Abstract
Several treatments have been suggested to improve the retention of zirconia-based restorations luted with different cements. Resin cements are believed to improve crown retention under certain circumstances. The aim of the present study was to examine the effect of three cements with different mixing methods on the retention of CAD/CAM zirconia crowns. Thirty extracted human molars were randomly divided into three groups and prepared for all-ceramic crowns (6° taper, 4-mm height and a 1.2 mm rounded shoulder finish line). A zirconia crown (Tizian CAD/CAM) was fabricated for each tooth. The crowns were air-abraded using airborne particles, adjusted, and cemented to the corresponding tooth with one of the following cements: Panavia F2 (PAN group), RelyX Unicem (UNH group) or RelyX Unicem Aplicap (UNA group). After 3,000 rounds of thermal cycling, retention was measured using a specific retentive jig and a universal testing machine. The retention strength was measured by dividing the retention force by the surface area of each tooth. The means of the pull-out test results for each group were compared using analysis of variance and Tukey’s HSD test (α = 0.05). The mode of failure was examined using a stereomicroscope. The mean retention value was 6.45 (0.34) MPa for the UNA group, 4.99 MPa (0.47) for the UNH group, and 4.45 (0.39) for the PAN group; the differences among the three test groups were significant. A mixed failure was observed in 83.3 % of specimens, while no cohesive failure occurred in the crowns. Within the limitations of the present study, of the three tested cements, Relyx Unicem Aplicap cement was associated with the highest retention force for Tizian zirconia crowns.
Keywords: Zirconia crowns, Resin cements, Mixing method, Retention strength
Introduction
The use of all-ceramic restorations with improved mechanical properties and a natural appearance has become a common practice in dental offices [1]. Of the most recently developed all-ceramic systems, zirconia-based materials are particularly attractive due to their high strength and durability, as well as their esthetic appeal. Several studies have investigated the longevity of zirconia-based fixed partial dentures (FPDs); in one study, the survival of the zirconia fixed partial dentures (FPDs) was reported as 94 % over 4 years, 92 % over 5 years, and even 100 % over 3 years, which was equal to metal ceramic FPDs [2–4]. However, the cumulative 5-year survival of single crowns was found to be 88.8 % in another study [5]. In clinical trials, the most frequent complications associated with zirconia-based restorations were chipping of the veneering ceramic, fracture of the framework, and loss of retention [6]. Several strategies have been proposed to increase the retention of all-ceramic restorations, including different surface treatments and cement selection [7, 8].
The use of resin cements is highly recommended in the literature to compensate for marginal discrepancies, to improve retention, and to strengthen the restoration itself [9].Typically, the adhesive procedure involves the creation of micromechanical retention by the selective removal of amorphous silica with an inorganic acid such as hydrofluoric acid, silanization, and application of a resin cement and a bonding system. However, unlike silica-based ceramic, zirconia is a polycrystalline ceramic, which lacks amorphous glass and is acid-resistant. In fact, it has been reported that conventional Bis-GMA resin cements offer no improvement in performance over conventional non-adhesive cements for zirconia-based FPDs [10]. However, in cases that involve short abutments and unusual dislodging forces, the retention must be enhanced to achieve more predictable outcomes [9, 11]. Because adhesive failure is a common occurrence with cement bonding to zirconia surfaces, it has been proposed that only intermolecular bonds such as hydrogen bonds must exist between the cement and the ceramic surface [11–14]. Several studies have recommended applying an organophosphate-containing monomer and/or bonding agents in combination with airborne particle abrasion to achieve a durable bond [14–19].
Regardless of the cement type, the cement layer is the weakest link in adhesive-bonded ceramic restorations [14, 20]. Accordingly, the quality of the cement layer can affect the longevity of these restorations [9]. In addition to the proper fitness of the restoration itself, cement thickness, flaws in the cement layer, and mixing methods may also negatively affect the bond strength. For example, errors in the base/catalyst proportion have been shown to significantly reduce the strength of a self-adhesive resin cement [21]. Voids and discontinuities in the cement layer also promote debonding due to occlusal loading, fatigue, and degradation in the oral environment [20, 22].
Generally, luting cements consist of at least two pastes. Studies have shown that when the pastes are mixed, air bubbles and voids can be introduced into the cement, leading to inferior mechanical properties, including reduced strength [23]. Studies have also addressed the effect of mixing methods on the porosity of the final set and its correlation with cement strength. Covey et al. [24] found that machine-mixed resin-modified glass ionomer exhibited a significantly lower porosity than manually mixed cement. In contrast, Nomoto et al. [25] found that greater porosity and lower strength were associated with automatically mixed glass ionomer. Limited evidence exists regarding the effect of mixing methods of resin cements on the retention of zirconia-based crowns. Therefore, the aim of the present study was to examine the effect of three cements with different mixing methods on the retention of CAD/CAM zirconia crowns. The null hypothesis was that the different cement types and mixing methods do not affect the retention of zirconia crowns.
Methods and Materials
Thirty human maxillary premolars, extracted within a single month, were selected for the study. Only teeth without caries, cracks, or excessive wear were included in the study. The teeth were cleaned to remove tissue tags and calculus using a hand instrument and were stored in a 0.1 % chloramine solution for 2 weeks and in distilled water thereafter. To ensure a consistent tooth size, the mesiodistal and buccolingual surfaces were measured using a digital caliper (Series 500 Mitutoyo, Tokyo, Japan) with an accuracy of 0.01 mm. Teeth within 1 mm of the mean size were selected. One-way analysis of variance (ANOVA) was performed to confirm that no significant difference in size existed among the selected teeth.
All of the specimens were mounted in an acrylic block (20 × 20 × 30 mm) along their long axes and prepared for full ceramic crowns. The occlusogingival height was reduced to 4 mm, and the axial surfaces were reduced using a round-end tapered diamond (ISO 856.018, D+Z, Lemgo, Germany) with a 1 mm round shoulder finish line. To improve the accuracy, a custom-made device was used during preparation that attached to the surveyor and to the rotary instrument (Fig. 1). In addition, the occlusal convergence was measured using photographs and image processing software (Adobe Photoshop CS2, version 9.0; Adobe Systems Inc., San Jose, CA, USA). The preparations were finished after final approval by two authors (AF and LS). Impressions of all of the specimens were made using a polyvinyl siloxane impression material (Elite Regular Body; Zehrmack, Marl, Germany) with a custom-made tray (Major, Moncalieri, Italy) and poured in type IV stone (Fujirock EP, GC Corp., Tokyo, Japan). Dies on the master models were scanned using a Tizian CAD/CAM Opt Scanner (Schutz Dental GmbH, Rosbach, Germany), and the zirconia crowns were fabricated using pre-sintered blank blocks of partially stabilized zirconia. For the pull-out test, four wings were included in the coping design, as described by Ernst et al. [26] (Fig. 2). The internal surface of the copings were air-abraded using 110 μm aluminum oxide particles at a distance of 10 mm and a pressure of 0.4 MPa for 20 s. The copings were adjusted onto their corresponding teeth using a disclosing silicone (FIT CHECKER; GC Co., Aslip, IL, USA).
Fig. 1.
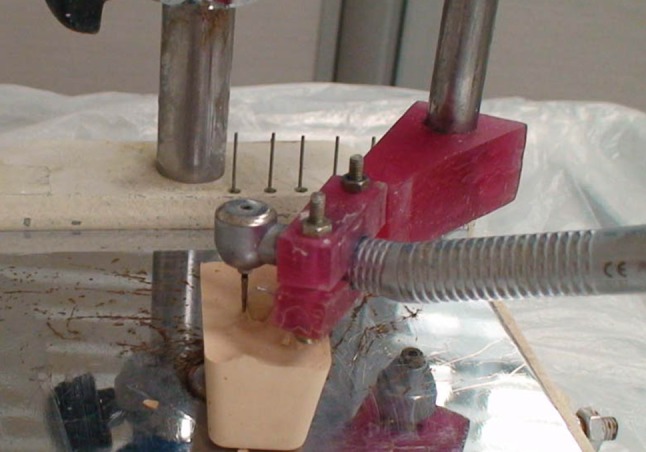
A special jig was designed for standardized preparation of teeth
Fig. 2.
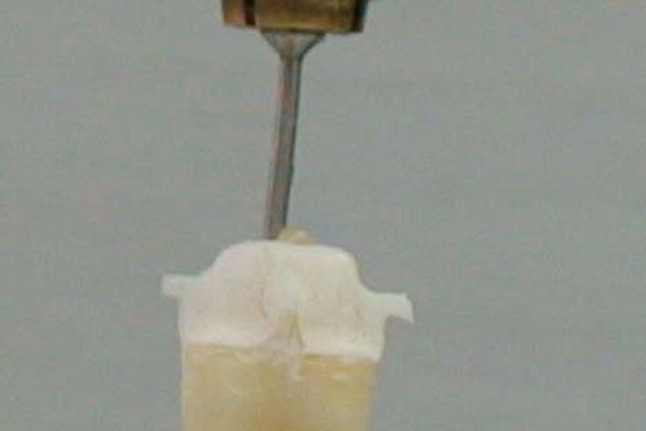
Retentive sings were included in the design of copings
The teeth were then randomly assigned to three different groups (n = 10 each) according to the cement type to be used. For the PAN group, Panavia F2 (Kurary, Osaka, Japan) was used as the cement; for the UNH group, hand-mixed Unicem (RelyX Unicem; 3 M/ESPE, Seefeld, Germany) was used; and for the UNA group, Unicem Aplicap (RelyX Unicem; 3 M/ESPE, Seefeld, Germany) was used. All of the cementations were performed according to the manufacturer’s instructions. To ensure an even seating pressure, a 5-kg weight was used to hold the crowns in place during the primary setting of the cement. The crowns were then light-polymerized with a light unit (Coltolux/Whaledent, Cuyahoga Falls, OH, USA) for 40 s on each side at 600 mW/cm2 and a distance of 1.0 mm. The specimens were kept in 37 °C water for 1 week and then subjected to 3,000 rounds of thermal cycling between 5 and 55 °C with a dwelling time at 12 °C. To perform the pull-out test, a screw hook was embedded in an acrylic block that was glued to the crowns with a cyanoacrylate adhesive (Superglue; RAZI Chemical Co., Tehran, Iran) to achieve an even stress distribution (Fig. 3).The pull-out test was performed using a universal testing machine (Zwick Roell Z050, Ulm, Germany) with a crosshead speed of 0.5 mm/min. The retention force was sketched automatically in N using Zwick software. In addition, the surface area of each abutment tooth was measured by adapting tin foil and measuring the surface area of the tin foil using engineering graph paper with a 0.5 mm grid. The strength was obtained by dividing the retention force by the surface area in MPa. The retentive force and retentive strength among the test groups were analyzed statistically by one-way ANOVA and Tukey’s honest significant difference (HSD) post hoc test using SPSS (version 13) statistical software (SPSS Inc., Chicago, IL, USA) at the level of significance of α = 0.05. The mode of failure was determined using a Zeiss OPM1 stereomicroscope (Carl Zeiss, Oberkochen, Germany) at a 40× magnification. The mode of failure was classified as cohesive, adhesive, or mixed.
Fig. 3.
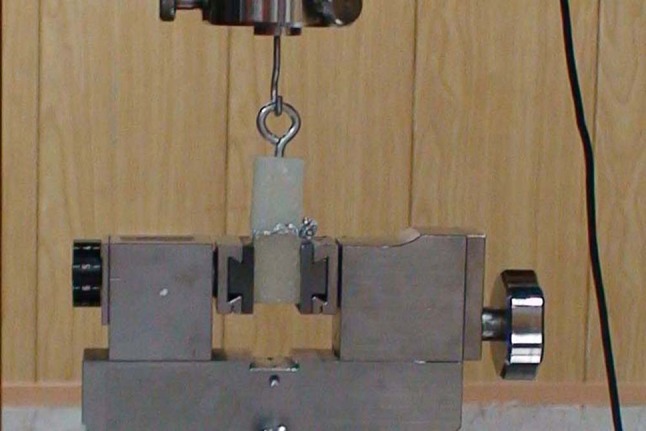
Each specimen was glued to a spitted jig for distributed retentive force in universal testing machine
Results
The mean values of the retention force and strength are summarized in Tables 1 and 2. A significant difference among the means of the test groups (P = 0.001) was demonstrated using one-way ANOVA. Tukey’s HSD test revealed that the mean retentive force and retentive strength values of the UNA were significantly higher than the mean values obtained for the PAN and UNH groups (P = 0.001) (Tables 3, 4). A mixed failure was observed in 83.3 % of the crowns. Five adhesive failures occurred with no adhesive on the abutment surface (two in the PAN group, two in the UNA group, and one in the UNH group). No crown was fractured during the pull-out test.
Table 1.
Descriptive data for retentive force of test groups
| Test groups | Valid number | Minimum force (N) | Maximum force (N) | Mean (std) |
|---|---|---|---|---|
| PAN | 10 | 297.2 | 427.28 | 354.10 (35.89) |
| UNA | 10 | 490.3 | 592.3 | 525.60 (36.48) |
| UNH | 10 | 351.9 | 480.3 | 399.11 (42.34) |
std Standard deviation
Table 2.
Descriptive data of retentive strength of test groups
| Test groups | Valid number | Minimum strength (Mpa) | Maximum strength (Mpa) | Mean (std) |
|---|---|---|---|---|
| PAN | 10 | 3.85 | 5.08 | 4.45 (0.39) |
| UNA | 10 | 6.02 | 7.18 | 6.45 (0.34) |
| UNH | 10 | 4.53 | 5.85 | 4.99 (0.47) |
std Standard deviation
Table 3.
Comparison between mean retentive force of test groups (α = 0.05)
| (I) cement | (J) cement | Mean difference (N) | Standard error | Significant | 95 % Confidence interval | |
|---|---|---|---|---|---|---|
| Upper | Lower | |||||
| PAN | UNA | −196.106 | 12.898 | 0 | −227.191 | −165.02 |
| UNH | −45.771 | 12.898 | 0.002 | −76.856 | −14.685 | |
| UNA | PAN | 196.06 | 12.898 | 0 | 165.02 | 227.191 |
| UNH | 50.335 | 12.898 | 0 | 119.249 | 181.42 | |
| UNH | PAN | 45.771 | 12.898 | 0.002 | 14.685 | 76.856 |
| UNA | −150.335 | 12.898 | 0 | −181.42 | −119.249 | |
Table 4.
Comparison between mean retentive strength of test groups (α = 0.05)
| (I) cement | (J) cement | Mean difference (MPa) | Standard error | Significant | 95 % confidence interval | |
|---|---|---|---|---|---|---|
| Upper | Lower | |||||
| PAN | UNA | −2 | 0.181 | 0 | −2.45 | −1.551 |
| UNH | 0.544 | 0.181 | 0.015 | 0.993 | 0.094 | |
| UNA | PAN | 2.001 | 0.181 | 0 | 1.551 | 2.45 |
| UNH | 1.457 | 0.181 | 0 | 1.007 | 1.906 | |
| UNH | PAN | 0.544 | 0.181 | 0.015 | 0.094 | 0.993 |
| UNA | −1.457 | 0.181 | 0 | −1.906 | −1.007 | |
Discussion
This study demonstrated that the cement type and mixing method significantly influence the retention of zirconia-based crowns. Hence, the null hypothesis is rejected. Human teeth were selected for the present study, and crowns were made to reflect real clinical conditions. These types of studies are less common than tests of bond strength, such as shear bond or tensile bond strength [10].
The primary challenge of studies using human teeth lies in standardizing the specimens. In this study, teeth of similar size and condition were selected. All of the preparations were performed with an equal occlusal height of 4 mm and a 6° taper with the aid of a custom-made device to hold the rotary instrument and cutting bur in a similar position. A consistent seating pressure was provided during the crown cementation with a 5-kg weight. Proper seating pressure during the initial stage of cement setting, in addition to being clinically relevant, is crucial for simultaneous demineralization and infiltration to the tooth stump when self-etch, high-viscosity, or self-adhesive cements are used [26]. These conditions were applied in our study, which high viscosity cements such as RelyX™ Unicem and RelyX™ Aplicap were used. Both cements produce an acidic pH, which helps to demineralize and infiltrate hard tissue.
Many studies have evaluated the effect of cement type on the bond strength to zirconia. Regardless of the method and test design, similar results have been obtained. For example, it has been shown that conventional cements have a lower bond strength than resin cements, and that resin cements containing MDP monomer have a higher bond strength than Bis-GMA-based resin [7, 8, 13, 16]. The long saturated carbonyl chain in the organophosphate monomer of 10-MDP was suggested to be responsible for a more hydrophobic bonded interface, which, in turn, made it water-resistant and durable [19]. In addition, the speculation was made that a functional monomer may bond chemically to the hydroxyl groups available on the zirconia surface [13]. Moreover, sandblasting may improve adhesive surface energy by increasing the roughness and increasing the contact angles of adhesion surfaces [8, 16, 18]. Therefore, an MDP-containing monomer resin cement, Panavia™ F2, was included in the study, and all crowns were air-abraded before cementation. However, no silanization was performed because zirconia ceramic contains no silica glass [10].
Generally, the average stress obtained with human teeth is much lower than that observed in bond-strength studies using simple disk-shaped specimens. Several factors may contribute to this difference. First, the complex geometry of restorations, such as crowns, apply more complex forms of stress on the cement layer, which may increase the tensile force in combination with the shear force during the pull-out test. In restorations, such as crowns, other factors—including retention and resistance forms—may interfere with the bond strength of the cements. For taller and less convergent walls of abutments, less stress is experienced in the cement layer [27]. In the present study, a 6° convergence and a 4-mm height were used for all groups. Ernst et al. [26] evaluated the effect of four luting cements, including Panavia™ and RelyX™ Unicem, on the retentive force of zirconia crowns. The preparation heights were all 3 mm, and the axial walls were parallel. Despite differences in the test design, the retentive force obtained was similar to that measured in our study (4.0 MPa for Panavia™ and 4.9 MPa for Unicem). The slightly higher values obtained in the Ernst study could be the result of using Rocatec™ for the surface treatment of the crowns, a cement that is believed to increase the resin bond strength to ceramic surfaces [28].
Quality of the cement layer also affects the retention stress of crowns. In general, application of cement into the intaglio surface of crown restorations is less controllable than applying cement to a single flat surface in a shear bond test [10]. Trapped air and porosity in the cement layer that develops during mixing, applying, seating, and setting may also have a negative effect on the quality of the cement layer. In the present study, the effect of the mixing method was addressed by examining Panavia F2, a hand-mixed resin cement recommended in many studies for its high performance in bonding to zirconia, and two versions of a self-adhesive cement, Unicem, one of which was mixed by hand, and Unicem Aplicap, which was machine-mixed. Unicem Aplicap was associated with the highest retention stress. Similar studies were not found in the literature for comparison. However, Palacios et al. [29] evaluated the retention of three resin cements, including Panavia F2 and Unicem Clicker. The latter is a paste/paste product that benefits from automatic mixing similar to the method used in our study. No significant difference was found among the tested groups in their study. Although the stress range was similar to that obtained in our study, the standard deviation in the Palacio study was relatively high, which may explain the lack of detectable significant differences between the cements. In addition, different materials, methods of fabrication, and test designs may also explain the conflicting results. A number of studies have reported that machine-mixed or auto-mixed cements perform better than hand-mixed cements. However, none of the resin cements used in this study has been examined in previous studies. Nomoto et al. demonstrated that, for the more viscous glass ionomer cements in the Aplicap form, automatic mixing was less likely to produce porosity. These authors also confirmed that cements with lower strength contained more large bubbles. In the same way, Covey et al. [24] investigated the porosity of hand- and machine-mixed resin-modified glass ionomer cements and observed significantly more porosity in the manually prepared specimens. In the present study, Unicem aplicap showed significantly higher retention force, which is in agreement with the previously described studies.
In our study, mode of failure was identified by investigating the abutment tooth surface. The failure type was mixed when a remnant of resin was observed in at least one area of the abutment tooth. A mixed type of failure was observed in 25 out of 30 samples, while adhesive failure occured in the remaining samples. Adhesive failure occurred in all three groups with no significant difference. The complex configuration of a crown develops a complex form of stress in the cement layer during loading. Therefore, no correlation could be found between the retention strength values and the observed mode of failures. However, a mixed mode of failure may suggest a cohesive failure in resin cement, which is generally a favorable indicator of retention [18].
Our study is limited by the lack of long term results, which were not obtained because the storage time was limited to 7 days, and by the lack of fatigue loading, which may propagate microcracks and/or flaws in the cement layer to promote cement failure [22]. Future studies are needed to examine these parameters.
Conclusion
Within the limitations of the present study, we conclude that the method of mixing—namely, automixing—may produce a more homogeneous cement layer and may improve the retention of Unicem self-adhesive cement to zirconia crown.
Acknowledgments
This research was an undergraduate dissertation and partly funded by Vice Chancellor for Research at Tehran University off Medical Sciences.
Contributor Information
Leyla Sadighpour, Phone: +98-21-88015860, FAX: +98-21-88015800, Email: sedighle@tums.ac.ir, Email: lsedigh@yahoo.com.
Akbar Fazel, Email: dabirdandan@yahoo.com.
Farideh Geramipanah, Email: geramipa@tums.ac.ir.
Mahdi Allahdadi, Email: mahdi.allahdadi@yahoo.com.
References
- 1.Donavan ET. Factors essential for successful all ceramic restorations. J Am Dent Assoc. 2008;139:14s–18s. doi: 10.14219/jada.archive.2008.0360. [DOI] [PubMed] [Google Scholar]
- 2.Roediger M, Gersdorff N, Huels A, Rinke S. Prospective evaluation of zirconia posterior fixed partial dentures: four-year clinical results. Int J Prosthodont. 2010;23:141–148. [PubMed] [Google Scholar]
- 3.Schmitt J, Goellner M, Lohbauer U, Wichmann M, Reich S. Zirconia posterior fixed partial dentures: 5-year clinical results of a prospective clinical trial. Int J Prosthodont. 2012;25(56):585–589. [PubMed] [Google Scholar]
- 4.Sailer I, Gottner J, Kanel S, Hammerte CHF. Randomized controlled clinical trial of zirconia–ceramic and metal–ceramic posterior fixed dental prostheses: a 3-year follow-up. Int J Prosthodont. 2009;22:553–560. [PubMed] [Google Scholar]
- 5.Ortorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 2012;40:527–530. doi: 10.1016/j.jdent.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Raigrodski AJ, Hillstead MB, Graham KM, Chung KH. Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent. 2012;107:170–177. doi: 10.1016/S0022-3913(12)60051-1. [DOI] [PubMed] [Google Scholar]
- 7.Oyague RC, Monticelli F, Toledano EO, Ferrari M, Osorio R. Influence of surface treatments and resin cement selection on bonding to densely-sintered zirconium-oxide ceramic. Dent Mater. 2009;25:172–179. doi: 10.1016/j.dental.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 8.Blatz MB, Chiche G, Holst S, Sadan A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007;38:745–753. [PubMed] [Google Scholar]
- 9.Edelhoff D, Ozcan M. To what extent does the longevity of fixed dental prostheses depends on the function of the cement? Clin Oral Implant Res. 2007;18:193–204. doi: 10.1111/j.1600-0501.2007.01442.x. [DOI] [PubMed] [Google Scholar]
- 10.Derand T, Molin M, Kleven E, Hagg P, Karlsson S. Bond strength of luting materials to ceramic crowns after different surface treatments. Eur J Prosthodont Rest Dent. 2008;16:35–38. [PubMed] [Google Scholar]
- 11.Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zirconia and other non-silicate ceramics: where are we now? Dent Mater. 2011;27:71–82. doi: 10.1016/j.dental.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lahbauer U, Zipperle M, Rischka K, Patschelt A, Muller FA. Hydroxylation of dental zirconia surfaces: characterization and bonding potential. J Biomed Mater Res, Part B. 2008;87:461–467. doi: 10.1002/jbm.b.31126. [DOI] [PubMed] [Google Scholar]
- 13.Aboushelib MN, Matinlinna JF, Salameh Z, Ounsi H. Innovations in bonding to zirconia-based materials: part I. Dent Mater. 2008;24:1268–1272. doi: 10.1016/j.dental.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Kim MJ, Kim YK, Kim KH, Kwon TY. Shear bond strength of various luting cements to zirconia ceramic: surface chemical aspects. J Dent. 2011;39:795–803. doi: 10.1016/j.jdent.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Ozcan M, Nijhuis H, Valandro LF. Effect of various surface conditioning methods on adhesion of dual-cure resin cement with MDP functional monomer to zirconia after thermal aging. Dent Mater J. 2008;27:99–104. doi: 10.4012/dmj.27.99. [DOI] [PubMed] [Google Scholar]
- 16.Kern M, Barloi A, Yang B. Surface conditioning influences zirconia ceramic bonding. J Dent Res. 2009;88:817–822. doi: 10.1177/0022034509340881. [DOI] [PubMed] [Google Scholar]
- 17.Mirmohammadi H, Aboushelib MN, Salameh Z, Feilzer AJ, Kleverlaan CJ. Innovations in bonding to zirconia based ceramics: part III. Dent Mater. 2010;26:786–792. doi: 10.1016/j.dental.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Shahin R, Kern M. Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent Mater. 2010;26:922–928. doi: 10.1016/j.dental.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Geramipanah F, Majidpour M, Sadighpour L, Kharazi Fard MJ. Effect of artificial saliva and pH on shear bond strength of resin cements to zirconia-based ceramic. Eur J Prosthodont Rest Dent. 2013;21:5–8. [PubMed] [Google Scholar]
- 20.Hernandez AI, Roongruangphol T, Katsube N, Seghi RR. Residual interface tensile strength of ceramic bonded to dentin after cyclic loading and aging. J Prosthet Dent. 2008;99:209–217. doi: 10.1016/S0022-3913(08)60045-1. [DOI] [PubMed] [Google Scholar]
- 21.Behr M, Rosentritt M, Loher H, Kolbeck C, Trempler C, Stemplinger B, Kozon V, Handel G. Changes of cement properties caused by mixing errors: the therapeutic range of different cement types. Dent Mater. 2008;24:1187–1193. doi: 10.1016/j.dental.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Bolhuis P, de Gee A, Feilzer A. The influence of fatigue loading on the quality of the cement layer and retention strength of carbon fiber post-resin composite core restorations. Oper Dent. 2005;30(2):220–227. [PubMed] [Google Scholar]
- 23.Cantoro A, Goracci C, Coniglio I, Magni E, Polimeni A, Ferrari M. Influence of ultrasound on inlays luting with self-adhesive resin cements. Clin Oral Invest. 2011;15:617–623. doi: 10.1007/s00784-010-0451-5. [DOI] [PubMed] [Google Scholar]
- 24.Covey DA, Ewoldsen NO. Porosity in manually and machine mixed resin-modified glass ionomer cements. Oper Dent. 2001;25:617–628. [PubMed] [Google Scholar]
- 25.Nomoto R, Komoriyama M, McCabe JF, Hirano S. Effect of mixing method on the porosity of encapsulated glass ionomer cement. Dent Mater. 2004;20:972–978. doi: 10.1016/j.dental.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 26.Ernst CP, Cohnen U, Stender E, Willershausen B. In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prosthet Dent. 2005;93:551–558. doi: 10.1016/j.prosdent.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Viotti RG, Kasaz A, Pena CE, Alexandre RS, Arrais CA, Reis AF. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102:306–321. doi: 10.1016/S0022-3913(09)60180-3. [DOI] [PubMed] [Google Scholar]
- 28.Ersu B, Narin D, Aktas G, Yuzugullu B, Canay S. Effect of preparation taper and height on strength and retention of zirconia crowns. Int J Prosthodont. 2012;25:582–584. [PubMed] [Google Scholar]
- 29.Palacios RP, Johnson GH, Phillips KM, Raigrodski AJ. Retention of zirconium oxide ceramic crowns with three types of cement. J Prosthet Dent. 2006;96:104–114. doi: 10.1016/j.prosdent.2006.06.001. [DOI] [PubMed] [Google Scholar]


