Abstract
Background:
Organophosphorus (OP) compounds are commonly used pesticides. In OP poisoning, intermediate syndrome (IMS) manifests between the end of the acute cholinergic crisis and delayed neuropathy. Respiratory paralysis in IMS, if identified early can reduce the need for ventilator support, morbidity, and mortality. Serum creatine phosphokinase (CPK) is elevated in IMS. The objectives of our study were to measure serum CPK level, correlate CPK levels with severity of poisoning and estimate atropine dose used.
Materials and Methods:
A prospective, observational study was conducted for 1-year. Patients diagnosed with OP poisoning were included. Demographic characteristics, type of poison, time since poisoning, Peradeniya Organophosphorus Poisoning (POP) score, serum pseudocholinesterase, CPK levels, atropine dose, and outcome of treatment were documented.
Results:
Seventy-five patients were recruited of which 57% and 43% were males and females, respectively, with a mean age of 31.48 ± 11.76 years. The most common OP compound was chlorpyriphos followed by triazophos and methylparathion. The time required to reach hospital was 181.26 ± 89.53 min. About 73.3% and 26.7% of patients had mild and moderate poisoning, respectively, as per POP scale. Pseudocholinesterase level was 364 (205–2168) IU. The amount of atropine used was 190.66 ± 78.83 mg. Serial serum CPK values were 279.72 ± 350.21 IU, 389.78 ± 376.33 IU and 163.13 ± 155.15 IU at admission, 48 h, and 96 h after admission, respectively. A weak positive correlation between serum CPK levels and severity of poisoning (r = 0.352) was observed. All patients recovered completely within 10.69 ± 5.57 days. Three patients developed IMS, and their serial CPK levels were 1837.33 ± 243.19 IU/L, 1935 ± 97.41 IU/L, and 714.66 ± 394.82 IU/L; and recovered in 17 ± 5.6 days.
Conclusion:
Increased serum CPK levels at 48 h after poisoning was observed in all the patients, but three patients had more than 1500 IU/L, who manifested with IMS. Early diagnosis of IMS by serial estimation of CPK may help in timely intervention and reduce further life-threatening complications.
Keywords: Creatine phosphokinase, intermediate syndrome, organophosphorus poisoning
Introduction
Organophosphorus (OP) compound is one of the common causes of poisoning in rural India as they are easily available.[1,2] Deaths reported due to OP compounds was 92,000 in the year 2010.[3] The most commonly used are methyl parathion, diazinon, chlorpyriphos, and dimicron.[4] OP poisoning leads to three main syndromes: Acute cholinergic syndrome, intermediate syndrome (IMS), and OP induced delayed neuropathy (OPIDN).[5,6]
IMS occurs 48–96 h after ingestion of OP compound and following recovery from the acute cholinergic crisis. It is characterized by skeletal muscle weakness.[7] Respiratory paralysis in IMS if identified early can reduce the need for ventilator support and appropriate treatment can be initiated at the earliest.[8] Hence, identifying the patients at high risk for IMS may lead to a decrease in morbidity and mortality.
Various prognostic tools such as serum creatine phosphokinase (CPK), lactate dehydrogenase (LDH), serum immunoglobulins, and circulating complements for early detection of patients at high risk for developing respiratory failure have been tried.[9] There will be the elevation of serum CPK in OP poisoning due to myonecrosis caused by persistent depolarization at the neuromuscular junction and oxidative cellular damage to muscle membrane.[10,11] Serum CPK level has also been studied as a predictor for the onset of IMS, but in earlier studies CPK has been measured only at admission and/or prior to discharge.[12]
The objectives of our study were to measure serial serum CPK levels, correlate CPK levels with severity of poisoning and to record the total dose of atropine required.
Materials and Methods
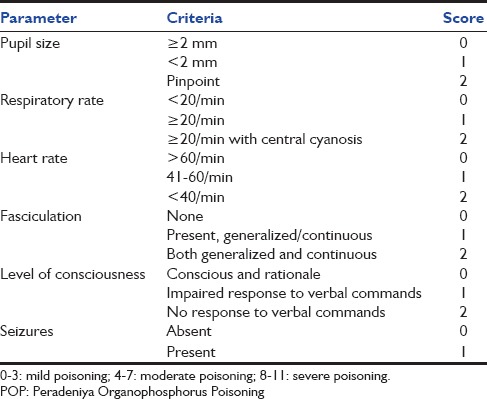
The protocol was approved by the Institutional Ethics Committee. Informed consent was obtained from all the patients if conscious or their relatives. This was an observational study conducted by the Departments of Pharmacology and Medicine from May 2013 to April 2014. Patients are aged 16 years and above, who reached the hospital within 6 h of exposure, with signs of mild to moderate OP poisoning were included. The severity of poisoning at admission was assessed using Peradeniya Organophosphorus Poisoning (POP) scale [Table 1].[13] Severe OP poisoning patients were excluded as seizures in them lead to elevation of serum CPK levels. Patients exposed to other drugs or substances with cholinergic activity, renal or hepatic diseases, and chronic alcoholism were also excluded from the study.
Table 1.
POP scale
Patients were treated according to standard treatment protocol of our hospital with atropine 3–5 ml (0.6 mg/ml) bolus followed by continuous infusion with titration based on clinical assessment, and pralidoxime 2 g bolus over 30 min followed by 1 g/h for 48 h. The total dose of atropine given to the patient till recovery was calculated. Data collected as per the proforma included type of poison, time since poisoning, and POP score. Serial serum CPK levels were estimated at admission, 48 and 96 h after poisoning. Treating physicians were blinded to serial serum CPK values. Serum pseudocholinesterase or butyrylcholinesterase (BChE) was measured at admission.
CPK was measured by using VITROS CPK microslide method, which uses the conversion of creatine phosphate to creatine and ATP. This assay is sensitive from 20 to 1600 IU/L of total CPK activity. For out of range samples “sample dilution” was done. The assay is precise with 2.4% co-efficient of variation when compared with VITROS 750, 950, and 5600 systems. BChE was measured by using VITROS cholinesterase microslide method, which uses butyrylthiocholine as a substrate. This assay is sensitive from 200 to 12,500 IU/L of butyrylcholinestrase activity. The assay is precise with 4.3% co-efficient of variation when compared with VITROS 750, 950, and 5600 systems. Both the parameters were measured in VITROS 250 dry chemistry analyzer (Johnson and Johnson). Both internal and external quality control were done during the assay process.
Statistical analysis
Demographic data was expressed as mean ± standard deviation, BChE levels were expressed as median and interquartile range. Serum CPK levels were correlated with POP scale, plasma BChE levels, and atropine dose using Pearson's correlation coefficient. Student t-test was used to test the significance between serial serum CPK values of patients without IMS and with IMS. The test for normality applied was Shapiro-Wilk for CPK distribution. The statistical software used was Epi Info 7 - manufactured by Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia (USA) and SPSS 22.0 Version- Manufactured by International Business Management (IBM) Corporation.
Results
Data were collected from 75 patients of which 43 (57%) were males and 32 (43%) females, with a mean age of 31.48 ± 11.76 years. The majority of them were farmers by occupation; others were students and housewives. Chlorpyriphos (24%) was the most common poison consumed followed by triazophos and methyl parathion 10.6% each and rest were combinations. The average time was taken to reach the hospital was 181.26 ± 89.53 min.
We observed that as the severity of the poisoning increased in respect to POP score, the serum CPK levels and total dose of atropine required for treatment also increased. The levels of BChE were reduced [Table 2]. Shapiro-Wilk normality test was applied for CPK distribution, it was not Gaussian distribution, probably the three patients with IMS had a mean CPK (IU/L) of 1837.33 ± 243.19, and in other 72 it was 214.81 ± 139.22. Table 3 shows the difference in serial CPK levels in patients without IMS and with IMS, it was observed that the difference in CPK between these patients was highly significant at baseline and 48 h, but not at 96 h.
Table 2.
POP score, BChE, initial CPK, and atropine (mg) dose
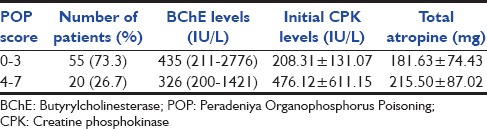
Table 3.
Serial serum CPK levels (IU/L)
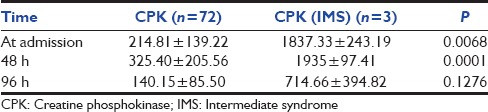
During the study, three patients with moderate poisoning developed IMS. CPK levels at 48 h in these patients were 2000 IU/L, 1982 IU/L, and 1823 IU/L, which is much higher than CPK levels in the patients without IMS. Among them, two patients needed mechanical ventilation for 3 and 5 days, respectively. The third patient developed tachypnea, weakness and fall in SPO2, so the patient was under observation in ICU for 24 h. All these three patients recovered completely, and their duration of stay in the hospital was 13, 21, and 5 days, respectively.
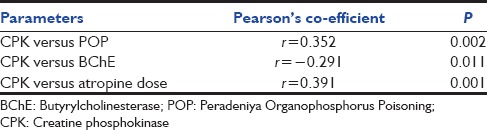
Figure 1 depicts the serial serum CPK levels, there was an increase in CPK levels at admission and 48 h, but reduced by 96 h. A weak positive correlation was observed between POP score and CPK levels, as well as CPK, and atropine dose. A negative correlation was observed between BChE and CPK levels [Table 4].
Figure 1.
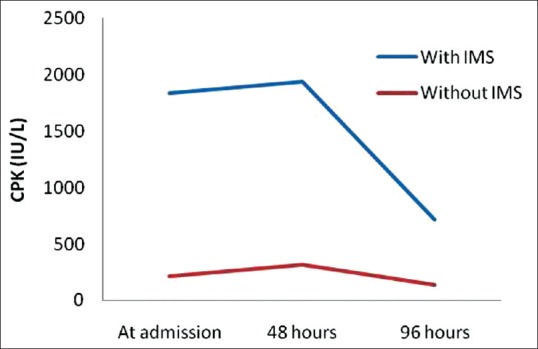
Serial serum creatine phosphokinase levels
Table 4.
Co-relation between POP, CPK, BChE, and atropine dose
Discussion
OP compounds are the most commonly used pesticides in agriculture. Because of their wide use and easy accessibility, poisoning with these compounds has emerged as an important health problem especially in developing countries. Acute OP poisoning can manifest with three different phases of toxicity namely acute cholinergic crisis, IMS, and OPIDN. Inhibition of acetylcholinesterase is the major mechanism of cholinergic crisis, which leads to stimulation of muscarinic and nicotinic receptors. Muscarinic features include excessive salivation, lacrimation, urination, diarrhea, gastrointestinal cramps, emesis, blurred vision, miosis, bradycardia, and wheezing. Nicotinic features include fasciculation, paresis or paralysis. Central receptor features include anxiety, confusion, psychosis, seizures, and ataxia.[9]
IMS is termed so because it occurs in the interval between the end of the acute cholinergic crisis and OPIDN. Studies have shown that IMS occurred between 48 and 96 h after acute poisoning and is characterized by weakness of proximal limb muscles, neck flexors, respiratory muscles, and is attributed to muscle fiber necrosis. Reversible myocyte injury results in increased muscle enzymes such as myoglobin, LDH, troponin, and CPK. Serum CPK rises in 6 h following muscle injury and remains elevated for 5–6 days.[14]
Patients in our study were in the third decade who would contribute to the economic status of the family. Various reasons contributing for consumption of poison were a financial loss, family disputes, and stress. Chlorpyriphos was most commonly consumed as it is the widely used pesticide in our area. There was a delay in patient reaching the hospital, which could be attributed to lack of transport facility in rural areas.
Mild and moderate OP poisoning patients had elevated serum CPK level at least in one of the three serial measurements. These findings were similar to other studies where they have tried to develop serum CPK as a tool for diagnosing the severity of OP poisoning and also as a prognostic marker for the recovery from OP poisoning.[15] Another study has shown raised serum CPK level only in a fraction of their patients who had severe poisoning.[16]
We have observed that three patients with IMS had marked elevation of CPK at baseline and 48 h and required intensive care. Similar findings were observed in other studies, where the serum CPK levels were more than 10,000 IU/L in moderate to severe poisoning, and they had recovered completely.[15] In our study, a weak positive correlation was observed between serum CPK levels, POP score, and dose of atropine, but another study has shown a strong positive correlation.[15]
These observations suggest that there is a direct relation between serum CPK levels and IMS. Hence, it is necessary for estimating CPK levels, especially after 48 h, in moderate to severe poisoning patients, so that IMS can be recognized at the earliest and patients can be referred to higher centers for immediate management of respiratory failure, reducing morbidity and mortality. Limitations: Incidence of IMS is higher in severe OP poisoning patients who were not included in our study. The possible reasons being these patients may require early ventilator support due to the severe cholinergic crisis itself and also they may manifest with convulsion, which will predispose to increase in CPK levels.
IMS is an important complication associated with OP poisoning, which worsens the prognosis, as it can cause respiratory failure requiring intubation. Even though we have observed IMS in only three patients, the CPK in these patients was more than 1500 IU/L at baseline, and it persisted or increased at 48 h. The correlation of CPK and IMS should be explored in a larger, prospective study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Batra AK, Keoliya AN, Jadhav GU. Poisoning: An unnatural cause of morbidity and mortality in rural India. J Assoc Physicians India. 2003;51:955–9. [PubMed] [Google Scholar]
- 2.Indian Council of Medical Research. Pesticide pollution trends and perspectives. Indian Counc Med Res Bull. 2001;31:367–71. [Google Scholar]
- 3.Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, et al. Suicide mortality in India: A nationally representative survey. Lancet. 2012;379:2343–51. doi: 10.1016/S0140-6736(12)60606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banerjee I, Tripathi S, Roy AS. Clinico-epidemiological characteristics of patients presenting with organophosphorus poisoning. N Am J Med Sci. 2012;4:147–50. doi: 10.4103/1947-2714.93884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poojara L, Vasudevan D, Kumar AS, Kamath V. Organophosphate poisoning: Diagnosis of intermediate syndrome. Indian J Crit Care Med. 2003;7:94–102. [Google Scholar]
- 6.Kalyanam B, Narayana S, Kamarthy P. A rare neurological complication of acute organophosphorous poisoning. Toxicol Int. 2013;20:189–91. doi: 10.4103/0971-6580.117270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jayawardane P, Dawson AH, Weerasinghe V, Karalliedde L, Buckley NA, Senanayake N. The spectrum of intermediate syndrome following acute organophosphate poisoning: A prospective cohort study from Sri Lanka. PLoS Med. 2008;5:e147. doi: 10.1371/journal.pmed.0050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang CC, Deng JF. Intermediate syndrome following organophosphate insecticide poisoning. J Chin Med Assoc. 2007;70:467–72. doi: 10.1016/S1726-4901(08)70043-1. [DOI] [PubMed] [Google Scholar]
- 9.Sen R, Nayak J, Khadanga S. Study of serum cholinesterase, CPK and LDH as prognostic biomarkers in organophosphorus poisoning. Int J Med Res Rev. 2014;2:185–9. [Google Scholar]
- 10.John M, Oommen A, Zachariah A. Muscle injury in organophosphorous poisoning and its role in the development of intermediate syndrome. Neurotoxicology. 2003;24:43–53. doi: 10.1016/s0161-813x(02)00111-0. [DOI] [PubMed] [Google Scholar]
- 11.Dandapani M, Zachariah A, Kavitha MR, Jeyaseelan L, Oommen A. Oxidative damage in intermediate syndrome of acute organophosphorous poisoning. Indian J Med Res. 2003;117:253–9. [PubMed] [Google Scholar]
- 12.Nermeen AM, Hassan, Madboly AG. Correlation between serum creatine phosphokinase and severity of acute organophosphorus poisoning: A prospective clinical study (2012–2013) J Environ Sci Tox Food Technol. 2013;4:18–29. [Google Scholar]
- 13.Senanayake N, de Silva HJ, Karalliedde L. A scale to assess severity in organophosphorus intoxication: POP scale. Hum Exp Toxicol. 1993;12:297–9. doi: 10.1177/096032719301200407. [DOI] [PubMed] [Google Scholar]
- 14.Sahjian M, Frakes M. Crush injuries: Pathophysiology and current treatment. Nurse Pract. 2007;32:13–8. doi: 10.1097/01.NPR.0000287464.81259.8b. [DOI] [PubMed] [Google Scholar]
- 15.Bhattacharyya K, Phaujdar S, Sarkar R, Mullick OS. Serum creatine phosphokinase: A probable marker of severity in organophosphorus poisoning. Toxicol Int. 2011;18:117–23. doi: 10.4103/0971-6580.84263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aygun D, Erenler AK, Karatas AD, Baydin A. Intermediate syndrome following acute organophosphate poisoning: Correlation with initial serum levels of muscle enzymes. Basic Clin Pharmacol Toxicol. 2007;100:201–4. doi: 10.1111/j.1742-7843.2007.00042.x. [DOI] [PubMed] [Google Scholar]


