Abstract
Objective
The cortisol awakening response (CAR) is a natural metabolic response that can be potentiated by negative cognitive-emotional processes, including stress appraisals, negative affect, and rumination. Psychological distress and the CAR are not consistently related, however. Individual differences in aspects of dispositional mindfulness which reflect how people relate to negative thoughts and emotions may help explain such inconsistencies. We tested whether the tendency to 1) label and describe inner experiences and 2) accept negative thoughts and feelings without judgment moderated the association between psychological distress and the CAR.
Methods
Self-reported dispositional mindfulness, perceived stress, anxiety, negative affect, and rumination, and the CAR were assessed among overweight/obese women. Regression analyses were conducted to examine whether dispositional mindfulness moderated the relationship between indicators of psychological distress and the CAR.
Results
While psychological distress was consistently positively related to the CAR, these associations were qualified by significant interactions with both components of dispositional mindfulness. Psychological distress was associated with the CAR at lower levels of dispositional mindfulness but not at higher levels.
Conclusion
These findings support the idea that the tendency to describe and accept distressing experiences may buffer the impact of psychological distress on physiological arousal. These metacognitive processes may be important moderators in unraveling the complex relationship between psychological distress and physiological stress reactivity. Further research is recommended to replicate this approach in other populations.
Keywords: Dispositional Mindfulness, Meditation, Cortisol, Cortisol Awakening Response, Perceived Stress, Negative Affect, Rumination, Acceptance
The cortisol awakening response (CAR) is a naturalistic indicator of hypothalamic-pituitary-adrenal (HPA) axis activation. Cortisol concentrations are low at night and rise in the early morning hours. The CAR is the increase or total amount of cortisol concentrations up to 45 minutes after awakening. The CAR has a slope steeper than the circadian rise of cortisol concentrations in the early morning hours suggesting that the CAR reflects psychophysiological processes unique to awakening (Wilhelm et al., 2007). Core identity and personality representations as well as anticipation of daily events are thought to become conscious upon awakening triggering HPA activation.
According to a meta-analysis, higher CARs are associated with increased appraisals of general life and job stress (Chida & Steptoe, 2009). However, negative affect, anxiety, and rumination are not reliably associated with the CAR (Chida & Steptoe, 2009; Zoccola &Dickerson, 2012). A lack of consistency across studies could be due to methodological issues, yet dispositional factors may moderate the relationship between psychological distress and the CAR and account for some of the observed inconsistencies.
Dispositional mindfulness is one potential factor that may moderate the association between psychological distress and the CAR. Dispositional mindfulness is the natural tendency to be aware of present-moment experiences in an accepting and nonjudgmental manner (Baer et al., 2004). The process of attending to internal experiences with mindful awareness entails a shift in relation to those experiences. Rather than identifying with thoughts and emotions as accurate reflections of “me” or “reality”, thoughts and emotions are experienced as passing mental events - which may or may not be valid - occurring in a larger field of awareness (Teasdale et al., 2002). This shift in perspective is thought to prevent escalation of dysfunctional cognitive and emotional patterns and allow for the occurrence of more adaptive responses. Therefore, mindfulness may promote well-being not just by changing the content of thought, such as reducing the frequency of negative thoughts or emotions, but also by shifting the relationship to negative thoughts and feelings themselves.
Dispositional mindfulness is associated with less psychological distress (Brown, Ryan, &Creswell, 2007) and reduced HPA reactivity to a standardized laboratory stressor (Brown, Weinstein, & Creswell, 2012). Additionally, a mindfulness intervention reduced the CAR compared to a waitlist control condition in a subgroup of obese women (Daubenmier et al., 2011).
Here we examine whether components of dispositional mindfulness moderate the association between psychological distress and HPA activity. One component involves the ability to label or describe experiences (Baer, 2004). The process of mentally or verbally labeling internal experiences may reduce identification with negative states. A second component involves accepting unwanted thoughts and feelings without judging them or oneself as good/bad or right/wrong. Individuals who tend to label or refrain from judging initial negative thoughts and emotions may have reduced emotional reactivity. In turn, such individuals may show attenuated activation of or quicker recovery from physiological stress responses. Therefore, how individuals relate to distressing thoughts and emotions may impact the duration or intensity of physiological stress reactivity.
In support of this theory, components of dispositional mindfulness have been shown to moderate the association between psychological risk factors and mental health outcomes. For example, neuroticism predicts depressive symptoms six years later among individuals with lesser tendency to label experiences but not among those with greater tendency, suggesting that the ability to describe inner experiences may protect against long-term negative effects of neuroticism (Barnhofer et al., 2011). However, to our knowledge, no studies have investigated whether dispositional mindfulness moderates the relationship between psychological distress and indicators of physiological arousal, such as the CAR. In the current study, we predicted that (1) indicators of psychological distress, including perceived stress, negative affect, anxiety, and rumination would be positively related to the CAR, and that (2) mindfulness would be negatively related to the CAR, but also that (3) components of dispositional mindfulness, including the tendencies to describe inner experiences and accept them without judgment, would moderate the relationship between distress and the CAR. Specifically, we hypothesized positive relations between distress and the CAR at lower but not higher levels of dispositional mindfulness, as higher levels would presumably buffer the impact of psychological distress on the CAR.
Methods
Participants
This study was comprised of 43 of 47 women enrolled in a mindfulness-based intervention at the University of California, San Francisco (UCSF) who had complete data on measures used in the present study (for more detailed description of the parent study see Daubenmier et al., 2011). All measures were collected at baseline prior to randomization. Pre-menopausal overweight and obese women with no history of diabetes, cardiovascular disease, or active endocrine disorder, not taking steroid medications, and had no prior meditation or yoga practice were eligible. Potential participants visited the lab for two baseline assessment sessions and responded to an online questionnaire battery before being enrolled into a mindfulness intervention. All participants were compensated for their participation. The study was approved by the UCSF Institutional Review Board and all participants provided informed consent.
Measures
Self-Report Measures
Two components of dispositional mindfulness that reflect how individuals relate to thoughts and emotions were assessed using the Kentucky Inventory of Mindfulness Skills (Baer et al., 2004): Describe—the ability to express one’s experience verbally and Accept—the ability to accept one’s experience without judgment were rated on a 5-point scale ranging from 1 (never or very rarely true) to 5 (almost always or always true). General feelings of anxiety were assessed with the Spielberger State-Trait Anxiety Inventory (Spielberger, 1983). Participants rated statements on a 4-point scale which ranged from 1 (almost never) to 4 (almost always). The Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983) was used to assess perception of stress over the past month on a 5-point scale ranging from 0 (never) to 4 (very often). The Rumination and Reflection Questionnaire (Trapnell & Campbell, 1999) assessed rumination along a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Negative Affect was assessed with the Positive and Negative Affect Scale (Watson, Clark, & Tellegen, 1988) along a 5-point scale ranging from 1 (very slightly or not at all) to 5 (extremely).
Salivary cortisol
Participants collected saliva samples at home across 4 days at awakening and 30 minutes post-awakening (more details provided in Daubenmier et al., 2011). Participants were instructed to wake according to their regular schedule and collect the first morning sample in bed prior to eating, drinking or brushing teeth. Saliva was collected into 2mL SaliCaps tubes (IBL Hamburg, Germany) using the passive drool method. Participants were asked to record the time at which they took the samples. In 95% of cases across the four days of saliva collection (138 out of 145 samples), participants reported taking the second morning sample within ± 5 minutes of the 30 minute guideline. Cortisol analysis was performed at Dresden Lab Service, overseen by Dr. Clemens Kirschbaum, at the Dresden University of Technology (Germany) using a commercial chemiluminescence immunoassay (CLIA, IBL, Hamburg, Germany). Intra and inter-assay coefficients of variation were below 9%. The CAR was calculated by subtracting the 30-minute post-waking value from the morning value. Values were averaged across days and participants with at least one full day of sampling were included in analyses.
Statistical Analyses
Separate regression analyses were used to test whether aspects of dispositional mindfulness moderated the relation between indicators of distress and the CAR. On Step 1 of the model, one of four measures of psychological distress was entered (perceived stress, anxiety, negative affect, or rumination). On Step 2, one component of dispositional mindfulness (Describe, Accept) and one distress factor were regressed simultaneously onto the CAR. One Step 3, the corresponding interaction term was entered to test for moderation (e.g., Accept × Anxiety). Eight models were computed in total reflecting the eight possible interactions between the four psychological distress and two dispositional mindfulness variables. Additional follow-up analyses were conducted in the case of a significant interaction to assess associations between psychological distress factors and the CAR at low and high levels of dispositional mindfulness (i.e., 1 SD below and above the mean, respectively). Specifically, the coefficient for a psychological distress variable (e.g, Anxiety) at a particular value of dispositional mindfulness (e.g., Accept) is a linear combination of the coefficients for the psychological distress variable and the interaction term. Using the /LMATRIX subcommand of SPSS GLM, we tested whether this combination of parameter estimates was significantly different from 0. A significant difference would indicate that the relationship between psychological distress and the CAR was significant at a specific level of dispositional mindfulness. Variables were centered to avoid multi-collinearity in the models. SPSS version 21 was used to compute analyses.
Results
Descriptive Results and Correlations
The sample was predominantly White (61.7%), but also included Hispanic/Latino and Asian/Pacific Islander participants (14.9% each), with 8.6% endorsing “other” for ethnicity. Other sample characteristics are presented in Table 1 along with scale and cortisol means and standard deviations. As predicted, the CAR was negatively related to Describe (r = -.39, p = .009) and Accept (r = -.37, p = .01). Describe and Accept were moderately correlated (r = .37, p = .01).
Table 1.
Means and Standard Deviations of Variables Across Entire Sample (n=43)
| Variable | Mean | Standard Deviation |
|---|---|---|
| Perceived Stress | 18.6 | 5.8 |
| Rumination | 3.73 | 0.7 |
| Negative Affect | 2.18 | 0.6 |
| Anxiety | 43.0 | 8.7 |
| Accept – KIMS | 3.14 | 0.8 |
| Describe – KIMS | 3.38 | 0.7 |
| Morning Cortisol (nmol/L) | 17.6 | 6.3 |
| Cortisol 30 min After Waking (nmol/L) | 24.7 | 8.9 |
| Cortisol Awakening Response (nmol/L) | 7.0 | 7.8 |
Regression Models Predicting Cortisol Awakening Response
Of the eight interaction models, four were statistically significant, two were of marginal significance, and two were non-significant (see Table 2). Specifically, in regards to the four models including Accept, the two interactions including negative affect and anxiety were statistically significant and those including perceived stress and rumination were of marginal significance (ps = .08 and .09, respectively). The pattern of interaction was similar across models such that the association between psychological distress and the CAR was positively related at lower levels of Accept (1 SD below the mean) but not at higher levels (1 SD above the mean; see Figure 1). For example, a significant interaction between Accept and negative affect was observed such that a 1-SD increase in negative affect was associated with a 4.15 nmol/L increase in the CAR when Accept was low (p = .003), but no significant association with the CAR was observed when Accept was high (p = .92).
Table 2.
Results of Regression Models Testing Interactions Between Components of Dispositional Mindfulness and Psychological Distress on the Cortisol Awakening Response.
| Cortisol Awakening Response | ||||||
|---|---|---|---|---|---|---|
| Predictor | Adj R2 | Unst B | SE | Beta | P value | |
| Model 1 | ||||||
| Step 1 | Anxiety | .10 | .31 | .13 | .35 | .02 |
| Step 2 | Anxiety | .15 | .19 | .14 | .22 | .18 |
| Describe | -3.25 | 1.76 | -.30 | .072 | ||
| Step3 | Anxiety | .23 | .08 | .15 | .09 | .57 |
| Describe | -3.19 | 1.68 | -.29 | .065 | ||
| Anxiety × Describe | -.39 | .17 | -.33 | .031 | ||
| Model 2 | ||||||
| Step 1 | Perceived Stress | .17 | .59 | .19 | .44 | .003 |
| Step 2 | Perceived Stress | .26 | .50 | .18 | .38 | .008 |
| Describe | -3.54 | 1.49 | -.32 | .023 | ||
| Step 3 | Perceived Stress | .25 | .47 | .19 | .35 | .015 |
| Describe | -3.38 | 1.50 | -.31 | .031 | ||
| Perceived Stress × Describe | -0.23 | 0.24 | -.13 | .36 | ||
| Model 3 | ||||||
| Step 1 | Rumination | .16 | 4.46 | 1.50 | .42 | .005 |
| Step 2 | Rumination | .27 | 4.12 | 1.40 | .39 | .005 |
| Describe | -3.95 | 1.50 | -.36 | .010 | ||
| Step 3 | Rumination | .43 | 5.13 | 1.28 | .48 | .000 |
| Describe | -3.47 | 1.30 | -.32 | .011 | ||
| Rumination × Describe | -6.52 | 1.88 | -.42 | .001 | ||
| Model 4 | ||||||
| Step 1 | Negative Affect | .10 | 4.79 | 2.00 | .35 | .02 |
| Step 2 | Negative Affect | .24 | 4.67 | 1.84 | .34 | .015 |
| Describe | -4.25 | 1.49 | -.39 | .007 | ||
| Step 3 | Negative Affect | .25 | 3.73 | 1.98 | .27 | .07 |
| Describe | -4.17 | 1.48 | -.38 | .007 | ||
| Negative Affect × Describe | -3.09 | 2.51 | -.18 | .23 | ||
| Model 5 | ||||||
| Step 1 | Anxiety | .10 | 0.31 | 0.13 | .35 | .02 |
| Step 2 | Anxiety | .14 | .20 | .14 | .23 | .16 |
| Accept | -2.74 | 1.6 | -.27 | .10 | ||
| Step 3 | Anxiety | .32 | 1.0 | .13 | .11 | .47 |
| Accept | -4.36 | 1.5 | -.43 | .007 | ||
| Anxiety × Accept | -.49 | 0.15 | -.46 | .002 | ||
| Model 6 | ||||||
| Step 1 | Perceived Stress | .17 | .59 | .19 | .44 | .003 |
| Step 2 | Perceived Stress | .23 | .49 | .19 | .37 | .013 |
| Accept | -2.81 | 1.43 | -.28 | .057 | ||
| Step 3 | Perceived Stress | .27 | .45 | .18 | .34 | .018 |
| Accept | -3.79 | 1.5 | -.37 | .016 | ||
| Perceived Stress × Accept | -.34 | 0.19 | -.26 | .08 | ||
| Model 7 | ||||||
| Step1 | Rumination | .16 | 4.46 | 1.50 | .42 | .005 |
| Step 2 | Rumination | .18 | 3.3 | 1.68 | .32 | .053 |
| Accept | -2.28 | 1.62 | -.22 | .17 | ||
| Step 3 | Rumination | .22 | 5.26 | 1.98 | .50 | .012 |
| Accept | -1.75 | 1.61 | -.17 | .283 | ||
| Rumination × Accept | -3.11 | 1.81 | -.29 | .094 | ||
| Model 8 | ||||||
| Step 1 | Negative Affect | .10 | 4.79 | 2.00 | .35 | .02 |
| Step 2 | Negative Affect | .20 | 4.32 | 1.90 | .32 | .028 |
| Accept | -3.47 | 1.42 | -.34 | .019 | ||
| Step 3 | Negative Affect | .26 | 3.32 | 1.88 | .24 | .086 |
| Accept | -4.13 | 1.40 | -.41 | .005 | ||
| Negative Affect × Accept | -4.48 | 2.13 | -.29 | .042 | ||
Figure 1.
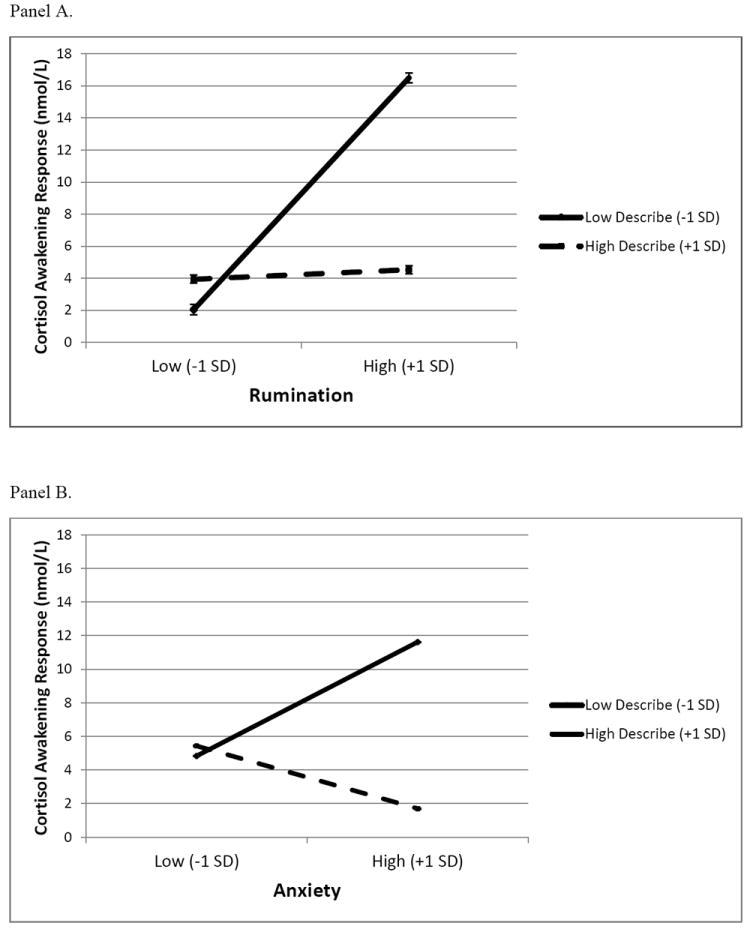
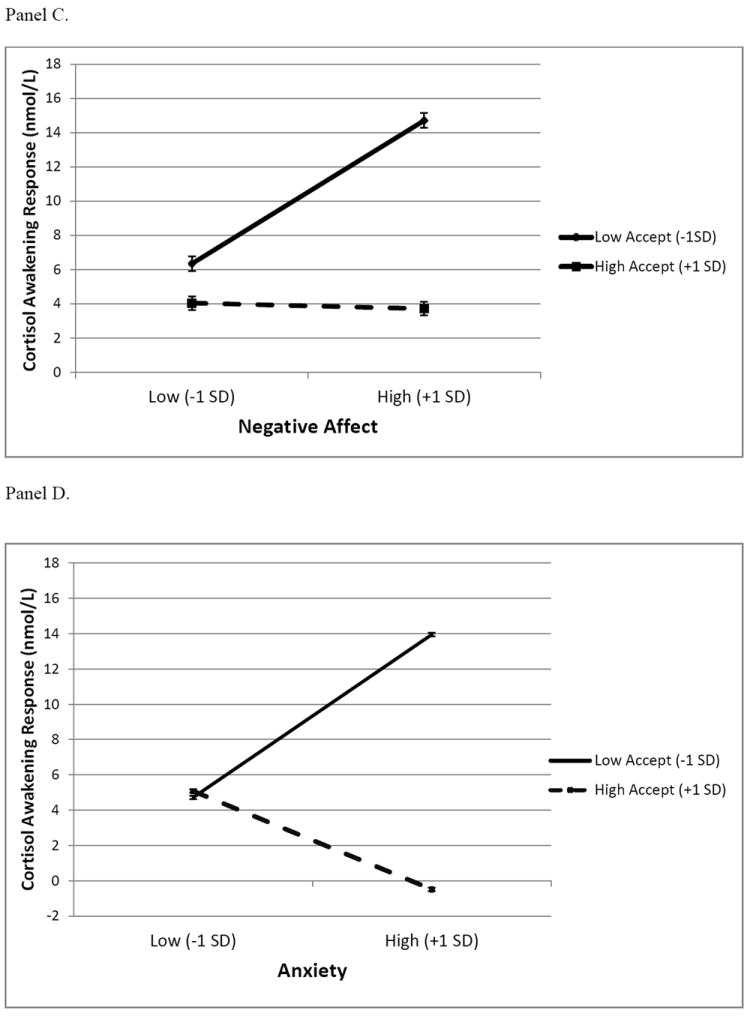
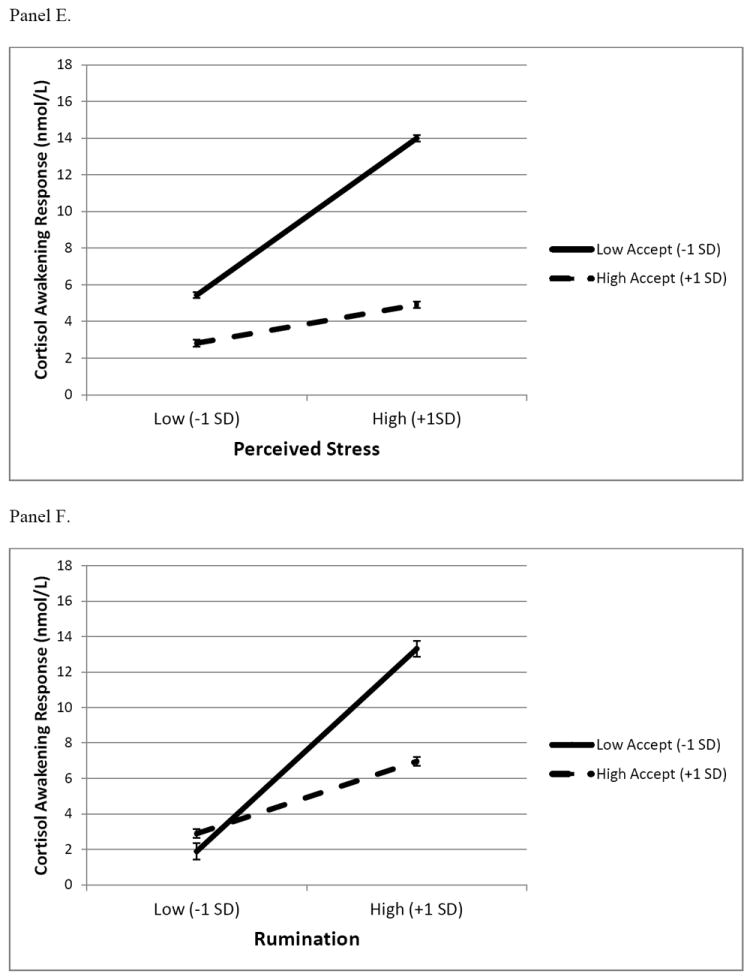
Interactions between aspects of psychological distress and components of dispositional mindfulness predicting the cortisol awakening response. For Panels A-D, the interaction terms are significant indicating that psychological distress is related to the cortisol awakening response at low levels of dispositional mindfulness (i.e., 1 SD below the mean) but not at higher levels (i.e., 1 SD above the mean). Interactions represented in Panels E and F are of marginal significance (p < .10). Panel A: Rumination is positively related to the CAR at low levels of Describe (p < .0001) but not at high levels (p = .81). Panel B: Anxiety is positively related to the CAR at low levels of Describe (p = .025) but not at high levels (p = .38). Panel C: Negative Affect is positively related to the cortisol awakening response (CAR) at low levels of Accept (p = .003) but not at high levels (p = .91). Panel D: Anxiety is positively related to the CAR at low levels of Accept (p = .003) but not at high levels (p = .14). Panel E: Interaction between perceived stress and Accept (p = .08). Panel F: Interaction between rumination and Accept (p = .09).
Note: Graphs of non-centered variables are presented for ease of interpretation. Error bars represent ± 1 standard error of the estimate.
The models testing the interaction of Describe with rumination and anxiety were significant, showing a similar pattern to those including Accept (see Figure 1). However, the two remaining interactions of Describe with perceived stress and negative affect were not significant. Collectively, these results provide convergent evidence that dispositional mindfulness, particularly the acceptance component, moderates the association between psychological distress and the CAR.
Discussion
To our knowledge, this is the first study to report that aspects of dispositional mindfulness – the tendency to describe and accept thoughts and emotions – are negatively related to the CAR. As expected, psychological distress was positively associated with the CAR as found in prior studies. However, these associations were qualified by interactions with components of dispositional mindfulness, which explained significant proportions of variance in the CAR (13-27%) beyond indicators of psychological distress alone. Anxiety, negative affect, and rumination were positively related to the CAR at lower levels of dispositional mindfulness but not at higher levels. These findings suggest that the reported tendency to consciously label or accept negative thoughts and emotions may buffer their impact on HPA axis activation. Put another way, strong identification with or judgment of negative thoughts and emotions may increase or prolong HPA axis activation but not if those thoughts and emotions are experienced with mindful awareness.
Neuroimaging findings suggest “top down” and “bottom up” pathways reflecting the labeling and acceptance aspects of mindfulness, respectively, by which dispositional mindfulness may attentuate HPA axis activity. First, the process of labeling negative affective stimuli increases prefrontal activation and reduces amygdala activation (Hariri, Bookheimer, and Mazziotta, 2000; Lieberman et al, 2007) and this response is enhanced among individuals higher in dispositional mindfulness (Creswell et al., 2007). Rather than a passive response, the mental process of labeling negative thoughts or emotions - without changing their content - may activate prefrontal cortical regions and thereby attenuate limbic regions and downstream HPA activation. Secondly, other research suggests that the acceptance component of mindfulness involves deactivation of the medial pre-frontal cortex in response to negative affective stimuli, suggesting reduced rumination about emotional states (Kross et al, 2009; Taylor et al, 2011). Although mindful awareness of emotions led to reduced subjective emotional intensity among experienced meditators in this study, initial amydala activity was not reduced, suggesting that acceptance may involve a full experience but quicker dissipation of the emotion (Taylor et al, 2011). In support, higher dispositional mindfulness is related to reduced resting state amygdala activity (Way, Creswell, Eisenberger, & Lieberman, 2010), and smaller right amygdala volumes (Taren, Creswell, & Gianaros, 2013), potential mechanisms for reduced HPA reactivity. Hence, the present research is consistent with previous studies implicating both top-down prefrontal regulatory processes in labeling and reduced bottom-up central stress reactivity during acceptance in mindful individuals (Creswell, 2014).
The potential buffering effect of mindfulnes on the CAR did not clearly generalize to stress appraisals, although the interaction with acceptance was marginally sigificant. Interestingly, perceived stress was the only psychological distress variable consistently related to the CAR in a meta-analysis (Chido and Steptoe, 2009). Stress appraisals may more closely reflect the presence of objective stressors. Accordingly, labeling and accepting internal experiences may do less to buffer the impact of negative thoughts and feelings on physiological responses in the presence of objective stressors, as HPA reactivity to objective stressors may be adaptive. Mindful awareness of internal experiences may more likely reduce HPA reactivity when situations are ambiguous, trait levels of negative affect or rumination are high, or during recovery from stressors. Of note, these findings were observed in non-meditators, suggesting natural variations in trait aspects of mindfulness may be protective of physical health.
The sample included highly-stressed overweight and obese women (based on a comparison of perceived stress scores to the national average, reported in Daubenmier et al, 2011) and was prodiminately White, although approximately 40% of the sample identified as non-White. It will be important to test the generalizability of these findings and establish whether they replicate in other populations, including men and among individuals with training in mindfulness meditation. Of note, these effects may be most observable in highly stressed populations, according to the stress-buffering hypothesis of mindfulness (Creswell, 2014). In addition, it is important to note the cultural context of this study. Recent research suggests cultural variation in acceptance of negative emotions, with individuals from Asian cultures tending to accept negative emotions as a part of life and individuals from Western cultures tending to view negative emotions as unacceptable and to be avoided (Miyamoto et al, 2013). This cultural variation is thought to account for the positive association of negative emotions with elevated levels of a pro-inflammatory cytokine (interleukin-6) among individuals in the United States but not in Japan (Miyamoto et al, 2013). In the current study, we found that a lack of acceptance of negative emotions is associated with physiological stress arousal and that psychological distress is associated with physiological arousal among those with low but not high levels of acceptance in the United States, yet future work could test the generalizability of these findings among members of Asian cultures or by comparing how such associations may differ on a cultural level.
In terms of methodological improvements, future research could validate time of saliva collection using hidden time-stamped devices. Finally, these results are cross-sectional and we cannot be sure of the causal direction of the relation among variables or whether genetic predispositions or environmental exposures account for the relations.
In summary, inconsistent findings in the literature on psychological distress and the CAR may be due to variations across samples in moderating variables that reflect how individuals relate to distressing thoughts and emotions. If individuals are able to label distressing internal experiences or not judge themselves for having them (presumably decreasing identification with them) the impact of those experiences on HPA stress arousal may be attenuated. Further consideration of components of dispositional mindfulness as moderating variables may show for whom and in what circumstances negative psychological factors affect the CAR and other stress reactivity measures.
Acknowledgments
We are grateful to the dedicated study participants, volunteers and staff who made this research possible. We would also like to thank two anonymous reviewers and J. David Creswell, PhD for commenting on an earlier draft of this manuscript.
Role of funding source
This research was supported by the Mt Zion Health Fund; The William Bowes, Jr., Fund; the Robert Deidrick Fund; and NIH grant K01AT004199 awarded to JD from the National Center For Complementary & Alternative Medicine and the National Institutes of Health/National Center for Research Resources UCSF-CTSI Grant no. ULI RR024131. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Complementary & Alternative Medicine or the National Institutes of Health.
Footnotes
Contributors
Author EE and JD designed the study and wrote the protocol. Authors JD and DH managed the literature searches. Authors JD, EE and VC established the methodology; Author JD completed the statistical analysis. Author DH wrote the first draft of the manuscript. Authors JD, VC, DH and EE reviewed and edited the manuscript. Author JD wrote the final draft of the manuscript. All authors significantly contributed to and have approved the final manuscript.
Conflict of Interest
The authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment. 2004;11:191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- Barnhofer T, Duggan DS, Griffith JW. Dispositional mindfulness moderates the relation between neuroticism and depressive symptoms. Personality and Individual Differences. 2011;51:958–962. doi: 10.1016/j.paid.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18:211–237. [Google Scholar]
- Brown KW, Weinstein N, Creswell JD. Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology. 2012;37:2037–2041. doi: 10.1016/j.psyneuen.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Goodman RJ, Inzlicht M. Dispositional mindfulness and the attenuation of neural responses to emotional stimuli. Social Cognitive and Affective Neuroscience. 2013;8:93–99. doi: 10.1093/scan/nss004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: A systemic review and meta-analysis. Biologocal Psychology. 2009;80:265–278. doi: 10.1016/j.biopsycho.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:386–396. [PubMed] [Google Scholar]
- Creswell JD. Biological pathways linking mindfulness with health. In: Brown KW, Creswell JD, Ryan R, editors. Handbook on Mindfulness Science. Guilford Publications; New York, NY: in press. [Google Scholar]
- Creswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosomatic Medicine. 2007;69:560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Daubenmier J, Kristeller J, Hecht FM, Maninger N, Kuwata M, Jhaveri K, Epel E, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: An exploratory randomized controlled study. Journal of Obesity. 2011;2011:1–13. doi: 10.1155/2011/651936. Article ID 651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariri AR, Bookheimer SY, Mazziotta JC. Modulating emotional responses: effects of a neocortical network on the limbic system. Neuroreport. 2000;11:43–8. doi: 10.1097/00001756-200001170-00009. [DOI] [PubMed] [Google Scholar]
- Kross E, Davidson M, Weber J, Ochsner K. Coping with emotions past: the neural bases of regulating affect associated with negative autobiographical memories. Biological Psychiatry. 2009;65:361–6. doi: 10.1016/j.biopsych.2008.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman MD, Eisenberger NI, Crockett MJ, Tom SM, Pfeifer JH, Way BM. Putting Feelings Into Words: Affect Labeling Disrupts Amygdala Activity in Response to Affective Stimuli. Psychological Science. 2007;18:421–8. doi: 10.1111/j.1467-9280.2007.01916.x. [DOI] [PubMed] [Google Scholar]
- Miyamoto Y, Boylan JM, Coe CL, Curhan KB, Levine CS, Markus HR, Park J, Kitayama S, Kawakami N, Karasawa M, Love GD, Ryff CD. Negative emotions predict elevated interleukin-6 in the United States but not in Japan. Brain Behavior and Immunity. 2013;34:79–85. doi: 10.1016/j.bbi.2013.07.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the state-trait anxiety inventory: STAI. Palo Alto, CA: Consulting Psychologist Press; 1983. [Google Scholar]
- Taren AA, Creswell JD, Gianaros PJ. Dispositional Mindfulness Co-Varies with Smaller Amygdala and Caudate Volumes in Community Adults. PLoS ONE. 2013;8(5):e64574. doi: 10.1371/journal.pone.0064574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VA, Grant J, Daneault V, Scavone G, Breton E, Roffe-Vidal S, Beauregard M, et al. Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. NeuroImage. 2011;57(4):1524–1533. doi: 10.1016/j.neuroimage.2011.06.001. http://dx.doi.org/10.1016/j.neuroimage.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive Awareness and Prevention of Relapse in Depression: Empirical Evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: Distinguishing rumination from reflection. Journal of Personality and Social Psychology. 1999;76:284–304. doi: 10.1037//0022-3514.76.2.284. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and neagtive affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:11063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Way BM, Creswell JD, Eisenberger NI, Lieberman MD. Dispositional mindfulness and depressive symptomatology: correlations with limbic and self-referential neural activity during rest. Emotion. 2010;10(1):12–24. doi: 10.1037/a0018312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm I, Born J, Kudielka BM, Schlotz W, Wust S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007;32(4):358–366. doi: 10.1016/j.psyneuen.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Zoccola PM, Dickerson SS. Assessing the relationship between rumination and cortisol: A review. Journal of Psychosomatic Research. 2012;10(1):1–9. doi: 10.1016/j.jpsychores.2012.03.007. [DOI] [PubMed] [Google Scholar]


