Abstract
Objectives:
To review the epidemiology of scorpion sting in Qatar, to explore both the clinical significance, and the role of the emergency department (ED) in the management of such cases.
Methods:
In this retrospective study, we reviewed the records of all scorpion sting cases presented to the ED of Hamad General Hospital, Doha, Qatar between October 2010 and May 2013.
Results:
A total of 111 cases of scorpion stings were reviewed, 81 (72.9%) were males and 30 (27.1%) were females, with a mean age of 38 years. Localized pain was the most frequent presenting complaint (89 [80.2%]), whereas localized redness (44 [39.6%]) and swelling (38 [34.2%]) were the most common clinical signs. Abroug’s classification was used, and all cases were found to be class I. All patients received symptomatic treatment and were sent home.
Conclusion:
Scorpion sting problem in Qatar has a low clinical significance. Data from such studies should be utilized to create more specific (local) management guidelines, which should be more efficient with more rational utilization of ED resources.
Scorpion sting cases are a frequent presentation to emergency departments (EDs) in many areas around the world; in certain regions it is encountered on a daily basis. Scorpions are arachnids that have been on Earth for over 400 million years.1 Scientific literature reports approximately 2000 species,2 despite the huge number, only very few, approximately 25 of these species are recognized to be medically significant to human.3 Toxins vary according to species, and consist of a mixture of proteins and other substances.4 Worldwide, the overall estimated number of scorpion stings is approximately 1.2 million per year, with approximately 3250 deaths per year (0.3%).5 The clinical presentation can be challenging for emergency physicians, this is based on the wide spectrum of the clinical manifestations, which ranges from simple localized skin signs to critical conditions with possible fatality.6,7 Current available guidelines for management of scorpion sting mainly focus on symptomatic treatment and observation; some clinical protocols indicate recognition of the type of the scorpion based on discretion provided by the victim, which can be difficult in most of the cases or even misleading.6 In EDs, prolonged observation and monitoring of scorpion sting victims can be a burden to these departments, which are usually overloaded and expected to be efficient. Many published studies on scorpion sting cases (wherein the majority agreed that the general threat to human health is low)7-9 provide descriptive reviews of clinical and demographic aspects, and rarely focus on creating efficient management guidelines. This study reports scorpion sting cases from Qatar, and in addition to the clinical aspects, it raises the need for forming less redundant guidelines for management of scorpion sting cases in EDs, aiming for more resourceful utilization of EDs, and more efficient clinical management.
Methods
In this study, all scorpion sting cases presenting to the ED, Hamad General Hospital, Doha, Qatar (the main tertiary care hospital in Qatar) between October 2010 and May 2013 were included. Sting cases which were not confirmed by history to be due to scorpion were excluded. Collected data included demographic data (including age, gender, and so forth), clinical characteristics (signs, symptoms, time intervals, vital signs, clinical condition), and management steps (medications and disposition). Data were entered onto an Excel spreadsheet, checked for accuracy and reviewed prior to analyses by study investigators. Ethical approval was obtained from the ethics committee of the Medical Research Center, Hamad Medical Corporation in accordance with ethical standards laid down by the Declaration of Helsinki. Extracted data were reviewed and analyzed, and the Abroug’s classification8 was utilized to grade the clinical severity of envenomation for all cases recorded, class I: localized symptoms; class II: localized symptoms and general symptoms, class III: localized symptoms, and general symptoms, together with systematic involvement (systemic): cardiovascular, respiratory, and/or neurological disorders.
Results
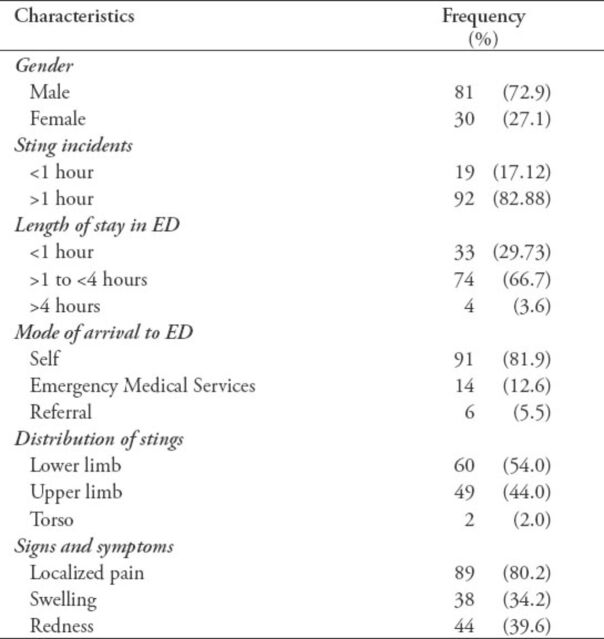
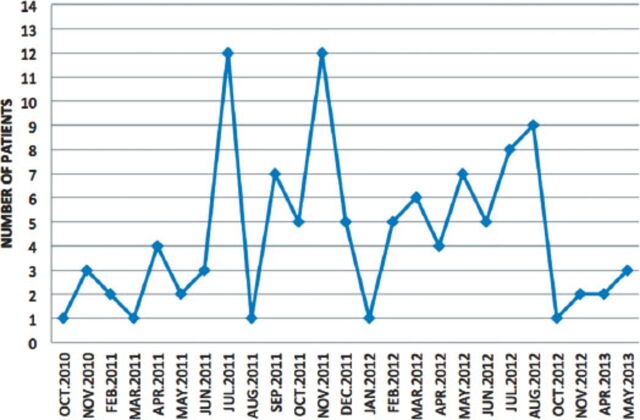
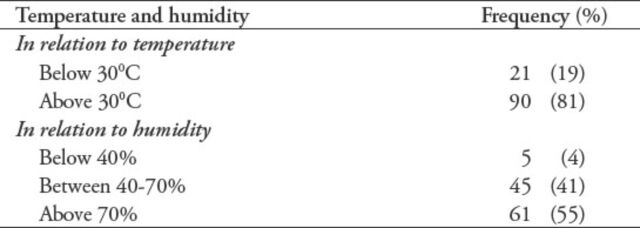
At the time of this study, the total population in Qatar was approximately 1.9 million (Qatar Statistics Authority, Qatar). Hamad General Hospital is the main tertiary care hospital in Qatar with an average of 240,000 visits to the ED annually. During the study period (October 2010 to September 2013), the total number of scorpion sting cases reviewed was 111 (Table 1). The gender distribution showed 72.9% males and 27.1% females. The age of the victims ranged from 1-73 year old, and mostly were young males (mean age of 38 years). Out of 23 nationalities involved, 22 (19.8%) of the stings occurred in the local population. Most of the incidents occurred during summer months as shown in Figure 1, and more than half of the patients (n=61 [54.9%]) were stung during day time between 6:00 am to 6:00 pm. Table 2 summarizes the temperature and humidity records on days of stings. Mode of arrival to the hospital was reviewed (Table 1).
Table 1.
Characteristics of scorpion sting patients among 111 patients presenting to the Emergency Department (ED), Hamad General Hospital, Doha, Qatar.
Figure 1.
Stings in relation to months in each year among 111 patients presenting to the Emergency Department, Hamad General Hospital, Qatar.
Table 2.
Frequency of scorpion stings according to temperature and humidity among 111 patients presenting to the Emergency Department, Hamad General Hospital, Qatar.
Different treatment regimens were implemented, in general 107 (96.4%) patients received treatment in the ED, out of that: 78 (70.2%) patients received analgesia, 76 (68.4%) patients received tetanus toxoid, and 19 (17.1 %) patients received steroids. Four (3.6%) patients did not receive any parenteral treatment in the ED. The length of stay was classified into 3 groups, 74 (66.6%) of the patients stayed from 1-4 hours, and 33 (29.7%) patients stayed for <1 hour. Only 4 (3.6%) patients stayed beyond 6 hours for observation. All patients presented with only localized signs and symptoms, none of them had systemic manifestation, According to Abroug’s classification, all of our patients (100%) were class I. All patients were discharged in good condition.
Discussion
The epidemiological aspect of scorpion sting is poorly studied worldwide5 including the Arabian Peninsula, where a few published articles have explored the size and the clinical significance of this encounter. We review scorpion sting epidemiology in the state of Qatar on the northeastern coast of the Arabian Peninsula. Except Antarctica, scorpions can be found in all continents,9,10 mostly in tropical, subtropical, and partly in temperate zones. While dry and hot regions are the natural habitat for these creatures, some species live in forests and wet savannas. In general, scorpions are shy, non-aggressive, nocturnal creatures that typically lie in wait for their prey, and only sting if threatened.11 The scorpion species that is considered medically dangerous belongs to the family of Buthidae, which is the largest group in scorpion families (more than 800 scorpion species), and is mainly found in North Africa, Asia, Middle East, and India, and represented by the genera Androctonus, Buthus, Mesobuthus, Buthotus, Parabuthus, and Leirus. Among the 2000 species; approximately 25 are medically significant to humans. In the Arabian Peninsula, 2 scorpion families have been identified, the Buthidae and the Scorpionidae,12 but no work has yet begun specifically in Qatar to determine how many species of scorpion are available. The real number of scorpion stings is expected to be much higher than what was announced, as many of the incidents happen in regions where a scorpion sting is common, and victims prefer traditional treatment over medical care. This study has recorded 111 cases of scorpion stings over a period of 36 months (October 2010 to September 2013), where all of the cases were found to be class I according to Abroug’s classification, both facts reflects the low gravity of this clinical problem in the state of Qatar. In other studies,13 none of the class I patients on the same classification system with localized signs and symptoms progressed to death. In the current study, the higher rate of stings in young males (72.9%) compared with females (27%) could be attributed to the demographic and social aspects in Qatar. In other studies, it was well demonstrated that most incidents occurred in summer months,3,6 which is true in this study as well. Weather factors, specifically temperature and humidity were found to be strongly correlated to the rate of stings. It was noted that 90 (81%) of the stings happened when the temperature was above 30°C, and only 21 (19%) occurred when temperature was below 30°C, in addition, 106 (96%) of the stings occurred when the humidity was above 40%. These factors could be considered for prevention such as avoiding or reducing desert tips, camping and similar outdoor activities when temperature were >30°C and humidity 40%. In this study, the vast majority of stings (109 patients [98%]) occurred in the limbs, this can be explained by the shy non aggressive nature of scorpions. The records of vital signs of all patients were within normal limits from the time they presented to the hospital until the end of treatment and disposition. All patients in this study had only localized manifestation (pain n=89 [80.2%], redness n=44 [39.6%], and swelling n=38 [34.2%]) with no systemic involvement, despite this, it is possible that the scaring reputation of scorpion stings and the public fear lead to 14 (12.6%) victims transported by the Emergency Medical Services, and 6 (5.5%) were referred from other healthcare facilities to the ED. The localized signs and symptoms can be attributed to allergic rather that toxic etiology, keeping in mind the complex composition of scorpions venom, which includes mucopolysaccharides, hyaluronidase, phospholipase, serotonin, histamine, enzyme inhibitors, neurotoxic peptides, and other proteins.14-17 The signs and symptoms of scorpion envenomation begin instantly within a few minutes of the sting and progress over several hours.3,18,19 In our study, all cases presented after at least 50 minutes of the sting, with localized non-progressive manifestations, and with totally absent signs of systemic toxicity, which are usually neurological, cardiovascular, and respiratory. This type of presentation can predict the nontoxic nature of the stings, which requires only symptomatic treatment.20 This was supported by the fact that 78 (70.2%) patients received only analgesic medication (either local infiltration with aesthetic agent or parenteral analgesia), 19 (17.1%) patients received steroids, and 4 (3.68%) patients did not require any immediate treatment in the ED and they were sent home with prescriptions. Lack of such data in the past caused the variability in decisions made on patients treatment and disposition, that was reflected by the variability in length of stay among all of the 111 stable patients, data showed that 73 (66%) patients stayed in the ED for 1-4 hours, 34 (31%) patients stayed for <1 hour, and only 3% of the patients stayed beyond 6 hours for observation. Data regarding length of stay can help in understanding patients flow in such crowded ED. The above data can lead to a better understanding of the nature of this problem in Qatar where we concluded that scorpion sting is not a serious clinical problem, therefore, more conservative management for such cases should be expected, but a lot of work is needed to identify the common scorpion species. It is a public understanding that scorpion stings are serious or even fatal incidents, and it represents a frightening situation for many people, leading them to seek medical care in EDs. Data extracted from scorpion stings review studies should be utilized to help in making decisions regarding the toxicity of local scorpions in each region separately as toxicity varies from species to species, this should result in clear guidelines and more efficient management plans.3,21,22 In our study, all patients presented to the ED with scorpion sting during a period of 36 months were reviewed. All patients showed localized signs and symptoms, minimum treatment was required, and all had an excellent outcome.
This study is limited mainly by the unavailability of some clinical data due to the retrospective design of the study.
In conclusion, we suggest that scorpion sting cases should be managed according to the level of clinical significance in each region. In our study, this can be symptomatic treatment at any suitable medical facility (not necessarily EDs) with a more rational utilization of medical resources.
Footnotes
Related Articles
Al Asmari AK, Al Zahrani AG, Al Jowhary S, Arshaduddin M. Clinical aspects and frequency of scorpion stings in the Riyadh Region of Saudi Arabia. Saudi Med J 2012; 33: 852-858.
Al-Asmari AK, Al-Seif AA, Hassen MA, Abdulmaksood NA. Role of prazosin on cardiovascular manifestations and pulmonary edema following severe scorpion stings in Saudi Arabia. Saudi Med J 2008; 29: 299-302.
References
- 1.Ozkan O, Adiguzel S, Kar S, Kurt M, Yakistiran S, Cesaretli Y, et al. Effects of Androctonus crassicauda (Olivier, 1807) (Scorpiones: Buthidae) venom on rats: correlation among acetyl cholinesterase activities and electrolytes levels. J Venom Anim Toxins Trop Dis. 2007;13:69–81. [Google Scholar]
- 2.van der Meijden A, Lobo Coelho P, Sousa P, Herrel A. Choose your weapon: defensive behavior is associated with morphology and performance in scorpions. PLoS One. 2013;8:e78955. doi: 10.1371/journal.pone.0078955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mansour N. Waiting time and characteristics of taking in charge scorpion priced persons in Sidi-Bouzid region Institute Pasteur de Tunis, Tunis, Tunisia. Archives de l’Institut Pasteur de Tunis. 2001;78:25–31. [Google Scholar]
- 4.Quintero-Hernández V, Jiménez-Vargas JM, Gurrola GB, Valdivia HH, Possani LD. Scorpion venom components that affect ion-channels function. Toxicon. 2013;76:328–342. doi: 10.1016/j.toxicon.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chippaux JP, Goyffon M. Epidemiology of scorpionism: a global appraisal. Acta Trop. 2008;107:71–79. doi: 10.1016/j.actatropica.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Shahbazzadeh D, Amirkhani A, Djadid ND, Bigdeli S, Akbari A, Ahari H, et al. Epidemiological and clinical survey of scorpionism in Khuzestan province, Iran (2003) Toxicon. 2009;53:454–459. doi: 10.1016/j.toxicon.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Bawaskar HS, Bawaskar PH. Scorpion sting: a study of the clinical manifestations and treatment regimes. Curr Sci. 2008;95:1337–1341. [Google Scholar]
- 8.Abroug F, Nouira S, Saguiga H. Scorpion envenomation: Advanced chemical, physiopathologies and therapeutics. [Monogragh] 1994:1–68. [Google Scholar]
- 9.Dehesa-Dávila M, Martin BM, Nobile M, Prestipino G, Possani LD. Isolation of a toxin from Centruroides infamatus infamatus Koch scorpion venom that modifies Na+permeability on chick dorsal root ganglion cells. Toxicon. 1994;32:1487–1493. doi: 10.1016/0041-0101(94)90307-7. [DOI] [PubMed] [Google Scholar]
- 10.Chowell G, Díaz-Dueñas P, Bustos-Saldaña R, Mireles AA, Fet V. Epidemiological and clinical characteristics of scorpionism in Colima, Mexico (2000-2001) Toxicon. 2006;47:753–758. doi: 10.1016/j.toxicon.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Satyawali V, Pandey S, Prakash C, Singh Y. Scorpion Sting Masquerading As Myocardial Infarction. Journal of Indian Academy of Forensic Medicine. 2014;36:89–91. [Google Scholar]
- 12.Al-Asmari AK, Al-Saif AA, Abdo NM, Al Moutaery KR. New additions to the scorpion fauna of Riyadh region, Saudi Arabia. J Venom Anim Toxins Incl Trop Dis. 2009;15:612–632. [Google Scholar]
- 13.Hmimou R, Soulaymani A, Mokhtari A, Arfaoui A, Eloufir G, Semlali I, et al. Risk factors caused by scorpion stings and envenomations in the province of Kelâa Des Sraghna (Morocco) J Venom Anim Toxins Incl Trop Dis. 2008;14:628–640. [Google Scholar]
- 14.Müller GJ. Scorpionism in South Africa. A report of 42 serious scorpion envenomations. S Afr Med J. 1993;83:405–411. [PubMed] [Google Scholar]
- 15.Gwee MC, Nirthanan S, Khoo HE, Gopalakrishnakone P, Kini RM, Cheah LS. Autonomic effects of some scorpion venoms and toxins. Clin Exp Pharmacol Physiol. 2002;29:795–801. doi: 10.1046/j.1440-1681.2002.03726.x. [DOI] [PubMed] [Google Scholar]
- 16.Jalali A, Pipelzadeh MH, Sayedian R, Rowan EG. A review of epidemiological, clinical and in vitro physiological studies of envenomation by the scorpion Hemiscorpius lepturus (Hemiscorpiidae) in Iran. Toxicon. 2010;55:173–179. doi: 10.1016/j.toxicon.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 17.Ouanes-Besbes L, El Atrous S, Nouira S, Aubrey N, Carayon A, El Ayeb M, et al. Direct vs. mediated effects of scorpion venom: an experimental study of the effects of a second challenge with scorpion venom. Intensive Care Med. 2005;31:441–446. doi: 10.1007/s00134-005-2555-y. [DOI] [PubMed] [Google Scholar]
- 18.Mebs D. [Scorpions and snakes, such as cobras, mambas and vipers made the African continent famous for venomous animals] Bull Soc Pathol Exot. 2002;95:131. French. [PubMed] [Google Scholar]
- 19.Petricevich VL. Scorpion venom and the inflammatory response. Mediators Inflamm. 2010;2010:903295. doi: 10.1155/2010/903295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cesratli Y, Ozkan O. Scorpion stings in Turkey: Epidemiological and clinical aspects between the years 1995 and 2004. Rev Inst Med Trop (Sao Paulo) 2010;52:215–220. doi: 10.1590/s0036-46652010000400010. [DOI] [PubMed] [Google Scholar]
- 21.Antopolsky M, Salameh S, Stalnikowicz R. Need for emergency department observation after scorpion sting: prospective study and review of the literature in the Middle East. Eur J Emerg Med. 2009;16:206–208. doi: 10.1097/mej.0b013e32831f8f4a. [DOI] [PubMed] [Google Scholar]
- 22.Bouaziz M, Bahloul M, Kallel H, Samet M, Ksibi H, Dammak H, et al. Epidemiological, clinical characteristics and outcome of severe scorpion envenomation in South Tunisia: multivariate analysis of 951 cases. Toxicon. 2008;52:918–926. doi: 10.1016/j.toxicon.2008.09.004. [DOI] [PubMed] [Google Scholar]