Abstract
Background: Cell phone text messaging, via the Short Messaging Service (SMS), offers the promise of a highly portable, well-accepted, and inexpensive modality for engaging youth and young adults in the management of their diabetes. This pilot and feasibility study compared two-way SMS cell phone messaging with e-mail reminders that were directed at encouraging blood glucose (BG) monitoring.
Methods: Forty insulin-treated adolescents and young adults with diabetes were randomized to receive electronic reminders to check their BG levels via cell phone text messaging or e-mail reminders for a 3-month pilot study. Electronic messages were automatically generated, and participant replies with BG results were processed by the locally developed Computerized Automated Reminder Diabetes System (CARDS). Participants set their schedule for reminders on the secure CARDS website where they could also enter and review BG data.
Results: Of the 40 participants, 22 were randomized to receive cell phone text message reminders and 18 to receive e-mail reminders; 18 in the cell phone group and 11 in the e-mail group used the system. Compared to the e-mail group, users in the cell phone group received more reminders (180.4 vs. 106.6 per user) and responded with BG results significantly more often (30.0 vs. 6.9 per user, P=0.04). During the first month cell phone users submitted twice as many BGs as e-mail users (27.2 vs. 13.8 per user); by month 3, usage waned.
Conclusions: Cell phone text messaging to promote BG monitoring is a viable and acceptable option in adolescents and young adults with diabetes. However, maintaining interest levels for prolonged intervals remains a challenge.
Introduction
Successful diabetes management requires the delivery of complicated medical tasks like blood glucose (BG) monitoring and insulin administration along with the practice of healthful behaviors around food and exercise. BG monitoring remains a critical component of diabetes care, and its daily frequency correlates consistently with glycemic control.1–5 However, BG monitoring frequency often declines in adolescents and young adults with diabetes who are frequently challenged by the competing demands of diabetes management and their social and developmental needs.6,7 Indeed, adolescents and young adults often experience poor metabolic control compared with other age groups because of reduced adherence.8–12 It is critical to maintain BG monitoring frequency through this developmental stage since it has been demonstrated that those with poor adjustment to diabetes in adolescence are likely to continue such behaviors into adulthood.13,14
Increased involvement with healthcare providers may improve glycemic control and reduce the risk of complications,15 but these interactions are labor-intensive and expensive. Low-cost clinic-based interventions in younger adolescents have yielded a positive impact on both glycemic control and quality of life.16–18 Identifying other effective, low-cost interventions using telemedicine may benefit the adolescent and young adult age group.19,20
Emerging technologies, such as cell phone text messaging, offer another inexpensive yet well-accepted way to increase communication with adolescents with diabetes.21 Indeed, cell phones are nearly universal; as of June 2007, 81% of Americans owned a cell phone,22 including the overwhelming majority of adolescents and 97% of college students.23
Almost all cell phones offer text messaging capabilities known as Short Messaging Service (SMS), which is a popular communication tool among teens.24 SMS messaging appears ideal for sending and receiving small snippets of data, such as BG values. SMS messages have provided reminders for clinic visits,25,26 tuberculosis medication compliance,27 and asthma control,28,29 as well as diabetes monitoring30–38 in adults. Few studies have focused on teens. Some for-profit Internet companies offer such a reminder service directly to patients, and phones integrated with BG meters have been marketed.39,40
The purpose of our pilot study was to test the feasibility of implementing a fully automated, two-way text messaging system to encourage increased BG monitoring in teens and young adults with diabetes using the Computerized Automated Reminder Diabetes System (CARDS). We hypothesized that reminders sent via cell phone messaging would result in greater frequency of BG monitoring compared to reminders sent via e-mail messaging. We also hypothesized that such a reminder system would be well accepted by this age group. Finally, we sought to assess user satisfaction of a reminder system and current technology usage patterns among adolescents/young adults.
Subjects and Methods
Participants
This study was approved by the Joslin Diabetes Center (Boston, MA) institutional review board. Eligibility included insulin-treated patients, 12–25 years old, who had an SMS-capable cell phone and home Internet with e-mail access. Forty participants, recruited as a convenience sample, agreed to participate during a regularly scheduled visit. Participants were offered free parking and compensation to cover the costs of text messaging.
After informed consent (and assent for youths under 18 years of age) was obtained, participants completed a brief questionnaire to ascertain their current technology use. Participants were randomized to receive reminders either via cell phone text messaging or by e-mail, and they had access to the automated reminder system for 3 months. Participants received a 15-min introduction to CARDS. The number and frequency of reminders were determined by the participants, and no reminders were sent until participants logged onto the website. Approximately 1 week after study entry, study staff (D.A.H.) called participants to answer any questions and encourage usage. After 4 weeks, participants also received a follow-up e-mail. At the next regularly scheduled clinic visit, participants completed a final questionnaire concerning their use of CARDS. Chart review provided data regarding the participants' diabetes management. Glycemic control was assessed by hemoglobin A1c (HbA1c) (reference level 4–6%) (Tosoh 2.2 glycohemoglobin analyzer, Tosoh Corp., Foster City, CA) at entry and at follow-up.
CARDS
CARDS, created by the authors, included a web-based module and a messaging/reminder module designed to run autonomously. All actions were recorded to a log for later analysis. The entire system operated on a 500 MHz Apple (Cupertino, CA) Macintosh PowerBook laptop computer with 768 MB of memory.
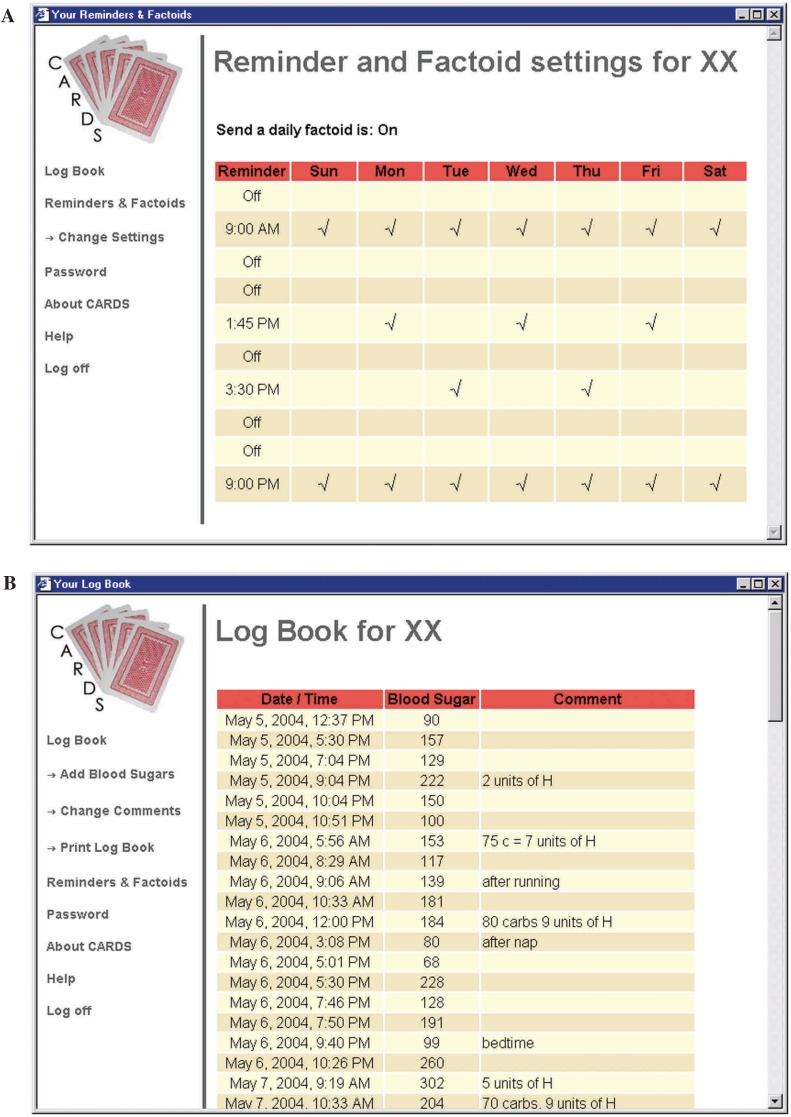
Participants logged into the system via a secure website with their chosen username and password. The web site provided a screen for participants to customize their schedule for reminder messages (Fig. 1A) by time of day and day of week. The CARDS website offered participants the ability to comment, edit, view, and print their BG diaries with a time and date stamp (Fig. 1B). Comments could be changed, but BG values, once entered, could not. Participants could also opt to receive two daily factoids: one related to diabetes education/nutrition (e.g., “Did you know? One 12 fluid oz. can of soda has 10 teaspoons of sugar?”) and one related to unusual fun facts or trivia (e.g., “Butterflies taste with their feet.”). In contrast to the BG reminders, each factoid was sent randomly between 4:00 p.m. and 9:00 p.m. daily, and the factoids were only sent after the participant opted-in to receive them.
FIG. 1.
(A) A screenshot of the CARDS website showing a customized reminder schedule. This example shows four daily reminder times (9:00 a.m., 1:45 p.m., 3:30 p.m., and 9:00 p.m.) out of the maximum of 10 possible reminder times. The reminders at 9:00 a.m. and 9:00 p.m. occur daily, whereas those for 1:45 p.m. and 3:30 p.m. occur on alternating days Monday–Friday. A user may alter at anytime the reminder times and schedule. (B) A screenshot of the CARDS diary displaying BG data received by either e-mail or cell phone response as well as by retrospective data entry on the website by the user. H, Humalog insulin.
At a preset time, CARDS would send either by cell phone text message or by e-mail a reminder to check the BG. If CARDS did not receive a response from the participant within 15 min, a single repeat reminder was sent (e.g., “In case you missed the first reminder, it's time to check your blood sugar.”) The wording of the reminders varied and was chosen randomly from a list (e.g., “Just a reminder to check your blood sugar.”). After a user submitted a BG value, regardless of the result, he or she received positive feedback (e.g., “The blood sugar was received. Keep up the good work!”). If the submitted BG value was out of range (<70 or >300 mg/dL; <3.9 or >16.7 mmol/L), CARDS provided a warning to take appropriate action according to the healthcare team's recommendations and then recheck the BG. Users could submit a BG value at any time, and feedback was provided. In addition, if a BG value was sent within 1 h of a preset reminder, the reminder was suppressed. BG values submitted by cell phone or e-mail could be viewed immediately and printed. Every Sunday, cell phone and e-mail participants received a reminder to view and print their BG diaries.
Statistical analysis
Data from system usage, either by e-mail or cell phone, contributed to the definition of user. Characteristics are compared between the e-mail and cell phone groups and between users and nonuser groups. Participants were considered users if they logged into the system or submitted a BG measurement. Both baseline and final survey responses refer to all study participants, not just the users. Statistical analyses employed Microsoft (Redmond WA) Excel and SAS version 8.2 for Windows (SAS Institute, Cary, NC). Unpaired t tests and χ2 analyses were performed. Two-tailed P values of <0.05 were considered significant.
Results
Of the 40 participants recruited, 18 were randomly assigned to received e-mail reminders and 22 to receive cell phone reminders. Following randomization, 11 (27.5%) never used the system (nonusers): seven from the e-mail group and four from the cell phone group. There were 11 e-mail users and 18 cell phone users. Table 1 compares the baseline characteristics of the groups. There were no significant differences between e-mail and cell phone groups, and users and nonusers only differed by gender. Females were more likely to be users than males (P=0.04), regardless of the communication modality, with 86% of females compared with 56% of males using the system.
Table 1.
Baseline Characteristics of the Study Participants According to Group
| Assigned group | User status | |||
|---|---|---|---|---|
| E-mail (n=18) | Phone (n=22) | Users (n=29) | Nonusers (n=11) | |
| Age (years) | 18.2±2.3 | 17.7±3.0 | 17.9±2.8 | 18.0±2.2 |
| Duration of diabetes (years) | 9.5±5.6 | 9.0±4.2 | 9.2±4.9 | 9.2±4.9 |
| Gender (% female) | 50 | 60 | 66a | 27a |
| Pre-study HbA1c (%) | 8.8±1.5 | 9.0±1.8 | 8.8±1.4 | 9.3±2.1 |
| Insulin route | ||||
| % injection | 72 | 73 | 69 | 82 |
| % pump | 28 | 27 | 31 | 18 |
P=0.04.
Table 2 displays the 3-month usage patterns for different components of CARDS. Users in the phone group compared with users in the e-mail group requested more reminders (180.4 vs. 106.6 per user) and submitted more BG values (46 vs. 23.5 per user). Phone users responded to a higher percentage of reminders within 30 min compared to e-mail users (16.6% vs. 6.5%). As a result, cell phone users submitted significantly more BG measurements to CARDS by responding to reminders than e-mail users (33.1 vs. 2.3 per user, P<0.02).
Table 2.
Comparison of 3 Months of CARDS Use Between E-Mail and Cell Phone Users
| E-mail (n=11) | Phone (n=18) | |
|---|---|---|
| Logins to the system | 4.2 | 3.6 |
| Reminders sent | 106.6 | 180.4 |
| Responses to remindersa | 6.9 | 30.0 |
| Response rate (%) | 6.5 | 16.6 |
| BG values submitted via phone/e-mailb | 2.3 | 33.1 |
| BG values submitted via web | 21.2 | 12.9 |
| Total BG values submitted | 23.5 | 46.0 |
| Viewed diary | 3.7 | 2.7 |
| Diabetes factoids sent | 67.7 | 49.2 |
Usage data were obtained from the CARDS system log over the 3-month trial period. All numbers are mean values. Response rate was (number of responses to reminders/number of reminders sent)×100. Total BG values submitted was (number of BG values submitted via phone/e-mail+number of BG values submitted via web).
P=0.04, bP=0.02 by unpaired t test.
Participants could submit BG values directly onto the website for entry into the diary (see Fig. 1B). While the e-mail group responded significantly less often to reminders than the cell phone group (6.9 vs. 30 per user, P=0.04), the e-mail group entered more BG values directly into the web diary independent of reminders compared to the cell phone group (21.2 vs. 12.9 per user).
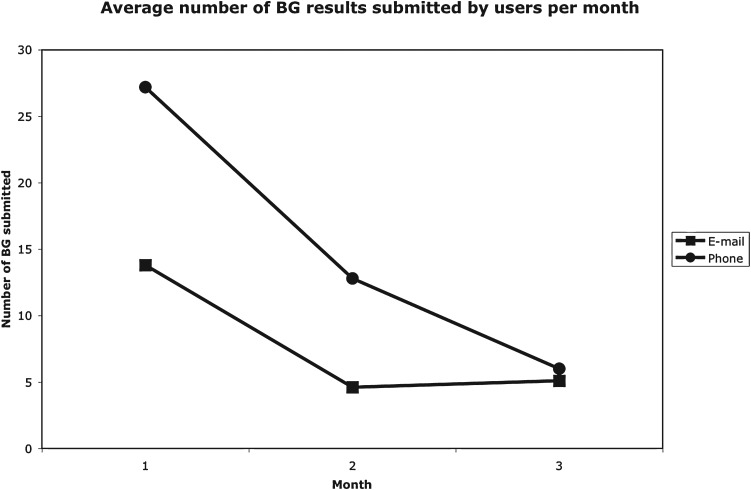
During the first month of the study, on average, users in the cell phone group submitted nearly twice as many BG measurements as those in the e-mail group (27.2 vs. 13.8 per user) (Fig. 2). With time, the average number of BG values submitted to CARDS decreased in both groups. By the third month, only one user in the e-mail group and five users in the cell phone group continued to submit BG measurements.
FIG. 2.
The average number of BG results per user by study month submitted to CARDS declined with time. In month 1, there were twice as many BG measurements submitted in the cell phone group compared with the e-mail group. By month 3, the number of BG measurements submitted declined markedly, and values were similar between groups.
In this pilot trial, no difference in glycemic control between groups was anticipated. At baseline, the mean HbA1c values were 8.6±0.9% and 8.9±1.7% in the e-mail and cell phone users, respectively. After the study, the mean values remained similar, at 8.8±0.9% for e-mail users and 8.7±1.5% for cell phone users.
Baseline questionnaires revealed that 60% of participants in general used instant messaging daily, 35% used e-mail daily, and 23% used cell phone text messaging daily. Notably, at enrollment, 75% of participants carried cell phones to their clinic visits, while 65% had their BG meters, and only 28% had their paper BG diaries. Ten participants (25%) brought neither their meters nor a logbook to the clinic visit.
At the study's conclusion, participants were asked how they would prefer to access CARDS in the future if it were available. Half (50%) chose the cell phone, 17% chose e-mail, another 10% chose both, and 23% chose neither option. Two-thirds (12 of 18) of the participants assigned to the e-mail group commented that they did not like their assignment and would have preferred cell phone reminders. Participants also provided suggestions for improving CARDS. Two suggested incorporating the functionality of CARDS into a pump or a meter. Another suggested having a healthcare provider call if the participant did not submit BG measurements for several days.
Discussion
Our pilot and feasibility study demonstrated that it is technically possible to implement a fully automated system to engage youth with diabetes. CARDS used a very inexpensive computing system. In addition, the ongoing operation of the system required few resources other than electricity and an Internet connection. Finally, training participants to use CARDS was relatively easy, likely because of this age group's familiarity with technology.
While the design and implementation of CARDS may be viewed as a success in this pilot, there are two obvious areas of disappointment. First, 11 of the 40 (27.5%) enrolled participants never used the system, the majority of whom (seven of 11) were randomized to the e-mail group. Second, usage dropped off considerably after the first month, even in the more popular cell phone group. A crossover study design would have allowed all participants to use the cell phone and e-mail modalities to provide direct comparison. In addition, a standard set-up of reminders for both the cell phone and e-mail groups, created in clinic, may have allowed us to assess responses to an equivalent stimulus by each group. Further, eligibility criteria for CARDS participation included availability of both cell phone and e-mail access. Thus, there was likely a small subset of patients who lack cell phones and/or e-mail access who would be unable to utilize such technologies.
It is possible that the limited use and drop-off in CARDS usage in months 2 and 3 may have resulted from the study's timing over the summer months. All CARDS participants were enrolled during mid- to late spring. One study with patients 18–75 years old found a similar drop in mobile phone text messaging use during holiday periods.32 On the other hand, one study from Finland of SMS messaging in adult patients with diabetes found no change in BG measurement activity over a 12-month study period.33 A recent study from the United Kingdom compared cell phones, e-mail, and written diaries for the tracking of hypoglycemic episodes in children with diabetes.41 These authors reported that cell phones were the preferred modality and generated the highest response rate for tracking hypoglycemia, a finding similar to our experience with CARDS in the first month.
It is also likely that the innovation of the system, related to its spontaneity and encouragement, became repetitive and exhausting with time. In a study of technology involving automated pump alerts, youths 8–20 years old received reminder alarms to bolus insulin.42 Similarly, by the third month of that trial, many participants were ignoring the reminder alarms such that the positive impact of the bolus reminders on the decrement in HbA1c was lost from month 3 to month 6. The pump reminders led to an initial increase in mealtime insulin bolus dosing that waned after 3 months. Likewise, fatigue from the BG reminders in CARDS was evident with drop-off in usage in months 2 and 3. In addition, use of the CARDS website was low and may reflect the need for such websites to consider in their design the interests of adolescents and the recognized burden of diabetes management.43 In an earlier study, we demonstrated a short-term increase in BG monitoring frequency in association with the implementation of an interactive BG monitoring guessing game.44 There was similar drop-off in the BG monitoring frequency as the trial progressed.
Our population of youth and young adults carried cell phones to their diabetes visits, without prior knowledge of the CARDS study. Fewer patients had meters, and even less had a paper BG diary. A study from Australia found that 91% of patients (16–24 years old) attending a general practice clinic owned a phone.45 This suggests that cell phones may be an ideal modality with which to target youths with diabetes, especially since this population embraces new technologies.46
Our study was not powered to detect a difference in outcomes between the cell phone and the e-mail group. Rather, we designed the investigation as a pilot study to assess feasibility and acceptability of an electronic BG reminder system. In fact, we assessed CARDS usage with the frequency of BG reminders and responses rather than the values of the BG results since our interest was to encourage BG monitoring behavior. On average, CARDS automatically sent 2.1 daily messages (reminders and factoids) to the e-mail group and 2.7 daily messages to the cell phone group. In a recent study, a two-way paging system sent an average of 3.2 messages per day.30 In our cell phone group, users responded to 16.6% of reminders, similar to the 14% response rate in the pager study. Thus, it seems unrealistic to expect users to respond to every message received, although participants could have checked their BG level in response to the reminder prompt even if they did not reply to the reminder.
This pilot study demonstrated a small nonsignificant increase in HbA1c in the e-mail group and a small nonsignificant decrease in the cell phone group. Similarly, a recent study found a small, nonsignificant decrease in HbA1c levels for patients with poorly controlled diabetes who received weekly support messages via SMS for 6 months.47 A review of various telemedicine interventions (e.g., modem transfer, telephone calls, text messages, etc.) for diabetes management concluded that, to date, there was little evidence to suggest that such interventions actually improved HbA1c levels.34
While not all patients may benefit from interventions such as CARDS, the low cost of implementation may make automated reminder systems worthwhile for those patients responsive to such reminders. Additionally, further refinements could include appointment reminders and alerts for patients to bring their logbooks and/or meters to their clinic visits. In addition, medication reminders and educational messages may be helpful for some patients.48
While the participants in our study selected the timing and frequency of the reminders to check BG levels and the automated responses were always supportive, there was no immediate medical advice provided by the healthcare team. Future iterations of such a system may incorporate functionality for notification of healthcare providers when results are out of range or data are absent. In turn, the healthcare team could reach out to these patients by phone, by e-mail, or in person, although funding of any phone or e-mail outreach would likely be required. As technologies such as cell phone text messaging continue to advance and gain popularity, it will likely be helpful for healthcare providers to reinvent their approaches to utilize such innovation to reach youths with diabetes in efforts to optimize their glycemic control.
Acknowledgments
D.A.H. provided the technical capabilities for the design and implementation of CARDS. We would also like to thank Robert A. Greenes, Andrew Seger, Steven Labkoff, and the Joslin Information Technology staff. Financial support was provided by the Katherine Adler Astrove Fund and the Maria Griffin Drury Pediatric Research Fund.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Karter AJ, Ackerson LM, Darbinian JA, D'Agostino RB, Jr, Ferrara A, Liu J, Selby JV: Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med 2001;111:1–9 [DOI] [PubMed] [Google Scholar]
- 2.Haller MJ, Stalvey MS, Silverstein JH: Predictors of control of diabetes: monitoring may be the key. J Pediatr 2004;144: 660–661 [DOI] [PubMed] [Google Scholar]
- 3.Nathan DM, McKitrick C, Larkin M, Schaffran R, Singer DE: Glycemic control in diabetes mellitus: have changes in therapy made a difference? Am J Med 1996;100:157–163 [DOI] [PubMed] [Google Scholar]
- 4.Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L: Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr 1997;130:257–265 [DOI] [PubMed] [Google Scholar]
- 5.Levine BS, Anderson BJ, Butler DA, Brackett J, Laffel L: Predictors of glycemic control and short-term adverse outcomes in youth with type 1 diabetes. J Pediatr 2001;139:197–203 [DOI] [PubMed] [Google Scholar]
- 6.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB: Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care 2001;24:1536–1540 [DOI] [PubMed] [Google Scholar]
- 7.Moreland EC, Tovar A, Zuehlke JB, Butler DA, Milaszewski K, Laffel LM: The impact of physiological, therapeutic and psychosocial variables on glycemic control in youth with type 1 diabetes mellitus. J Pediatr Endocrinol Metab 2004;17:1533–1544 [DOI] [PubMed] [Google Scholar]
- 8.Laffel L, Pasquarello C, Lawlor M: Treatment of the child and adolescent with diabetes. In: Kahn CR, Weir GC, King GL, Jacobson AM, Moses AC, Smith RJ, eds. Joslin's Diabetes Mellitus, 14th ed. Philadelphia: Lippincott Williams & Wilkins, 2005:711–736 [Google Scholar]
- 9.Anderson BJ, Laffel L: Behavioral and family aspects of the treatment of children and adolescents with insulin dependent diabetes mellitus. In: Porte D, Sherwin R, Rifkin H, eds. Ellenberg and Rifkin's Diabetes Mellitus, 5th ed. Stamford, CT: Appleton & Lange, 1996:811–825 [Google Scholar]
- 10.Glasgow AM, Weissberg-Benchell J, Tynan WD, Epstein SF, Driscoll C, Turek J, Beliveau E: Readmissions of children with diabetes mellitus to a children's hospital. Pediatrics 1991;88:98–104 [PubMed] [Google Scholar]
- 11.Laron-Kenet T, Shamis I, Weitzman S, Rosen S, Laron Z: Mortality of patients with childhood onset (0–17 years) Type 1 diabetes in Israel: a population based study. Diabetologia 2001;44:B81–B86 [DOI] [PubMed] [Google Scholar]
- 12.Wibell L, Nystrom L, Ostman J, Arnqvist H, Blohme G, Lithner F, Lottorin B, Sundkvist G: Increased mortality in diabetes during the first 10 years of the disease: a population-based study (DISS) in Swedish adults 15–34 years old at diagnosis. J Intern Med 2001;249:263–270 [DOI] [PubMed] [Google Scholar]
- 13.Wysocki T, Hough BS, Ward KM, Green LB: Diabetes mellitus in the transition to adulthood: adjustment, self-care, and health-status. Dev Behav Pediatr 1992;13:194–201 [PubMed] [Google Scholar]
- 14.Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA: Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care 2003;26:1052–1057 [DOI] [PubMed] [Google Scholar]
- 15.Kaufman FR, Halvorson M, Carpenter S: Association between diabetes control and visits to a multidisciplinary pediatric diabetes clinic. Pediatrics 1999;103:948–951 [DOI] [PubMed] [Google Scholar]
- 16.Laffel LM, Brackett J, Ho J, Anderson BJ: Changing the process of diabetes care improves metabolic outcomes and reduces hospitalizations. Qual Manag Health Care 1998;6:53–62 [DOI] [PubMed] [Google Scholar]
- 17.Brink SJ: How to apply the experience from the Diabetes Control and Complications Trial to children and adolescents? Ann Med 1997;29:425–438 [DOI] [PubMed] [Google Scholar]
- 18.Grey M, Boland EA, Davidson M, Li J, Tamborlane WV: Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr 2000;137:107–113 [DOI] [PubMed] [Google Scholar]
- 19.Farmer A, Gibson O, Hayton P, Bryden K, Dudley C, Neil A, Tarassenko L: A real-time, mobile phone-based telemedicine system to support young adults with type 1 diabetes. Inform Prim Care 2005;13:171–177 [DOI] [PubMed] [Google Scholar]
- 20.Farmer AJ, Gibson OJ, Dudley C, Bryden K, Hayton PM, Tarassenko L, Neil A: A randomized controlled trial of the effect of real-time telemedicine support on glycemic control in young adults with type 1 diabetes (ISRCTN 46889446). Diabetes Care 2005;28:2697–2702 [DOI] [PubMed] [Google Scholar]
- 21.Gimenez-Perez G, Gallach M, Acera E, Prieto A, Carro O, Ortega E, Gonzalez-Clemente JM, Mauricio D: Evaluation of accessibility and use of new communication technologies in patients with type 1 diabetes mellitus. J Med Internet Res 2002;4:E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cellular Telecommunications & Internet Association: Wireless Quick Facts: 2007. http://www.ctia.org/media/industry_info/index.cfm/AID/10323 (accessed January8, 2008)
- 23.Ransford M: Study: College Students Receive, but Don't Recall, Cell Phone Ads. http://bsu.edu/news/article/0,1370,-1019-31674,00.html (accessed January8, 2008)
- 24.Johnson B: Connected and Craving: Teens Hunger for Latest Cell Phone Technology. http://www.rcrnews.com/apps/pbcs.dll/article?AID=/20060320/SUB/603200738/1008/FREE (accessed January8, 2008)
- 25.Downer SR, Meara JG, Da Costa AC: Use of SMS text messaging to improve outpatient attendance. Med J Aust 2005;183:366–368 [DOI] [PubMed] [Google Scholar]
- 26.Dyer O: Patients will be reminded of appointments by text messages. BMJ 2003;326:1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evaluation of the On Cue Compliance Service Pilot: Testing the Use of SMS Reminders in the Treatment of Tuberculosis in Cape Town, South Africa. http://bridges.org/files/active/0/Cmplnc-EvlRpt_FIN_29Mar05.pdf (accessed May20, 2006)
- 28.Anhoj J, Moldrup C: Feasibility of collecting diary data from asthma patients through mobile phones and SMS (short message service): response rate analysis and focus group evaluation from a pilot study. J Med Internet Res 2004;6:e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anhoj J, Nielsen L: Quantitative and qualitative usage data of an Internet-based asthma monitoring tool. J Med Internet Res 2004;6:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leu MG, Norris TE, Hummel J, Isaac M, Brogan MW: A randomized, controlled trial of an automated wireless messaging system for diabetes. Diabetes Technol Ther 2005;7:710–718 [DOI] [PubMed] [Google Scholar]
- 31.Rami B, Popow C, Horn W, Waldhoer T, Schober E: Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr 2006;165:701–705 [DOI] [PubMed] [Google Scholar]
- 32.Ferrer-Roca O, Cardenas A, Diaz-Cardama A, Pulido P: Mobile phone text messaging in the management of diabetes. J Telemed Telecare 2004;10:282–285 [DOI] [PubMed] [Google Scholar]
- 33.Vahatalo M, Virtamo H, Viikari J, Ronnemaa T: Cellular phone transferred self blood glucose monitoring: prerequisites for positive outcome. Pract Diabetes Int 2004;21:192–194 [Google Scholar]
- 34.Farmer A, Gibson OJ, Tarassenko L, Neil A: A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med 2005;22:1372–1378 [DOI] [PubMed] [Google Scholar]
- 35.Kim HS: A randomized controlled trial of a nurse short-message service by cellular phone for people with diabetes. Int J Nurs Stud 2007;44:687–692 [DOI] [PubMed] [Google Scholar]
- 36.Gammon D, Arsand E, Walseth OA, Andersson N, Jenssen M, Taylor T: Parent-child interaction using a mobile and wireless system for blood glucose monitoring. J Med Internet Res 2005;7:e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwon HS, Cho JH, Kim HS, Lee JH, Song BR, Oh JA, Han JH, Kim HS, Cha BY, Lee KW, Son HY, Kang SK, Lee WC, Yoon KH: Development of web-based diabetic patient management system using short message service (SMS). Diabetes Res Clin Pract 2004;66(Suppl 1):S133–S137 [DOI] [PubMed] [Google Scholar]
- 38.Franklin V, Waller A, Pagliari C, Greene S: “Sweet Talk”: text messaging support for intensive insulin therapy for young people with diabetes. Diabetes Technol Ther 2003; 5:991–996 [DOI] [PubMed] [Google Scholar]
- 39.Carroll AE, Marrero DG, Downs SM: The HealthPia Gluco-Pack Diabetes phone: a usability study. Diabetes Technol Ther 2007;9:158–164 [DOI] [PubMed] [Google Scholar]
- 40.www.textmemos.com (accessed January11, 2008)
- 41.Tasker AP, Gibson L, Franklin V, Gregor P, Greene S: What is the frequency of symptomatic mild hypoglycemia in type 1 diabetes in the young?: assessment by novel mobile phone technology and computer-based interviewing. Pediatr Diabetes 2007;8:15–20 [DOI] [PubMed] [Google Scholar]
- 42.Chase HP, Horner B, McFann K, Yetzer H, Gaston J, Banion C, Fiallo-Scharer R, Slover R, Klingensmith G: The use of insulin pumps with meal bolus alarms in children with type1 diabetes to improve glycemic control. Diabetes Care 2006;29:1012–1015 [DOI] [PubMed] [Google Scholar]
- 43.Terdiman D: What Websites Do to Turn on Teens. http://www.wired.com/news/culture/0,1284,66514,00.html (accessed January8, 2008)
- 44.Kumar VS, Wentzell KJ, Mikkelsen T, Pentland A, Laffel LM: The DAILY (Daily Automated Intensive Log for Youth) Trial: a wireless, portable system to improve adherence and glycemic control in youth with diabetes. Diabetes Technol Ther 2004;6:445–453 [DOI] [PubMed] [Google Scholar]
- 45.Haller D, Sanci L, Sawyer S, Coffey C, Patton G: R U OK 2 TXT 4 RESEARCH?—feasibility of text message communication in primary care research. Aust Fam Physician 2006;35:175–176 [PubMed] [Google Scholar]
- 46.Hanauer DA, Wentzell K, Tovar A, Zeuhlke J, Kumar V, Laffel LM: Parent and youth assessments of a handheld wireless device to enhance diabetes mellitus management. Arch Pediatr Adolesc Med 2006;160:321. [DOI] [PubMed] [Google Scholar]
- 47.Benhamou PY, Melki V, Boizel R, Perreal F, Quesada JL, Bessieres-Lacombe S, Bosson JL, Halimi S, Hanaire H: One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes Metab 2007;33:220–226 [DOI] [PubMed] [Google Scholar]
- 48.Wangberg SC, Arsand E, Andersson N: Diabetes education via mobile text messaging. J Telemed Telecare 2006;12(Suppl 1):55–56 [DOI] [PubMed] [Google Scholar]