Abstract
Objectives:
To determine the prevalence of thyroid cancer in patients with hyperthyroidism.
Methods:
This is a retrospective observational study using the data of 71 Omani patients with a diagnosis of hyperthyroidism due to Grave’s disease, toxic multinodular goiter, and solitary toxic adenoma. These patients underwent thyroidectomy at the Royal Hospital (RH), Muscat, Oman, and were followed up at the National Diabetes and Endocrine Center (NDEC) between 2007 and 2013. The details were collected from the medical records of both the RH and the NDEC. Patients who underwent thyroidectomy for other reasons like non-toxic goiter and hypothyroidism with cancer were excluded from the study.
Results:
Thyroid cancer was identified in 32.8% (n=23) of patients with hyperthyroidism. Half of these patients 52.1% (n=12) had papillary micro-cancer (intra-thyroidal), and 3 patients with Grave’s disease (13%) had lymph nodes metastasis (loco-regional infiltration. The cancer preponderance was higher in young (n=21, 91.3%) and female patients (n=18, 73.9%). Most patients with thyroid cancer had abnormal ultrasound neck findings and thyroid scintigraphy (99 mTc uptake).
Conclusion:
Many patients with hyperthyroidism in Muscat, Oman, especially those with Grave’s disease, show malignancy, and hence a proper initial evaluation of these patients is required as part of long-term management.
Hyperthyroidism is a state of over-functioning of the thyroid gland due to an autoimmune process as seen in Grave’s disease, or autonomous secretion as in toxic multi-nodular goiter or toxic adenoma. The association between thyroid cancer and hypothyroidism in Hashimoto’s thyroiditis is well known.1 The coexistence of thyroid cancer and hyperthyroidism was previously studied.2 These studies have demonstrated both an increased incidence of thyroid nodules and of thyroid cancer in patients with thyrotoxicosis. The role of the autoimmune processes in the origin and clinical course of thyroid cancer is still a subject of debate.3 The prevalence of palpable thyroid nodules in Grave’s disease is around 15.8%, and its detection may extend up to 33.6% using neck ultra-sonography.3 This raises concerns regarding the possible presence of thyroid malignancy. The incidence of thyroid cancer is probably high in patients with Grave’s disease presenting with a palpable nodule.4 However, micro cancer is discovered as an incidental finding in patients with Grave’s disease.5 There is controversy surrounding the disease course of thyroid cancer in hyperthyroid patients. Some studies suggested that thyroid cancer is more aggressive in Grave’s disease,6,7 though this is not a universal phenomenon.8 The discrepancies in the results seen are probably due to environmental, racial or other unknown factors.9 The published data on thyroid cancer with solitary toxic nodule or toxic multi-nodular goiter is scanty and anecdotal. To understand the association of thyroid cancer and thyrotoxicosis, this study retrospectively reviewed patients who had undergone thyroidectomy for hyperthyroidism.
Methods
This cohort study included subjects with hyperthyroidism who were managed with thyroidectomy at the Royal Hospital (RH), Muscat, Oman, and followed at the National Diabetes and Endocrine Centre (NDEC), Oman. We reviewed the data of all hyperthyroid patients that underwent thyroidectomy at RH between 2007 and 2013. Hyperthyroid patients with abnormal fine needle aspiration cytology (FNAc)results, and uncontrolled hyperthyroidism on higher dose of thionamides with nodules on US neck were sent for thyroidectomy, and all these patients were followed up at the NDEC after surgery. Collected variables were age, gender, diagnosis, findings of imaging studies, report of fine needle aspiration cytology (FNAc), and the indication for surgery. The RH is the largest hospital in the Sultanate of Oman and serves as the main tertiary care unit for many medical specialties including oncology and endocrine disorders. It accepts patients referred from secondary care centers in the governorates of Oman. The hospital has a team of highly skilled thyroid surgeons who perform approximately 150 thyroid surgeries annually. The NDEC is an outpatient division of the RH established in February 2013 and provides care for patients with diabetes and various endocrine disorders from all regions of Oman.
Inclusion and exclusion criteria
All patients, 17 years of age and older, and who underwent total thyroidectomy for hyperthyroidism were included in the study. Thyroidectomies for other reasons like non-toxic goiter or Hashimoto’s thyroiditis with thyroid cancer were excluded from the study. This study was carried out in accordance with the principles of the Helsinki Declaration. Ethical approval was obtained from the Research and Ethics Committee of the RH.
Statistical analysis
The analysis of the original data sets was carried out using IBM SPSS Statistics for Windows version 21.0 (IBM Corp, Armonk, NY, USA). This was a pooled analysis; hence, we used the same statistical models and variable categorization, wherever it was deemed to be feasible. Hence, the general inferences are similar, and p<0.05 was considered statistically significant. Data analysis was also carried out using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp, Armonk, NY, USA). Variables analyzed were age, gender, types of hyperthyroidism, cancer distributions in each group, tumour size, and extension. Pearson’s chi-square test was used to compare the categorical variables.
Results
Characteristics of the study sample
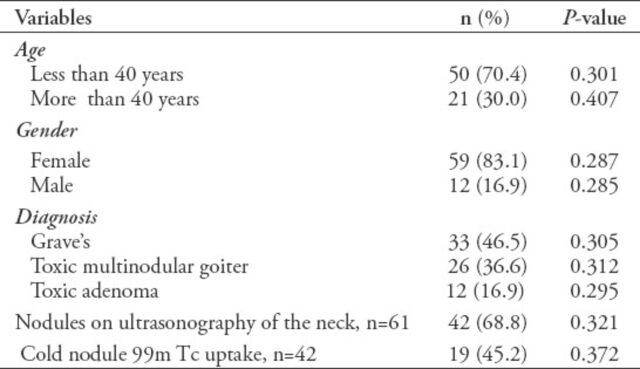
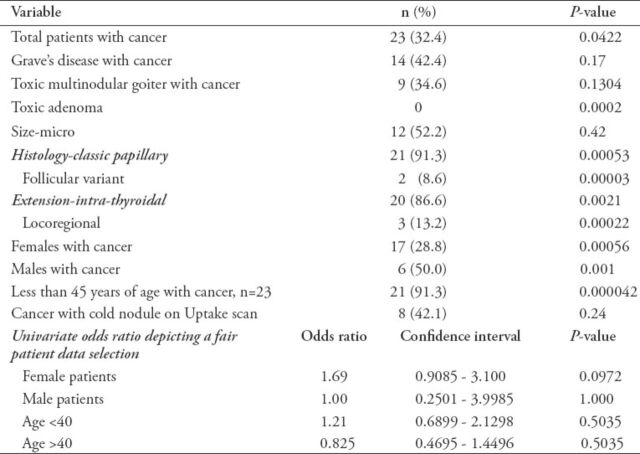
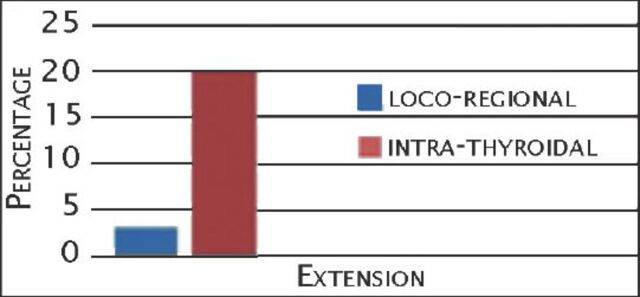
For every subject in each cohort we obtained age, gender, types of hyperthyroidism, and cancer distributions in each group, tumor size, and extension from the cohort. There were 71 patients in the cohort who ranged from 17-76 years. There was a female to male ratio of approximately 4:1. Thirty-three (46.5%) patients had Grave’s disease, 26 (36.6%) had toxic multinodular goiter (TMN), and 12 (16.9%) had toxic adenoma (TA). Most patients (n=61, 87%), had pre-operative imaging analysis with ultrasound (US) of the neck, and just over half (n=42, 60%) had 99 m Tc pertechnetate thyroid uptake scan. Half of the patients had fine needle aspiration. Table 1 summarizes demographics and disease characteristics. Out of 71 patients, 48 (67.6%) had benign changes, and 23 (32.4%, p=0.04) had cancerous changes (Table 2). Cancerous changes were seen more in Grave’s disease (n=14, 42%, p=0.17), followed by TMN (n=9 [39%], p=0.13), and no cancer was detected in patients with toxic adenoma (p=0.002). Out of 41 patients with nodules on uptake scan, 19 cases (46%) had cold nodules, and 8 cases (42%, p=0.24) of them had thyroid cancer. Among men, 50% (p=0.001) turned out to be cancerous. Seventeen female patients (28.8%, p=0.0005) had malignant changes. The distribution of thyroid cancer between the 3 types of hyperthyroid patients was observed, and in that the variables suggested were size, histology, and extensions. Histopathology examination revealed classic papillary thyroid cancer in almost all cancer patients (n=21 [91%], p=0.0005). One patient with Grave’s disease and one patient with toxic multi-nodular goiter had the follicular variant of papillary thyroid cancer. Most patients (n=20 [97%], p=0.002) had thyroid cancer confined to the thyroid gland (intra-thyroidal). Three cases with Grave’s disease had metastasis to cervical lymph nodes (loco-regional infiltration) (Figure 1). Just over half of the diagnosed patients (n=12 [56.5%], p=0.42) had tumor size of less than one centimeter (micro-cancer). It was observed that most of the patients diagnosed with cancer were young (age less than 45 years) (n=21, [91.3%], p=0.0004). Thyroid cancer was seen more in female patients (n=18, 78%), which is probably related to the larger females sample size in this study group. The opposite attribution could be made to the smaller sample (n=6, 50%) of hyperthyroid males who had thyroid cancer.
Table 1.
Demographics and characteristics of 71 patients with total thyroidectomy for hyperthyroidism.
Table 2.
Thyroid cancer distribution in 3 types of hyperthyroid patients.
Figure 1.
Percentage of thyroid cancer patients with metastasis to regional lymph nodes.
Discussion
On literature review, there is a scarcity of studies on thyroid cancer in hyperthyroid patients in the Gulf Cooperation Council (GCC) countries. This study explored the significant associations of thyroid cancer in hyperthyroid patients. Various literature reported thyroid cancer incidence between 0.8-9% of thyroidectomy patients with thyrotoxicosis.10,11 However, approximately one third of the patients with hyperthyroidism in this present study were affected by thyroid cancer. Stocker and Burch12 reported an increased incidence of nodules, and of thyroid cancer in patients with Grave’s disease. The malignancy rate of palpable thyroid nodules in Grave’s disease is approximately 16.9%.4 A similar picture is also observed from this study. Cancer was mainly detected in patients with hyperthyroidism due to Grave’s disease (42%). Most of the study population had abnormal US of neck and thyroid-uptake scan findings. Although studies carried out by Ocak et al10 reported the presence of thyroid cancer in patients with toxic adenoma, none of our patients with toxic adenoma had cancerous changes.
The autoimmune process of Grave’s disease may affect the clinical evolution of thyroid cancer by altering host immune responses.4 Hyperthyroidism does not protect patients from developing thyroid cancer, as was earlier believed. Thyroid stimulating hormone (TSH) has a central role in thyroid growth and functioning, and appears to play the same role in the development of thyroid cancer.11 However, many clinicians still consider it a rare event and treat patients with Grave’s using radioactive iodine therapy or long term medical therapy without proper assessment for coexisting thyroid nodules. The true incidence of thyroid cancer in patients with hyperthyroidism may be underestimated, especially when treated with long-term medical or radioactive iodine therapy. The TSH receptor antibody seen in Grave’s disease has led to the perception that thyroid cancer occurring in the context of Grave’s disease may become more aggressive.13 However, this view is not supported by many other studies.14 Hales et al14 described the variable behavior of thyroid cancer in hyperthyroid patients. Most patients in this study have not yet completed 3 years follow up, which prevented us from looking into the tumor prognostic behavior. Although a few follicular and medullar thyroid cancers were reported in some studies, many described papillary thyroid cancer as the most common form of cancer in hyperthyroid patients.
In this present study, 91% of thyroid cancer was of the papillary type, and more than 90% of thyroid cancer was intrathyroidal. As shown in the present study and previous literature, most thyroid carcinomas, which are associated with hyperthyroidism, are usually micro-cancers.15 Some studies showed that Grave’s disease patients with micro cancer have better outcome than patients with small thyroid cancer, which manifests clinically. Hyperthyroidism is more common among female gender than male (ratio - 7:1). Subsequently, studies also showed that thyroid cancer is seen more in female patients. In this current study, most of our cancer patients were also females (78%). However, it was observed that out of 12 total hyperthyroid males, 6 (50%) had thyroid cancer. Further studies including larger number of male patients with hyperthyroidism are needed to clarify gender association with thyroid cancer.
Although there are some limitations, such as small sample population, and the retrospective nature, this study, which included all possible cases, provides information on most hyperthyroid patients from Oman.
In conclusion, the diagnosis of thyroid cancer in thyrotoxic patients can be overlooked. Although there is insufficient evidence to base recommendations for any change in practice, clinicians managing hyperthyroidism need to be aware of the possible increased risk of thyroid cancer in this patient group. Therefore, prompt evaluation of all hyperthyroid patients is crucial to exclude the presence of co-existent malignancy. Ultrasonography of the neck and US-guided fine needle aspiration cytology (if indicated) should be considered for complete evaluation of these patients. Thyroidectomy may be considered in hyperthyroid patients in the presence of palpable nodules, or nodule on US of the neck, or if malignancy cannot be excluded by FNA biopsy.
Acknowledgment
We would like to thank Ms. Kavita G. Kreme writers group for her guidance in preparing this manuscript.
References
- 1.Zhang L, Li H, Ji QH, Zhu YX, Wang ZY, Wang Y, et al. The clinical features of papillary thyroid cancer in Hashimoto’s thyroiditis patients from an area with a high prevalence of Hashimoto’s disease. BMC Cancer. 2012;12:610. doi: 10.1186/1471-2407-12-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeh NC, Chou CW, Weng SF, Yang CY, Yen FC, Lee SY, et al. Hyperthyroidism and thyroid cancer risk: a population-based cohort study. Exp Clin Endocrinol Diabetes. 2013;121:402–406. doi: 10.1055/s-0033-1341474. [DOI] [PubMed] [Google Scholar]
- 3.Cirić J, Beleslin-Nedeljković B. [Differentiated thyroid carcinoma in previously manifested autoimmune thyroid disease] Srp Arh Celok Lek. 2005;133(Suppl 1):74–76. doi: 10.2298/sarh05s1074c. Serbian. [DOI] [PubMed] [Google Scholar]
- 4.Tamatea JA, Tu’akoi K, Conaglen JV, Elston MS, Meyer-Rochow GY. Thyroid cancer in Graves’ disease: is surgery the best treatment for Graves’ disease? ANZ J Surg. 2014;84:231–234. doi: 10.1111/j.1445-2197.2012.06233.x. [DOI] [PubMed] [Google Scholar]
- 5.Berker D, Isik S, Ozuguz U, Tutuncu YA, Kucukler K, Akbaba G, et al. Prevalence of incidental thyroid cancer and its ultrasonographic features in subcentimeter thyroid nodules of patients with hyperthyroidism. Endocrine. 2011;39:13–20. doi: 10.1007/s12020-010-9405-6. [DOI] [PubMed] [Google Scholar]
- 6.Belfiore A, Garofalo MR, Giuffrida D, Runello F, Filetti S, Fiumara A, et al. Increased aggressiveness of thyroid cancer in patients with Graves’ disease. J Clin Endocrinol Metab. 1990;70:830–835. doi: 10.1210/jcem-70-4-830. [DOI] [PubMed] [Google Scholar]
- 7.Yano Y, Shibuya H, Kitagawa W, Nagahama M, Sugino K, Ito K, et al. Recent outcome of Graves’ disease patients with papillary thyroid cancer. Eur J Endocrinol. 2007;157:325–329. doi: 10.1530/EJE-07-0136. [DOI] [PubMed] [Google Scholar]
- 8.Ahn D, Sohn JH, Jeon JH, Park J. Preoperative subclinical hyperthyroidism in patients with papillary thyroid carcinoma. Clin Exp Otorhinolaryngol. 2014;7:312–318. doi: 10.3342/ceo.2014.7.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pazaitou-Panayiotou K, Perros P, Boudina M, Siardos G, Drimonitis A, Patakiouta F, et al. Mortality from thyroid cancer in patients with hyperthyroidism: the Theagenion Cancer Hospital experience. Eur J Endocrinol. 2008;159:799–803. doi: 10.1530/EJE-08-0468. [DOI] [PubMed] [Google Scholar]
- 10.Ocak S, Akten AO, Tez M. Thyroid cancer in hyperthyroid patients: is it different clinical entity? Endocr Regul. 2014;48:65–68. doi: 10.4149/endo_2014_02_65. [DOI] [PubMed] [Google Scholar]
- 11.Edmonds CJ, Tellez M. Hyperthyroidism and thyroid cancer. Clin Endocrinol (Oxf) 1988;28:253–259. doi: 10.1111/j.1365-2265.1988.tb03662.x. [DOI] [PubMed] [Google Scholar]
- 12.Sarma SD, Kumar G, Kaddour H. Thyroid cancer and hyperthyroidism. Otolaryngyl Head & Neck Surg. 2014;151:182. [Google Scholar]
- 13.Pazaitou-Panayiotou K, Michalakis K, Paschke R. Thyroid cancer in patients with hyperthyroidism. Horm Metab Res. 2012;44:255–262. doi: 10.1055/s-0031-1299741. [DOI] [PubMed] [Google Scholar]
- 14.Hales IB, McElduff A, Crummer P, Clifton-Bligh P, Delbridge L, Hoschl R, et al. Does Graves’ disease or thyrotoxicosis affect the prognosis of thyroid cancer. J Clin Endocrinol Metab. 2013;75:886–889. doi: 10.1210/jcem.75.3.1517381. [DOI] [PubMed] [Google Scholar]
- 15.Kikuchi S, Noguchi S, Yamashita H, Uchino S, Kawamoto H. Prognosis of small thyroid cancer in patients with Graves’ disease. Br J Surg. 2006;92:434–439. doi: 10.1002/bjs.5279. [DOI] [PubMed] [Google Scholar]