthetic core. However the patient remained non compliant due to financial reasons.
The newer dual adhesive systems have the advantage of complete polymerisation and filling up any possible gaps existing at tooth post core interface.
The biologic post and core concept can be applied in clinical situations such as excessive loss of coronal tooth structure, large irregularly shaped canals and orifice and overzealous preparation of the root canal.
Disadvantages of the biological restoration technique using an intact natural tooth exist. There is difficulty in obtaining teeth with the required coronal dimensions and characteristics. The technique has its applications limited to anterior teeth. A thorough medical history of the donor patient should be carried out to rule out the possibility of any medical issues that may contradict the placement of the donor tooth in the recipient patient. Also acceptance by the patient to receive a tooth from another person, which can be overcome by emphasising the techniques of sterilization applied [25].
To conclude, this case report opens an introductory avenue in support of the clinical implications of using an intact natural tooth substance as a post and core.
When comparing the costs of intraradicular post core systems, the biological post and core foundation offers a cost effective treatment option using recycled natural tissue which would otherwise been wasted. Successful outcome of this case and similar clinical cases previously cited should ignite the need for human tooth banks in dental institutions and an increased focus on stricter sterilization protocols to ensure that all biosecurity standards are met.
Further long term studies are needed however to assess adhesion, fracture resistance and clinical outcome of this procedure to fully comprehend the benefits of this technique and make it a more acceptable practice among dental clinicians and patients at large.
References
- 1.Hamilton FA, Hill FJ, Holloway PJ. An investigation of dento alveolar trauma and its treatment in an adolescent population. Part 1: the prevalence and incidence of injuries and the extent and adequacy of treatment received. Br Dent J. 1997;182:91–95. doi: 10.1038/sj.bdj.4809313. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen FM, Rindom JL, Mnksgaard EC, Andreasen JO. Bonding of enamel dentine fractures with gluma and resin. Endod Dent Traumatol. 1986;2:1–4. doi: 10.1111/j.1600-9657.1986.tb00117.x. [DOI] [PubMed] [Google Scholar]
- 3.Chosak A, Eidelman E. Rehabilitation of a fractured incisor using patient’s natural crown: a case report. J Dent Child. 1964;31:19–21. [Google Scholar]
- 4.Santos J, Bianchi J. Restoration of severely damaged teeth with resin bonding systems. Quintessence Int. 1991;22:611–615. [PubMed] [Google Scholar]
- 5.Bothelo AM, Tavano K, Correa-Faria P, Morato L, Viana MR. Esthetic functional recovery of permanent posterior tooth using autogenous biological restoration. J Indian Soc Pedod Prev Dent. 2012;30:333–336. doi: 10.4103/0970-4388.108934. [DOI] [PubMed] [Google Scholar]
- 6.Durkan RK, Ozel MB, Celik D, Bagis B (2008) The restoration of a maxillary central incisor fracture with the original crown fragment using a glass fibre-reinforced post: a clinical report. Dent Traumatol 24(6):e71-e75 [DOI] [PubMed]
- 7.Grewal N, Reeshu S. Biological restorations: an alternative esthetic treatment for restoration of severely mutilated primary dentition. Int J Clin Pediat Dent. 2008;1:42–47. doi: 10.5005/jp-journals-10005-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hegde V, Kokate S, Shah R. Tooth within a tooth; restoration of maxillary central incisors using dentin posts: case reports. Baba Farid Univ Dent J. 2012;3(1):125–129. [Google Scholar]
- 9.Mandroli PS. Biologic restoration of primary anterior teeth: case report. J Indian Soc Pedod Prev Dent. 2003;21(3):95–97. [PubMed] [Google Scholar]
- 10.Alcântara CE, Corrêa-Faria P, Vasconcellos WA, Ramos-Jorge ML. Combined technique with dentin post reinforcement and original fragment reattachment for the esthetic recovery of a fractured anterior tooth: a case report. Dent Traumatol. 2010;26(5):447–450. doi: 10.1111/j.1600-9657.2010.00902.x. [DOI] [PubMed] [Google Scholar]
- 11.Ramires-Romito AC, Wanderley MT, Oliveria MD, Imparto JC, Pires Correa MS. Biological restoration of primary anterior teeth. Quintessence Int. 2000;35:405–411. [PubMed] [Google Scholar]
- 12.Kumar M, Sequeira PS, Peter S, Bhat GS. Sterilization of extracted human teeth for educational use. Indian J Med Microbiol. 2005;23:256–258. [PubMed] [Google Scholar]
- 13.Andreason JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int J Oral Surg. 1972;1:235–239. doi: 10.1016/S0300-9785(72)80042-5. [DOI] [PubMed] [Google Scholar]
- 14.Mentink AGB, Meeuwissen R, Kayser AF, Mulder J. Survival rate and failure characteristics of all metal posts and core restoration. J Oral Rehabil. 1993;20:455–461. doi: 10.1111/j.1365-2842.1993.tb01631.x. [DOI] [PubMed] [Google Scholar]
- 15.Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent. 1993;21:281–284. doi: 10.1016/0022-3913(84)90376-7. [DOI] [PubMed] [Google Scholar]
- 16.Akkayan B, Gulmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87:431–437. doi: 10.1067/mpr.2002.123227. [DOI] [PubMed] [Google Scholar]
- 17.Kapur A, Chawla HS, Goyal A, Gaube K. An esthetic point of view in very young children. J Clin Pediatr Dent. 2005;30:99–103. doi: 10.17796/jcpd.30.2.360k2j4452773418. [DOI] [PubMed] [Google Scholar]
- 18.Ehrmann EH. Restoration of a fractured incisor with exposed pulp using original tooth fragment: report of a case. J Am Dent Assoc. 1989;118:183. doi: 10.14219/jada.archive.1989.0244. [DOI] [PubMed] [Google Scholar]
- 19.Batista A, Lopes CG. Preformed dentin posts reinforcing teeth with immature apexes. Rev Bras Prot Clin Lab. 1999;3:199–210. [Google Scholar]
- 20.Galindo VAC, Nogueira JSF, Yamasaki E, Kos Miranda D. Biological posts and natural crowns bonding-alternatives for anterior primary teeth restoration. J Bras Odontoped Odontol Bebe. 2000;16:513–520. [Google Scholar]
- 21.Kaiser OB, Bonfante G, Pereira Filho LD, et al. Utilization of biological posts to reconstruct weakened roots. Rev Gaucha Odontol. 2008;56:7–13. [Google Scholar]
- 22.Ambica K, Mahendran K, Talwar S, Verma M, Padmini G, Periaswamy R. Comparative evaluation of fracture resistance under static and fatigue loading of endodontically treated teeth restored with carbon fiber posts, glass fiber posts, and an experimental dentin post system: an in vitro study. J Endod. 2013;39:96–100. doi: 10.1016/j.joen.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Kathuria A, Kavitha M, Khetarpal S. Ex vivo fracture resistance of endodontically treated maxillary central incisors restored with fiber-reinforced composite posts and experimental dentin posts. J Conserv Dent. 2011;14:401–405. doi: 10.4103/0972-0707.87211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grewal N, Seth R. Comparative in vivo evaluation of restoring severely mutilated primary anterior teeth with biological post and crown preparation and reinforced composite restoration. J Indian Soc Pedod Prevent Dent. 2008;26(4):141–148. doi: 10.4103/0970-4388.44028. [DOI] [PubMed] [Google Scholar]
- 25.Busato ALS, Loguercio AD, Barbosa NA, Sanseverino MCS, Macedo RP, Baldissera RA. Biological restorations using tooth fragments. Am J Dent. 1998;11:46–48. [PubMed] [Google Scholar]
- 26.Shaffer SE, Barkmeier WW, Gwinnett AJ. Effect of disinfection/sterilization in invitro enamel bonding. J Dent Educ. 1985;49:658–659. [PubMed] [Google Scholar]
- 27.Mc Guckin RS, Pashley DH. The effect of disinfection/sterilization treatments on gluma mediated dentin shear bond strengths. Am J Dent. 1990;3:278–282. [PubMed] [Google Scholar]



