Abstract
Hispanic women in the United States (US) are disproportionately affected by human immunodeficiency virus (HIV) infection. There are very limited data on the sexual risk differences among US-born Hispanic women (USBHW) and foreign-born Hispanic women (FBHW). Sexually active USBHW and FBHW were asked to complete a self-administered questionnaire. Demographics, sexual history, testing for HIV or sexually transmitted infection (STI), condom use, partner sexual risk and alcohol/substance use were compared between USBHW and FBHW. FBHW were 3.5 years older than USBHW at first sexual experience (95% CI: 2.8, 4.1; P < 0.001). This remained significant after controlling for age and education. There was no difference between groups in the proportion of women with >1 reported sexual partner in the last year. FBHW reported fewer risk behaviors and lower rates of STI and alcohol/drug abuse. However, FBHW were less likely to have been tested for HIV. HIV prevention strategies would better target Hispanic women in the US if differences in risk behavior between FBHW and USBHW were incorporated.
Keywords: Hispanic, Foreign-born, HIV/AIDS, Sexually transmitted disease, Sexual risk behavior
Introduction
It has been projected that Hispanics will account for 30% of the United States (US) population (132 million) by 2050 [1]. According to the 2011 US census, an estimated 19.8 million foreign-born Hispanics reside in the US, 11.4 million of which are from Mexican origin; this represents 30% of the foreign-born US population [2]. Human immunodeficiency virus type 1 (HIV-1) infection and the acquired immunodeficiency syndrome (AIDS) have disproportionately affected Hispanics in the US [3]. The 2010 HIV surveillance report from the Centers for Disease Control and Prevention (CDC) showed that Hispanics have the second highest incidence rate of HIV-1 infection among all ethnic groups in the US [4]. In addition, although Hispanics comprise approximately 13% of the US population, they accounted for 17% of the new HIV infections [5]. In regard to Hispanic women, a 2011 report from the CDC found that the US incidence of HIV-1 infection in this group (11.9 per 100,000) was almost five times that observed in white women; of these cases, more than 80% were infected through their male partners, and approximately 55–60% occurred in women of reproductive age [6]. In addition, the rate of AIDS diagnosis in Hispanic women in the US is over 5 times higher than white women (7.9/100,000 vs. 1.5/100,000) [6].
Mobility and immigration to a foreign country are well-documented risk factors for the acquisition of HIV-1 infection [7], particularly when individuals migrate from a low-prevalence area, like most countries in Latin America, to a higher prevalence area like the US. Specifically, migration has a direct influence on sexual behavior because it can modify an individual's propensity to engage in risky activities, which increases the risk for HIV-1 infection. Migrants often find themselves lonely and isolated, living in sub-standard conditions and most of them sustain prolonged periods of time away from home and family [8]. In addition, migrants may be faced with new and more sexually permissive norms and customs which they have never experienced in their country of origin. This new environment can give the migrant a sense of anonymity that facilitates risky behavior. In addition, migrants may also face new-onset depression, anxiety and loss of self-esteem, all of which have been associated with high-risk sexual practices such as casual sex with random partners, frequent access to commercial sex workers, illicit drug use and same-gender sexual activity such as oral and anal sex, among others [9–11]. Lastly, migration is also a risk factor for financial distress, homelessness and other social factors that increase the risk of HIV-1 and other sexually transmitted infections (STIs) [7, 8, 12].
Previous studies have identified differences in sexual risk factors among US-born blacks compared to Caribbean-born blacks [13], but there are no studies that evaluate differences in HIV-1/AIDS risk factors between foreign-born and US-born Hispanic adults, specifically in women. In addition, current HIV-1 prevention strategies in the US do not differentiate between Foreign-born Hispanic women (FBHW) and US-born Hispanic women (USBHW), and the stigmatization of sexual health among this ethnic group continues to be a major barrier for adequate sexual health education, particularly for younger generations.
The objective of this study was to identify differences in behavioral sexual risk factors between FBHW and USBHW. The available studies that have evaluated risk behavior in Hispanic women have focused on a specific subset of individuals, and their results cannot always be extrapolated to the general adult Hispanic women population. For example, a recent study that assessed the access to HIV-1 prevention and education services among Latinos at high risk for HIV-1 infection found that foreign-born Latinas had a lower number of sexual partners and an overall reduced risk of HIV-1/AIDS when compared to the US-born Latinas [14]. Similarly, a study conducted in HPV-infected Mexican-American women found that women born in Mexico were significantly older at the time of their first sexual encounter [15]. This led us to our primary hypothesis that FBHW women will show some advantages in comparison to USBHW in terms of high-risk sexual behavior such as older age at first sexual experience and a lower number of sexual partners. The secondary endpoints included differences by origin in STI rate, condom use, access to HIV-1 testing, concomitant alcohol and substance abuse and HIV-1/STI risk beliefs and disclosure. To address these questions, we conducted a self-administered survey on sexual risk behavior among USBHW and FBHW in a large metropolitan area in the US.
Methods
Setting, Sample and Recruitment
Our study was conducted at two urban primary care/gynecology clinics in the city of Aurora, Colorado, within the Greater Denver Metropolitan Area. One of our sites was located inside the largest teaching hospital in the area (University of Colorado Hospital), at which approximately 8,000 women are cared for over the course of 1 year. About 10–15% of the population at this site consists of Hispanic women and the majority of the clinic staff is fluent in Spanish. The other survey site was a primary care clinic at a federally qualified family health center (Metro Community Provider Network) located only three blocks from the teaching hospital. This clinic provides primary health care for approximately 7,000 women per year who have no other access to care. Hispanic women, the majority of whom are FBHW, constitute 70–80% of this clinic population and obstetrics and gynecology are the services most often provided at this site. Their staff is 100% fluent in Spanish (many of the staff members are Mexican immigrants themselves), which helps remove some of the cultural barriers to care. Both clinic sites have automated appointment reminder phone calls, which are usually made to the patients 24–48 h prior to their visit. Reflecting these clinic populations, the anticipated distribution of study accrual for FBHW versus USBHW was 2:1.
The survey was aimed towards heterosexual, sexually-active women (within the last year), who were 18 years of age or older. The women were initially approached by the medical assistants (MAs) for participation in the clinic exam rooms after checking-in for their appointment, usually before they were seen by their health care provider. If they agreed to participate, the MAs informed the research assistant (RA) who would then provide the questionnaire. Women were free to decline to take the survey for any reason; however, no records were kept of how many women declined to participate or why. To avoid duplication, individuals were asked if they had previously been asked to participate in the study or had previously completed the survey. There was no compensation for participation in the survey. We obtained approval by the Colorado Multiple Institutional Review Board (COMIRB Protocol #09-0295) prior to the initiation of the study.
Data
Data Collection
The bilingual RA was on-site to approach and recruit patients and to provide and collect the questionnaires from the participants. As previously noted, responses were anonymous. Participants were usually left alone in the exam room to answer the questions in private. If the participant requested assistance, the RA stayed in the room to answer any questions that the participants might have about the content of the questions. The participants were provided the questionnaire in either English or Spanish according to their language preference. Any women who admitted to not being able to read usually declined; however, when a woman indicated that she could not read but wanted to participate, she relied on the RA to read the questions and fill in the answers for her, but the RA was instructed not to influence the participant's responses. If it was known from previous contact with a woman that she could not read, the MAs did not ask the woman to participate in the study. The completed surveys were placed by the participant in a secure location within the exam rooms (locked box), and only the RA had access to the completed questionnaires. These locked boxes were emptied at the end of each clinic session and were discarded upon completion of the study. Data were entered into REDCap electronic data capture tools hosted at the University of Colorado, and verified with double data entry.
A two-page questionnaire was developed for this study and included an introductory paragraph with brief instructions followed by multiple choice and free-response questions with a total of 27 items in six different categories: demographics, sexual history, previous diagnosis of HIV or STI, condom use, partner sexual risk and alcohol/substance abuse. According to an analysis performed by Microsoft Word, the reading level of the survey was rated at 4.9 (readable to anyone with up to a 4th grade education), which is within the recommended reading level for the general US audience [16]. There were two categories of terminology that could be considered above a 4th grade reading level: methods of birth control and the names of common STIs, but neither of those tended to be a problem. Any method of birth control that required purchase of an over-the-counter item or prescription medication from a pharmacy was familiar and, therefore, recognizable to the participant. Multi-syllabic names of STIs were usually recognizable to participants if they had been verbally informed that they had the condition. When a woman did not recognize the words on the questionnaire but had been diagnosed with an STI, she would explain the symptoms to the RA, MA or health care provider, who then marked the correct diagnosis or diagnoses on the questionnaire.
Measures and Analysis
Primary outcomes were tested using two-sided tests with a significance level of 0.05. Ordinary least squares regression was used to model age at first sexual experience and logistic regression was used to model the number of women with more than one sex partner in the last year. Model selection for the primary outcomes included testing for an interaction term between current age and region of origin. For all estimates 95% confidence intervals (CI) are reported. Demographics, behavioral characteristics and self-reported medical history were compared between FBHW and USBHW using an exact Pearson Chi-square test for categorical outcomes [17, 18] and continuous outcomes were compared using an unequal variance, two-sample t test. Logistic regression was used to calculate odds ratios (OR), which allowed adjustment (aOR) for potential confounders. For small subgroups or where few events were observed P values utilize an exact chi-square test and odds ratios are not reported. Although a large number of secondary outcomes were analyzed (Tables 3, 4, 5), these models are considered hypothesis generating and are therefore not adjusted for multiple comparisons. All statistical analyses were conducted in SAS 9.2 (Cary, NC).
Table 3.
Birth control methods and condom use
| Outcome | FBHW n = 226 | USBHW n = 94 | Unadjusted |
Adjustedb |
||
|---|---|---|---|---|---|---|
| Odds ratioa | P value | Odds ratioa | P value | |||
| Used at least one form of birth control | 202 (89.4%) | 77 (81.9%) | 1.9 (0.9, 3.6) | 0.072 | 1.5 (0.7, 3.3) | 0.33 |
| If birth control used | n = 202 | n = 77 | ||||
| Used at least 2 forms | 184 (91.1%) | 50 (64.9%) | 5.5 (2.8, 10.8) | <0.001 | 9.9 (4.0, 24.6) | <0.001 |
| Condom use | 145 (64.2%) | 44 (46.8%) | 2.0 (1.2, 3.3) | 0.004 | 2.2 (1.2, 4.0) | 0.008 |
| Oral contraceptives/birth control pills | 71 (31.4%) | 11 (11.7%) | 3.4 (1.7, 6.9) | 0.0004 | 2.8 (1.3, 6.1) | 0.008 |
| Trying to get pregnant | 1 (0.4%) | 6 (6.4%) | – | 0.003 | – | – |
| Other | 67 (29.7%) | 30 (31.9%) | 0.9 (0.5, 1.5) | 0.69 | 0.9 (0.5, 1.7) | 0.85 |
| Asked male partner/s to use a condom | 168 (77.8%) | 68 (78.2%) | 1.0 (0.5, 1.8) | 0.94 | 1.5 (0.7, 3.2) | 0.26 |
| Used condom last time had vaginal or anal sex | 57 (27.7%) | 14 (16.1%) | 2.0 (1.0, 3.8) | 0.04 | 2.3 (1.1, 4.9) | 0.03 |
| In the last year a condom used | n = 101 | n = 69 | ||||
| At least some of the time | 64 (63.4%) | 33(47.8%) | 1.9 (1.0,3.5) | 0.04 | 2.3 (1.1, 4.8) | 0.03 |
| At least half of the time | 38 (37.6%) | 13 (18.8%) | 2.6 (1.3, 5.4) | 0.01 | 3.9 (1.6, 9.4) | 0.002 |
| Have oral sex with male partner/s | 124 (62.0%) | 66 (75.9%) | 0.5 (0.3, 0.9) | 0.02 | 0.6 (0.3, 1.2) | 0.16 |
| If yes | n = 124 | n = 66 | ||||
| Condom used at least some of the time with oral sex | 59 (47.6%) | 16 (24.2% | 2.8 (1.5, 5.5) | 0.002 | 2.5 (1.1, 5.4) | 0.02 |
| Have anal sex with male partner/s | 75 (40.8%) | 30 (34.9%) | 1.3 (0.8, 2.2) | 0.36 | 1.4 (0.7, 2.6) | 0.33 |
| If yes | n = 75 | n = 30 | ||||
| Condom used at least some of the time with anal sex | 41 (54.7%) | 13 (43.3% | 1.6 (0.7, 3.7) | 0.30 | 0.9 (0.3, 2.8) | 0.91 |
| Confident or very confident in convincing partner to use condom | 158 (82.3%) | 74 (88.1%) | 0.6 (0.3, 1.3) | 0.23 | 1.1 (0.5, 2.7) | 0.80 |
| Partner ever refused to use condom | 40 (20.1%) | 12 (14.0%) | 1.6 (0.8, 3.1) | 0.22 | 1.2 (0.5, 2.6) | 0.71 |
| Had sex when you did not want to | 8 (3.8%) | 12 (14.1%) | – | 0.003 | – | – |
FBHW foreign-born Hispanic women, USBHW US-born Hispanic women
FBHW versus USBHW; USBHW are reference group in all ORs
Estimates from model adjusted for current age and education
Table 4.
HIV and STI diagnoses
| Outcome | FBHW n = 226 | USBHW n = 94 | Unadjusted |
Adjustedb |
||
|---|---|---|---|---|---|---|
| ORa | P value | ORa | P value | |||
| Have you ever been tested for HIV? | 113 (54.9%) | 72 (82.8%) | 0.3 (0.1, 0.5) | <0.001 | 0.3 (0.2, 0.7) | 0.003 |
| If No: reason for not getting tested | n = 93 | n = 15 | ||||
| Fear of the result | 4 (4.3%) | 0 (0.0%) | – | 0.64 | – | – |
| Do not know where to get tested | 24 (25.8%) | 6 (40.0%) | – | 0.35 | – | – |
| Do not have health insurance | 20 (21.5%) | 1 (6.7%) | – | 0.29 | – | – |
| Do not think I need to be tested | 31 (33.3%) | 4 (26.7%) | – | 0.77 | – | – |
| Have been told that had an STI? | 42 (18.6%) | 31 (33.0%) | 0.5 (0.3, 0.8) | 0.006 | 0.3 (0.2, 0.6) | 0.001 |
| If yes: year of diagnosis | n = 42 | n = 31 | 0.35 | – | ||
| >10 years ago | 2 (11.8%) | 4 (23.5%) | – | – | ||
| 5–10 years ago | 4 (23.5%) | 1 (5.9%) | – | – | ||
| Past 5 years | 11 (64.7%) | 12 (70.6%) | – | – | ||
| Number of STIs in history | <0.001 | – | ||||
| None | 203 (89.8%) | 70 (74.5%) | – | – | ||
| One | 22 (9.7%) | 20 (21.3%) | – | – | ||
| More than one | 1 (0.4%) | 4 (4.3%) | – | – | ||
| Chlamydia | 10 (4.4%) | 17 (18.1%) | – | <0.001 | – | – |
| Gonorrhea | 2 (0.9%) | 4 (4.3%) | – | 0.06 | – | – |
| Trichomoniasis | 3 (1.3%) | 1 (1.1%) | – | >0.99 | – | – |
| Syphilis | 0 (0.0%) | 2 (2.1%) | – | 0.09 | – | – |
| Pelvic inflammatory disease | 1 (0.4%) | 0 (0.0%) | – | >0.99 | – | – |
| Genital warts | 2 (0.9%) | 0 (0.0%) | – | 0.58 | – | – |
| Genital herpes | 0 (0.0%) | 1 (1.1%) | – | 0.29 | – | – |
| Other | 6 (2.7%) | 3 (3.2%) | – | >0.99 | – | – |
FBHW foreign-born Hispanic women, USBHW US-born Hispanic women, HIV human immunodeficiency virus, STI sexually transmitted infection
FBHW versus USBHW; USBHW are reference group in all ORs
Estimates from model adjusted for current age and education
Table 5.
Partner risk and substance abuse
| Outcome | FBHW n = 226 | USBHW n = 94 | Unadjusted |
Adjustedb |
||
|---|---|---|---|---|---|---|
| ORa | P value | ORa | P value | |||
| Any high risk partner behavior? | 11 (5.6%) | 13 (15.5%) | 0.3 (0.1, 0.8) | 0.009 | 0.4 (0.2, 1.2) | 0.10 |
| Partner had STI in the past year | n = 205 | n = 86 | ||||
| Yes | 5 (2.4%) | 4 (4.7%) | 0.5 (0.1, 2.0) | 0.33 | 0.3 (0.1, 1.6) | 0.17 |
| Yes/I do not know | 24 (11.7%) | 18 (20.9%) | 0.5 (0.3, 1.0) | 0.04 | 0.3 (0.1, 0.7) | 0.006 |
| Partner had other partners, in relationship | n = 210 | n = 83 | ||||
| Yes | 7 (3.3%) | 9 (10.8%) | 0.3 (0.1, 0.8) | 0.016 | 0.5 (0.2, 1.7) | 0.29 |
| Yes/I do not know | 12 (5.7%) | 20 (24.1%) | 0.2 (0.1, 0.4) | <0.001 | 0.2 (0.1, 0.5) | 0.001 |
| Partner had sex with prostitutes? | n = 205 | n = 83 | ||||
| Yes | 0 | 0 | – | – | – | – |
| I do not know | 10 (4.9%) | 6 (7.2%) | 0.7 (0.2, 1.9) | 0.43 | 0.3 (0.1, 1.3) | 0.11 |
| Injected drugs? | n = 206 | n = 83 | ||||
| Yes | 0 (0.0%) | 1 (1.2%) | – | 0.29 | – | – |
| Yes/I do not know | 4 (1.9%) | 4 (4.8%) | – | 0.23 | – | – |
| Confidence in asking partner if he/she has an STI? | n = 204 | n = 83 | ||||
| Comfortable or very comfortable | 189 (92.7%) | 80 (96.4%) | 0.5 (0.1, 1.7) | 0.25 | 0.5 (0.1, 2.1) | 0.38 |
| Ever used or injected drugs | 25 (11.1%) | 23 (24.5%) | 0.4 (0.2, 0.7) | 0.003 | 0.4 (0.2, 0.8) | 0.02 |
| If yes | n = 14 | n = 23 | ||||
| Marijuana | 9 (4.0%) | 13 (13.8%) | – | 0.003 | – | – |
| Cocaine | 4 (1.8%) | 5 (5.3%) | – | 0.13 | – | – |
| Heroine | 1 (0.4%) | 1 (1.1%) | – | >0.99 | – | – |
| Methamphetamine | 0 (0.0%) | 4 (4.3%) | – | 0.007 | – | – |
| Drink alcohol | 44 (21.3%) | 53 (62.4%) | 0.2 (0.1, 0.3) | <0.001 | 0.3 (0.1, 0.5) | <0.001 |
| If yes | n = 42 | n = 49 | ||||
| Three or more drinks in past week | 6 (14.3%) | 8 (16.3%) | 0.9 (0.3, 2.7) | 0.79 | 0.8 (0.2, 3.4) | 0.76 |
| Sex with alcohol/drugs past year | 11 (5.3%) | 24 (28.2%) | 0.1 (0.1, 0.3) | <0.0001 | 0.3 (0.1, 0.6) | 0.002 |
FBHW foreign-born Hispanic women, USBHW US-born Hispanic women, STI sexually transmitted infection
FBHW versus USBHW; USBHW are reference group in all ORs
Estimates from model adjusted for current age and education
Inclusion Criteria
A total of 320 completed questionnaires were included in the analysis (226 FBHW and 94 USBHW). Ten questionnaires were excluded because the participants were younger than 18 years of age, were not sexually active with men within the past year or did not indicate place of birth. The surveys were completed over a period of 6 months at both clinic sites.
Demographic Characteristics
Demographic characteristics are reported in Table 1 for the two groups. FBHW were older and reported attaining lower levels of education. The majority of the USBHW were first generation Hispanics (only 46.8% of their parents were born in the US) and over two-thirds (67.7%) of the FBHW had lived in the US for more than 5 years. Nearly all of the women sampled reported having sex with males only.
Table 1.
Demographic characteristics
| Characteristic | FBHW n = 226 | USBHW n = 94 | P value |
|---|---|---|---|
| Current age: mean ± SD | 29.9 ± 6.25 | 27.6 ± 7.90 | 0.02 |
| Education: n (%) | <0.001 | ||
| Middle school | 108 (48.6%) | 6 (6.4%) | |
| High school | 87 (39.2%) | 52 (55.3%) | |
| College/university/post grad | 27 (12.2%) | 36 (38.3%) | |
| Questionnaire language | <0.001 | ||
| Spanish | 206 (91.2%) | 16 (17.0%) | |
| English | 20 (8.8%) | 78 (83.0%) | |
| Parent born in the US | |||
| Father | 4 (1.8%) | 44 (46.8%) | <0.001 |
| Mother | 4 (1.8%) | 44 (46.8%) | <0.001 |
| Duration lived in the US | <0.001 | ||
| Less than 1 year | 10 (4.4%) | 2 (2.2%) | |
| 1–3 years | 29 (12.8%) | 1 (1.1%) | |
| 3–5 years | 34 (15.0%) | 1 (1.1%) | |
| More than 5 years | 153 (67.7%) | 89 (95.7%) | |
| Has sex with males only | 216 (99.1%) | 84 (97.7%) | 0.58 |
SD standard deviation, FBHW foreign-born Hispanic women, USBHW US-born Hispanic women
Results
Sexual History (Primary Outcomes)
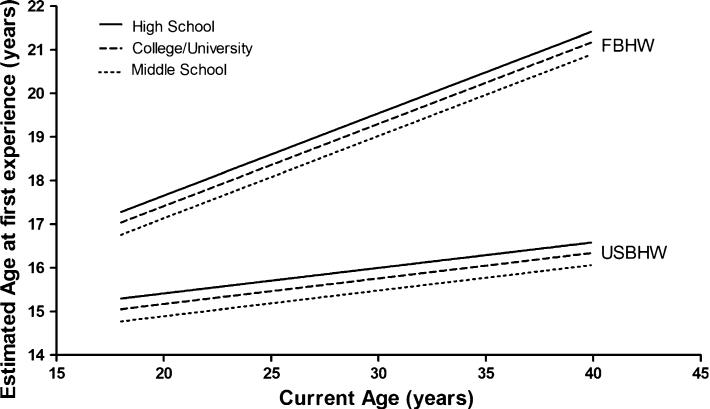
Table 2 shows the differences in sexual history between FBHW and USBHW. FBHW were 3.5 years older (95% CI: 2.8, 4.1) than USBHW at age of first sexual experience. For FBHW, the average age for a first sexual experience was 19.1 years (95% CI: 18.6, 19.6) versus 15.7 years (95% CI: 15.2, 16.1) for USBHW (P < 0.001). After controlling for current age and education this difference remained significant at every observed age in the sample, with a greater difference between FBHW and USBHW who are currently age 40 (4.9 years) than age 20 (2.2 years) (Fig. 1). A significant difference was not observed in the proportion of women with >1 sexual partner in the previous year between FBHW and USBHW (aOR = 2.99 (0.61, 14.76), P = 0.18).
Table 2.
Sexual history
| Outcome | Unadjusted |
Adjusted |
|||
|---|---|---|---|---|---|
| Estimate | P value | Comparison | Estimate | P value | |
| Age at 1st sexual experiencea | |||||
| FBHW | 19.1 (18.6, 19.6) | Difference, age 20 | 2.24 (0.67) | 0.001b | |
| USBHW | 15.7 (15.2, 16.1) | Difference, age 30 | 3.54 (0.51) | <0.001b | |
| FBHW–USBHW (diff) | 3.5 (2.8, 4.1) | <0.001 | Difference, age 40 | 4.85 (0.93) | <0.001b |
| >1 sex partnerc | 0.39 | >1 sex partnerd | 0.18 | ||
| FBHW versus USBHW OR | 1.75 (0.49, 6.31) | FBHW versus USBHW OR | 2.99 (0.61, 14.76) | ||
| FBHW | 6.2% (13/211) | ||||
| USBHW | 3.6% (3/83) | ||||
FBHW foreign-born Hispanic women, USBHW US-born Hispanic women, OR odds ratio
Linear regression
Linear regression including 3-category education and interaction term for current age and region of origin
Exact chi-square test
Odds ratio (95% CI) from logistic regression (age and 3-category education adjusted)
Fig. 1.
Age at first sexual experience comparing FBHW and USBHW. The average age for a first sexual experience was 3.5 years older for FBHW than USBHW (P < 0.001), Table 2. After controlling for education, this difference remained significant at every current age observed within the sample (P values provided in Table 2). Education P value = 0.96. FBHW Foreign-born Hispanic women, USBHW US-born Hispanic women
Birth Control Methods and Condom Use
Table 3 presents a comparison of FBHW and USBHW with respect to number and type of birth control methods and condom use. FBHW did not demonstrate a greater odds than USBHW of using at least one form of birth control [aOR = 1.6 (0.7, 3.5)]; although FBHW had a higher odds of using more than one form of birth control [aOR = 9.9 (4.0, 24.6)]. Oral contraceptives were a more common method of choice for FBHW than for USBHW [aOR = 2.8 (1.3, 6.1)]. At the time of the survey, a greater proportion of USBHW than FBHW (6.4% vs. 0.4%) were trying to get pregnant.
FBHW had higher odds of condom use than USBHW [aOR = 2.2 (1.2, 4.0)], but the proportion of women who had ever asked their male partner(s) to use a condom was similar for both groups [aOR = 1.5 (0.7, 3.2)]. However, only a small proportion of FBHW and USBHW had actually used a condom the last time they had vaginal or anal intercourse (27.7% vs. 16.1%); although FBHW had a higher odds of using a condom at least half of the time [aOR = 3.9 (1.6, 9.4)]. For the women who practiced oral sex, FBHW had a higher odds of using a condom at least some of the time compared to USBHW [aOR = 2.5 (1.1, 5.4)]. Condom rates were similar for women who practiced anal sex as were confidence rates on convincing their male partner(s) to use a condom or in the proportion of women whose partner had ever refused to use a condom. Lastly, USBHW were more likely than FBHW to have had sex at least once in the past without their consent (14.1% vs. 3.8%).
HIV and STI Diagnoses
Table 4 displays results for testing and diagnosis of HIV and STIs. FBHW had lower odds than USBHW to have ever been tested for HIV infection [aOR = 0.3 (0.2, 0.7)]. Of the 93 FBHW and 15 USBHW who had never been tested for HIV, greater than 25% overall thought they did not need to be tested or they did not know where to be tested; only a very small proportion of FBHW reported “fear of the result” as the main reason for not ever having had an HIV test.
FBHW were less likely than USBHW to have had a previous diagnosis of an STI [aOR = 0.3 (0.2, 0.6)] and to have been diagnosed with >1 STI (4.3% vs. 0.4%). Of women with a history of STI diagnosis, there was no significant difference in the duration of time since STI diagnosis between the two groups. Chlamydia infection was more common in USBHW than in FBHW (18.1% vs. 4.4%; P < 0.001). Differences in the rates of other STIs including trichomoniasis, pelvic inflammatory disease, genital HPV and genital herpes were not statistically significant between the two groups.
Partner Risk and Substance Abuse
In Table 5 we present the comparison among FBHW and USBHW regarding sexual partner(s) behavior and substance abuse. FBHW had lower odds than USBHW to have a partner with any high risk behavior, although this difference was not statistically significant [aOR = 0.4 (0.2, 1.2)]. In particular, FBHW had lower odds than USBHW of not knowing or having partner who had other sexual partners while in a relationship with them [aOR = 0.2 (0.1, 0.5)]. Similarly FBHW had lower odds of not knowing or having sex with a partner with an STI in the past year [aOR = 0.3 (0.1, 0.7)]. There were no significant differences in regard to having a partner who, had sex with prostitutes or used injected drugs between the two groups.
FBHW had lower odds of alcohol consumption than USBHW [aOR = 0.3 (0.1, 0.5)]. There was no difference in the odds of consuming more than 3 alcoholic drinks consumed in the previous week. Life time substance abuse was also evaluated among the participants. We observed a trend towards a higher marijuana use in USBHW compared to FBHW (13.8% vs. 4.0%). Methamphetamine use was not reported in FBHW but was reported in 4.3% (4/23) of USBHW. Odds of using or injecting drugs were lower in FBHW than USBHW [aOR = 0.4 (0.2, 0.8)]. Differences in cocaine and heroin abuse were not statistically significant between both groups. FBHW had lower odds of reporting sexual activity under the influence of alcohol or drugs within the last year [aOR = 0.3 (0.1, 0.6)].
Discussion
The HIV-1/STI risk profile of Hispanics and other minority groups in the US does not currently differentiate between foreign-born and US-born individuals, rendering those groups indistinguishable with respect to public health indicators. Our study was aimed at identifying differences in HIV-1/AIDS risk factors and sexual risk behavior among Hispanic women according to their place of birth. As a primary outcome we analyzed the age at first sexual encounter, as this has been associated with an increased risk of HIV infection in women from different social and ethnic compositions [19, 20]. The results of our study demonstrated that FBHW initiate sexual activity at an older age compared to their US-born peers. Although our findings reflect the behavior of a specific urban population in the Greater Denver Metropolitan Area, these results are consistent with other studies that have shown a delayed sexual initiation in Hispanic women as a group [21] and in foreign-born Hispanic teenage girls in particular [22, 23]. However, this difference has not been previously documented in the adult female Hispanic population taking into consideration their place of birth. This “protective” effect in sexual risk can be attributed to cultural factors and to a more traditional family structure and a stronger social support among the Hispanic community. Nevertheless, not all data available to date support the theory of a delayed sexual initiation among FBHW. A study comparing US-born and foreign-born Dominican teenagers showed earlier initiation of sexual practices among Dominican youth living on the island [24]. This serves as an example of the conflicting information available on the sexual risk behavior and the heterogeneity of sexual practices within a minority group in the US, a topic that warrants additional investigation.
Condom use was not significantly different among FBHW and USBHW in our survey. Previous studies have documented a similar incidence in condom use between Hispanics and blacks [25], but there is limited information that has shown that US-born women are more likely to use or intend-to-use condoms than foreign-born women [26] and no studies to date have evaluated this practice among Hispanic immigrant women in the US. Although a different ethnic group, our findings are contrary to what Hoffman et al. reported among Caribbean-born and US-born blacks. In their study, foreign-born blacks had less favorable attitudes toward condom use than US-born blacks, and they were also less likely to intend to always use condoms with their sexual partners [13]. This difference could be explained by cultural beliefs and social acceptance of condom use among blacks and Hispanics, which reflects the need for ethnicity-oriented interventions in minority groups aimed at preventing HIV-1 infection and other STIs.
Similar to condom use, oral and anal sexual practices were similar in both groups in our survey, but their frequency was greater than what would have been expected [26, 27]. Hispanic women have been reported to engage in oral sex at twice the rate of African American women and in anal sex at nearly three times the rate of African American and white women [27]. This proportion remains significant when FBHW are evaluated as an individual group [28]; however, this was not observed in our study. Similarly, we did not find a difference in the proportion of women with >1 sexual partner in the last year among FBHW and USBHW. A possible explanation for these findings could be due to the fact that the majority of our FBHW population (67.7%) had been living in the US for more than 5 years, which could categorize them as an acculturated population according to previously published acculturation scales [29]. It is well known that acculturation has a direct influence on the sexual behaviors of foreign-born individuals and that highly acculturated women can modify their ethnically-inherent protective sexual practices and report more sexual partners, a higher incidence of STIs and riskier behavior than are less acculturated women [30–32].
Another example of the influence of acculturation in our sample was a higher than expected frequency of oral contraceptive use in the FBHW. Several studies performed in the US have found that Hispanic women in general, and FBHW in particular, use oral contraceptives at a lower rate when compared to White women [19, 33–35]. In addition, oral contraceptive use in rural Mexico (where most of the FBHW population coming to the US originates from) is still considered a “sin” with a risk for infertility and long-term sequelae [36]. However, some studies have demonstrated a trend towards a greater acceptance and awareness of oral contraceptives in second and third generations of Hispanic women in the US [37, 38]. Therefore, we believe that acculturation could explain the increased frequency of oral contraceptive use among FBHW in our sample.
HIV testing was also evaluated in our survey. It has been previously documented that Hispanic women are less frequently tested for HIV infection when compared to women of other ethnicities [39]. An evident finding in our study was the difference in HIV testing between FBHW and USBHW, which has been documented in adolescents but not in adult Hispanic women [39]. A possible explanation for this difference could be a theoretical advantage that USBHW may have over FBHW in terms of access to medical and preventive care. This theory is partially supported by a noticeable trend in the lack of healthcare coverage found in our FBHW population since a larger proportion of these women answered “I do not have health insurance” as the main reason for not being tested for HIV. In this context, a surprising finding in our survey was that a higher proportion of USBHW responded “I do not know where to get tested” as the main reason why they had never had an HIV test. Although unexpected for a population born in the US, this finding reflects the limited effect that the current HIV testing strategies exert within the Hispanic community in this country, particularly among women.
The incidence of previous STI among our USBHW population was higher when compared to the FBHW, as were the number of events for those women with a previous STI diagnosis. This is consistent with previous reports that show marked differences on STI prevalence between US-born and foreign-born minorities, including Hispanics [40, 41]. As an example, the higher frequency of Chlamydia infection observed among the USBHW in our study could simply be explained by the relatively better access to medical care, diagnosis and treatment that USBHW have over FBHW. On the other hand, this could also be explained on the basis of behavioral differences among these groups. It is well known that Hispanics tend to choose sexual partners based on ethnic similarities and geographic proximity [42]. Sexual partner selection may lead to a relatively closed sexual network and be protective against STIs, especially if the prevalence of STIs in the Hispanic community is lower than in the surrounding communities [41]. However, this protective effect may dilute as acculturation ensues. US-born Hispanic adults (including USBHW) are usually more independent and autonomous than foreign-born Hispanic adults, and thus are more likely to move outside of a predominantly Hispanic neighborhood and create ethnically discordant sexual partnerships, which have been associated with an increased risk of STIs [43, 44]. This phenomenon illustrates how protective sexual behaviors, such as partner selection, can be negatively modified as foreign-born minorities and their descendants resemble the US population. Conversely, it is also a clear example of how a proven risk factor for the acquisition of HIV-1, such as concomitant Chlamydia infection, can be positively modified as access to care improves for the US-born minorities.
In our study, alcohol use, drug abuse and sexual activity while intoxicated were less frequently observed in FBHW when compared to USBHW, which is consistent with what has been previously reported in the literature [40, 45–47]. These differences can be explained by the social and environmental influences that USBHW face during their formative years and increase their exposure to drugs and alcohol. US-born minority youth may acquire some harmful behaviors from second or third generation Hispanics and from non-Hispanic peers and adopt some pro-drug attitudes that are unfamiliar to their immigrant parents. As a result of this generational detachment, a cultural gap can emerge between parent and child, which will ultimately challenge the parents’ ability to influence the child's behavior [48]. In contrast, most FBHW come from very strict and hierarchal families where drugs and alcohol are seldom available to women. In these relatively protected communities, experimenting with alcohol drugs is severely punished and their consumption still has a very low level of social acceptance among the female immigrant community, regardless of their level of acculturation [49].
Our survey has some limitations. Self-administered sexual health surveys have an inherent risk of reporting bias, communication barriers and disclosure of risk behaviors [50]. In addition, we evaluated a relatively small sample in a single metropolitan area with a suspected low risk of HIV/STI. Applying this survey to a population at risk (i.e. STI clinic attendee) could provide interesting results, but may minimize the existing differences among USBHW and FBHW. Patients attending STI clinics are not a representative sample of the general population, which was the main target of our study. Although our results require caution when generalized, we do believe that they dissect some of the differences in sexual risk behavior that exist between FBHW and USBHW.
Conclusions
In this study we evaluated the differences in sexual risk behavior and HIV-1 risk factors among a population of Hispanic women according to their place of birth (US vs. foreign-born). We found evidence that FBHW and USBHW have identifiable differences in sexual risk behavior and HIV-1/STI risk factors. Among FBHW, some protective behaviors may decrease their risk for acquiring an STI and HIV-1. In the other hand, USBHW seem to have an advantage over FBHW in terms of HIV testing and access to care. Future minority sexual risk behavior research must take into consideration the unique characteristics that exist in foreign-born individuals and future prevention strategies in the US should be tailored to meet the needs of this vulnerable population.
Acknowledgments
The present study was supported by the University of Colorado Center for AIDS Research (CFAR) and the National Institutes of Health under the grant NIH P30 AI054907. Also, support in part came from the NIH/NCRR Colorado CTSI Grant Number UL1 RR025780. Contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Contributor Information
Jose Castillo-Mancilla, Division of Infectious Diseases, School of Medicine, University of Colorado Denver, 1635 Aurora Ct, B163, Aurora, CO 80045, USA.
Amanda Allshouse, Department of Biostatistics, School of Public Health, University of Colorado Denver, 13001 E. 17th Pl, B119, Aurora, CO 80045, USA.
Caitilin Collins, College of Nursing, University of Colorado Denver, 13120 E. 19th Ave, C288-6, Aurora, CO 80045, USA.
Marie Hastings-Tolsma, College of Nursing, University of Colorado Denver, 13120 E. 19th Ave, C288-6, Aurora, CO 80045, USA.
Thomas B. Campbell, Division of Infectious Diseases, School of Medicine, University of Colorado Denver, 1635 Aurora Ct, B163, Aurora, CO 80045, USA
Samantha MaWhinney, Department of Biostatistics, School of Public Health, University of Colorado Denver, 13001 E. 17th Pl, B119, Aurora, CO 80045, USA.
References
- 1.United States Census Bureau [16 Feb 2011];Public information office. 2008 Aug 14; Available from www.census.gov/newsroom/releases/archives/population/cb08-123.html.
- 2.United States Census Bureau . Statistical abstract of the United States: 2011. 130th Edition. Washington, DC: 2010. [8 June 2011]. Available from www.census.gov/prod/2011pubs/11statab/pop.pdf. [Google Scholar]
- 3.Espinoza L, Hall HI, Selik RM, Hu X. Characteristics of HIV infection among Hispanics, United States 2003–2006. J Acquir Immune Defic Syndr. 2008;49(1):94–101. doi: 10.1097/QAI.0b013e3181820129. [DOI] [PubMed] [Google Scholar]
- 4.CDC. HIV surveillance report. Vol. 21. US DHHS, CDC; Atlanta, GA: 2010. [8 June 2011]. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2009. Available from www.cdc.gov/hiv/surveillance/resources/reports/2009report/index.htm. [Google Scholar]
- 5.Hall HI, Song R, Rhodes P, Prejean J, Qian A, Lee L, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. [8 June 2011];HIV surveillance in women. 2011 Available from www.cdc.gov/hiv/topics/surveillance/resources/slides/women/slides/Women.pdf.
- 7.Deane KD, Parkhurst JO, Johnston D. Linking migration, mobility and HIV. Trop Med Int Health. 2010;15(12):1458–63. doi: 10.1111/j.1365-3156.2010.02647.x. [DOI] [PubMed] [Google Scholar]
- 8.Bronfman M, Campos-Ortega S, Medina H. La migración inter-nacional y el SIDA: el caso de México y Estados Unidos. In: Sepulveda J, Bronfman M, Ruiz PG, et al., editors. SIDA, ciencia y sociedad en México. Secretaria de Salud and Fondo de Cultura Económica; México DF, México: 1989. pp. 435–56. [Google Scholar]
- 9.Organista KC, Organista PB. Migrant laborers and AIDS in the United States: a review of the literature. AIDS Educ Prev. 1997;9:83–93. [PubMed] [Google Scholar]
- 10.Magis-Rodriguez C, Lemp G, Hernandez MT, Sanchez MA, Estrada F, Bravo-Garcia E. Going North: Mexican migrants and their vulnerability to HIV. J Acquir Immune Defic Syndr. 2009;51:S21–5. doi: 10.1097/QAI.0b013e3181a26433. [DOI] [PubMed] [Google Scholar]
- 11.Hirsch JS, Higgins J, Bentley ME, Nathanson CA. The social constructions of sexuality: marital infidelity and sexually transmitted disease-HIV risk in a Mexican migrant community. Am J Public Health. 2002;92(8):1227–37. doi: 10.2105/ajph.92.8.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loue S. Preventing HIV, eliminating disparities among Hispanics in the United States. J Immigr Minor Health. 2006;8(4):313–8. doi: 10.1007/s10903-006-9001-2. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman S, Beckford Jarrett ST, Augenbraun M, Bylander KE, Mantell JE, Wilson TE. HIV and sexually transmitted infection risk behaviors and beliefs among Black West Indian immigrants and US-born Blacks. Am J Public Health. 2008;98(5):2042–50. doi: 10.2105/AJPH.2006.106443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rios-Ellis B, Frates J, D'Anna LH, Dwyer M, Lopez-Zetina J, Ugarte C. Addressing the need for access to culturally and linguistically appropriate HIV/AIDS prevention for Latinos. J Immigr Minor Health. 2008;10(5):445–60. doi: 10.1007/s10903-007-9105-3. [DOI] [PubMed] [Google Scholar]
- 15.Giuliano AR, Papenfuss M, Schneider A, Nour M, Hatch K. Risk factors for high-risk type human papillomavirus infection among Mexican-American women. Cancer Epidemiol Biomarkers Prev. 1999;8(7):615–20. [PubMed] [Google Scholar]
- 16.Association of Medical Directors of Information Systems and The Improve-IT Institute Comprehension and reading level. [6 July 2011];The informatics review. 2008 Sep 1;11(16) Available from www.informatics-review.com/FAQ/reading.html. [Google Scholar]
- 17.Agresti A. A survey of exact inference for contingency tables. Stat Sci. 1992;7(1):131–53. [Google Scholar]
- 18. [28 Aug 2011];SAS/Stat® 9.22 User's Guide. Available from www.support.sas.com/documentation/cdl/en/statug/63347/HTML/default/viewer.htm#statug_freq_a0000000658.htm.
- 19.Greenberg J, Magder L, Aral S. Age at first coitus. A marker for risky sexual behavior in women. Sex Transm Dis. 1992;19(6):331–4. [PubMed] [Google Scholar]
- 20.Duncan ME, Tibaux G, Pelzer A, Reimann K, Peutherer JF, Simmonds P, et al. First coitus before menarche and risk of sexually transmitted disease. Lancet. 1990;335(8685):338–40. doi: 10.1016/0140-6736(90)90617-e. [DOI] [PubMed] [Google Scholar]
- 21.Upchurch DM, Levy-Storms L, Sucoff CA, Aneshensel CS. Gender and ethnic differences in the timing of first sexual intercourse. Fam Plann Perspect. 1998;30(3):121–7. [PubMed] [Google Scholar]
- 22.Brindis C, Wolfe A, McCarter V, Ball S, Starbuck-Morales S. The associations between immigrant status and risk-behavior patterns in Latino adolescents. J Adolesc Health. 1995;17(2):99–105. doi: 10.1016/1054-139X(94)00101-J. [DOI] [PubMed] [Google Scholar]
- 23.Minnis AM, Padian NS. Reproductive health differences among Latin American- and US-born young women. J Urban Health. 2001;78(4):627–37. doi: 10.1093/jurban/78.4.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Westhoff WW, McDermott RJ, Holcomb DR. HIV risk behaviors: a comparison of U.S. Hispanic and Dominican Republic youth. AIDS Educ Prev. 1996;8(2):106–14. [PubMed] [Google Scholar]
- 25.Dodge B, Reece M, Herbenick D, Schick V, Sanders SA, Fortenberry JD. Sexual health among U.S. black and Hispanic men and women: a nationally representative study. J Sex Med. 2010;7(Suppl 5):330–45. doi: 10.1111/j.1743-6109.2010.02019.x. [DOI] [PubMed] [Google Scholar]
- 26.Upchurch DM, Kusunoki Y, Simon P, Doty MM. Sexual behavior and condom practices among Los Angeles women. Womens Health Issues. 2003;13(1):8–15. doi: 10.1016/s1049-3867(02)00175-5. [DOI] [PubMed] [Google Scholar]
- 27.Quadagno D, Sly DF, Harrison DF, Eberstein IW, Soler HR. Ethnic differences in sexual decisions and sexual behavior. Arch Sex Behav. 1998;27(1):57–75. doi: 10.1023/a:1018657825068. [DOI] [PubMed] [Google Scholar]
- 28.Dixon D, Peters M, Saul J. HIV sexual risk behavior among Puerto Rican women. Health Care Women Int. 2003;24(6):529–43. doi: 10.1080/07399330390199401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rogler LH, Cortes DE, Malgady RG. Acculturation and mental health status among Hispanics. Convergence and new directions for research. Am Psychol. 1991;46(6):585–97. doi: 10.1037//0003-066x.46.6.585. [DOI] [PubMed] [Google Scholar]
- 30.Van Oss Marin B, Gomez CL. HIV disease‘ and culture: strategies for HIV prevention. In: Cohen P, Sande M, Volberding P, editors. The AIDS knowledge base. Little Brown; New York: 1994. pp. 10.8–1. [Google Scholar]
- 31.Lee J, Hahm HC. Acculturation and sexual risk behaviors among Latina adolescents transitioning to young adulthood. J Youth Adolesc. 2010;39(4):414–27. doi: 10.1007/s10964-009-9495-8. [DOI] [PubMed] [Google Scholar]
- 32.Kinsler JJ, Lee SJ, Sayles JN, Newman PA, Diamant A, Cunningham W. The impact of acculturation on utilization of HIV prevention services and access to care among an at-risk Hispanic population. J Health Care Poor Underserved. 2009;20(4):996–1011. doi: 10.1353/hpu.0.0204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74(2):125–32. doi: 10.1016/j.contraception.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 34.Guendelman S, Denny C, Mauldon J, Chetcovitch C. Perceptions of hormonal contraceptive safety and side effects among low-income Latina and non-Latina women. Matern Child Health J. 2000;4(4):233–9. doi: 10.1023/a:1026643621387. [DOI] [PubMed] [Google Scholar]
- 35.Frost J, Darroch J. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sexual Reprod Health. 2008;40(2):94–104. doi: 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 36.Hirsch JS. Catholics using contraceptives: religion, family planning, and interpretive agency in rural Mexico. Stud Fam Plann. 2008;39(2):93–104. doi: 10.1111/j.1728-4465.2008.00156.x. [DOI] [PubMed] [Google Scholar]
- 37.Wilson EK. Differences in contraceptive use across generations of migration among women of Mexican origin. Matern Child Health J. 2009;13(5):641–51. doi: 10.1007/s10995-008-0382-9. [DOI] [PubMed] [Google Scholar]
- 38.Ward KK, Roncancio AM, Berenson AB. Cultural adaptation among Hispanic women as related to awareness and acquisition of emergency contraception. Contraception. 2010;82(6):534. doi: 10.1016/j.contraception.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hahm HC, Song IH, Ozonoff A, Sassani JC. HIV testing among sexually experienced Asian and Pacific Islander young women association with routine gynecologic care. Womens Health Issues. 2009;19(4):279–88. doi: 10.1016/j.whi.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harawa NT, Bingham TA, Cochran SD, Greenland S, Cunningham WE. HIV prevalence among foreign- and US-born clients of public STD clinics. Am J Public Health. 2002;92(12):1958–63. doi: 10.2105/ajph.92.12.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gindi RM, Erbelding EJ, Page KR. Sexually transmitted infection prevalence and behavioral risk factors among Latino and non-Latino patients attending the Baltimore City STD clinics. Sex Transm Dis. 2010;37(3):191–6. doi: 10.1097/OLQ.0b013e3181bf55a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zenilman JM, Ellish N, Fresia A, et al. The geography of sexual partnerships in Baltimore: applications of core theory dynamics using a geographic information system. Sex Transm Dis. 1999;26(2):75–81. doi: 10.1097/00007435-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Aral SO, Hughes JP, Stoner B, et al. Sexual mixing patterns in the spread of gonococcal and chlamydial infections. Am J Public Health. 1999;89(6):825–33. doi: 10.2105/ajph.89.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gorbach PM, Drumright LN, Holmes KK. Discord, discordance, and concurrency: comparing individual and partnership-level analyses of new partnerships of young adults at risk of sexually transmitted infections. Sex Transm Dis. 2005;32(1):7–12. doi: 10.1097/01.olq.0000148302.81575.fc. [DOI] [PubMed] [Google Scholar]
- 45.Hennessy-Burt TE, Stoecklin-Marois MT, Meneses-González F, Schenker MB. A pilot binational study of health behaviors and immigration. J Immigr Minor Health. doi: 10.1007/s10903-010-9387-8. Online FirstTM, 2 Sep 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lindenberg CS, Strickland O, Solorzano R, Galvis C, Dreher M, Darrow VC. Correlates of alcohol and drug use among low-income Hispanic immigrant childbearing women living in the USA. Int J Nurs Stud. 1999;36(1):3–11. doi: 10.1016/s0020-7489(98)00046-7. [DOI] [PubMed] [Google Scholar]
- 47.Vega WA, Kolody B, Hwang J, Noble A, Porter PA. Perinatal drug use among immigrant and native-born Latinas. Subst Use Misuse. 1997;32(1):43–62. doi: 10.3109/10826089709027296. [DOI] [PubMed] [Google Scholar]
- 48.Marsiglia FF, Kulis S, Luengo MA, Nieri T, Villar P. Immigrant advantage? Substance use among Latin American immigrant and native-born youth in Spain. Ethn Health. 2008;13(2):149–70. doi: 10.1080/13557850701830356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xaverius PK, Salas J, Tenkku LE. Preconception wellness: differences in health by immigrant status. J Immigr Minor Health. 2010 doi: 10.1007/s10903-010-9424-7. Online FirstTM, 16 Dec 2010. [DOI] [PubMed] [Google Scholar]
- 50.Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108(3):339–62. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]