Abstract
Background
The few previous studies on the onset of paroxysmal atrial fibrillation and meteorologic conditions have focused on outdoor temperature and hospital admissions, but hospital admissions are a crude indicator of atrial fibrillation incidence, and studies have found other weather measures in addition to temperature to be associated with cardiovascular outcomes.
Methods
Two hundred patients with dual chamber implantable cardioverter-defibrillators were enrolled and followed prospectively from 2006 to 2010 for new onset episodes of atrial fibrillation. The date and time of arrhythmia episodes documented by the implanted cardioverter-defibrillators were linked to meteorologic data and examined using a case-crossover analysis. We evaluated associations with outdoor temperature, apparent temperature, air pressure, and three measures of humidity (relative humidity, dew point, and absolute humidity).
Results
Of the 200 enrolled patients, 49 patients experienced 328 atrial fibrillation episodes lasting ≥30 seconds. Lower temperatures in the prior 48 hours were positively associated with atrial fibrillation. Lower absolute humidity (ie, drier air) had the strongest and most consistent association: each 0.5 g/m3 decrease in the prior 24 hours increased the odds of atrial fibrillation by 4% (95% confidence interval [CI]: 0%, 7%) and by 5% (95% CI: 2%, 8%) for exposure in the prior 2 hours. Results were similar for dew point but slightly weaker.
Conclusions
Recent exposure to drier air and lower temperatures were associated with the onset of atrial fibrillation among patients with known cardiac disease, supporting the hypothesis that meteorologic conditions trigger acute cardiovascular episodes.
A trial fibrillation is the most common arrhythmia in the US1 and is projected to affect up to 16 million people by 2050 due to the aging of the population and improved survival following myocardial infarction and congestive heart failure.2,3 Atrial fibrillation is frequently asymptomatic and the potential adverse consequences (eg, stroke, thromboembolism, heart failure, sudden cardiac death) often occur before it is diagnosed.2,4–7 Given the expected increase in prevalence of atrial fibrillation and the involvement of atrial fibrillation in a variety of cardiovascular disease processes, prevention of these episodes may have substantial public health implications, namely a reduction in atrial fibrillation-related morbidity, mortality, and healthcare costs.2
In both temperate8–12 and warmer Mediterranean and subtropical climates,5,9 paroxysmal atrial fibrillation displays a seasonal pattern and peaks in the colder months. This observation has led to the hypothesis that meteorologic conditions may trigger attacks of acute atrial fibrillation. Several studies have examined this hypothesis and have found an association with winter or lower outdoor temperatures5,8,11 or no association.10 All of these studies focused on hospital admissions for atrial fibrillation. Because atrial fibrillation is often asymptomatic, studies of symptomatic episodes that cause presentation to a hospital are likely a small percentage of atrial fibrillation events, and the delay between initiation of atrial fibrillation and hospital presentation is of variable duration and often unknown, leading to temporal misalignment and underestimation of any true association.13 Furthermore, these studies5,8,11 focused on outdoor temperature, but other meteorologic factors, such as humidity and air pressure, have been reported to be associated with adverse cardiovascular outcomes.14–16
We examined the association between meteorologic conditions and paroxysmal atrial fibrillation in a prospective cohort of patients implanted with dual chamber implantable cardioverter-defibrillator devices. These devices are capable of recording the date, time, and real-time electrocardiograms of atrial and ventricular arrhythmias, thereby allowing for a complete, objective record of all detected arrhythmias. We evaluated six outdoor weather measures: temperature, apparent temperature, air pressure, relative humidity, dew point, and absolute humidity. We focused on the 72 hours before atrial fibrillation onset. Studies of cold stress and incident cardiac events consistently find a 2- to 3-day lag between the time of exposure and event.17
METHODS
Patient Population
Participants were recruited and enrolled between November 2006 and March 2010 from patients followed at the Tufts Medical Center Cardiac Arrhythmia Center in Boston, MA. Patients were eligible for enrollment if they were implanted with a dual (ie, atrial and ventricular) chamber implantable cardioverter-defibrillator, ages 18 years or older, regularly followed-up at Tufts Medical Center, not in permanent atrial fibrillation, did not have a terminal illness, and were able to give informed consent. This study was originally designed to examine the relation between air pollution and arrhythmia, so all patients had residential zip codes within 50 km of the Harvard Supersite air quality monitoring station. The study protocol and informed consent were approved by the institutional review boards at Tufts Medical Center and the Harvard School of Public Health.
At the baseline visit, patients completed an interviewer-administered questionnaire on sociodemographic characteristics, medical history, medication use, and lifestyle, and were measured for height and weight. Additional information on past and current medical history was collected by study coordinators from a review of medical records.
Arrhythmias
Participants were followed every 3 months from study enrollment until June 30, 2010. Implantable cardioverter-defibrillator data, including the arrhythmia logbook and electrograms, were downloaded either at clinic visits at Tufts Medical Center or by trans-telephonic transmission. Arrhythmias documented by the device were reviewed and interpreted by an electrophysiologist (M.S.L.) and characterized as ventricular, sinus tachycardia, atrial fibrillation, atrial arrhythmia other than atrial fibrillation, or not an arrhythmia. In accordance with the American Heart Association, the American College of Cardiology and the Heart Rhythm Society definition of clinically relevant atrial fibrillation as episodes lasting ≥30 seconds,18 we restricted our analyses to atrial fibrillation episodes lasting at least 30 seconds. To reduce the possibility of over-representation of clustered events, atrial fibrillation episodes were included in the analysis if at least 1 hour had passed since the previous atrial fibrillation episode. We excluded episodes that occurred within 6 weeks following device implantation and excluded patients with <90 days of follow-up.
Meteorological and Air Quality Data
Hourly surface observations of outdoor temperature (°C), air pressure (hPa), relative humidity (%), and dew point (°C) were made at Boston Logan International Airport and extracted from National Weather Service records. Apparent temperature (°C) and absolute humidity (g/m3) were calculated from the temperature, relative humidity, and dew point.19,20 Apparent temperature is a measure of what a given temperature and humidity combination feels like to the typical person. Air pressure is the force exerted by the weight of air. Relative humidity is the ratio of the amount of water vapor present in the air relative to the amount of water vapor needed for saturation at the current temperature, expressed as a percentage, and is thus a temperature-dependent measure. Unlike relative humidity, dew point and absolute humidity are measures of the actual moisture content in the air (ie, are not relative measures). The dew point is the temperature to which air must be cooled to reach saturation. Absolute humidity expresses water vapor content in the air as a density, usually as g/m3. Moving averages for the past 2, 24, 48, and 72 hours were calculated if at least 75% of the hourly measurements were available; otherwise, we considered the exposure missing.
A previous study examining air pollutants and atrial fibrillation in this cohort found that exposure to particulate matter <2.5 μm in aerodynamic diameter (PM2.5) in the previous 2 hours was associated with atrial fibrillation.21 PM2.5 was measured hourly at a Harvard Supersite monitor located on the roof of the Countway Library 5 km from Tufts Medical Center using a Tapered Element Oscillating Microbalance (TEOM, Rupprecht and Patashnick, East Greenbush, New York).
Statistical Analysis
In a case-crossover design, exposures before the time of the event (case period) are compared with the distribution of exposures estimated from reference periods using conditional logistic regression. This matched design allows for each patient to serve as his or her control.22 The time of event onset was rounded to the nearest hour and linked to the corresponding hourly weather and PM2.5 value. We selected reference periods (three to four per case period) using a bidirectional time-stratified approach that matched the case period on month, day of the week, and hour of the day. In a case-crossover design, the relevant exposure term is the difference between exposure during the case period and the average exposure during the reference periods.23 We calculated the daily correlations (Pearson’s r) and the correlations for the differences in 2-hour-average exposure within matched sets between the meteorologic variables and PM2.5. Results are reported as the percent increased odds (odds ratio minus 1 times 100) for a decrease of 1°C in temperature, apparent temperature, and dew point, 3% in relative humidity, 0.5 g/m3 in absolute humidity, and 2 hPa for air pressure. We chose these increments because at 50% relative humidity, a drop in temperature from 20°C to 19°C lowers absolute humidity by 0.49 g/m3 and the dew point by 0.92°C. At 20°C and 50% relative humidity, lowering the dew point by 0.92°C while keeping the temperature constant lowers relative humidity by 3%. The increment for air pressure was chosen so as to have results similar in magnitude to the other variables. Each meteorologic variable was analyzed in separate models, and all analyses adjusted for PM2.5 in the previous 2 hours as a linear term.
We assessed the shape of the exposure–response relationships using penalized regression splines and likelihood ratio tests. We then examined whether the results were driven by patients experiencing many events (≥10 vs. <10) and whether the results changed without adjustment for PM2.5. We examined potential effect modification by demographics (gender, race, age), clinical history of atrial fibrillation, and environmental factors (air conditioner, humidifier, and season). Effect modification was assessed using an interaction term between the exposure and potential modifier. Effect sizes and confidence intervals (CIs) were obtained from stratified analyses. SAS version 9.2 (SAS Institute; Cary, NC) was used to construct datasets and to calculate descriptive statistics. R version 2.15.3 (R Foundation for Statistical Computing; Vienna, Austria) was used for all statistical analysis.
RESULTS
Study Population
Of 1,143 patients screened for participation, 300 were eligible to participate. The most common reasons for exclusion were for having a single chamber implantable cardioverter-defibrillator (n = 502), living >50 km away from the Harvard Supersite air quality monitoring station (n = 345), and for chronic atrial fibrillation (n = 84). Two hundred patients were enrolled (66%), of which 176 patients were followed for at least 90 days (mean follow-up time: 1.9 years) and 49 patients had 328 atrial fibrillations lasting at least 30 seconds. All subjects lived within 55 km of the Logan Airport (median = 26 km).
Patients with confirmed episodes of atrial fibrillation lasting at least 30 seconds were pre-dominantly white males with an average age of 68 years (total range: 35–88 years; Table 1). About 50% had a history of atrial fibrillation, and the majority had a history of myocardial infarction, congestive heart failure, revascularization, or ischemic heart disease. The average left ventricular ejection fraction among these patients was 31% (total range: 10%–70%). Most patients received the implantable cardioverter-defibrillator for primary prevention of sudden cardiac death and were on standard pharmacologic therapies for ischemic and nonischemic cardiomyopathies (ie, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and beta blockers). Almost all patients had air conditioning in their homes. Fifteen patients experienced a single episode of atrial fibrillation during follow-up, 13 had two to four, and 21 patients had five or more events during follow-up.
TABLE 1.
Characteristics of 49 Patients with 328 Confirmed Atrial Fibrillation Episodes
| Number of Patientsa | Number of Episodes ≥ 30 Secondsa | |
|---|---|---|
| Male | 33 (67%) | 253 (77%) |
| Race/ethnicity | ||
| White | 47 (96%) | 310 (95%) |
| Black | 2 (4%) | 18 (6%) |
| History of atrial fibrillation | 24 (49%) | 204 (62%) |
| Previous myocardial infarction | 28 (62%) | 205 (66%) |
| Previous stroke | 5 (10%) | 24 (7%) |
| History of congestive heart failure | 31 (63%) | 275 (84%) |
| History of revascularization | ||
| Coronary artery bypass grafting | 15 (31%) | 145 (44%) |
| Percutaneous coronary intervention | 13 (27%) | 69 (21%) |
| Comorbidities | ||
| Pulmonary disease | 13 (27%) | 66 (20%) |
| Diabetes | 13 (27%) | 112 (34%) |
| Hypertension | 27 (56%) | 197 (62%) |
| Indications for implant | ||
| Primary | 31 (63%) | 199 (61%) |
| Secondary (cardiac arrest or sustained ventricular tachycardia) | 7 (14%) | 29 (9%) |
| Syncope apparently arrhythmic | 11 (23%) | 100 (31%) |
| Structural heart disease | ||
| Ischemic | 30 (61%) | 225 (69%) |
| Non-ischemic | 10 (20%) | 35 (11%) |
| Other | 9 (18%) | 68 (21%) |
| History of sleep apnea | 7 (16%) | 92 (30%) |
| Obese (body mass index ≥ 30) | 15 (31%) | 137 (42%) |
| Medications | ||
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blocker | 41 (87%) | 311 (96%) |
| Beta blocker | 43 (92%) | 313 (97%) |
| Anti-arrhythmic agents | 10 (21%) | 117 (36%) |
| Platelet aggregation inhibitors | 31 (66%) | 153 (47%) |
| Statin | 38 (81%) | 264 (82%) |
| Air conditioning use | ||
| Central | 15 (33%) | 155 (53%) |
| Window | 28 (61%) | 121 (41%) |
| None | 3 (7%) | 19 (6%) |
| Use of a humidifier | 8 (17%) | 85 (29%) |
Values are n (%).
Percents may not add up to 100 due to rounding. Missing values (patients, events): previous myocardial infarction, n = (4, 16); previous stroke, n = (1, 1); pulmonary disease, n = (1, 1); history of sleep apnea, n = (4, 24); medications, n = (2, 4); air conditioning use, n = (3, 33); use of a humidifier, n = (3, 33).
Meteorological Conditions
Boston experienced a wide range of temperature and absolute humidity, from −13.8°C to 29.8°C and 0.6 g/m3 to 20 g/m3 (Table 2). Daily temperature, apparent temperature, dew point, and absolute humidity are strongly correlated to one another (Pearson r’s ≥ 0.89). The correlation between other meteorologic variables and PM2.5 is modest to low (Pearson r’s ≤ 0.55). Similarly for the exposure difference within matched sets (Appendix Table), the 2-hour-average temperature, apparent temperature, dew point, and absolute humidity were strongly correlated to each other (Pearson r’s ≥ 0.62) and weakly correlated to PM2.5 (Pearson r’s ≤ 0.36).
TABLE 2.
Summary Statistics and Pearson Correlation Coefficients of Daily Meteorologic Variables and Air Pollution in Boston from September 1, 2006, to June 30, 2010
| Parameter | # Days | Min | 25th | 50th | 75th | Max | Pearson Correlation Coefficient, r
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | AT | AP | RH | DP | AH | PM2.5 | |||||||
| T (°C) | 1,398 | −13.8 | 3.4 | 11.0 | 18.3 | 29.8 | 1 | 1 | −0.13 | 0.19 | 0.92 | 0.89 | 0.31 |
| AT (°C) | 1,398 | −13.8 | 2.9 | 9.9 | 17.9 | 31.6 | 1 | −0.14 | 0.22 | 0.93 | 0.91 | 0.33 | |
| AP (hPa) | 1,398 | 985.7 | 1,009.0 | 1,014.3 | 1,020.2 | 1,038.5 | 1 | −0.22 | −0.19 | −0.19 | 0 | ||
| RH (%) | 1,398 | 22.0 | 52.2 | 64.6 | 77.5 | 98.3 | 1 | 0.55 | 0.51 | 0.21 | |||
| DP (°C) | 1,398 | −26.1 | −3.7 | 4.1 | 11.9 | 22.8 | 1 | 0.96 | 0.34 | ||||
| AH (g/m3) | 1,398 | 0.63 | 3.7 | 6.4 | 10.4 | 20.0 | 1 | 0.40 | |||||
| PM2.5 (μg/m3) | 1,213 | 0.15 | 5.3 | 7.2 | 10.2 | 53.2 | 1 | ||||||
T indicates temperature; AT, apparent temperature; AP, air pressure; RH, relative humidity; DP, dew point; AH, absolute humidity; PM2.5, particulate matter < 2.5 μm in aerodynamic diameter.
APPENDIX TABLE.
Pearson Correlation Coefficients Between the Difference in 2-Hour Average Meteorological and Air Pollution Exposure Within Matched Sets (ie, the Difference Between Exposure During Case Periods and the Average Exposure During Reference Periods)
| T | AT | AP | RH | DP | AH | PM2.5 | |
|---|---|---|---|---|---|---|---|
| T | 1 | 0.99 | −0.25 | 0.06 | 0.69 | 0.62 | 0.26 |
| AT | 1 | −0.26 | 0.11 | 0.72 | 0.67 | 0.28 | |
| AP | 1 | −0.34 | −0.38 | −0.37 | 0.02 | ||
| RH | 1 | 0.75 | 0.67 | 0.20 | |||
| DP | 1 | 0.90 | 0.32 | ||||
| AH | 1 | 0.36 | |||||
| PM2.5 | 1 |
T indicates temperature; AT, apparent temperature; AP, air pressure; RH, relative humidity; DP, dew point; AH, absolute humidity; PM2.5, particulate matter < 2.5 μm in aerodynamic diameter.
Meteorology and Atrial Fibrillation
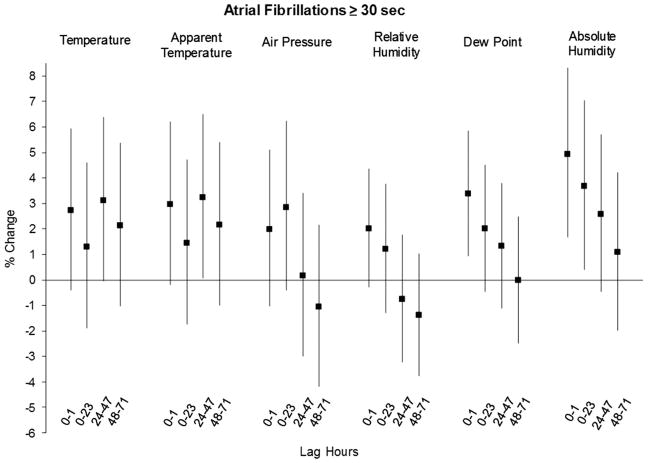
After excluding 23 episodes with missing PM2.5 information, analyses were confined to 47 patients and 305 atrial fibrillation episodes. Lower temperatures increased the odds of atrial fibrillation and were most strongly associated with exposure 48 hours prior (Figure). The odds of atrial fibrillation were increased by 3% (95% CI: 0%, 6%) and 3% (95% CI: 0%, 7%) per 1°C decrease in temperature and apparent temperature, respectively. Associations for air pressure and relative humidity were inconsistent. Both measures of the actual moisture content in the air—dew point and absolute humidity— were positively associated with atrial fibrillation. Each 1°C decrease in dew point in the prior 2 hours (lag 0–1 hours) increased the odds by 3% (95% CI: 1%, 6%). We observed the strongest and most consistent association for lower absolute humidity; each 0.5 g/m3 decrease in the prior 24 hours increased the odds by 4% (95% CI: 0%, 7%) and by 5% (95% CI: 2%, 8%) for exposure in the prior 2 hours. Dew point and absolute humidity also displayed a temporal pattern of weaker effects with increasing time since the atrial fibrillation event.
We examined the shape of the associations for each meteorologic variable using the averaging time most strongly related to atrial fibrillation (eg, lag 0–1 hours for absolute humidity, lag 24–47 hours for temperature, etc.). Likelihood ratio tests comparing a penalized spline model to a linear model indicated that a linear fit was adequate for all exposures. Based on these results, we focused on absolute humidity in the prior 2 hours in all further analyses.
In analyses comparing 40 patients who had <10 events (n = 140 episodes) to seven patients who had ≥10 events (n = 164 episodes) during follow-up, the association with absolute humidity in the prior 2 hours was identical (5%; 95% CI: 0%, 10%, and 5%; 95% CI: 1%, 9%, respectively). Without adjustment for PM2.5, the association for absolute humidity in the prior 2 hours attenuated slightly (3%; 95% CI: 0%, 6%).
Older patients and patients with no history of atrial fibrillation appeared to be more sensitive to lower absolute humidity (Table 3).
TABLE 3.
Percent Change in the Odds of Atrial Fibrillation for Each 0.5 g/m3 Decrease in Average Absolute Humidity in the Prior 2 Hours, Stratified by Potential Effect Modifier
| Effect Modifier | No. of Patients | No. of Arrhythmias | % Change | 95% Confidence Interval |
|---|---|---|---|---|
| Gender | ||||
| Male | 32 | 238 | 6% | 2%, 9% |
| Female | 15 | 66 | 2% | −6%, 10% |
| Race | ||||
| White | 45 | 287 | 5% | 1%, 8% |
| Black | 2 | 17 | 9% | −4%, 23% |
| Age (years) | ||||
| <65 | 17 | 98 | −2% | −8%, 4% |
| ≥65 | 30 | 206 | 8% | 4%, 12% |
| History of atrial fibrillation | ||||
| Yes | 24 | 191 | 3% | −1%, 7% |
| No | 23 | 113 | 9% | 3%, 15% |
| Air conditioninga | ||||
| Central | 9 | 52 | 9% | 2%, 17% |
| Window | 13 | 48 | 14% | 4%, 25% |
| None | 2 | 6 | 10% | −25%, 62% |
| Use of a humidifier | ||||
| Yes | 8 | 81 | 5% | −1%, 11% |
| No | 36 | 192 | 4% | 0%, 9% |
| Season | ||||
| Cold (Nov–Mar) | 34 | 121 | 3% | −3%, 10% |
| Warm (May–Sept) | 27 | 120 | 10% | 5%, 16% |
Analyses are restricted to the warm season (May–September).
DISCUSSION
Among a cohort of patients with known cardiac disease at high risk for subclinical and clinical cardiac events, a decrease in absolute humidity of 0.5 g/m3 in the previous 2 hours increased the odds of atrial fibrillation by 5%. Stated another way, a small drop in absolute humidity equivalent to lowering relative humidity from 50% to 47% at a constant temperature of 20°C (68°F) increased the odds of atrial fibrillation by 5%. Dew point and absolute humidity are both measures of the actual moisture content in the air, so it is not surprising that we observed a similar pattern of associations for dew point. Lower temperature and apparent temperature were also positively associated with atrial fibrillation, particularly in the prior 48 hours.
Previous studies relating meteorologic conditions to atrial fibrillation focused on hospital admissions, which likely miss atrial fibrillation episodes with mild or no symptoms. Furthermore, the variable delay time between arrhythmia onset and hospital presentation will lead to temporal misalignment of the exposure and outcome, which leads to considerable bias toward observing no association when a true association exists.13 An advantage of this study is our ability to detect and identify the time of onset of all atrial fibrillations, including asymptomatic episodes. Earlier studies tended to focus on outdoor temperature, which may have missed associations with other meteorologic conditions. We examined several weather measures and found atrial fibrillation to be related to both temperature and humidity. Previous studies also did not adjust for confounding by air pollution. Several studies have reported an association between air pollution and atrial fibrillation onset.21,24,25 In this study, not adjusting for PM2.5 attenuated the association for absolute humidity.
Consistent with previous studies,5,8,11 we observed a negative association between temperature and atrial fibrillation. Gluszak et al10 examined atrial fibrillation in relation to several meteorologic conditions and found no association with temperature, air pressure, or relative humidity. Studies of supraventricular tachycardia and supraventricular premature beats have found associations with higher relative humidity and higher air pressure,26,27 which conflicts with our results. Although we observed associations for several weather measures, it is unclear whether or not a measure is acting as a marker for another exposure. Outdoor weather conditions are highly correlated, and the relation between indoor and outdoor conditions is not straightforward. In Boston, outdoor absolute humidity tracks closely with indoor absolute humidity, but also tracks with indoor temperature, apparent temperature, and relative humidity. Similarly, outdoor temperatures correlate strongly with indoor temperatures, but also with indoor apparent temperature and absolute humidity. Further complicating the interpretation of these results is the fact that outdoor and indoor temperatures in Boston correlate weakly in the colder months because of universal home heating.28 Nguyen et al29 found a nonlinear association between outdoor temperature and ventricular arrhythmias in a cohort of patients implanted with cardioverter-defibrillators living in Boston, which they attributed to the poor correlation between outdoor and indoor temperatures during the winter months. It is possible that the current study did not have sufficient power to detect a nonlinear association for temperature.
We observed a stronger association between lower absolute humidity and atrial fibrillation among older patients and patients without a clinical history of atrial fibrillation. The elderly are especially sensitive to cold, dry air.30,31 They have lower metabolic heat production and are more prone to develop disorders of thermoregulatory function.32 In general, about 90% of paroxysmal atrial fibrillations are thought to be triggered by muscular sleeves in the pulmonary veins.33 As atrial fibrillation progresses, atrial substrates formed through electrical, contractile, and structural remodeling34,35 play a more important role in onset.33 This may be why we observed a stronger association for absolute humidity among patients without a history of atrial fibrillation; episodes in these patients may be more likely triggered by external factors rather than abnormalities in atrial tissue.
The mechanisms for how outdoor ambient meteorologic conditions affect human physiologic responses remain to be clarified, considering that people in industrialized countries spend about 90% of their time indoors. The most likely explanation is that outdoor weather conditions are serving as proxies for indoor temperature and humidity levels. Exposure to colder temperatures and drier air induces thermoregulation processes36 that activate both the sympathetic nervous system and the coagulation system.17 Regardless of ambient conditions, inspired air is conditioned to 37°C and 100% relative humidity in the respiratory tract. This process results in substantial heat and water loss in the larger airways.37 A s the temperature and/or water content of inspired air decreases, the degree of airway cooling and drying increases and moves to more central airways.38 Changes in air temperature trigger a sympathetic reflex that strengthens with lower temperature. Reflex-mediated vasoconstriction limits heat loss by redistributing blood to the core and causes an increase in cardiac output that supports higher metabolic production.17 These processes increase sympathetic drive, peripheral arterial resistance, blood pressure, central blood volume, and ventricular filling pressure, which could result in increased left atrial distention and promote the propensity of the atria to fibrillate.11,17
There are several limitations to this study. Using outdoor weather measures as indicators of exposure suffers from nondifferential misclassification of exposure and attenuates associations to the null. We adjusted for potential confounders using the case-crossover design and statistical analysis, but the influence of unknown confounders that vary quickly over time (eg, physical exertion, diet, alcohol consumption, mental or emotional stress) cannot be ruled out. Some of the results presented here may due to chance; we evaluated six weather measures using four different averaging times. However, the consistent adverse association of lower temperature and apparent temperature and the stronger association at shorter lag times for dew point and absolute humidity make it unlikely that these results are entirely due to chance.
Strengths of this study include the prospective design, which allowed collection of detailed data on medical, behavioral, and housing characteristics, the complete ascertainment of outcomes using implantable cardioverter-defibrillator records which likely minimized the potential for selection bias, and the ability to adjust for air pollution. The extent to which our results generalize to other patients or to other geographies is unclear. Although we studied a cohort of high-risk patients, our results were consistent with previous studies on the same topic that instead focused on hospitalizations (which includes both high risk and asymptomatic patients), which suggests that our findings may be generalizable to patients without severe cardiac disease. However, the effect of colder temperatures on cardiac outcomes is not consistent between study populations. Differences in housing quality, clothing worn, culture, and time spent outdoors may partly explain this heterogeneity.39,40 Interestingly, absolute humidity was recently reported to be more consistently predictive of summertime cause-specific mortality than temperature, apparent temperature, or dew point across cities with different climates,40 so our results for absolute humidity may generalize to other patient groups and climates.
FIGURE.
Percent change in the odds of atrial fibrillation associated with lower outdoor temperatures, air pressure, and humidity as a function of moving and lagged averages in the prior 72 hours. Lower temperature and apparent temperature in the prior 48 hours were positively associated with atrial fibrillation. Absolute humidity in the prior 2 hours had the strongest association; fibrillation the odds of atrial increased by 5% (95% confidence interval: 2%, 8%) for each decrease of 0.5 g/m3. Dew point and absolute humidity displayed a temporal pattern of weaker effects with increasing time since the atrial fibrillation event.
Acknowledgments
Supported by National Institute of Environmental Health Sciences (NIEHS) Grants PO1 ES009825, P30 ES000002, R21ES020194-01, and T32ES007069, and by the Environmental Protection Agency-Harvard Clean Air Research Center (R83479801). These grants partially supported Drs. Nguyen, Luttmann-Gibson, Laden, Schwartz, Mittleman, Gold, and Dockery. Dr. Nguyen was also supported by NIEHS Grant T32ES023770.
The authors would like to thank Michaela Kapp, Melanie E. Marshall, Robert Paninski, and Brandon Udelhofen for their contributions to patient enrollment, follow-up, and data collection.
Footnotes
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com). This content is not peer-reviewed or copy-edited; it is the sole responsibility of the authors.
All other authors report no conflicts of interest.
References
- 1.Thomas G, Lerman BB. Prediction of stroke risk in atrial fibrillation, prevention of stroke in atrial fibrillation, and the impact of long-term monitoring for detecting atrial fibrillation. Curr Atheroscler Rep. 2011;13:290–297. doi: 10.1007/s11883-011-0188-x. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Chen PS, Bild DE, et al. Prevention of atrial fibrillation: report from a National Heart, Lung, and Blood Institute workshop. Circulation. 2009;119:606–618. doi: 10.1161/CIRCULATIONAHA.108.825380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–1046. doi: 10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 4.Healey JS, Connolly SJ, Gold MR, et al. ASSERT Investigators. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366:120–129. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 5.Kiu A, Horowitz JD, Stewart S. Seasonal variation in AF-related admissions to a coronary care unit in a “hot” climate: fact or fiction? J Cardiovasc Nurs. 2004;19:138–141. doi: 10.1097/00005082-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Lip GY. Stroke in atrial fibrillation: epidemiology and thromboprophylaxis. J Thromb Haemost. 2011;9(Suppl 1):344–351. doi: 10.1111/j.1538-7836.2011.04302.x. [DOI] [PubMed] [Google Scholar]
- 7.Sinnaeve PR, Brueckmann M, Clemens A, Oldgren J, Eikelboom J, Healey JS. Stroke prevention in elderly patients with atrial fibrillation: challenges for anticoagulation. J Intern Med. 2012;271:15–24. doi: 10.1111/j.1365-2796.2011.02464.x. [DOI] [PubMed] [Google Scholar]
- 8.Frost L, Johnsen SP, Pedersen L, et al. Seasonal variation in hospital discharge diagnosis of atrial fibrillation: a population-based study. Epidemiology. 2002;13:211–215. doi: 10.1097/00001648-200203000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Fustinoni O, Saposnik G, Esnaola y Rojas MM, Lakkis SG, Sposato LA ReNACer Investigators. Higher frequency of atrial fibrillation linked to colder seasons and air temperature on the day of ischemic stroke onset. J Stroke Cerebrovasc Dis. 2013;22:476–481. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Głuszak A, Kocoń S, Zuk K, Aljabali P, Gluza A, Siwek K. Episodes of atrial fibrillation and meteorological conditions. Kardiol Pol. 2008;66:958–963. discussion 964. [PubMed] [Google Scholar]
- 11.Kupari M, Koskinen P. Seasonal variation in occurrence of acute atrial fibrillation and relation to air temperature and sale of alcohol. Am J Cardiol. 1990;66:1519–1520. doi: 10.1016/0002-9149(90)90549-g. [DOI] [PubMed] [Google Scholar]
- 12.Watanabe E, Kuno Y, Takasuga H, et al. Seasonal variation in paroxysmal atrial fibrillation documented by 24-hour Holter electrocardiogram. Heart Rhythm. 2007;4:27–31. doi: 10.1016/j.hrthm.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 13.Lokken RP, Wellenius GA, Coull BA, et al. Air pollution and risk of stroke: underestimation of effect due to misclassification of time of event onset. Epidemiology. 2009;20:137–142. doi: 10.1097/ede.0b013e31818ef34a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abrignani MG, Corrao S, Biondo GB, et al. Effects of ambient temperature, humidity, and other meteorological variables on hospital admissions for angina pectoris. Eur J Prev Cardiol. 2012;19:342–348. doi: 10.1177/1741826711402741. [DOI] [PubMed] [Google Scholar]
- 15.Dilaveris P, Synetos A, Giannopoulos G, Gialafos E, Pantazis A, Stefanadis C. CLimate Impacts on Myocardial infarction deaths in the Athens TErritory: the CLIMATE study. Heart. 2006;92:1747–1751. doi: 10.1136/hrt.2006.091884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Houck PD, Lethen JE, Riggs MW, Gantt DS, Dehmer GJ. Relation of atmospheric pressure changes and the occurrences of acute myocardial infarction and stroke. Am J Cardiol. 2005;96:45–51. doi: 10.1016/j.amjcard.2005.02.042. [DOI] [PubMed] [Google Scholar]
- 17.Cagle A, Hubbard R. Cold-related cardiac mortality in King County, Washington, USA 1980-2001. Ann Hum Biol. 2005;32:525–537. doi: 10.1080/03014460500153758. [DOI] [PubMed] [Google Scholar]
- 18.Estes NA, III, Halperin JL, Calkins H, et al. ACC/AHA/Physician Consortium 2008 clinical performance measures for adults with nonvalvular atrial fibrillation or atrial flutter: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and the Physician Consortium for Performance Improvement (Writing Committee to Develop Clinical Performance Measures for Atrial Fibrillation) developed in collaboration with the Heart Rhythm Society. J Am Coll Cardiol. 2008;51:865–884. doi: 10.1016/j.jacc.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 19.National Weather Service, Weather Prediction Center. [Accessed August 11, 2014];The heat index equation. Available at: http://www.hpc.ncep.noaa.gov/html/heatindex_equation.shtml.
- 20.Parish OO, Putnam TW. NASA Technical Note D-8401. National Aeronautics and Space Administration; 1977. [Accessed September 19, 2012]. Equations for the determination of humidity from dewpoint and psychrometric data. Available at: http://www.nasa.gov/centers/dryden/pdf/87878main_H-937.pdf. [Google Scholar]
- 21.Link MS, Luttmann-Gibson H, Schwartz J, et al. Acute exposure to air pollution triggers atrial fibrillation. J Am Coll Cardiol. 2013;62:816–825. doi: 10.1016/j.jacc.2013.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- 23.Künzli N, Schindler C. A call for reporting the relevant exposure term in air pollution case-crossover studies. J Epidemiol Community Health. 2005;59:527–530. doi: 10.1136/jech.2004.027391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rich DQ, Mittleman MA, Link MS, et al. Increased risk of paroxysmal atrial fibrillation episodes associated with acute increases in ambient air pollution. Environ Health Perspect. 2006;114:120–123. doi: 10.1289/ehp.8371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liao D, Shaffer ML, He F, et al. Fine particulate air pollution is associated with higher vulnerability to atrial fibrillation–the APACR study. J Toxicol Environ Health A. 2011;74:693–705. doi: 10.1080/15287394.2011.556056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Culić V, Eterović D, Mirić D, Giunio L, Lukin A, Fabijanić D. Triggering of ventricular tachycardia by meteorologic and emotional stress: protective effect of beta-blockers and anxiolytics in men and elderly. Am J Epidemiol. 2004;160:1047–1058. doi: 10.1093/aje/kwh335. [DOI] [PubMed] [Google Scholar]
- 27.Čulić V, Silić, Hodžić M. Triggering of supraventricular tachycardia by physical activity and meteorologic factors. Int J Cardiol. 2013;168:4295–4300. doi: 10.1016/j.ijcard.2013.04.195. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen JL, Schwartz J, Dockery DW. The relationship between indoor and outdoor temperature, apparent temperature, relative humidity, and absolute humidity. Indoor Air. 2014;24:103–112. doi: 10.1111/ina.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nguyen JL, Laden F, Link MS, Schwartz J, Luttmann-Gibson H, Dockery DW. Weather and triggering of ventricular arrhythmias in patients with implantable cardioverter-defibrillators. J Expo Sci Environ Epidemiol. 2015;25:175–181. doi: 10.1038/jes.2013.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hajat S, Kovats RS, Lachowycz K. Heat-related and cold-related deaths in England and Wales: who is at risk? Occup Environ Med. 2007;64:93–100. doi: 10.1136/oem.2006.029017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collins KJ. Low indoor temperatures and morbidity in the elderly. Age Ageing. 1986;15:212–220. doi: 10.1093/ageing/15.4.212. [DOI] [PubMed] [Google Scholar]
- 33.Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124:2264–2274. doi: 10.1161/CIRCULATIONAHA.111.019893. [DOI] [PubMed] [Google Scholar]
- 34.Kourliouros A, Savelieva I, Kiotsekoglou A, Jahangiri M, Camm J. Current concepts in the pathogenesis of atrial fibrillation. Am Heart J. 2009;157:243–252. doi: 10.1016/j.ahj.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 35.McManus DD, Shaikh AY, Abhishek F, Vasan RS. Atrial fibrillation and heart failure parallels: lessons for atrial fibrillation prevention. Crit Pathw Cardiol. 2011;10:46–51. doi: 10.1097/HPC.0b013e31820e1a4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ricquier D, Bouillaud F. Mitochondrial uncoupling proteins: from mitochondria to the regulation of energy balance. J Physiol. 2000;529:3–10. doi: 10.1111/j.1469-7793.2000.00003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Larsson K, Tornling G, Gavhed D, Müller-Suur C, Palmberg L. Inhalation of cold air increases the number of inflammatory cells in the lungs in healthy subjects. Eur Respir J. 1998;12:825–830. doi: 10.1183/09031936.98.12040825. [DOI] [PubMed] [Google Scholar]
- 38.Giesbrecht GG. The respiratory system in a cold environment. Aviat Space Environ Med. 1995;66:890–902. [PubMed] [Google Scholar]
- 39.Barnett AG, Dobson AJ, McElduff P, Salomaa V, Kuulasmaa K, Sans S WHO MONICA Project. Cold periods and coronary events: an analysis of populations worldwide. J Epidemiol Community Health. 2005;59:551–557. doi: 10.1136/jech.2004.028514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang K, Li Y, Schwartz JD, O’Neill MS. What weather variables are important in predicting heat-related mortality? A new application of statistical learning methods. Environ Res. 2014;132:350–359. doi: 10.1016/j.envres.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]