Abstract
To explore the mechanism of Th17 cells and Treg cells in the peripheral blood of patients with pancreatic cancer through analyzing the changes of the related genes and cytokines expression. 40 patients were divided into three groups based on clinical staging, and 20 healthy subjects were treated as normal control. Proportion of Th17 cells and Treg cells were detected by flow cytometry. RORα, RORγt, FoxP3, and CTLA-4 expression in peripheral blood mononuclear cells were detected by RT-PCR. IL-10, IL-23, INF-γ, TGF-β, and IL-17 cytokine levels in peripheral blood were determined by enzyme-linked immunosorbent assay (ELISA). The proportion of Th17 cells in peripheral blood of pancreatic cancer patients was lower than that in the normal control, while the proportion of Treg was higher. RORα and RORγt mRNA expression in Th17 cells from pancreatic cancer patients decreased, while FoxP3 and CTLA-4 mRNA expressions in Treg cells increased compared with the normal control. And the correlation analysis revealed that they were significantly correlated with clinical staging. Compared with healthy control, IL-23, IL-17 and INF-γ levels were lower in pancreatic cancer patients, while IL-10 and TGF-β levels were higher. Following the progression of disease, patients in advanced stage exhibited higher level of IL-10 and TGF-β, and lower levels of IL-23 and INF-γ. Pancreatic cancer patients exhibited Th17/Treg balance disorders with higher Treg and lower Th17 cells. They affect cytokine IL-10, IL-23, INF-γ, TGF-β, and IL-17 expression changes mainly through regulating transcription factors such as RORα, RORγt, FoxP3 and CTLA-4, suggesting that Th17/Treg balance disorders plays an important role in the tumorigenesis of pancreatic cancer.
Keywords: Pancreatic cancer, Th17/Treg, cytokine, RORα and RORγt, FoxP3, CTLA-4
Introduction
Pancreatic cancer is one of the digestive tract tumors with worst prognosis. The incidence of pancreatic cancer is 5.1/100,000, which rises dramatically in the last 20 years. Only 10%~15% of the patients have the surgical treatment opportunity, in which only 5%~7.5% can obtain a radical cure [1]. 1 year survival rate of pancreatic cancer was 8%, while the 5-year survival rate was 3%. The median survival time was only 2-3 month [2]. Immune escape has played an important role in tumor progression. Recently, effector T cell Th17 subset was found derived from initial CD4+ T cell. Numerous studies suggested Thl7 cells is an important effector cell in the tumor microenvironment [3]. Treg mediated immune escape is one of the reasons for anti-tumor treatment failure. Immune escape related cytokine causes the environment changes, promoting tumor cells escape immune surveillance, and eventually leading to immune escape and tumor metastasis [4]. This study tried to explore the changes and mechanism of Th17 cells and Treg cells in the peripheral blood of patients with pancreatic cancer through genes and cytokines expression.
Materials and methods
General information
40 pancreatic cancer patients between January 2013 and April 2014 were enrolled from our hospital. The patients were divided into three groups based on clinical staging as follows: early stage group (n = 5), progression stage group (n = 15) and advanced group (n = 20). Another 20 healthy volunteers were chose as control. There were 21 males and 19 females in the observation group with average age 59.02±10.03 years old, while 10 males and 10 females in the normal control group with average age 58.35±9.09 years old. The two groups showed no significant difference in age and gender (P>0.05).
The study protocol was approved by the Research Ethics Committee of our hospital, and all patients gave their informed consent before study commencement.
Diagnostic, inclusion and exclusion criteria
Diagnostic criteria
All the pancreatic cancer patients were diagnosed by cytology or histopathology as epithelial cancer based on the standard of diagnosis and treatment of common malignant tumor.
Inclusion criteria
Patients in stage III or IV according to the UICC TNM staging criteria [5] that unable to receive radical resection or refuse surgery; measurable lesions; expected survival period longer than 3 months.
Exclusion criteria
Hospital stay <24 hours; hospital patients with poor compliance or incomplete clinical data; patients in pregnancy, lactating period, or mental illness; KPS score ≤60; patients with unstable vital signs or severe liver and renal insufficiency; patients used drugs that affect the immune function in last 3 months.
Reagents and instruments
Facscan flow cytometry (Becton Dickinson co, USA); Fluorescence quantitative PCR analysis and software MXPro4.01 (Stratagene co, USA).
PE tagged IL-17, FITC anti-CD8 monoclonal antibody and PE-Cy5 anti-CD3 monoclonal antibody (EB co, USA), FITC CD25, APC CD4, and PE Foxp3 tagged cell membrane antibody (EB co, USA); TRIzol reagent kit (Gibco co, USA); Primers for RT-PCR were synthesized by Takara biotechnology co., LTD., reverse transcription-polymerase chain reaction kit (RT-PCR) were products from the company.
Specimen collection
4 ml peripheral blood was collected from 40 pancreatic cancer patients and 20 healthy control after they hospitalized for 1 week. The collected peripheral venous blood was gradient centrifuged with lymphocyte separation medium to separate peripheral blood mononuclear cells (PBMC). Another 2 ml peripheral venous blood was collected and centrifuged at 3000 r/min for 10 min to collect the serum for ELISA detection.
Thl7 cells proportion detection by flow cytometry
Cell culture
400 μL whole blood specimen anticoagulated by heparin was diluted by RPMI1640 medium at 1:1 with 25 ng/mL PMA, 1 μg/mL penicillin streptomycin, and 1.7 µg/mL protein transport inhibitor Monensin in a humid atmosphere containing 5% CO2 at 37°C for 4-6 hours.
Cell staining
20 μL FITC-CD8 antibody, 20 μL PE-Cy5-CD3 antibody, 100 μL Fix & Perm stationary liquid, 100 μL Fk & Perm membrane broken and blood dissolving liquid, PE-IL-17 antibody were sequentially added to the cells and incubated at room temperature for 15 min away from light. Then, the cells were resuspended in 300 μL PBS and tested by flow cytometry for Th17 cells (CD3+ CD8- IL-17A+).
Treg cells proportion detection by flow cytometry
PBMC was separated by density gradient centrifugation, and FITC CD4, APC CD25, PE Foxp3 antibodies were applied for staining and detected by flow cytometry for Treg.
RT-PCR
Mononuclear cells extraction: 10-20 ml blood specimen was diluted with isovolumetric Hank’s liquid. Then the mixture was added to the lymphocyte separation medium and centrifuged at 800 rpm for 20 min at room temperature. The mononuclear cells were in the layer between upper and middle-level. Another Hank’s liquid (1:5) was added and centrifuged for 8 min. After washed twice, the supernatant was discarded and the cells were stored at -80°C.
TRIzol was used for total RNA extraction. Each RT-PCR reaction (in 20 µL) contained 2.5× Real Master Mix/20× SYBR Solution, 0.4 µL 10 μM primers and 2.5 µL of template cDNA. The primers used are listed as followed:
RORα Forward primer: 5’-AAACAAG CAGCGGGA GGTGA-3’; Reverse primer: 5’-TGGCAAA CTCCACC ACATAC-3’; RORyt Forward primer: 5’-CCTGGGCTCCT CGCCTG ACC-3’; Reverse primer: 5’-TCTCTCT GCC CTCA GCCTTGCC-3’; CTLA-4 Forward primer: 5’-ACCTTCAGTGGTGTTGGCTAG-3’; Reverse primer: 5’-TAAATCTGCGTCCCGTTGC-3’; FoxP3 Forward primer: 5’-TGTGAGGACTACCGAGCC-3’; Reverse primer: 5’-AGGAGAAAGCGGATACCA-3’; β-actin Forward primer: 5’-ATGGG TCAGA AGGATTCCT ATGTG-3’; Reverse primer: 5’-CTTCATGAGGTAG TCAGT CA GGTC-3’.
The cycling conditions consisted of an initial, single cycle of 5 min at 95°C, followed by 30 cycles of 30 s at 95°C, 30 s at 55°C, and 60 s at 72°C.
ELISA detection
Serum IL-10, TGF-β, IL-17, IL-23 and IFN-γ concentrations were detected by ELISA according to the manual. OD value was used to determine the concentration based on the standard curve.
Statistical analysis
Chi-square analysis was applied for enumeration data comparison. Measurement data was presented as X̅±Sand analyzed by t test. Spearman rank correlation test was used for analysis between clinical staging and the expression level of RORα, RORγt, FoxP3 and CTLA-4. All statistical analyses were performed using SPSS16.0 software (Chicago, IL) with P<0.05 as statistical significant.
Results
Th17 and Treg proportion in peripheral blood
Flow cytometry was applied to detect Th17 cells proportion in the peripheral blood from pancreatic cancer patients and healthy control (Table 1). Th17 cells proportion was lower in pancreatic cancer patients than that of healthy group (P<0.01). Following the progress of disease, Th17 cells proportion gradually decreased (P<0.01). At the same time, pancreatic cancer patients exhibited significantly lower IL-17 level than that of healthy control (P<0.01); while the IL-17 level in advanced stage patients is lower compared with patients in early and progression stage (P<0.01).
Table 1.
Th17 proportion in peripheral blood from pancreatic cancer patients and healthy control
| Group | N | Th17% | IL-17 |
|---|---|---|---|
| Healthy control | 20 | 8.72±1.04 | 67.86±11.08 |
| Early stage | 5 | 6.12±2.14** | 51.20±12.14** |
| Progression stage | 15 | 5.50±1.35** | 45.32±10.25** |
| Advanced stage | 20 | 1.99±0.46**,## | 17.87±1.29** |
P<0.01 compared with healthy control;
P<0.01 compared with progression stage group.
Flow cytometry was used to detect Treg cells proportion in the peripheral blood from pancreatic cancer patients and healthy control (Table 2). CD4+CD25+ Treg cells proportion in CD4+ T cells was higher in pancreatic cancer patients than that of healthy group (P<0.01), and the similar phenomena were seen in CD4+CD25+ Foxp3+ Treg cells and CD4+CD25+ Treg cells. Furthermore, they gradually increased following the progress of disease (P<0.01).
Table 2.
Treg proportion in peripheral blood from pancreatic cancer patients and healthy control
| Group | N | CD25+/CD4+ | FoxP3/CD4+ | CD25+FoxP3/CD4+ |
|---|---|---|---|---|
| Healthy control | 20 | 2.69±0.26 | 1.20±0.14 | 0.47±0.04 |
| Early stage | 5 | 3.11±0.45*,## | 1.22±0.21## | 0.56±0.07**,## |
| Progression stage | 15 | 4.20±0.40** | 1.76±0.28** | 0.95±0.18** |
| Advanced stage | 20 | 4.32±0.58** | 1.87±0.29** | 1.01±0.17** |
P<0.05 compared with healthy control;
P<0.01 compared with healthy control;
P<0.01 compared with progression stage group.
Cytokine expression in peripheral blood
Compared with healthy control, IL-23 and INF-γ levels were lower in pancreatic cancer patients (P<0.01), while IL-10 and TGF-β levels were higher (P<0.01). Following the progression of disease, patients in advanced stage exhibited higher level of IL-10 and TGF-β, and lower levels of IL-23 and INF-γ (P<0.01) (Table 3).
Table 3.
Cytokine level in peripheral blood from pancreatic cancer patients and healthy control
| Group | N | IL-23 (pg/ml) | IL-10 (pg/ml) | INF-γ (pg/ml) | TGF-β (ng/ml) |
|---|---|---|---|---|---|
| Healthy control | 20 | 87.67±7.35 | 0.66±0.09 | 314.34±40.06 | 395.68±30.57 |
| Early stage | 5 | 68.94±10.58**,## | 0.68±0.05## | 216.35±18.45**,## | 474.48±35.78**,## |
| Progression stage | 15 | 41.81±0.15** | 1.01±0.05** | 166.45±5.38** | 515.57±21.89** |
| Advanced stage | 20 | 21.86±0.12**,## | 1.28±0.22**,## | 129.01±4.17**,## | 631.45±36.66**,## |
P<0.01 compared with healthy control;
P<0.01 compared with progression stage group.
RORα and RORγt mRNA expression in Th17; FoxP3 and CTLA-4 mRNA expression in Treg
Agarose gel electrophoresis results showed that the total RNA purity meet experimental requirements (Figure 1). RORα and RORγt mRNA expression in Th17 cells from pancreatic cancer patients were lower compared with the normal control (P<0.01). As the disease process, their expression decreased obviously (P<0.01) (Table 4).
Figure 1.
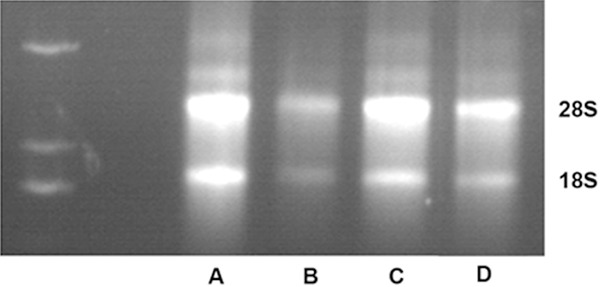
Agarose gel electrophoresis. A. Healthy control; B. Early stage; C. Progression stage; D. Advanced stage.
Table 4.
RORα and RORγt mRNA expression in Th17 cells
| Gene | Group | N | ΔCt | F value | P value | -2ΔΔCt |
|---|---|---|---|---|---|---|
| RORα | Healthy control | 20 | 4.72±0.35 | 661.09 | 0.000 | 3.58±0.13 |
| Early stage | 5 | 3.57±0.32 | ||||
| Progression stage | 15 | 2.01±0.23 | ||||
| Advanced stage | 20 | 1.15±0.16 | ||||
| RORγt | Healthy control | 20 | 2.02±0.21 | 98.593 | 0.000 | 2.17±0.11 |
| Early stage | 5 | 1.47±0.19 | ||||
| Progression stage | 15 | 1.10±0.17 | ||||
| Advanced stage | 20 | 1.06±0.20 |
FoxP3 and CTLA-4 mRNA expressions in Treg cells from pancreatic cancer patients were lower compared with the normal control (P<0.01). As the disease process, their expression increased significantly (P<0.01) (Table 5).
Table 5.
FoxP3 and CTLA-4 mRNA expression in Treg cells
| Gene | Group | N | ΔCt | F value | P value | -2ΔΔCt |
|---|---|---|---|---|---|---|
| FoxP3 | Healthy control | 20 | 1.18±0.16 | 338.5 | 0.000 | 0.23±0.02 |
| Early stage | 5 | 1.37±0.10 | ||||
| Progression stage | 15 | 2.88±0.29 | ||||
| Advanced stage | 20 | 3.72±0.35 | ||||
| CTLA-4 | Healthy control | 20 | 1.06±0.20 | 55.59 | 0.000 | 0.45±0.08 |
| Early stage | 5 | 1.26±0.20 | ||||
| Progression stage | 15 | 1.69±0.19 | ||||
| Advanced stage | 20 | 1.82±0.21 |
Correlation between pancreatic cancer clinical staging and the expression level of RORα, RORγt, FoxP3 and CTLA-4
Spearman correlation analysis showed that RORα and RORγt mRNA level were negatively correlated with clinical staging (P<0.05), and they decreased following the upstaging. FoxP3 and CTLA-4 mRNA level exhibited positively correlation with clinical staging, and they upregulated with the disease progression (P<0.05) (Table 6).
Table 6.
Spearman correlation analysis
| Item | r value | P value |
|---|---|---|
| RORγt | -0.522 | 0.000 |
| RORα | -0.368 | 0.036 |
| FoxP3 | 0.402 | 0.013 |
| CTLA-4 | 0.389 | 0.024 |
Discussion
Exploring new treatments and searching for more effective treatment mode become a research hotspot for pancreatic cancer. Antitumor immune imbalance of pancreatic cancer may provide a promising treatment mode. CD4+CD25+Foxp3+ Treg and Th17 cells are two types of CD4+ T lymphocytes different from Th1 and Th2.
Thl7 cells are produced by IL-17 inducing monocyte/macrophage that is secreted by cytokines and chemokines participating in the immune response [6]. Several studies have shown that Thl7 cells significantly decreased in a variety of tumors. TGF-β and IL-6 can induce Thl7 cells differentiation by vitamin A acid orphan nuclear receptor family which including three members such as RORγt, RORα, and RORβ steroid receptor superfamily. This receptor family is the main transcription factor of Thl7 cells, and can regulate its specificity effect factor IL-17 expression and secretion by promoting Thl7 cells differentiation [7]. CD4+CD25+Foxp3+ Treg is one of the important factors to maintain the immune tolerance. Its main function is to restrain autoimmune T cells activation and function, regulate immune response to antigens, and allow the body to avoid autoimmune diseases [8]. Treg mediated immune escape is an important factor in tumor immune, and it is also one of the reasons of the failure of anti-tumor treatment. It promotes tumor cells escape immune surveillance, and eventually leads to immune escape and tumor metastasis [9]. Treg number and proportion increased in the peripheral blood lymphocyte and tumor infiltrating lymphocytes in patients with gastric cancer, liver cancer, pancreatic cancer, breast cancer and other malignant tumors [10]. In present study, Th17 proportion in peripheral blood of pancreatic cancer patients was lower than that in healthy control, while Treg proportion was higher. Th17/Treg proportion decreased in pancreatic cancer and became worse with the progress of disease. It indicated that Th17/Treg exhibit balance disorder in the peripheral blood of pancreatic cancer patients with enhanced Treg cells expression and declined Th17 cells expression.
RORγt is especially necessary for survive of lymphocytes in the immune system and development of lymph node [11]. It has confirmed RORγt is the key nuclear factor for Thl7 cells differentiation in vitro [12]. CD4+ T cells that knockout RORγt will not express IL-17, while overexpressed RORγt result in expressing IL-17 without need foreign cytokine. The transcriptional regulation region of RORγt located in assuming enhancer saved non-coding sequences 2. There are two specific DNA response elements (ROREs) that can directly combined with ROR to transcriptional activate IL-17 target gene mediated by RORα and RORγt [13]. RORα is also proved to be an important transcription factor regulating Thl7 cells differentiation. The common induction of IL-6 and TGF-β depends on the RORα activation in the form of STAT3, and it can the activate IL-17 gene transcription to promote Thl7 cells differentiation. Delerive et al. revealed that RORα is a negative regulation factor for inflammation, as it can negatively influence the expression of regulation factor IκBa to positively regulate NF-κB signaling pathway [14]. RORα and RORγt deletion hindered the process of Th precursor cells differentiated into Thl7 cells [15], in which RORγt deletion showed stronger effect on IL-17 expression than RORα, indicating that the effect of RORγt is more important. FoxP3 is a member of the Fox transcription factor family, and play a role in regulating the development and function of CD4+CD25+Foxp3+ Treg cells. FoxP3 gene is highly expressed in lymphoid tissue, especially specific expressed in CD4+ T cells. CD4+CD25+ Treg cells no matter originated from the thymus or periphery can both specific express FoxP3. Thus, FoxP3 may be a specific marker of CD4+CD25+ Treg cells [16]. CTLA-4 is a member of the B7/CD28 family and expressed on the cell membrane of activated T lymphocytes, while its expression is quite weak on T lymphocytes. It almost has no expression in the non T lymphocytes such as NK cells, macrophages, liver cells and brain cells [17]. In this study, RORα and RORγt mRNA expression in Th17 cells from pancreatic cancer patients decreased, while FoxP3 and CTLA-4 mRNA expressions in Treg cells increased compared with the normal control. Furthermore, as the disease process, RORα and RORγt expression decreased and FoxP3 and CTLA-4 expression increased significantly. This indicated that RORα, RORγt, FoxP3 and CTLA-4 expression are closely related to tumorigenesis of pancreatic cancer.
TGF-β is an important cytokine that mediates Thl7 cells differentiation. IL-17 can promote myeloid dendritic cells and mononuclear cell activation, enhance DC inducing IL-1β, IL-6, IL-23 and TGF-β, and inducing Th17 differentiation [18]. CD4+ T cells can induce Treg cells specific transcription factor Foxp3 expression under the action of TGF-β and differentiate into the CD4+CD25+ Treg cells which can secrete IL-6, IL-10, IL-17 and INF-γ. This can inhibit immune cell activity and cause tumor cells escape from immune surveillance [19]. Compared with healthy control, IL-23, IL-17 and INF-γ levels were lower in the peripheral blood from pancreatic cancer patients, while IL-10 and TGF-β levels were higher. Following the progression of disease, patients in advanced stage exhibited higher level of IL-10 and TGF-β, and lower levels of IL-23 and INF-γ.
To sum up, pancreatic cancer patients exhibited Th17/Treg balance disorders with higher Treg and lower Th17 cells. They affect cytokine IL-10, IL-23, INF-γ, TGF-β, and IL-17 expression changes mainly through regulating transcription factors such as RORα, RORγt, FoxP3 and CTLA-4, suggesting that Th17/Treg balance disorders plays an important role in tumorigenesis of pancreatic cancer.
Disclosure of conflict of interest
None.
References
- 1.Wang P, Meng ZQ, Chen Z, Lin JH, Ping B, Wang LF, Wang BH, Liu LM. Diagnostic value and complications of fine needle aspiration for primary liver cancer and its influence on the treatment outcome-a study based on 3011 patients in China. Eur J Surg Oncol. 2008;34:541–546. doi: 10.1016/j.ejso.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Wang P, Meng ZQ, Chen Z, Lin JH, Zhou ZH, Chen H, Wang K, Shen YH, Zhu ZF, Zhao GF, Fu H, Liu LM. Survival rate of pancreatic cancer in elderly patients. Hepatogastroenterology. 2008;55:681–686. [PubMed] [Google Scholar]
- 3.Oberholzer A, Oberholzer C, Moldawer LL. Sepsis syndromes: understanding the role of innate and acquired immunity. Shock. 2001;16:83–96. doi: 10.1097/00024382-200116020-00001. [DOI] [PubMed] [Google Scholar]
- 4.Bosch FX, Ribes J, Diaz M, Cleries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004;127:S5–S16. doi: 10.1053/j.gastro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Wang P, Chen Z, Huang WX, Liu LM. Current preventive treatment for recurrence after curative hepatectomy for liver metastases of colorectal carcinoma: a literature review of randomized control trials. World J Gastroenterol. 2005;11:3817–3822. doi: 10.3748/wjg.v11.i25.3817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zelante T, Bozza S, De Luca A, D’Angelo C, Bonifazi P, Moretti S, Giovannini G, Bistoni F, Romani L. Th17 cells in the setting of Aspergillus infection and pathology. Med Mycol. 2009;47(Suppl 1):S162–169. doi: 10.1080/13693780802140766. [DOI] [PubMed] [Google Scholar]
- 7.Gocke AR, Cravens PD, Ben LH, Hussain RZ, Northrop SC, Racke MK, Lovett-Racke AE. T-bet regulates the fate of Th1 and Th17 lymphocytes in autoimmunity. J Immunol. 2007;178:1341–1348. doi: 10.4049/jimmunol.178.3.1341. [DOI] [PubMed] [Google Scholar]
- 8.Liu CX XP, Peng Y. Challenges in research and development of traditional Chinese medicines. Chin Herb Med. 2009;1:1–28. [Google Scholar]
- 9.Zou W. Regulatory T cells, tumour immunity and immunotherapy. Nat Rev Immunol. 2006;6:295–307. doi: 10.1038/nri1806. [DOI] [PubMed] [Google Scholar]
- 10.Peng L, Kjaergaard J, Plautz GE, Awad M, Drazba JA, Shu S, Cohen PA. Tumor-induced L-selectinhigh suppressor T cells mediate potent effector T cell blockade and cause failure of otherwise curative adoptive immunotherapy. J Immunol. 2002;169:4811–4821. doi: 10.4049/jimmunol.169.9.4811. [DOI] [PubMed] [Google Scholar]
- 11.Sun Z, Unutmaz D, Zou YR, Sunshine MJ, Pierani A, Brenner-Morton S, Mebius RE, Littman DR. Requirement for RORgamma in thymocyte survival and lymphoid organ development. Science. 2000;288:2369–2373. doi: 10.1126/science.288.5475.2369. [DOI] [PubMed] [Google Scholar]
- 12.Yang XO, Pappu BP, Nurieva R, Akimzhanov A, Kang HS, Chung Y, Ma L, Shah B, Panopoulos AD, Schluns KS, Watowich SS, Tian Q, Jetten AM, Dong C. T helper 17 lineage differentiation is programmed by orphan nuclear receptors ROR alpha and ROR gamma. Immunity. 2008;28:29–39. doi: 10.1016/j.immuni.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mangan PR, Harrington LE, O’Quinn DB, Helms WS, Bullard DC, Elson CO, Hatton RD, Wahl SM, Schoeb TR, Weaver CT. Transforming growth factor-beta induces development of the T(H)17 lineage. Nature. 2006;441:231–234. doi: 10.1038/nature04754. [DOI] [PubMed] [Google Scholar]
- 14.Delerive P, Monte D, Dubois G, Trottein F, Fruchart-Najib J, Mariani J, Fruchart JC, Staels B. The orphan nuclear receptor ROR alpha is a negative regulator of the inflammatory response. EMBO Rep. 2001;2:42–48. doi: 10.1093/embo-reports/kve007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao X, Gigoux M, Yang J, Leconte J, Yang X, Suh WK. Anti-chlamydial Th17 responses are controlled by the inducible costimulator partially through phosphoinositide 3-kinase signaling. PLoS One. 2012;7:e52657. doi: 10.1371/journal.pone.0052657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alegre ML, Noel PJ, Eisfelder BJ, Chuang E, Clark MR, Reiner SL, Thompson CB. Regulation of surface and intracellular expression of CTLA4 on mouse T cells. J Immunol. 1996;157:4762–4770. [PubMed] [Google Scholar]
- 17.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. [PubMed] [Google Scholar]
- 18.Biron CA, Nguyen KB, Pien GC, Cousens LP, Salazar-Mather TP. Natural killer cells in antiviral defense: function and regulation by innate cytokines. Annu Rev Immunol. 1999;17:189–220. doi: 10.1146/annurev.immunol.17.1.189. [DOI] [PubMed] [Google Scholar]
- 19.Dooley S, Weng H, Mertens PR. Hypotheses on the role of transforming growth factor-beta in the onset and progression of hepatocellular carcinoma. Dig Dis. 2009;27:93–101. doi: 10.1159/000218340. [DOI] [PubMed] [Google Scholar]


