Abstract
Background:
Dilative arteriopathy plus leucencephalopathy as a manifestation of a mitochondrial disorder (MID) is rare.
Case report:
In a 70yo Caucasian female, height 160cm, weight 62kg, with mild right-sided hemiparesis due to subacute ischemic stroke in the posterior leg of the left internal capsule, a megadolichobasilar artery and marked leucencephalopathy and gliosis of the pons were detected. In addition, microbleeds in a peripheral distribution at the cortical/subcortical border were noted. After the exclusion of various differentials, which could have explained her abnormalities, a MID was suspected.
Conclusions:
Dilative arteriopathy of the intra-cerebral arteries, in association with recurrent stroke and supra- and infratentorial leucencephalopathy, but the absence of neurofibromatosis or increased low-density lipoprotein values, is most likely attributable to a non-syndromic MID.
Keywords: Mitochondrial disorder, genetics, dilative arteriopathy, megadolichobasilar artery, arteriopathy, stroke
Dilative arteriopathy is a vascular anomaly of the large extra- and intra-cerebral arteries consisting of the widening and elongation of the basilar and carotid arteries and the proximal anterior, medial and posterior cerebral arteries [6]. Dilative arteriopathy may manifest as ectasia or aneurysms [6]. It may be responsible for a number of cerebral manifestations such as vertigo, deafness, trigeminal neuralgia, facial spasms, facial palsy, hydrocephalus or stroke (Table 1) [9]. Occasionally, dilative arteriopathy is associated with leucencephalopathy. Dilative arteriopathy plus leucencephalopathy as a manifestation of a mitochondrial disorder (MID), as in the following case, is rare.
Table 1.
Clinical manifestations of dilative arteriopathy.
| Vertigo | [9] |
| Deafness | [9, 21] |
| Trigeminal neuralgia | [9, 28] |
| Facial hemispasm | [4, 9] |
| Facial palsy | [9] |
| Multiple cranial nerve palsy | [25] |
| Hydrocephalus | [1, 18, 25] |
| Central alveolar hypoventilation | [10] |
| SUNCT syndrome | [23] |
| Locked-in-syndrome with yawning | [16] |
| Subarachnoid or intracerebral hemorrhaghe | [5] |
| Agenesis of the internal carotid arteries | [20] |
| Stroke | [3, 24] |
SUNCT: short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing
The patient is a 70-year-old Caucasian female, height 160 cm, weight 62 kg, who was admitted for mild right-sided hemiparesis one day after onset. Cerebral MRI revealed a subacute ischemic stroke in the posterior leg of the left internal capsule. In addition, marked leucencephalopathy and gliosis of the pons were evident. Furthermore, microbleeds in a peripheral distribution at the cortical/subcortical border were noted. She had a history of a prior left-sided stroke three years earlier in the parietal, subcortical white matter and of hypercholesterolemia. Other cardiovascular risk factors were negative. Blood chemical investigations were completely normal. There were no indications for endocrine, cardiac or skeletal muscle abnormalities. The family history was negative for neurometabolic disease.
The patient is interesting as presenting with supra- and infra-tentorial leucencephalopathy in addition to dilative arteriopathy. Stroke as a manifestation of dilative arteriopathy is in line with previously reported cases of dilative arteriopathy and stroke (Table 1). Although the cause of cerebral white matter lesions remains elusive, Several differential diagnoses have to be discussed.
Dilative arteriopathy is a large vessel disease affecting the large intra- or extra-cranial cerebral arteries [6]. It has been associated with a number of disorders, including arterial hypertension [26], Fabry’s disease [19, 27], neurofibromatosis [22], Pompe’s disease [17], kidney dysfunction [12], low-density lipoprotein elevation [11] and non-syndromic MID [6, 29] (Table 2). In the majority of cases, angiography reveals fusiform dilation of the basilar artery, elongation of the top of the basilar trunk and asymmetric tortuosity or dislocation of the irregular shaped wall of the basilar artery [15].
Table 2.
Differential diagnoses of a mega-dolicho basilar artery.
| Disorder | Leucencephalopathy | Reference |
|---|---|---|
| Neurofibromatosis | Yes | [22] |
| Fabry’s disease | No | [8, 19, 27] |
| Pompe disease | No | [17] |
| Arterial hypertension | No | [13, 14, 26] |
| Kidney disease | No | [12] |
| Low-density lipo-protein | Yes | [11] |
| Mitochondrial disorder | Yes | [2, 6, 7, 29] |
Clinical manifestations of dilative arteriopathy are numerous and include vertigo [9], deafness [9, 21], trigeminal neuralgia [9, 28], facial spasms, usually hemispasms [9, 4], facial palsy [9], multiple cranial nerve palsy [25], compression hydrocephalus [1, 18, 25], central alveolar hypoventilation [10], short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT)-syndrome [23] and stroke [3, 24] (Table 1). Of these, stroke is the most frequent.
Why dilative arteriopathy and leucencephalopathy in the presented patient were attributed to a non-syndromic MID, manifesting as leucencephalopathy exclusively is based on several arguments. The simultaneous occurrence of leucencephalopathy and dilative arteriopathy generally occurs in neurofibromatosis, low-density lipoprotein-associated dilated arteriopathy, or MID (Table 2). Neurofibromatosis was excluded based on the clinical presentation and the neuroradiological findings and a low-density lipoprotein-associated dilated arteriopathy based on the repeatedly normal low-density lipoprotein levels. As such, the most likely cause of dilated arteriopathy with leucencephalopathy in the patient presented remains a non-syndromic MID [7]. Further arguments for the MID are the patient’s short stature and hyperlipidemia. The marginally-sized kidneys are an argument for kidney disease as the cause of dilative arteriopathy, but renal disease with dilative arteriopathy is not usually associated with leucencephalopathy.
This case shows that dilative arteriopathy of the large intra-cerebral arteries in association with supra- and infratentorial leucencephalopathy and normal low-density lipoprotein values is probably attributable to non-syndromic mitochondrial leucencephalopathy. Recurrent stroke may be a manifestation of dilative arteriopathy.
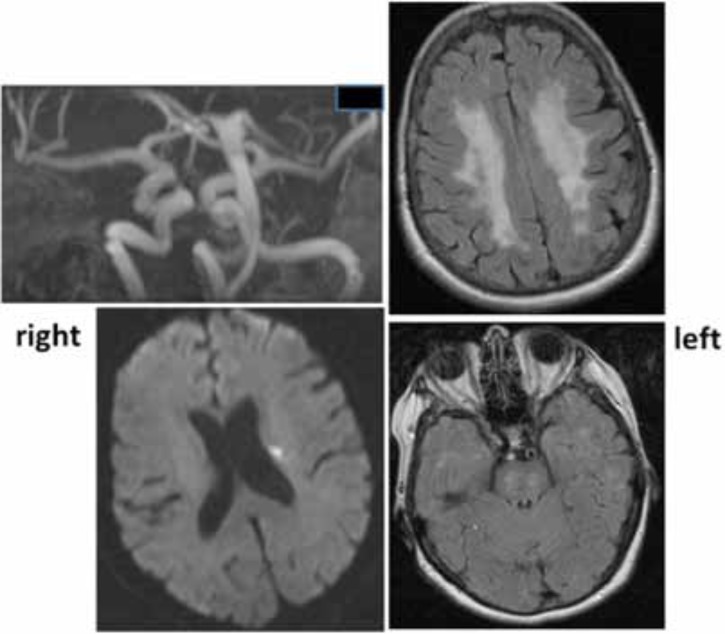
Fig. (1).
Cerebral imaging of the described patient. Ektasia of the basilary artery (upper left). Periventricular ischemic stroke in the territory of the left median cerebral artery (lower left). Supratentorial leucencephalopathy (upper right). Leucencephalopathy of the pons (lower right).
ACKNOWLEDGEMENTS
Conflict of Interest
The author confirms that this article content has no conflict of interest.
Declared none.
REFERENCES
- 1.Aiba T, Nakazawa T. Non-communicating hydrocephalus due to megadolichobasilar artery--case report. Neurol Med Chir (Tokyo). 1995;35:104–6. doi: 10.2176/nmc.35.104. [DOI] [PubMed] [Google Scholar]
- 2.Byrne E. Does mitochondrial respiratory chain dysfunction have a role in common neurodegenerative disordersκ. J Clin Neurosci. 2002;9:497–501. doi: 10.1054/jocn.2001.0991. [DOI] [PubMed] [Google Scholar]
- 3.Cambron M, Van Hooff RJ, Nieboer K, De Keyser J, Brouns R. Successful repetitive intravenous thrombolysis in a patient with recurrent brainstem infarctions due to megadolichobasilar ectasia. JAMA Neurol. 2013;70:520–1. doi: 10.1001/jamaneurol.2013.618. [DOI] [PubMed] [Google Scholar]
- 4.Campos E, Matías-Guíu J, Romero F, Fernández JM, Dávalos A. Megadolichobasilar presentation as facial hemispasm. Med Clin (Barc). 1984;82:332. [PubMed] [Google Scholar]
- 5.D'Andrea F, Maiuri F, Gangemi M, Iaconetta G. Megadolichobasilar anomaly.Clinical and diagnostic considerations on 30 cases. . Acta Neurol (Napoli). 1992;14:611–9. [PubMed] [Google Scholar]
- 6.Finsterer J. Dilative arteriopathy in metabolic myopathies, particularly Pompe's disease. Acta Neurol Belg. 2012;112:15–8. doi: 10.1007/s13760-012-0009-1. [DOI] [PubMed] [Google Scholar]
- 7.Finsterer J, Mahjoub SZ. Primary mitochondrial arteriopathy. Nutr Metab Cardiovasc Dis. 2012;22:393–9. doi: 10.1016/j.numecd.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Garzuly F, Maródi L, Erdös M, Grubits J, Varga Z, Gelpi E, Rohonyi B, Mázló M, Molnár A, Budka H. Megadolichobasilar anomaly with thrombosis in a family with Fabry's disease and a novel mutation in the alpha-galactosidase A gene. Brain. 2005;128:2078–83. doi: 10.1093/brain/awh546. [DOI] [PubMed] [Google Scholar]
- 9.Guiral H, Risco J, Ferrer F. Otoneurological manifestations of basilar dolicoectasia. A report of six cases. Acta Otorrinolaringol Esp. 1997;48:337–40. [PubMed] [Google Scholar]
- 10.Heckmann JG, Ernst S. Central Alveolar Hypoventilation (Ondine's Curse) Caused by Megadolichobasilar Artery. J Stroke Cerebrovasc Dis. 2013;doi:pii: S1052–3057(13)00031-1. doi: 10.1016/j.jstrokecerebrovasdis.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Ichikawa H, Mukai M, Ohno H, Shimizu Y, Itaya K, Kawamura M. Dee white matter hyperintensities, decreased serum low-density lipoprotein, and dilative large arteriopathy. J Stroke Cerebrovasc Dis. 2012;21:225–30. doi: 10.1016/j.jstrokecerebrovasdis.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Ichikawa H, Takahashi N, Mukai M, Katoh H, Akizawa T, Kawamura M. Intracranial dilative arteriopathy is associated with chronic kidney disease and small vessel diseases in the elderly. J Stroke Cerebrovasc Dis. 2009;18:435–42. doi: 10.1016/j.jstrokecerebrovasdis.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Ishikawa T, Nagayama M, Iida M, Shinohara Y. Bulbovascular compression by megadolichobasilar artery manifested as neurogenic and refractory hypertension. Rinsho Shinkeigaku. 2004;44:359–64. [PubMed] [Google Scholar]
- 14.Ikeda K, Iwasaki Y. Megadolichobasilar artery and neurogenic hypertension. Rinsho Shinkeigaku. 2004;44:707–10. [PubMed] [Google Scholar]
- 15.Klinge H, Braunsdorf WE. Clinical signs associated with megadolichobasilar artery anomaly. Neurosurg Rev. 1991;14:303–7. doi: 10.1007/BF00383269. [DOI] [PubMed] [Google Scholar]
- 16.Krasnianski M, Gaul C, Neudecker S, Behrmann C, Schlüter A, Winterholler M. Yawning despite trismus in a patient with locked-in syndrome caused by a thrombosed megadolichobasilar artery. Clin Neurol Neurosurg. 2003;106:44–6. doi: 10.1016/s0303-8467(03)00045-3. [DOI] [PubMed] [Google Scholar]
- 17.Laforêt P, Petiot P, Nicolino M, Orlikowski D, Caillaud C, Pellegrini N, Froissart R, Petitjean T, Maire I, Chabriat H, Hadrane L, Annane D, Eymard B. Dilative arteriopathy and basilar artery dolichoectasia complicating late-onset Pompe disease. Neurology. 2008;70:2063–6. doi: 10.1212/01.wnl.0000313367.09469.13. [DOI] [PubMed] [Google Scholar]
- 18.Lemke AJ, Sander B, Benndorf G, Balzer J, Boerschel MF, Hosten N, Sprung C, Ricke J, Felix R, Lanksch WR. Megadolichobasilar artery as a rare cause of hydrocephalus internus synopsis of modern imaging methods. Aktuelle Radiol. 1995;5:310–4. [PubMed] [Google Scholar]
- 19.Mitsias P, Levine SR. Cerebrovascular complications of Fabry's disease. Ann Neurol. 1996;40:8–17. doi: 10.1002/ana.410400105. [DOI] [PubMed] [Google Scholar]
- 20.Okabe S, Oda N, Ishii M. Agenesis of left internal carotid artery associated with megadolichobasilar anomaly and olivopontocerebellar atrophy. Rinsho Shinkeigaku. 1989;29:1395–400. [PubMed] [Google Scholar]
- 21.Otterstedde CR, Tischendorf M, Reisser C. Megadolichobasilar artery as the etiology of sensorineural deafness in differential sudden deafness diagnosis. HNO. 1999;47:494–6. doi: 10.1007/s001060050411. [DOI] [PubMed] [Google Scholar]
- 22.Roth C, Gaiser T, Nagelmeier I, Rüschoff J, Ferbert A. Type I neurofibromatosis and megadolichobasilar artery. Nervenarzt. 2007;78:1195–9. doi: 10.1007/s00115-007-2263-7. [DOI] [PubMed] [Google Scholar]
- 23.Santos-Garcia D, Prieto JM, Blanco-Gonzalez M, Iglesias-Gomez S, Rodriguez-Constenla I, Lema M. SUNCT syndrome secondary to megadolichobasilar anomaly. Rev Neurol. 2005;41:638–9. [PubMed] [Google Scholar]
- 24.Shirakuni T, Tamaki N, Matsumoto S, Fujiwara M. Megadolichobasilar anomaly associated with brain stem infarction a case report. J Comput Tomogr. 1985;9:79–81. doi: 10.1016/0149-936x(85)90055-4. [DOI] [PubMed] [Google Scholar]
- 25.Uncini A, Lugaresi A, Porrini AM, Gallucci M. Recurrent cranial nerve palsies, midbrain infarction and hydrocephalus due to megadolichobasilar artery. Ital J Neurol Sci. 1990;11:489–92. doi: 10.1007/BF02336569. [DOI] [PubMed] [Google Scholar]
- 26.Unkelbach MH, Radeloff A, Bink A, Gstöttner W, Ziemann U. Megadolichobasilar anomaly causing acute deafness with vertigo. HNO. 2008;56:62–4. doi: 10.1007/s00106-006-1498-0. [DOI] [PubMed] [Google Scholar]
- 27.Uyama E. Fabry disease in light of recent review. Brain Nerve. 2008;60:1235–44. [PubMed] [Google Scholar]
- 28.Yoshida M, Asano M. Direct compression by megadolichobasilar anomaly as a cause of trigeminal neuralgia; a case diagnosed by MRI. Tohoku J Exp Med. 1994;172:327–32. doi: 10.1620/tjem.172.327. [DOI] [PubMed] [Google Scholar]
- 29.Zhang ZQ, Niu ST, Liang XH, Jian F, Wang Y. Vascular involvement in the pathogenesis of mitochondrial encephalo-myopathies. Neurol Res. 2010;32:403–8. doi: 10.1179/016164110X12670144526345. [DOI] [PubMed] [Google Scholar]