Abstract
Objectives:
To review cases of ovarian cysts managed at a University Hospital, and to identify the factors necessitating the use of laparotomy over laparoscopy.
Methods:
We carried out a retrospective chart review of all cases of ovarian cysts diagnosed and managed at the Department of Obstetrics & Gynecology, King Abdulaziz University Hospital, Jeddah, Saudi Arabia between January 2010 and August 2014. All data collected from medical record charts, patents details, clinical presentations, ovarian cysts description, and pathology type were recorded, and management by laparoscopy or laparotomy was identified. Ethical approval was obtained from ethical hospital committee.
Results:
There were 244 cases of ovarian cysts during the study period. The age ranged from 3 months to 77 years of age. The parity from 0-6. The height range from 37-180 cm. The weight range from 3-161 kg, and calculated body mass index ranged from 12-47. Out of 244 patients diagnosed, 165 were married (67.4%). Of those, only 16 patients were pregnant (6.6%). The most common presentation was abdominal pain in 142 patients (58.2%). Only 79.9% were ovarian cysts, and 17.5% were either para-ovarian or retroperitoneal. The right ovaries were affected in 63.1%, and only 18.9% were bilateral. The types of ovarian cysts included functional cysts 33.2%, benign cyst-adenoma 19.3%, and dermoid cysts 12.3%.
Conclusion:
Factors associated with laparotomy management rather than laparoscopy included older age >35, single, pregnant, or patients presenting with abdominal pain, and more than one cyst.
An ovarian cyst is a common gynecological problem and is divided into 2 main categories; physiological and pathological.1 Physiological cysts are follicular cysts and luteal cysts. Pathological cysts are considered as ovarian tumors, which might be benign, malignant, and borderline. Benign tumors are more common in young females, but malignant are more frequent in elderly females.2 Most ovarian cysts are asymptomatic and disappear spontaneously. When ovarian cysts are large, they may cause abdominal discomfort. If pressing on the bladder it may also cause frequency of urination.3 The signs and symptoms of ovarian cysts may include; pelvic pain, dysmenorrheal, and dyspareunia. Other symptoms are nausea, vomiting, or breast tenderness, fullness and heaviness in the abdomen and frequency and difficulty emptying of the bladder.4 Patients with clear, simple ovarian cysts diagnosed by ultrasound might not require any treatment. However, monitoring using serial ultrasonography was carried out in women with simple ovarian cysts smaller than 5 cm in diameter and a normal CA 125. There is a good evidence to suggest safety of observing even a 10 cm ovarian cyst.5,6 The aim of this study is to review cases of ovarian cysts treated at a university hospital, and to analyze the method of management and factors affecting the decision regarding the method of management (laparoscopy versus laparotomy).
Methods
We carried out a retrospective medical charts review of all cases of ovarian cysts diagnosed and managed at the Department of Obstetrics and Gynecology, King Abdulaziz University Hospital (KAUH), Jeddah, Saudi Arabia, between January 2010 and August 2014. Ethical approval was obtained from the hospital ethical committee. The study included 244 cases diagnosed as ovarian cysts. The data collected from medical record charts included; age in years, nationality (Saudi or non-Saudi), parity, weight in kilograms, height in centimeters, body mass index (BMI), the patient’s marital status (single, married, or having been married), whether patient was pregnant or not. Also, their clinical presentation, such as vaginal bleeding, abdominal pain or swelling, and infertility was reviewed and collected. In addition, asymptomatic women found to have an ovarian cyst as an “incidental” finding on ultrasound examination for other reasons, such as pregnancy, were included in this study. The number of cysts, unilateral or bilateral, clear cysts or complicated, plus the location or side of the cysts and type (functional, simple clear, dermoid, endometriosis, cystadenoma, malignant, and complicated) were all recorded. Finally, how they were managed either by laparoscopy or laparotomy was documented.
Inclusion and exclusion criteria
Patients admitted with a diagnosis of ovarian cysts and managed at KAUH were included. Exclusion criteria cases were those transferred to another facility, or if we found their chart was incomplete.
The IBM SPSS Statistics for Windows version 22.0 (IBM Corp, Armonk, NY, USA) was used to analyze data. Variables included age in years, nationality Saudi and non-Saudi, married or not, parity, height in cm, weight, BMI, and pregnant or not. Clinical presentation abdominal pain or otherwise, number of cysts, location and type of cysts was also included. The mean and standard deviation was calculated for the continuous variables. Frequency and percentage of other nominal variables were also computed. Using bivariate correlation, the different data variables were analyzed according to the surgical management; with the code 0 for laparoscopy, and 1 for laparatomy. In addition, Pearson correlation and logistic regression were carried out determining factors affecting the choice of surgical modality used.
Results
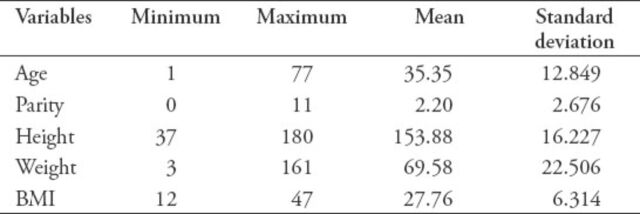
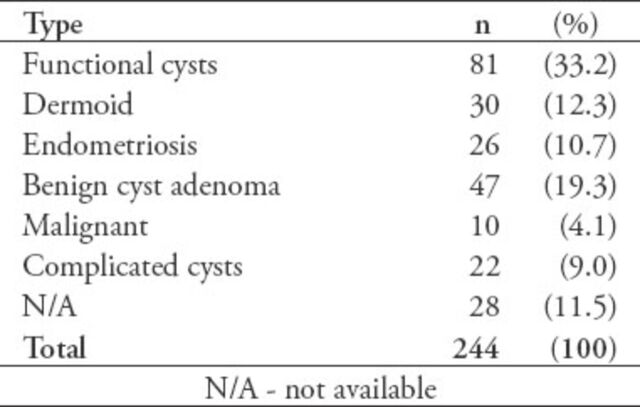
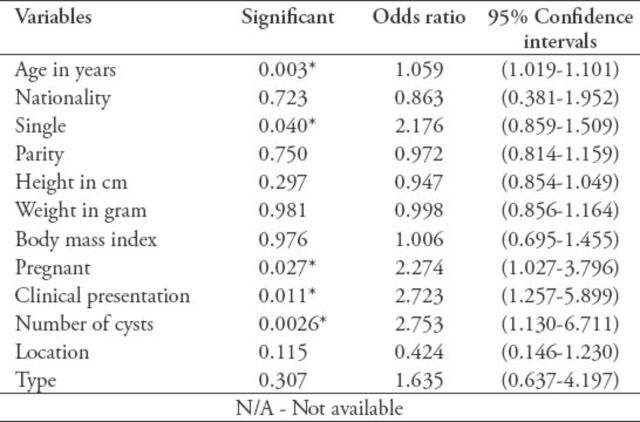
A total of 244 cases of ovarian cysts were included. The mean ± standard deviation [SD] age of these patients was 35.35±12.849 years. The mean±SD parity was 2.20±2.676. The height ranged was from 37-180 cm with a mean±SD of 153.88±16.227. The weight ranged from 3-161 kg with a mean±SD of 69.58±22.506. The calculated BMI ranged from 12-47 with a mean±SD of 27.76±6.314 (Table 1). Out of 244 patients diagnosed with ovarian cysts, 165 were married (67.4%), and of those only 16 were pregnant (6.6%). The most common clinical presentation was abdominal pain in 142 patients (58.2%). Only 79.9% were ovarian cysts, and 17.5% were either para- ovarian or retroperitoneal. The most common affected was the right ovaries (63.1%) and only 18.9% were bilateral (Table 2). The type of ovarian cysts were recorded accordingly; 33.2% were functional cysts, 19.3% benign cyst adenoma, and 12.3% dermoid cysts (Table 3). Factors that are associated with the use of laparotomy for management rather than laparoscopy; older age >35 (odds ratio [OR] = 1.059; 95% confidence interval [CI]: 1.019-1.101), single (OR = 2.176; 95% CI: 0.859-1.509), pregnant (OR = 2.274; 95% CI: 1.027-3.796), patients presenting with abdominal pain (OR = 2.723; 95% CI: 1.257-5.899), and if more than one cysts (OR = 2.753; 95% CI: 1.130-6.711) (Table 4).
Table 1.
Demographic characteristics of 244 cases diagnosed with ovarian cysts.
Table 2.
Analysis of 244 cases diagnosed with ovarian cysts.
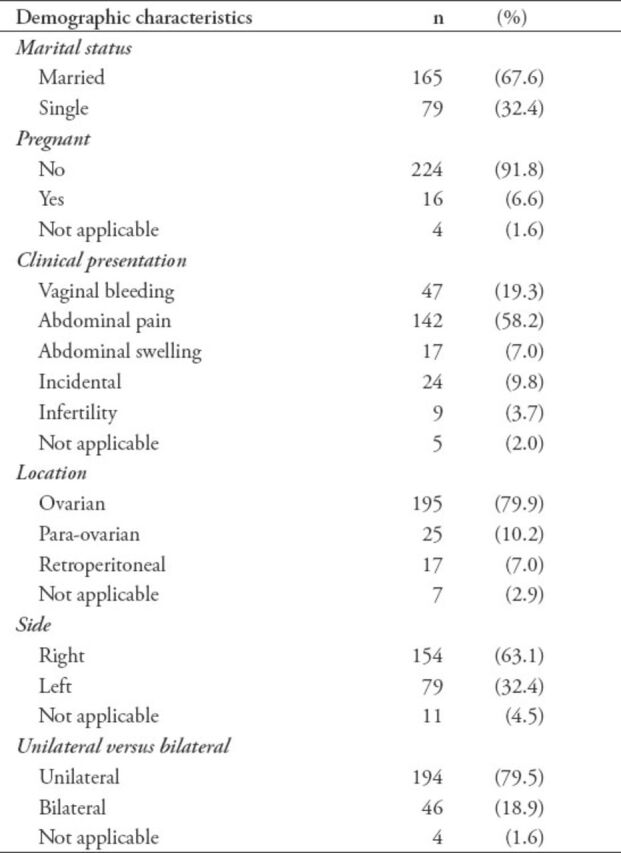
Table 3.
Type of ovarian cysts including the frequency in number and percentage.
Table 4.
Factors affecting decisions of ovarian cysts.
Discussion
Functional ovarian cysts are common in women of reproductive age, but rare after menopause. It can occur at any age including the fetus (in uterus).1 In the present study, the patients were of all ages, the youngest 3-months-old, and the eldest 77 years old.7 Treatment of ovarian cysts with laparoscopy was found to be a safe and effective method in young females provided that features of the cyst was benign and malignancy was not suspected clinically.8 It was found clinical features of the cysts correlated well with the final pathology.
Symptomatic patients commonly present with abdominal pain, although most of the patients are asymptomatic and the cysts were found accidently by bimanual examination or ultrasound. Pain can present as dull ache or pain in the lower back or abdomen. Acute severe pain can occur in complicated ovarian cysts, torsion, infarction, or hemorrhage.9 The incidence of ovarian cysts in pregnant women is one out of 600. Most are benign cysts, and 50% are mature cystic teratoma, followed by benign cyst adenomas (20%). Ovarian cancer contributes to only 0.6% of cases and 13% of functional ovarian cysts.10 When managing giant benign ovarian cysts, laparoscopy is considered a safe and minimally invasive surgical procedure.11 Ultrasound-guided drainage with excision of giant ovarian cysts is a safe and appropriate modality of treatment. Even in suspected torsions; laparoscopy can be used to diagnose and treat these cases.12 In an Iranian study,13 functional cysts (57%) were the most common benign ovarian mass followed by serous cyst adenoma (13%), and dermoid cyst (10%). In a study from Ireland,14 the most common was endometrioma (29%) followed by dermoid cyst (24%), and functional cyst (19%).14 In an Italian study,15 the most common was also endometrioma (19%) followed by functional cyst (18%).15 In our study, the most common was functional cysts (33%) followed by cyst adenoma (19.3%), and endometriosis (10.7%).
In conservative management of ovarian cysts, the cysts can disappear or be under control. In a situation, where it has to be removed, this can be carried out laparoscopically or through a laparotomy.16 The traditional option for ovarian cyst removal is laparotomy, and this approach is the oldest method, and is an entirely invasive procedure. Over the last 2 decades, gynecologists have aimed for less invasive procedures in the pelvis; namely, laparoscopy. The choice of which procedure to use in most cases, will be laparoscopy if possible, and laparotomy is only used if there are contraindications with the use of laparoscopy, such as cardiopulmonary disease, history of previous operations in the pelvis, known adhesion in the abdominal cavity, and late trimester of pregnancy.17 One advantage of laparoscopic surgery of the ovary is that it is safe and effective and used for many indications for benign simple to more complicated hemorrhagic cysts, and many more gynecological problems.18 Other advantages of laparoscopy over laparotomy include; small scar, less operative time, fast recovery, fewer adhesions, and lower cost. In addition, laparoscopy is associated with less postoperative pain, less febrile complications, a reduction in the number of days in the hospital, and total cost.19
Certain factors such as umbilical hernia or the presence of mesh or adhesion, in cases of pregnancy, and obese patients makes laparoscopy difficult or dangerous, and the surgeon may choose laparotomy for the procedure, or non-umbilical access.20,21 In cases where adhesions are suspected in patients with a history of abdominal surgery or infection or others, micro laparoscopy is indicated instead of a blind trocar insertion or an alternate location for entry.22,23 Large pelvic mass, pregnancy, obesity, extreme thinness, and abdominal wall laxity all can dictate the surgeon to shift to laparotomy or use a different approach.24
Limitations of this study included its retrospective design, and management of patient by different consultants. Future study should be prospective, and management should be by either one consultant or by a protocol followed by group of consultants to identify the relevant factors.
In conclusion, the types of ovarian cysts were functional cysts in 33.2%, followed by benign cyst adenoma, and dermoid cysts. Factors that are associated with laparotomy for management rather than laparoscopy are older age >35, single, pregnant, patients presenting with abdominal pain, and more than one cyst.
Footnotes
Related Articles
Abdullah LS, Bondagji NS. Histopathological pattern of ovarian neoplasms and their age distribution in the western region of Saudi Arabia. Saudi Med J 2012; 33: 61-65.
Al-Nuaim LA. The impact of obesity on reproduction in women. Saudi Med J 2011; 32: 993-1002.
Rouzi AA. Operative laparoscopy in pregnancy for a large paraovarian cyst. Saudi Med J 2011; 32: 735-737.
References
- 1.Grimes DA, Jones LB, Lopez LM, Schulz KF. Oral contraceptives for functional ovarian cysts. Cochrane Database Syst Rev. 2014;4:CD006134. doi: 10.1002/14651858.CD006134.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hongqian L, Xiangao W, Donghao L, Zhihong L, Gang S. Ovarian masses in children and adolescents in China: analysis of 203 cases. J Ovarian Res. 2013;6:47. doi: 10.1186/1757-2215-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rofe G, Auslend R, Dirnfeld M. Benign ovarian cysts in reproductive-age women undergoing assisted reproductive technology treatment. Open J Obstet Gynecol. 2013;3:17–22. [Google Scholar]
- 4.Farghaly SA. Current diagnosis and management of ovarian cysts. Clin Exp Obstet Gynecol. 2014;41:609–612. [PubMed] [Google Scholar]
- 5.Medeiros L, Rosa D, Bozzetti M, Fachel J, Furness S, Garry R, Rosa M, et al. Laparoscopy versus laparotomy for benign ovarian tumour. Cochrane Database Syst Rev. 2009;2:CD004751. doi: 10.1002/14651858.CD004751.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Bottomley C, Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol. 2009;23:711–724. doi: 10.1016/j.bpobgyn.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Pérez-López F, Chedraui P, Troyano-Luque J. Peri- and post-menopausal incidental adnexal masses and the risk of sporadic ovarian malignancy: new insights and clinical management. Gynecol Endocrinol. 2010;26:631–643. doi: 10.3109/09513590.2010.487611. [DOI] [PubMed] [Google Scholar]
- 8.Seckin B, Ozdener T, Tapisiz OL, Batioglu S. Laparoscopic treatment of ovarian cysts in adolescents and young adults. J Pediatr Adolesc Gynecol. 2011;24:300–303. doi: 10.1016/j.jpag.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Goh W, Bohrer J, Zalud I. Management of the adnexal mass in pregnancy. Curr Opin Obstet Gynecol. 2014;26:49–53. doi: 10.1097/GCO.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 10.Surampudi K, Nirmalan PK, Gundabattula SR, Chandran JB. Management of adnexal masses in pregnancy: our experience from a tertiary referral perinatal centre in South India. Arch Gynecol Obstet. 2015;291:53–58. doi: 10.1007/s00404-014-3395-1. [DOI] [PubMed] [Google Scholar]
- 11.Dubuisson J, Fehlmann A, Petignat P. Management of presumed benign giant ovarian cysts: a minimally invasive technique using the alexis® laparoscopic system. J Minim Invasive Gynecol. 2015;22:540. doi: 10.1016/j.jmig.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 12.Murawski M, Gołębiewski A, Sroka M, Czauderna P. Laparoscopic management of giant ovarian cysts in adolescents. Wideochir Inne Tech Malo Inwazyjne. 2012;7:111–113. doi: 10.5114/wiitm.2010.22530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arab M, Hashemi M, Masoumi N, Yaseri M, Golfam F, Ebrahimi M. Surgical histopathology of benign ovarian cysts: a multicentre study. Iranian Journal of Pathology. 2010;5:132–136. [Google Scholar]
- 14.Alcázar JL, Guerriero S, Laparte C, Ajossa S, Ruiz-Zambrana A, Melis GB. Diagnostic performance of transvaginal gray-scale ultrasound for specific diagnosis of benign ovarian cysts in relation to menopausal status. Maturitas. 2011;68:182–188. doi: 10.1016/j.maturitas.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Guerriero S, Alcazar JL, Pascual MA, Ajossa S, Gerada M, Bargellini R, et al. Diagnosis of the most frequent benign ovarian cysts: is ultrasonography accurate and reproducible? J Womens Health (Larchmt) 2009;18:519–527. doi: 10.1089/jwh.2008.0997. [DOI] [PubMed] [Google Scholar]
- 16.Kirkham YA, Kives S. Ovarian cysts in adolescents: medical and surgical management. Adolesc Med State Art Rev. 2012;23:178–191. [PubMed] [Google Scholar]
- 17.Bottomley C, Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol. 2009;23:711–724. doi: 10.1016/j.bpobgyn.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Kumar A, Pearl M. Mini-laparotomy versus laparoscopy for gynecologic conditions. J Minim Invasive Gynecol. 2014;21:109–114. doi: 10.1016/j.jmig.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 19.Medeiros LR, Rosa DD, Bozzetti MC, Fachel JM, Furness S, Garry R, et al. Laparoscopy versus laparotomy for benign ovarian tumour. Cochrane Database Syst Rev. 2009;(2):CD004751. doi: 10.1002/14651858.CD004751.pub3. [DOI] [PubMed] [Google Scholar]
- 20.Cuss A, Bhatt M, Abbott J. Coming to terms with the fact that the evidence for laparoscopic entry is as good as it gets. J Minim Invasive Gynecol. 2015;22:332–341. doi: 10.1016/j.jmig.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 21.Krpata DM, Ponsky TA. Needlescopic surgery: what’s in the toolbox? Surg Endosc. 2013;27:1040–1044. doi: 10.1007/s00464-012-2548-1. [DOI] [PubMed] [Google Scholar]
- 22.Afors K, Centini G, Murtada R, Castellano J, Meza C, Wattiez A. Obesity in laparoscopic surgery. Best Pract Res Clin Obstet Gynaecol. 2015;29:554–564. doi: 10.1016/j.bpobgyn.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 23.McIlwaine K, Manwaring J, Ellett L, Cameron M, Readman E, Villegas R, et al. The effect of patient body mass index on surgical difficulty in gynaecological laparoscopy. Aust N Z J Obstet Gynaecol. 2014;54:564–569. doi: 10.1111/ajo.12258. [DOI] [PubMed] [Google Scholar]
- 24.Kassir R, Blanc P, Lointier P, Tiffet O, Berger JL, Amor IB, et al. Laparoscopic entry techniques in obese patient: veress needle, direct trocar insertion or open entry technique? Obes Surg. 2014;24:2193–2194. doi: 10.1007/s11695-014-1452-2. [DOI] [PubMed] [Google Scholar]