INTRODUCTION
Benign esophageal cysts—a type of gastrointestinal duplication cysts are rare embryonic malformations with an incidence of 1:1,00,000 in childhood with only 160 cases reported in the adults. Duplication can occur in any part of esophagus but the most common is lower thoracic region to right.[1] Esophageal cysts though asymptomatic in most cases may manifest with dysphagia, hematemesis, and sometimes malignant transformation, which warrants surgery in these patients.[2] Based on morphology, esophageal duplications may be cystic, tubular, and diverticular with cystic being the most common. Here we present a case of tubular esophageal duplication cysts diagnosed incidentally in a young adult.
PRESENTATION
An 18-year-old female presented to medicine outpatient department with chief complaints of fever, cough, and breathlessness for 1–2 months. Fever was high grade, associated with chills and rigor. She also had productive cough with expectoration of copious, non-foul smelling sputum. This was associated with breathlessness and left-sided, dull aching chest pain. Past history failed to reveal any history of tuberculosis, dysphagia, odynophagia, and recurrent vomiting.
On examination, the patient was febrile and had clubbing. The rest of the general physical examination was unremarkable. Chest revealed coarse, leathery crepitations in base of left lung. Other systemic examination was normal. An initial working diagnosis of postinfective bronchiectasis was made.
Laboratory tests reported the hemoglobin to be 9.5 mg/dL and a raised leukocyte count, which settled during the course of treatment with antibiotics. Liver function tests, kidney function tests, and electrolytes were within normal limits. Sputum culture was sterile.
The chest radiography revealed bronchiectatic lesions in left lung lower zone, which was consistent with clinical findings and surprisingly revealed a cystic lesion on left side of trachea, just below carina [Figure 1], which led to possibility of a mass lesion in the thorax. In view of this, contrast-enhanced computed tomography of thorax was done and it revealed a tubular cystic lesion measuring 9.1 × 3.1 × 2.9 cm in the left paratracheal region with minimal fluid and thin enhancing wall causing slight deviation of trachea and esophagus to the right side. There were cystic and tubular bronchiectatic changes in all segments of left lower lobe with large cavity formation of 3.5 × 4.4 × 2.8 cm in superior segment [Figures 2 and 3].
Figure 1.
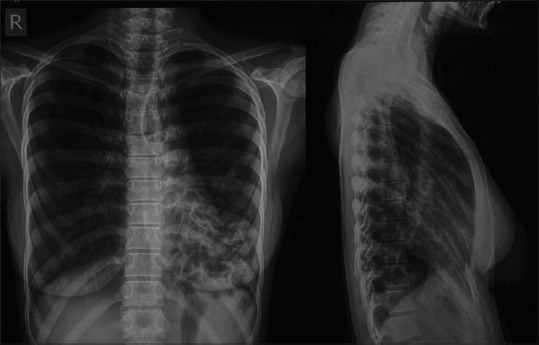
Chest postero-anterior and lateral radiographs show a cystic lesion with air fluid level in the mediastinum, indenting the trachea along with cystic lucencies predominantly in the left lower zone
Figure 2.
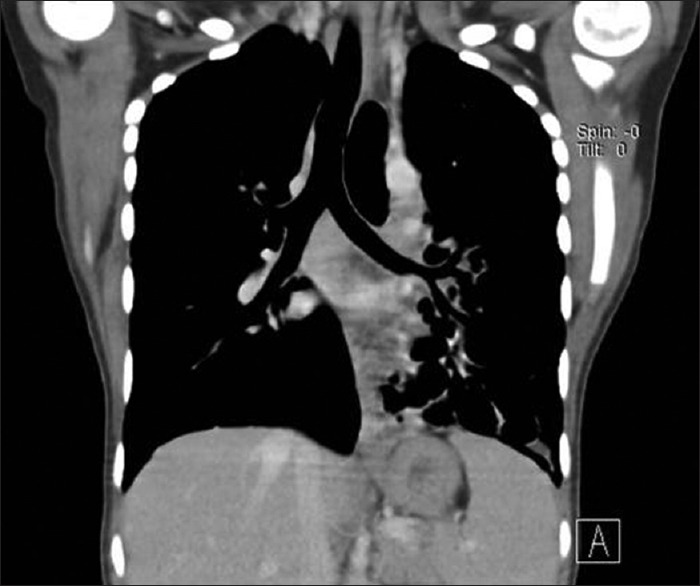
Coronal contrast-enhanced computed tomography shows tubular structure (with air), between the trachea and aortic arch, also displacing the trachea to right
Figure 3.

Coronal lung window demonstrates the tubular cystic lesion, adjacent to trachea, and also cystic bronchiectasis involving left lower lobe
Upper gastrointestinal endoscopy was suggestive of extrinsic compression extending from 21 cm to 28 cm causing partial luminal compression. However, scope negotiated across without any resistance (radial endoscopic ultrasound done using Olympus CLV 180 scope) suggested an elongated tubular structure parallel to esophagus with common serosal lining likely to be an esophageal duplication cyst.
The patient was started on a course of antibiotics and improved. The patient was referred to gastroenterology department where she was managed conservatively.
DISCUSSION
Esophageal duplication cysts are a manifestation of anomalies of the foregut along with bronchogenic cysts and constitute up to 1 out of 15 cases of mediastinal cysts. Most of them are found incidentally in children evaluated for other medical problems and may be associated with other congenital anomalies, such as small intestine duplications, esophageal atresias distal to the duplication, tracheoesophageal fistulas, and spinal abnormalities.[3] Esophageal cysts are mostly asymptomatic but a manifestation in long-standing cyst is a sign of development of complication, hence surgery is warranted.
We present here the incidental finding of an esophageal duplication cyst on radiological investigations, which was unusual as the diagnosis was made at the age of 18 years as opposed to childhood in majority of cases.[4] Moreover, majority of the cases have a finding on the right, whereas we present a case of cyst on the left reflecting the embryogenesis.
In view of complications, the treatment of choice for asymptomatic esophageal cyst is surgery[5]; however, our patient was discharged on treatment for bronchiectasis and managed conservatively for esophageal duplication cyst.
Footnotes
Source of Support: There was no funding received for this study from any source
Conflict of Interest: All the authors have seen the final manuscript and approved it for submission. The authors have no competing interests in the publication of this manuscript to declare.
REFERENCES
- 1.Nazem M, Amouee AB, Eidy M, Khan IA, Javed HA. Duplication of cervical oesophagus: A case report and review of literatures. Afr J Paediatr Surg. 2010;7:203–5. doi: 10.4103/0189-6725.70429. [DOI] [PubMed] [Google Scholar]
- 2.Petrović S, Ljuština R, Lovrenski J, Milović I, Barišić N. Persistent wheezing as manifestation of esophageal tubular duplication cyst. Ups J Med Sci. 2011;116:216–9. doi: 10.3109/03009734.2011.574165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sethi GK, Marsden J, Johnson D. Duplication cysts of the esophagus. South Med J. 1974;67:616–8. doi: 10.1097/00007611-197405000-00025. [DOI] [PubMed] [Google Scholar]
- 4.Wootton-Gorges SL, Eckel GM, Poulos ND, Kappler S, Milstein JM. Duplication of the cervical esophagus: A case report and review of the literature. Pediatr Radiol. 2002;32:533–5. doi: 10.1007/s00247-002-0693-8. [DOI] [PubMed] [Google Scholar]
- 5.Wiechowska-Kozlowska A, Wunsch E, Majewski M, Milkiewicz P. Esophageal duplication cysts: Endosonographic findings in asymptomatic patients. World J Gastroenterol. 2012;18:1270–2. doi: 10.3748/wjg.v18.i11.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]


