Abstract
Introduction:
Hypomagnesemia has been common, but mostly underdiagnosed electrolyte abnormality. Studies regarding this is lacking in India especially in rural setting. Here, we have correlated serum magnesium (Mg) level with outcome in patients of medicine Intensive Care Unit (ICU) with respect to length of ICU stay, need for mechanical ventilatory support and its duration and ultimate outcome (discharge/death).
Materials and Methods:
This is a prospective observational study carried out over a period of 1-year enrolling 601 patients of Medical ICU (MICU). The Chi-square test is applied to correlate hypomagnesemia with the outcome.
Result and Observation:
About 25% patients had admission hypomagnesemia. When compared with the normal Mg group, there was significant association of hypomagnesemia with outcome in terms of duration of MICU stay 5.46 (5.75) versus 3.93 (3.88), need for mechanical ventilation (56.86% vs. 24.33%), discharge/cured from ICU (61.43% vs. 85.26%), and death (38.56% vs. 14.73%). However, no significant difference was found in the duration of ventilation between the two groups.
Conclusion:
Hypomagnesemia is associated with a higher mortality rate in critically ill patients. The need for ventilatory support, but not its duration is significantly higher in hypomagnesemic patients. Hypomagnesemia is commonly associated with sepsis and diabetes mellitus. The duration of MICU stay is significantly higher in patients with low serum Mg.
Keywords: Hypomagnesemia, Intensive Care Unit, outcome
Introduction
Magnesium (Mg) is the second most prevalent intracellular cation and has an important role as a cofactor in various enzymatic reactions.[1] It also provides energy and regulates various processes in the cell and cell membrane, as well as protein and DNA synthesis, and the regulation of mitochondrial function.[1] Hence, recognition of hypomagnesemia in patients of Medical Intensive Care Unit (MICU) may be important as this may be associated with severity of illness or increased mortality and morbidity. The incidence of hypomagnesemia is reported as 2% in the general population, 10–20% in hospitalized patients, 50–60% in Intensive Care Unit (ICU) patients, and 30–80% in persons with alcoholism, and 25% in outpatients with diabetes.[2]
Although many templates have been assessed to study the mortality and morbidity in ICUs regarding Mg and its impact, it is less reported especially in India, in this respect leading to inconclusive results.[3,4] No data are available from the rural part of India. In this study, we have tried to correlate serum Mg level with outcome in patients of medicine ICU with respect to the length of ICU stay, need for mechanical ventilatory support and its duration and ultimate outcome (discharge/death).
Materials and Methods
This prospective observational study was carried out in the ICU of medicine department in Jawaharlal Nehru Medical College and Acharya Vinoba Bhave Rural Hospital, Wardha, Maharashtra, India, in year 2012; from January to December, after approval by the Institutional Ethics Committee. Among 651 patients admitted to the MICU 601 were included in the study. Patients were enrolled at random, and the selection bias was avoided by registering those patients who fulfilled the criteria for critical illness on the basis of severity scoring system (Acute Physiology and Chronic Health Evaluation-II [APACHE II]). Fifty patients were excluded from the study as 42 were stable and 8 due to financial constraints shown in flow chart [Figure 1]. Patients who had received Mg prior to transfer to MICU were excluded though there was no such history in our patients. Demographic data (age and sex), past medical history, medications administrated, and length of ICU stay were recorded for each patient. The severity scoring system used was APACHE-II. Blood, urine, and endotracheal secretions were sent for culture screen in every febrile patient. Blood samples were collected for estimation of serum total Mg levels on admission to MICU, which was determined by colorimetric method. The study had not interfered with the patient management in MICU. The normal reference value of total serum Mg was between 1.5 and 2.5 mg/dl.[5] Less than 1.5 was considered as hypomagnesemia. Statistical analysis was done by using description and inferential statistics. All the data were expressed in mean ± standard deviation (SD). The analysis was performed by using test statistic Student's t-test for the difference of means, Chi-square test, and correlation. The software used in the analysis was SPSS 17.0 version [IBM Corporation, www.ibm.com/software/analytics/spss/] and Graph Pad Prism 5.0, and P < 0.05 was considered as significant.
Figure 1.
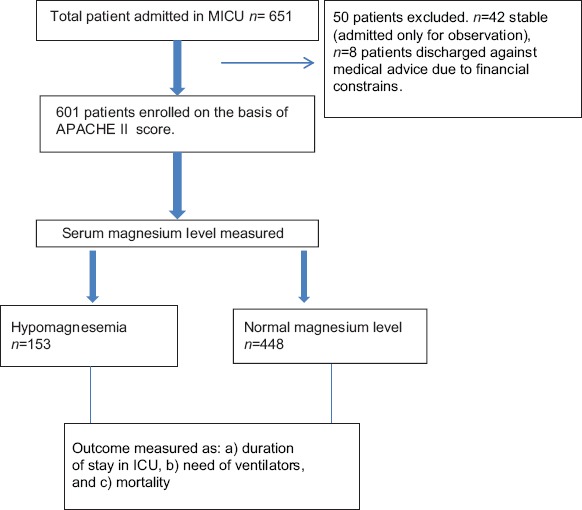
Flow chart showing enrolment of the patients
Results
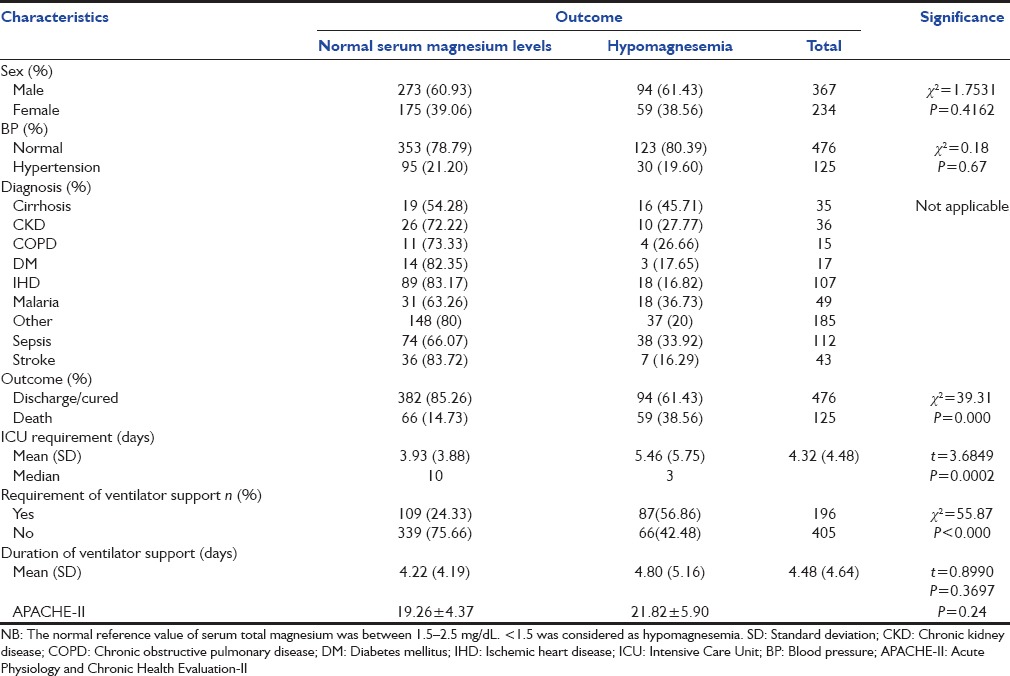
Altogether, 651 patients were admitted to MICU between April and October 2012, among them 601 were included in the study. Their mean age was 47.08 ± 17.18 in male and 46.37 ± 18.16 in female. Baseline comparison of characteristics of study subjects is shown in Table 1. On admission, 25.6% (94/367) in male patients and 25.2% (59/234) in female patients had hypomagnesemia. The lowest serum Mg value recorded was 1 mg/dl while the highest value was 2.5 mg/dl. The range of duration of stay in MICU varied from 1-day to 41 days with a mean of 4.60 days. The mean duration of stay in MICU was 3.93 (3.88) days among those with normal Mg level and 5.46 (5.75) days in patients of hypomagnesemia while overall it was 4.32 (4.48) days with t = 3.6849 and P = 0.0002. Median range in normomagnesemia was 10 days versus 3 days in hypomagnesemia [Table 2]. About 56.86% (87/153) patients with hypomagnesemia needed mechanical ventilatory support while 42.48% (65/153) did not need the support and in normomagnesemic group 24.33% (109/448) needed ventilatory support 75.66% (339/448) did not need it. The difference was statistically significant (P < 0.000 and χ2 = 55.87). The mean duration of ventilatory assistance for the hypomagnesemic group was 4.80 (5.16) days and that for the normomagnesemic group were 4.22 (4.19) days. The duration of ventilatory support was 4.22 days (SD 4.19) versus 4.80 days (SD 5.16) between hypomagnesemic and normomagnesemic patients, which was not found to be statistically significant P = 0.3697 and t = 0.8990 [Table 2]. The difference between cure rates/discharge between normal Mg and low Mg was 382 (85.26%) for normal Mg and 94 (61.43%) for low Mg, which was statistically significant. The mortality rate in hypomagnesemic group was 59/153 (38.56%); whereas in normomagnesemic group was 66/448 (14.73%) (χ2 = 39.31, P = 0.000). Finding of association between characteristics of study subjects and hypomagnesemia is shown in Table 2. The major groups of patients admitted in MICU were grouped as cirrhosis, chronic kidney disease (CKD), chronic obstructive pulmonary disease, diabetes mellitus (DM), ischemic heart disease (IHD), malaria, sepsis, stroke, and others [Table 2].
Table 1.
Baseline characteristics of study subjects
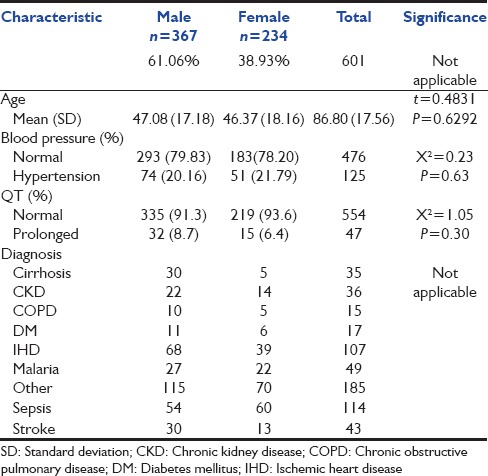
Table 2.
Comparison of patient characteristics between groups with normal vs. hypomagnesemia
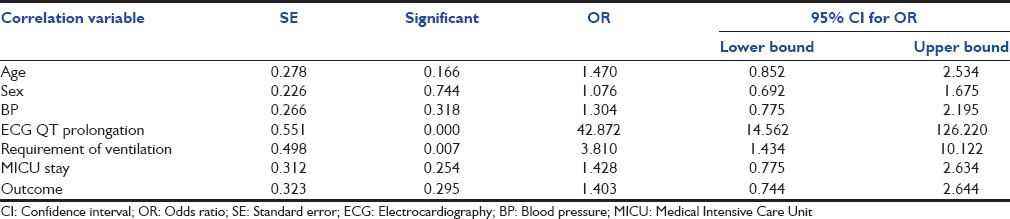
Multiple logistic regression models applied for the determination of factors associated with hypomagnesemia. Independent positive linear correlation was observed among QT prolongation on electrocardiography (ECG) and the longer requirement of ventilator support for patients with hypomagnesemia [Table 3].
Table 3.
Logistic regression for correlation between hypomagnesemia and various patients characteristics
Discussion
This study of hospitalized patients in MICU from rural Central India points to a possible impact of serum magnesium levels on outcomes in critically ill patients. In our study, of 601 critically ill patients, 25% (153/601) patients were hypomagnesemic, 75% (448/601) were normomagnesemic, suggesting frequent occurrence of low Mg in ICU patients. The primary endpoints of this study were serum Mg level and mortality of critically ill patients. Secondary outcome measures were the associated electrolyte disturbances and length of ICU stay. Mg deficiency along with other electrolyte abnormalities has been found to coexist in up to 40% of patients.[6,7] Many factors contribute to hypomagnesemia in critically ill patients such as decreased absorption caused by impaired gastrointestinal activity, malnutrition, renal wasting of various drugs (e.g., digitalis, gentamicin, loop diuretics, etc.), DM, hypokalemia, and hypocalcemia.[6]
Various studies have shown varying relationship between hypomagnesemia and mortality/morbidity rates. A higher mortality rate was detected in hypomagnesemia patients when compared with normomagnesemic patients by Limaye et al., (57% vs. 31%), Safavi and Honarmand (55% vs. 35%), and Rubeiz et al., (46% vs. 25%).[4,7,8] There was no significant difference in ICU mortality between hypomagnesemic and normomagnesemic groups (18% vs. 17%), but noted a higher mortality rate among hypermagnesemic patients by Guérin et al.,[9] our study revealed the mortality rate in hypomagnesemic group 38.56%, which was significantly higher as compared to 14.73% in the normomagnesemic group (P = 0.000, χ2 = 39.31). The higher mortality in our study can be ascribed to a greater incidence of electrolyte abnormalities especially hypokalemia and cardiac arrhythmias and a strong association of hypomagnesemia with sepsis and malnutrition. This was explained as independent positive linear correlation was observed among QT prolongation on ECG and outcomes for patients with hypomagnesemia [Table 3].
It has been observed in some studies, which had measured ionized Mg, the prevalence of hypomagnesemia was much lower (14% and 18%, respectively) than the studies, which had measured total serum or RBC Mg (20–70%).[10,11] We have not presented the actual Mg measurements for the groups, which may be one of the limitations.
Mg plays an important role in sepsis. Hypomagnesemia is associated with increased release of endothelin and proinflammatory cytokines.[12,13] This was strongly associated with increased mortality in experimental sepsis, and Mg replacement provides significant protection against endotoxin challenge. This effect was due to the down-regulation of the release of inflammatory cytokines (tumor necrosis factor-alpha, interleukin-6).[14,15] Sepsis was an independent risk factor for developing hypomagnesemia during ICU stay as found by Soliman et al.,[10] In the study conducted by Limaye et al., the incidence of sepsis was twice as more common in hypomagnesemic patients as compared to normomagnesem patients (P < 0.05).[4] Similarly, in the present study, the incidence of sepsis was twice as common in hypomagnesemic patents as in normomagnesemic patients.
Hypomagnesemia is also associated with DM, which may be due to increased renal losses of Mg that accompany glycosuria. There is also a strong relationship between hypomagnesemia and insulin resistance, and Mg supplementation is associated with decreased insulin requirements.[16] Limaye et al., carried out a study showing hypomagnesemia was more common in diabetic patients (P < 0.05).[4] In the present study, the incidence of hypomagnesemia was more common among diabetic patients.
Chronic alcoholism may be one of the predisposing factors for Mg deficiency. Hypomagnesemia was reported in 30% of hospital admissions with alcohol abuse and in 85% of admissions for delirium tremens. Low Mg in alcoholic individuals may be due to poor nutrition, renal tubular dysfunction so Mg wasting, pancreatitis, and an intracellular shift in alcohol withdrawal syndrome.[1,13] Soliman et al., had noted hypomagnesemia in one-third of patients with the chronic liver disease and alcoholism.[10] Limaye et al., showed the prevalence of hypomagnesemia was observed in one-half of alcoholic patients.[4] In the present study, the prevalence of hypomagnesemia is observed among one-third of the alcoholic patients.
Hypomagnesemia also leads to muscle weakness and respiratory failure, causing difficulty in weaning the patient from the ventilator. In the current study, it has been seen that patients with hypomagnesemia needed ventilatory support more frequently and for a longer duration. However, no significant difference was found in the duration of ventilation between the two groups (t = 0.8990, P = 0.3697). Fiaccadori et al., had observed that patients with low muscle Mg were on ventilatory support for more number of days.[17] Safavi and Honarmand had found that in patients with hypomagnesemia the duration of mechanical ventilation was longer (7.2 vs. 4.7 days, P < 0.01).[7] Prolonged ventilation is not just due to muscle weakness causing difficulty to wean. Hypermagnesemia is characteristically associated with neuromuscular blockade and muscle weakness and therefore also prolonged ventilation time.[7] Hypermagnesemia were not observed in our patients; the maximum level was 2.5 mg/dl.
In the study carried out by Soliman et al., there was no difference in the length of ICU stay among the hypo, as well as normomagnesium groups.[10] However, the patients who developed hypomagnesemia during their ICU stay had a longer duration of stay in the ICU. In the study conducted by Limaye et al., also there was no difference in the length of ICU stays among hypomagnesemic versus normomagnesemic patients.[4] In the present study, we have a significant difference in the length of ICU stay in hypomagnesemic and a normomagnesemic group of patients 5.46 ± 5.75 days vs. 3.93 ± 3.88 days, P = 0.0002, S).
The major limitation in our study design was the presence of many confounding variables that were not controlled for.
Conclusion
Mg alterations have frequently been observed in critically ill patients. In this study, there is a high prevalence of hypomagnesemia in the critically ill patients, which were associated with adverse outcomes. Physicians should be alert to the high incidence of hypomagensemia in critically ill patients and should consider their routine monitoring.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rude RK. Magnesium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, editors. Modern Nutrition in Health and Disease. 11th ed. Baltimore, Mass: Lippincott Williams and Wilkins; 2012. pp. 159–75. [Google Scholar]
- 2.Guerrera MP, Volpe SL, Mao JJ. Therapeutic uses of magnesium. Am Fam Physician. 2009;80:157–62. [PubMed] [Google Scholar]
- 3.Zafar MS, Wani JI, Karim R, Mir MM, Koul PA. Significance of serum magnesium levels in critically ill-patients. Int J Appl Basic Med Res. 2014;4:34–7. doi: 10.4103/2229-516X.125690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Limaye CS, Londhey VA, Nadkart MY, Borges NE. Hypomagnesemia in critically ill medical patients. J Assoc Physicians India. 2011;59:19–22. [PubMed] [Google Scholar]
- 5.Drueke TB, Lacour B. Magnesium homeostasis and disorders of magnesium metabolism. In: Feehally J, Floege J, Johnson RJ, editors. Comprehensive Clinical Nephrology. 3rd ed. Philadelphia, PA: Mosby; 2007. pp. 136–8. [Google Scholar]
- 6.Huijgen HJ, Soesan M, Sanders R, Mairuhu WM, Kesecioglu J, Sanders GT. Magnesium levels in critically ill patients. What should we measure? Am J Clin Pathol. 2000;114:688–95. doi: 10.1309/jr9y-pptx-ajtc-qdrd. [DOI] [PubMed] [Google Scholar]
- 7.Safavi M, Honarmand A. Admission hypomagnesemia - Impact on mortality or morbidity in critically ill patients. Middle East J Anaesthesiol. 2007;19:645–60. [PubMed] [Google Scholar]
- 8.Rubeiz GJ, Thill-Baharozian M, Hardie D, Carlson RW. Association of hypomagnesemia and mortality in acutely ill medical patients. Crit Care Med. 1993;21:203–9. doi: 10.1097/00003246-199302000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Guérin C, Cousin C, Mignot F, Manchon M, Fournier G. Serum and erythrocyte magnesium in critically ill patients. Intensive Care Med. 1996;22:724–7. doi: 10.1007/BF01709512. [DOI] [PubMed] [Google Scholar]
- 10.Soliman HM, Mercan D, Lobo SS, Mélot C, Vincent JL. Development of ionized hypomagnesemia is associated with higher mortality rates. Crit Care Med. 2003;31:1082–7. doi: 10.1097/01.CCM.0000060867.17556.A0. [DOI] [PubMed] [Google Scholar]
- 11.Koch SM, Warters RD, Mehlhorn U. The simultaneous measurement of ionized and total calcium and ionized and total magnesium in intensive care unit patients. J Crit Care. 2002;17:203–5. doi: 10.1053/jcrc.2002.35813. [DOI] [PubMed] [Google Scholar]
- 12.Lee JW. Fluid and electrolyte disturbances in critically ill patients. Electrolyte Blood Press. 2010;8:72–81. doi: 10.5049/EBP.2010.8.2.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marino P. The ICU Book. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2004. Fluid and electrolyte disorders - Magnesium; pp. 660–72. [Google Scholar]
- 14.Buckley MS, Leblanc JM, Cawley MJ. Electrolyte disturbances associated with commonly prescribed medications in the Intensive Care Unit. Crit Care Med. 2010;38:S253–64. doi: 10.1097/CCM.0b013e3181dda0be. [DOI] [PubMed] [Google Scholar]
- 15.Haque A, Saleem AF. On admission hypomagnesemia in critically ill children: Risk factors and outcome. Indian J Pediatr. 2009;76:1227–30. doi: 10.1007/s12098-009-0258-z. [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez M, Romero F. Oral magnesium supplementation improves insulin sensitivity and metabolic control in type 2 diabetic subjects. Diabetes Care. 2003;15:1045–9. doi: 10.2337/diacare.26.4.1147. [DOI] [PubMed] [Google Scholar]
- 17.Fiaccadori E, Del Canale S, Coffrini E, Melej R, Vitali P, Guariglia A, et al. Muscle and serum magnesium in pulmonary intensive care unit patients. Crit Care Med. 1988;16:751–60. doi: 10.1097/00003246-198808000-00004. [DOI] [PubMed] [Google Scholar]


