Abstract
Objective:
The aim of this cross-sectional study was to compare craniofacial growth among operated and unoperated unilateral cleft lip and palate non-syndromic subjects.
Materials and Methods:
A sample of 180 subjects of Indian origin was selected. Of them, 90 were operated, and 90 were unoperated complete unilateral cleft lip and palate individuals. The subjects were divided into three age groups of 3–5, 8–10, and 20–25 years comprised of 30 patients in each group. The following measurements were evaluated: Angle and length of the cranial base; maxillary spatial positioning and length; mandibular spatial positioning; morphology and length; maxillomandibular relationship. Comparative analysis of the means between the groups was performed with Student's t-test at the significance levels of 5%. The ANOVA test has been performed to test the effect of time.
Results:
No significant differences were observed between the measurements that represented the angle and length of the cranial base of unoperated and the operated patients (P>0.05). There was statistically significant decrease (P˂0.05) in the maxillary length (Co-A; 69.00 mm in 3–5 years, 68.33 mm in 8–10 years, and 67.17 mm in 20–25 years age group), and SNA angle (74.83° in 3–5 years, 74.17 ° in 8–10 years and 73.17 ° in 20–25 years age group) in operated group. No significant difference noticed on cephalometric values of the mandible, except Ar-Go-Me angle (P˂0.05), which showed vertical growth pattern in unoperated patients (132.50 ° in 3–5 years, 132.00 ° I 8–10 years and 138.33 ° in 20–25 years age group).
Conclusion:
Lip and palate repair has a significant influence on the maxilla and resulting in retarded growth of maxilla, which causes midface deficiency beyond acceptable sagittal limits. The Gonial angle showed vertical growth pattern in unoperated patients, but the cranial base angle and length of unoperated and the operated patients were similar.
Keywords: Cephalometry, craniofacial growth, maxillomandibular, unilateral cleft lip and palate
INTRODUCTION
Orofacial clefts, and in particular cleft lip and palate, are major human birth defects with complex etiology.[1] The cleft face has been studied extensively. However, the results reported in literature vary and sometimes are in disagreement. The reason for differences includes different treatment procedures for the same cleft types, functional changes resulting from the cleft, and inherited growth patterns.[2,3,4]
There has always been a keen interest in evaluating the effects of surgery on the growth of the craniofacial complex of cleft lip and/or palate patients. Many attempts have been made which have enlightened one aspect or another of this complex problem. From the time cephalometrics have been successfully used to evaluate craniofacial growth on both normal and cleft individuals, different investigators either totally or partially agreed, or on the other hand, disagreed completely among themselves about the effects of clefts and/or surgery on facial growth.[5,6,7,8,9,10,11]
Hence, this study was designed to evaluate the effects of cleft lip palate repair on craniofacial growth in patients with complete unilateral cleft lip and palate.
MATERIALS AND METHODS
This study evaluated lateral cephalograms of 180 patients of Indian origin from Karnataka state who had complete unilateral cleft lip and palate. Only non-syndromic patients were included in the study. Sampling was done by purposive sampling method. The patients were divided into two groups (A) unoperated and (B) operated, each group was further divided into three subgroups comprising of 30 patients.
According to age as follows:
Subgroups A1 and B1: 3–5 years
Subgroups A2 and B2: 8–10 years and
Subgroups A3 and B3: 20–25 years.
In operated group, lip closure was done by Millard's cleft lip repair and palate closure was performed by Bardach two-flap palatoplasty.
Lateral cephalograms were obtained using a fixed subject to X-ray distance of 5 feet. The head was oriented with the Frankfort horizontal plane parallel to the floor, with teeth in centric occlusion and lips relaxed. The machine was calibrated for 8% magnification, and this magnification was not corrected in our measurements. Soft tissue and bony structure were traced on polyester film, and mean shadow of bilateral structures were traced to minimize errors in positioning or skeletal or dental asymmetries.
Following landmarks were identified on each cephalogram [Figure 1]:
Figure 1.
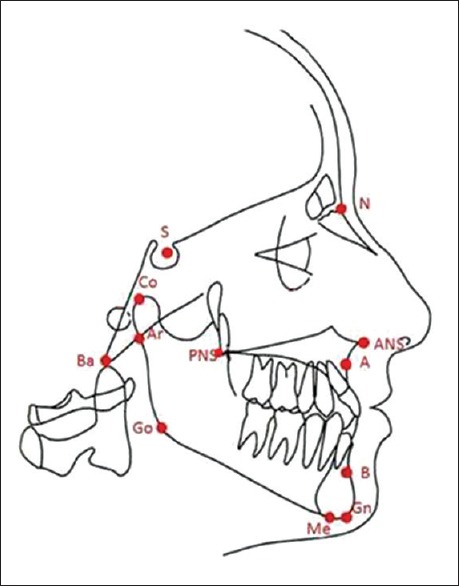
Landmarks
Sella (S), Nasion (N), Basion (Ba), point A (subspinale), anterior nasal spine (ANS), posterior nasal spine (PNS), Condylion (Cd), point B (supramentale), Articulare (Ar), Gonion (Go), Menton (Me), Gnathion (Gn).
The cephalometric measurements were carried out manually and following variables were evaluated [Figures 2 and 3]:
Figure 2.
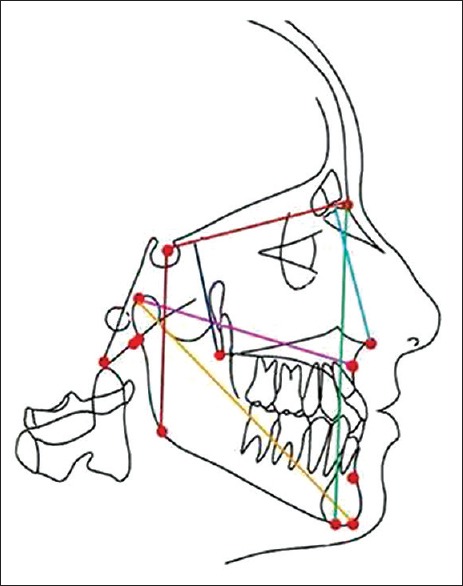
Linear measurements
Figure 3.
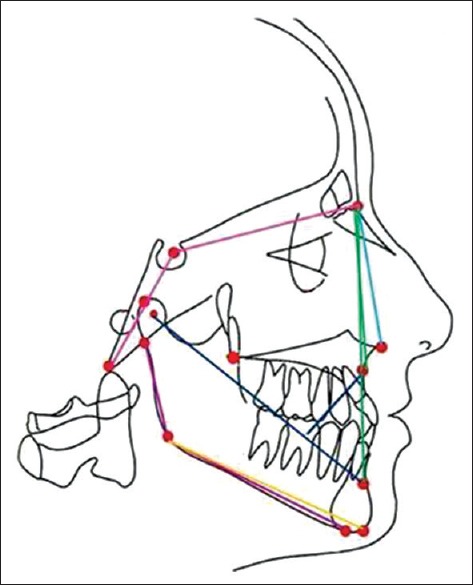
Angular measurements
Angle and length of the cranial base (Ba-S-N angle and S-N length).
Maxillary spatial positioning (SNA angle, SN-ANS angle, SN-PP angle, Co-A length).
Mandibular spatial positioning (SNB angle, Ar-Go-Me angle (Gonial angle), SN-GoGn angle, and Co-Gn length).
Maxillomandibular relationship (ANB angle, beta angle and wits appraisal).
The cephalometric values of both groups were compared; group A with group B of respective age group, to assess the difference in growth between operated and nonoperated groups and hence, the effect of the surgical procedure on growth.
Statistical Analysis
Mean and standard deviation was calculated for each cephalometric measurement obtained for unoperated and operated groups. Comparative analysis of the means between the groups was performed based on Student's t-test at the significance levels of 5%. ANOVA was performed to assess the effect of time on growth in both groups separately at the significance levels of 5%.
Intra-examiner repeatability and consistency (reliability) was tested using the Dahlberg's equation: s = √∑d2/2n, where d is the difference between two measurements and n the number of tested radiographs. Twenty lateral cephalograms were randomly selected, and each radiograph was traced twice. For the angular measurements, s ranged from 0.30° to 0.75° (mean 0.53°) and for the linear measurements, 0.12–0.65 mm (mean 0.39 mm).
All the data were analyzed statistically for means and standard deviations by using the SPSS Software for Windows (version 16.0, SPSS Inc., Chicago, IL, United States).
RESULTS
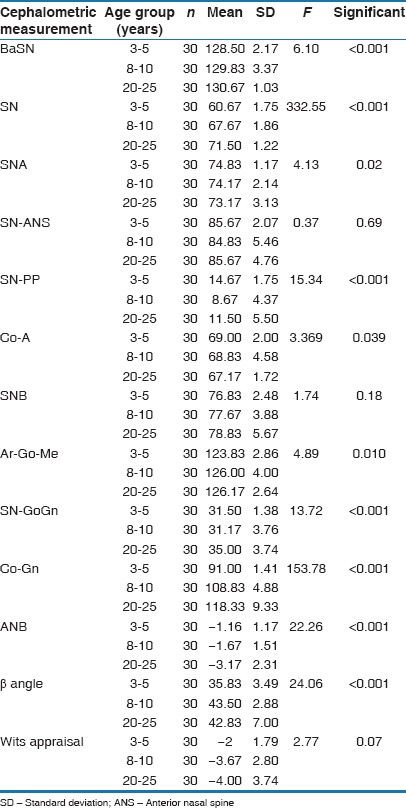
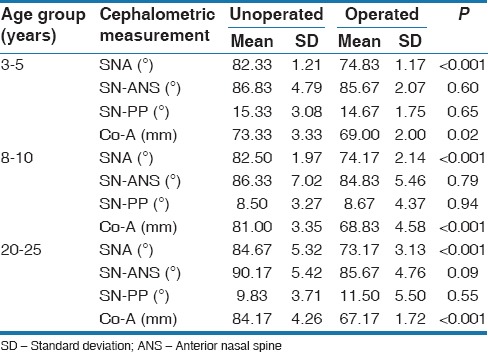
The mean values, standard deviations and Student's t-test of all the variables used in this study are shown in Tables 1-4. The effect of time on growth in both groups is shown in Tables 5 and 6.
Table 1.
Mean, SD, and t-test results for the cranial base cephalometric measurements
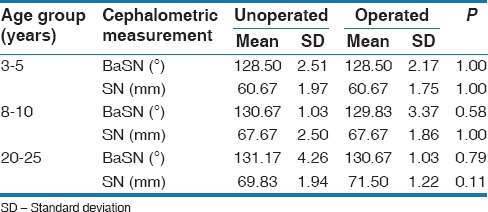
Table 4.
Mean, SD, and t-test results for the maxillomandibular cephalometric measurements
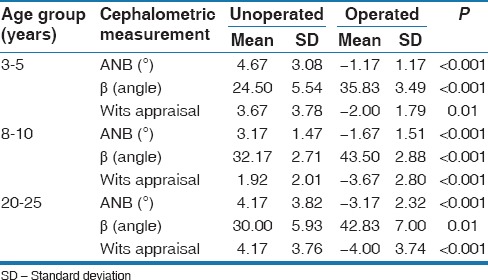
Table 5.
ANOVA test for unoperated group
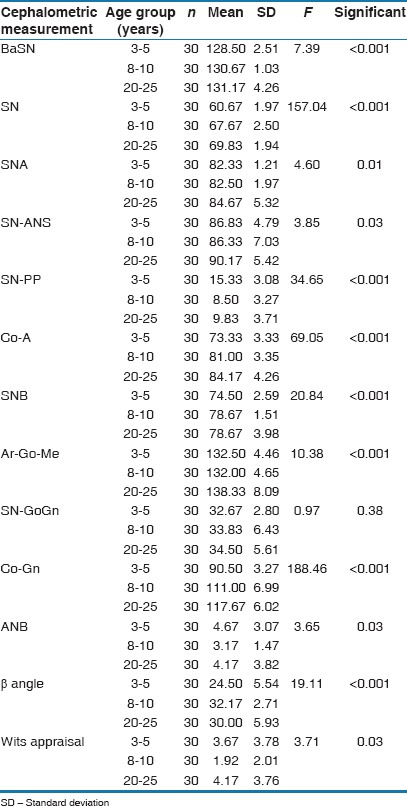
Table 6.
ANOVA test for operated group
The cranial base showed enough stability and remained uninfluenced by the surgical repair of cleft lip and palate, partly for being distant from the surgical area. This was noticed from the nonsignificant differences observed between the measurements that represented the angle and length of the cranial base of unoperated patients and the operated patients (p>0.05) [Table 1].
Premaxilla was retropositioned during growth because of lip and palate repair. Angle SNA and maxillary length (Co-A) showed lesser values and statistically significant differences (p<0.05), respectively on operated patients. However, the same statistical pattern was not observed for the SN-ANS angle, which represents the skeletal maxillary anterior projection. Statistically significant differences (p<0.05) noticed in angle SNA, at all age groups, which showed that the maxilla is retrognathic in operated group [Table 2].
Table 2.
Mean, SD, and t-test results for the maxillary cephalometric measurements
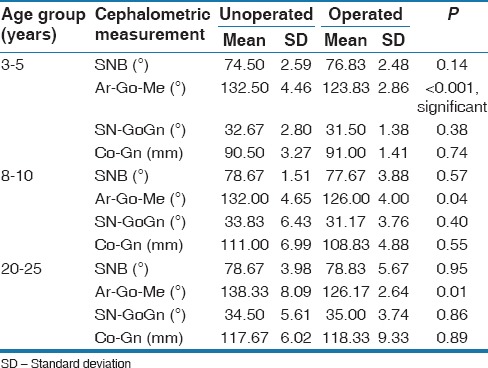
The cephalometric values referring to the mandible (SNB, SN-GoGn and Co-Gn) showed no alteration after lip-palate repair (p>0.05). The only statistically significant difference was found in Ar-Go-Me angle, which showed a more vertical growth pattern in unoperated patients as compared to operated patients (p<0.05) [Table 3].
Table 3.
Mean, SD, and t-test results for the mandibular cephalometric measurements
Facial convexity dramatically reduced in the operated patients when evaluated by angle ANB, Beta angle, and Wits appraisal, as a consequence of the premaxillary retro positioning induced by lip palate repair [Table 4].
The ANOVA test results showed statistically significant differences between mean scores of all the cephalometric values except Sn-GoGn in the unoperated group and SN-ANS and SNB in operated group [Tables 5 and 6].
DISCUSSION
Dentofacial problems in patients with cleft lip and palate can be divided into problems related to the cleft and the problems related to the sometimes iatrogenic treatment protocol. Researchers seem to agree with the idea that forces released by repairing surgeries on the maxilla prevail over genetic factors as for the determination of the final facial pattern in patients with cleft lip palate.[7,12,13,14,15]
The longitudinal analysis of cephalometric values for both groups of patients at different age groups with complete unilateral cleft lip and palate (unoperated vs. operated lip and palate during childhood) allowed for identification of the influence of lip palate repair, when performed during childhood on craniofacial morphology during growth.
In this cross-sectional study, no significant difference in the mean the cranial base angle and anterior cranial base length values was found in any of the operated and unoperated cleft group. Our results were in agreement with the results of previous studies,[5,16,17,18,19] but different from Bishara et al., whose study showed a reduction in cranial base angle.[2]
The cephalometric evaluation of maxilla showed that unoperated group maxilla showed normal growth in 3–5 years and 8–10 years of age groups, and protrusive pattern in 20–25 years age group. Whereas in the operated group, maxilla showed retarded growth in all the three sub-groups, as compared to unoperated group. This proved that lip palate surgery has restraining effect on the growth of maxilla. Our results were in agreement with the results of previous studies.[2,16,20]
No significant difference was found in SN-ANS angle (sella nasion to anterior nasal spine angle that represents basal part of premaxilla); our results were similar to the results of Da Silva Filho et al.[13] This showed that the restraining effect of the anterior maxillary growth due to the lip repair is selective and located within the alveolar bone. The basal part of the premaxilla (SN-ANS) was less influenced by lip repair than its alveolar part (both SNA and Co-A were decreased in the operated group). These (SNA and Co-A) decreased cephalometric values indicates that the muscular bridge created by surgery is able to influence the alveolar bone, but it has less influence in the sagittal growth of the premaxillary basal structure (SN-ANS). SN-PP angle was similar in both the groups.
In general, the values showed that the maxilla is near normal in the unoperated cleft lip palate group and retrusive in the operated group. The midfacial hypoplasia observed in the operated group may be the outcome of the surgical intervention. In surgically treated patients, inhibition of the normal development of the maxilla has been attributed to scar tissue.[4] There may be no damage to the bone itself because of surgery, but the fibrous scar tissue formed near the bony growth sites may prevent normal maxillary remodeling and development in a downward and forward direction. The extent of interference is directly related to the severity of the cleft because more extensive procedures have to be performed to mobilize tissue to close a large defect; resulted in large scar tissue and retarded growth of maxilla.
No significant difference was found in angles SNB, SN-GoGn and Co-Gn length. This showed that mandibular spatial position and length remained unaffected by surgical procedures. These findings are similar to the previous studies.[21,22]
Statistically significant difference was found in gonial angle [Table 3]. The gonial angle was larger in an unoperated group than the operated group. On comparing with normal individuals, the value of gonial angle recorded in the unoperated group is greater, and this angle did not seem to change with age. These findings are in agreement with studies conducted by Hayashi et al. and Fudalej et al.[21,22]
The data reveals that the mandible was of normal length, but the chin was posteriorly displaced. This retroposition of chin was essentially the result of mandibular rotation with subsequent remodeling of the muscle attachments in the gonial area (indicated by the increased gonial angle and mandibular inclination) and may have been a functional response to the altered maxillary complex. The normal mandible and tongue established a satisfactory relation with a small, shallow-vaulted, maxilla. The changes may also have been induced by mouth breathing, a common finding.[23]
Table 4 shows a significant difference in angle ANB between the groups. In operated group average value of angle SNA is less than normal whereas in unoperated group it is normal in birth to 3 years and 6–12 years age group and increased in 12–20 years age group by 2°. This shows negative value for ANB in the operated group, which indicates class III malocclusion. These findings are in agreement to previous studies.[5,15,24,25,26] Similarly statistically, significant differences were found in Wits appraisal and beta angle.
According to the results of this study, there were significant differences in all cephalometric values except (SN-GoGn) for the unoperated group showed growth at the cranial base, maxilla, and mandible. Nonsignificant changes in SN-GoGn showed that the mandibular plane does not change with growth [Table 5]. These findings are in agreement with previous studies.[2,5,16,19]
In the present study, we found statistically significant differences in all cephalometric values (except SN-ANS and SNB) for operated group, which showed growth at cranial base, maxilla and mandible [Table 6], but when both group compared we found the similar results to previous studies,[4,5,13,14] which showed less growth of maxilla in operated group [Table 2].
CONCLUSION
There is normal growth potential of the maxilla in the unoperated group. In the operated group, the maxilla is retrognathic, indicating that surgical repair of cleft lip and palate affects the growth of maxilla, whereas growth of mandible is similar in both the groups. The restraining effect of lip repair is selective and located within the alveolar bone. The basal part of premaxilla was less influenced by lip repair than its alveolar part.
Financial Support and Sponsorship
Nil.
Conflict of Interest
There are no conflict of interest.
REFERENCES
- 1.Saleem S, Rajendran R, Moinak B, Anna J, Pramod BJ. Evidence for transforming growth factor-beta 3 gene polymorphism in non-syndromic cleft lip and palate patients from Indian sub-continent. Med Oral Patol Oral Cir Bucal. 2012;17:e197–200. doi: 10.4317/medoral.17453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bishara SE, Krause CJ, Olin WH, Weston D, Ness JV, Felling C. Facial and dental relationships of individuals with unoperated clefts of the lip and/or palate. Cleft Palate J. 1976;13:238–52. [PubMed] [Google Scholar]
- 3.Chierici G, Harvold EP, Vargervik K. Morphogenetic experiments in cleft palate: Mandibular response. Cleft Palate J. 1973;10:51–61. [PubMed] [Google Scholar]
- 4.Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Part I. Treatment affecting growth. Cleft Palate J. 1987;24:5–23. [PubMed] [Google Scholar]
- 5.Bishara SE. Cephalometric evaluation of facial growth in operated and non-operated individuals with isolated clefts of the palate. Cleft Palate J. 1973;10:239–46. [PubMed] [Google Scholar]
- 6.Smahel Z, Betincová L, Müllerová Z, Skvarilová B. Facial growth and development in unilateral complete cleft lip and palate from palate surgery up to adulthood. J Craniofac Genet Dev Biol. 1993;13:57–71. [PubMed] [Google Scholar]
- 7.Liao YF, Mars M. Long-term effects of palate repair on craniofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2005;42:594–600. doi: 10.1597/04-077r.1. [DOI] [PubMed] [Google Scholar]
- 8.Bing S, Joseph EL. The impact of cleft lip and palate repair on maxillofacial growth. Int J Oral Sci. 2014;59:1–4. doi: 10.1038/ijos.2014.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richard B, Russell J, McMahon S, Pigott R. Results of randomized controlled trial of soft palate first versus hard palate first repair in unilateral complete cleft lip and palate. Cleft Palate Craniofac J. 2006;43:329–38. doi: 10.1597/05-065.1. [DOI] [PubMed] [Google Scholar]
- 10.Chate R, Di Biase D, Ball J. Singapore: Stamford Press, Academy of Medicine; 1997. A Comparison of the Dental Occlusions from a United Kingdom Sample of Complete Unilateral Cleft Lip and Palate Patients with those from the Eurocleft Study. Transactions of the 8th International Congress on Cleft Palate and Related Craniofacial Anomalies; pp. 371–6. [Google Scholar]
- 11.Shao Q, Chen Z, Yang Y, Chen Z. Effects of lip repair on maxillofacial morphology in patients with unilateral cleft lip with or without cleft palate. Cleft Palate Craniofac J. 2014;51:658–64. doi: 10.1597/12-316. [DOI] [PubMed] [Google Scholar]
- 12.Capelozza Filho L, Normando AD, da Silva Filho OG. Isolated influences of lip and palate surgery on facial growth: comparison of operated and unoperated male adults with UCLP. Cleft Palate Craniofac J. 1996;33:51–6. doi: 10.1597/1545-1569_1996_033_0051_iiolap_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 13.Da Silva Filho OG, Valladares Neto J, Capelloza Filho L, de Souza Freitas JA. Influence of lip repair on craniofacial morphology of patients with complete bilateral cleft lip and palate. Cleft Palate Craniofac J. 2003;40:144–53. doi: 10.1597/1545-1569_2003_040_0144_iolroc_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 14.Nagasao T, Miyamoto J, Konno E, Ogata H, Nakajima T, Isshiki Y. Dynamic analysis of the effects of upper lip pressure on the asymmetry of the facial skeleton in patients with unilateral complete cleft lip and palate. Cleft Palate Craniofac J. 2009;46:154–60. doi: 10.1597/07-177.1. [DOI] [PubMed] [Google Scholar]
- 15.Borzabadi-Farahani A, Lane CJ, Yen SL. Late maxillary protraction in patients with unilateral cleft lip and palate: a retrospective study. Cleft Palate Craniofac J. 2014;51:e1–e10. doi: 10.1597/12-099. [DOI] [PubMed] [Google Scholar]
- 16.Mars M, Houston WJ. A preliminary study of facial growth and morphology in unoperated male unilateral cleft lip and palate subjects over 13 year of age. Cleft Palate Craniofac J. 1990;27:7–10. doi: 10.1597/1545-1569(1990)027<0007:apsofg>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 17.Smahel Z. Craniofacial morphology in adults with bilateral complete cleft lip and palate. Cleft Palate J. 1984;21:159–69. [PubMed] [Google Scholar]
- 18.Smahel Z, Müllerová Z. Craniofacial morphology in unilateral cleft lip and palate prior to palatoplasty. Cleft Palate J. 1986;23:225–32. [PubMed] [Google Scholar]
- 19.Oztürk Y, Cura N. Examination of craniofacial morphology in children with unilateral cleft lip and palate. Cleft Palate Craniofac J. 1996;33:32–6. doi: 10.1597/1545-1569_1996_033_0032_eocmic_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 20.Krogman WM, Mazaheri M, Harding RL, Ishiguro K, Bariana G, Meier J, et al. A longitudinal study of the craniofacial growth pattern in children with clefts as compared to normal, birth to six years. Cleft Palate J. 1975;12:59–84. [PubMed] [Google Scholar]
- 21.Hayashi I, Sakuda M, Takimoto K, Miyazaki T. Craniofacial growth in complete unilateral cleft lip and palate: a roentgeno-cephalometric study. Cleft Palate J. 1976;13:215–37. [PubMed] [Google Scholar]
- 22.Fudalej P, Obloj B, Dudkiewicz Z, Hortis-Dzierzbicka M. Mandibular morphology and spatial position following one-stage simultaneous repair of complete unilateral cleft lip and palate. Cleft Palate Craniofac J. 2008;45:272–7. doi: 10.1597/06-195. [DOI] [PubMed] [Google Scholar]
- 23.Shibasaki Y, Ross RB. Facial growth in children with isolated cleft palate. Cleft Palate J. 1969;6:290–302. [PubMed] [Google Scholar]
- 24.Zúñiga C, Miralles R, Carvajal R, Ravera MJ, Contreras P, Cavada G. Comparative study between children with and without cleft lip and cleft palate, part 1: Cephalometric analysis. Cleft Palate Craniofac J. 2000;37:281–5. doi: 10.1597/1545-1569_2000_037_0281_csbcwa_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 25.Enemark H, Bolund S, Jorgensen I. Evaluation of unilateral cleft lip and palate treatment: Long term results. Cleft Palate Craniofac J. 1990;27:354–61. doi: 10.1597/1545-1569(1990)027<0354:eoucla>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 26.Da Silva Filho OG, Carvalho Lauris RC, Capelozza Filho L, Semb G. Craniofacial morphology in adult patients with unoperated complete bilateral cleft lip and palate. Cleft Palate Craniofac J. 1998;35:111–9. doi: 10.1597/1545-1569_1998_035_0111_cmiapw_2.3.co_2. [DOI] [PubMed] [Google Scholar]


