Abstract
Objectives. We sought to understand more about women affected by a law enacted in January 2013 that led Georgia providers to stop providing abortion services at 24 weeks from a woman’s last menstrual period (LMP), and who would be affected if Georgia enforces the law banning abortions at 22 weeks from LMP.
Methods. We obtained data on women obtaining abortions at or after 20 weeks from LMP in 2012 and 2013 from 4 Georgia facilities providing later abortion care. We analyzed data descriptively and with the χ2 test.
Results. More than half of the women were Black; one fourth were White. Close to half of the women had education beyond high school and a similar proportion had a previous live birth. Eighty-three percent of women at or after 24 weeks came from the South, 4% from the Northeast, and 13% from the Midwest; 99% of those at 20 to 24 weeks were from the South. One third of women at or after 24 weeks and half at 20 to 24 weeks were Georgia residents.
Conclusions. These bans will likely affect women throughout the South, as well as the Midwest and Northeast.
In May 2012, the Georgia governor signed a “20-week” abortion ban. Georgia was the 10th state to pass a 20-week ban.1 However, it was the first state to impose such a ban where a considerable number of abortions after 20 weeks were being provided.2 In 2009, 9% of all abortions performed after 21 weeks in the United States were performed in Georgia2 (estimate based on the assumption that the later abortions reported to the Centers for Disease Control and Prevention represent two thirds of later abortions in the United States3), whereas fewer than 5% of all abortions after 21 weeks had been performed in the other states in which 20-week bans were subsequently enacted before Georgia’s ban. Although Georgia’s ban has been referred to as a 20-week ban, it actually bans abortion providers from performing abortions starting at 22 weeks from a woman’s last menstrual period (LMP).4 Thus, we refer to Georgia’s ban as a 22-week ban in the rest of this article.
Before 2013, abortion care was available in Georgia up to 26 weeks and was available after that gestation with exceptions for women’s health.3,5 Georgia’s 22-week ban has been partially blocked by a court order on a preliminary basis.6 However, part of the law went into effect on January 1, 2013.6 As a way to comply with the part of the law that went into effect, abortion providers in Georgia have generally stopped providing abortion care starting at 24 weeks from LMP,3,7 with very limited exceptions for certain types of fetal anomalies and very limited exceptions for maternal health.5 If the preliminary block on the rest of the 22-week ban is lifted, Georgia will begin banning abortions starting at 22 weeks from LMP with extremely limited exceptions.
In addition to the considerable number of abortions after 22 weeks provided in Georgia, Georgia’s 22-week ban is important to consider because Georgia and Florida are the only states in the Southeast (south of Maryland and east of Colorado) where abortion care starting at 22 weeks from LMP for reasons other than fetal anomalies is available.3 Georgia’s ban that went into effect in January 2013 effectively eliminated all abortion care starting at 24 weeks from LMP in the entire Southeast, with few exceptions.3 Thus, it is important to understand more about the women affected by the part of the ban that Georgia started enforcing in January 2013, and the women who would be affected if Georgia is allowed to enforce the entire 22-week ban.
METHODS
We sought to identify abortion facilities in Georgia that were providing services that would be affected by the ban. We first contacted a facility with which colleagues had collaborated previously. We asked about services at their facility and knowledge of other facilities providing abortion care after 22 weeks. Through this word-of-mouth process and online searches, we identified 5 Georgia outpatient abortion facilities that were providing care at or after 22 weeks in 2012. We also learned that some hospitals perform these procedures, but that these are uncommon. All of the outpatient facilities were located in Atlanta. Four of the 5 facilities identified agreed to work with us.
We obtained data on all abortions at or after 20 weeks from LMP in 2012 and 2013 from 4 of the 5 facilities. Neither the part of the ban that took effect in January 2013 nor the entire 22-week ban restricts abortion care between 20 and 22 weeks from LMP. However, we also collected data on these abortions to compare populations of women already and potentially affected to a population not directly affected by the restriction. The state of Georgia requires providers to complete Induced Termination of Pregnancy forms for each abortion they provide and to submit these data to the Georgia Department of Public Health. A University of California, San Francisco, research assistant abstracted de-identified data from copies of Induced Termination of Pregnancy forms that the 4 facilities had retained for their own records.
Measures included year of abortion, age (as 13–19, 20–24, 25–34, or 35–49 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, or other), education (less than high school, high school, some college, or college), marital status (single, never married; married; or divorced, separated, or widowed), parity (nulliparous or 1, 2, or 3 or more previous children), weeks’ gestation category (20 weeks to < 22 weeks from LMP; 22 weeks to < 24 weeks from LMP; 24 or more weeks from LMP; based on clinical estimate of gestation), state (state of residence at the time of abortion seeking), Georgia resident (a dichotomous variable of whether the woman was a resident of Georgia at the time of abortion seeking), and region (Pacific, Midwest, South, Northeast, based on census regions8).
Analyses were primarily descriptive, describing demographic, geographic, and pregnancy-related characteristics of women having an abortion at 20 weeks or later in Georgia. We compared differences across groups with the χ2 test. When the χ2 test indicated overall differences, we followed up with logistic regression for year and multinomial logistic regression for weeks’ gestation comparisons. For year comparisons, 2012 is the reference; for weeks’ gestation comparisons, 20 to 22 weeks is the reference. We dropped missing cases from statistical comparisons; when more than 5% of cases were missing data for a variable, we noted this in a footnote in Table 1. We considered differences at P < .05 statistically significant. We conducted all analyses in Stata version 13.0 (StataCorp LP, College Station, TX).
TABLE 1—
Characteristics of Women Having an Abortion at or After 20 Weeks by Weeks From Last Menstrual Period: Georgia, 2012 and 2013
| Characteristics | Total (n = 2027), No. (%) | 20 to < 22 Weeks (n = 851), No. (%) | 22 to < 24 Weeks (n = 783), No. (%) | ≥ 24 Weeks (n = 393),a No. (%) | Pb |
| Age, y | .176 | ||||
| 13–19 | 416 (21) | 157 (19) | 164 (21) | 95 (24) | |
| 20–24 | 646 (32) | 262 (31) | 258 (33) | 126 (32) | |
| 25–34 | 715 (36) | 316 (37) | 271 (35) | 128 (33) | |
| 35–49 | 233 (12) | 109 (13) | 83 (11) | 41 (22) | |
| Race/ethnicity | .374 | ||||
| White | 540 (27) | 214 (25) | 211 (27) | 115 (29) | |
| Black | 1114 (55) | 469 (55) | 440 (56) | 205 (52) | |
| Hispanic | 134 (7) | 64 (8) | 41 (5) | 29 (7) | |
| Other | 239 (12) | 104 (12) | 91 (12) | 44 (11) | |
| Educationc | .119 | ||||
| < high school | 370 (19) | 152 (19) | 141 (19) | 77 (20) | |
| High school | 684 (36) | 297 (38) | 274 (37) | 113 (30) | |
| Some college | 558 (29) | 221 (28) | 206 (28) | 131 (34) | |
| College graduate | 302 (16) | 120 (15) | 123 (17) | 59 (16) | |
| Parity | .001 | ||||
| Nulliparous | 926 (46) | 340 (41) | 381 (49; Ref) | 205 (53; Ref) | |
| 1 | 497 (25) | 229 (27) | 175** (23) | 93** (24) | |
| 2 | 320 (16) | 146 (17) | 120* (16) | 54** (14) | |
| ≥ 3 | 256 (13) | 123 (15) | 95* (12) | 38** (10) | |
| Marital statusd | .247 | ||||
| Single, never married | 1469 (79) | 604 (77) | 579 (81) | 286 (81) | |
| Married | 237 (13) | 116 (15) | 79 (11) | 42 (12) | |
| Divorced, separated, widowed | 148 (8) | 65 (8) | 56 (8) | 27 (8) | |
| Georgia resident | |||||
| Yes | 1011 (50) | 491 (58) | 378 (49) | 142 (37) | < .001 |
| No | 1002 (50) | 355 (42) | 400 (51) | 247 (64) | |
| Region | |||||
| South | 1932 (96) | 842 (100) | 769 (99) | 321 (83; Ref) | < .001 |
| Pacific | 2 (< 1) | 1 (< 1) | 0 (0) | 1 (< 1) | |
| Midwest | 62 (3) | 3 (< 1) | 8 (1) | 51*** (13) | |
| Northeast | 17 (1) | 0 (0) | 1 (< 1) | 16 (4) |
Note. Neither the part of the ban that took effect in January 2013, nor the entire 20-week ban, restricted abortion care between 20 and 22 weeks from last menstrual period. However, we also collected data on these abortions to be able to compare populations of women already—and potentially—affected to a population not currently directly affected by the restriction. Percentages might not add to 100 because of rounding.
In 2012, abortion up to 26 weeks,3 with a health exception after 26 weeks, was available; in 2013, abortion starting at 24 weeks from last menstrual period was limited to a very narrow fetal anomaly or health exception.
For global χ2 test.
Missing is 6% for education and 9% for marital status. The categories were excluded from statistical testing.
*P < .05; **P < .01; ***P < .001.
RESULTS
We obtained data on 2027 women who had an abortion at or after 20 weeks from LMP in Georgia in 2012 or 2013. About two fifths received abortions between 20 and less than 22 weeks and another two fifths between 22 and less than 24 weeks, with one fifth at 24 or more weeks from LMP. About one third of women having an abortion at or after 20 weeks in Georgia in 2012 or 2013 were aged between 20 and 24 years, and one third were aged between 25 and 34 years, with slightly fewer adolescents and women aged 35 years and older (Table 1). More than half were Black, with about one fourth White, 7% Hispanic, and 12% other race/ethnicity. Fewer than half had education beyond high school. More than three fourths were single, and about 13% were married. A little less than half had not had a previous live birth, with one fourth having had 1 previous live birth. The only statistically significant difference found by gestation category was parity. Fewer women having an abortion between 22 and less than 24 and 24 or more weeks than 20 to less than 22 weeks had had a previous live birth (Table 1).
Changes From 2012 to 2013
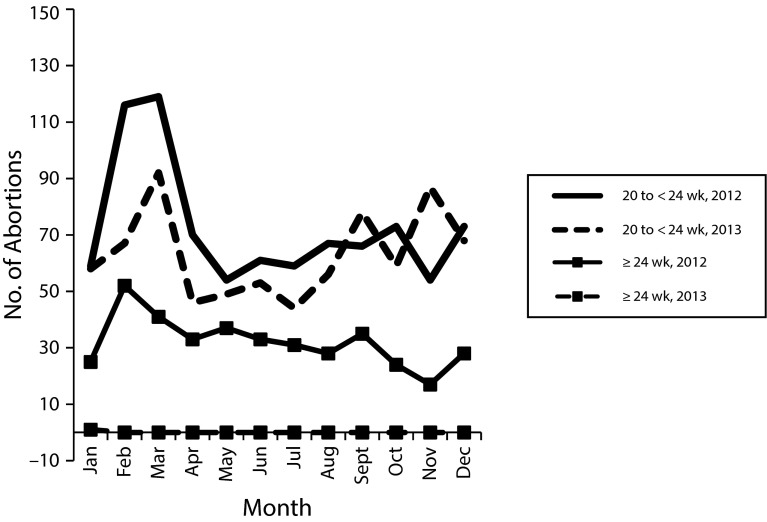
There were 1269 abortions at or after 20 weeks from LMP in Georgia in 2012 and 758 in 2013, representing a difference of 511 or a reduction of 40%. Not all of this reduction was in abortions at 24 or more weeks from LMP; there were 119 fewer abortions between 20 and less than 24 weeks after LMP in 2013 than in 2012. The decrease in abortions at 24 or more weeks was sudden in January 2013; the decrease in abortions 20 to less than 24 weeks was concentrated in the first few months of 2013 (Figure 1).
FIGURE 1—
Abortions at or after 20 weeks from last menstrual period in Georgia by month: 2012 and 2013.
Fewer Hispanic women and fewer women with less than high-school education had an abortion in Georgia in 2012 versus 2013 (P < .05 and P < .01, respectively; Table 2).
TABLE 2—
Characteristics of Women Having an Abortion at or After 20 Weeks From Last Menstrual Period by Year: Georgia, 2012 and 2013
| Characteristics | Total, No. (%) | 2012 (n = 1269), No. (%) | 2013 (n = 758), No. (%) | Pa |
| Age, y | .068 | |||
| 13–19 | 416 (21) | 262 (21) | 154 (21) | |
| 20–24 | 646 (32) | 429 (34) | 217 (29) | |
| 25–34 | 715 (36) | 435 (35) | 280 (37) | |
| 35–49 | 233 (12) | 135 (11) | 98 (13) | |
| Race/ethnicity | .001 | |||
| White | 540 (27) | 345 (27) | 195 (26; Ref) | |
| Black | 1114 (55) | 663 (52) | 451 (60) | |
| Hispanic | 134 (7) | 101 (8) | 33* (4) | |
| Other | 239 (12) | 160 (13) | 79 (10) | |
| Educationb | .005 | |||
| < high school | 370 (19) | 251 (21) | 119 (16; Ref) | |
| High school | 684 (36) | 391 (33) | 293** (40) | |
| Some college | 558 (29) | 354 (30) | 204 (28) | |
| College graduate | 302 (16) | 191 (16) | 111 (15) | |
| Parity | .236 | |||
| Nulliparous | 926 (46) | 588 (47) | 338 (45) | |
| 1 | 497 (25) | 315 (25) | 182 (24) | |
| 2 | 320 (16) | 206 (16) | 114 (15) | |
| ≥ 3 | 256 (13) | 146 (12) | 110 (15) | |
| Marital statusb | .331 | |||
| Single, never married | 1469 (79) | 893 (78) | 576 (81) | |
| Married | 237 (13) | 156 (14) | 81 (11) | |
| Divorced, separated, widowed | 148 (8) | 92 (8) | 56 (8) | |
| Weeks after last menstrual period | .602c | |||
| 20 to < 22c | 851 (42) | 462 (36) | 389 (51) | |
| 22 to < 24 | 783 (39) | 415 (33) | 368 (49) | |
| ≥ 24d,e | 393 (19) | 392 (31) | 1 (< 1) | |
| Georgia resident | .055 | |||
| Yes | 1002 (50) | 614 (49) | 397 (53) | |
| No | 1016 (50) | 650 (51) | 352 (47) | |
| Region | < .001 | |||
| South | 1932 (96) | 1186 (94) | 746 (100; Ref) | |
| Pacific | 2 (< 1) | 1 (< 1) | 1 (< 1) | |
| Midwest | 62 (3) | 61 (5) | 1*** (< 1) | |
| Northeast | 17 (1) | 16 (1) | 1* (< 1) |
Note. Neither the part of the ban that took effect in January 2013, nor the entire 20-week ban, restricted abortion care between 20 and 22 weeks from last menstrual period. However, we also collected data on these abortions to be able to compare populations of women already—and potentially—affected to a population not currently directly affected by the restriction. Percentages might not add to 100 because of rounding.
For global χ2 test.
Missing is 6% for education and 9% for marital status. The categories were excluded from statistical testing.
Of the 462 in 2012, there were 223 between 21 and < 22 weeks, for a total of 1030 abortions in 2012 at ≥ 21 weeks.
In 2012, abortion up to 26 weeks,3 with a health exception after 26 weeks, was available; in 2013, abortion starting at 24 weeks from last menstrual period was limited to a very narrow fetal anomaly or health exception.
χ2 test drops ≥ 24 weeks from last menstrual period because of the 2013 cell size. Our interest is in the changes in lower weeks’ gestation.
*P < .05; **P < .01; ***P < .001.
State and Region of Residence
In our sample, one half of women having an abortion in Georgia at or after 20 weeks from LMP in 2012 or 2013 were residents of Georgia (Table 1). Fewer women having abortions later in pregnancy were Georgia residents—22 to less than 24 weeks and at 24 or more weeks—than women having abortions at 20 to less than 22 weeks (P < .001). Most (96%) women were from the South. Region of residence differed by weeks’ gestation, with fewer women from the South and more women from the Midwest among women having an abortion at 24 or more weeks versus 20 to 22 weeks from LMP (P < .001; Table 1). Region of residence also differed between 2012 and 2013; fewer women from the Midwest and Northeast had an abortion at or after 20 weeks in Georgia in 2013 than 2012 (P < .001 and P < .05, respectively; Table 2).
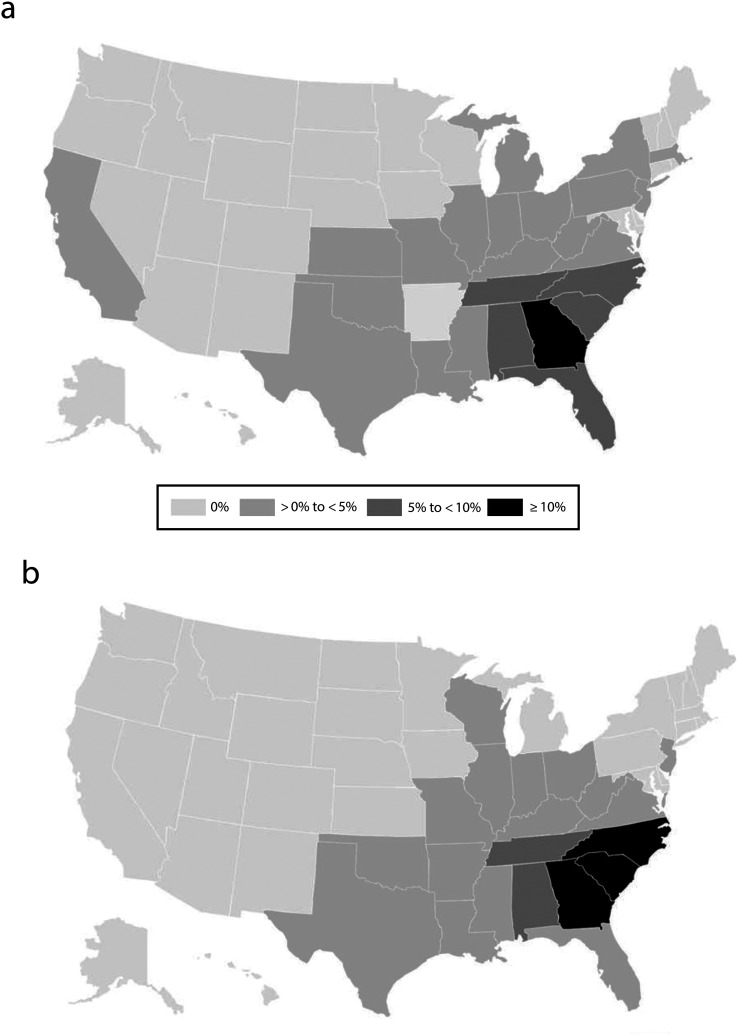
Specific states of residence for women having an abortion between 22 and less than 24 weeks and at 24 or more weeks are in Figure 2. Residents of 2 states other than Georgia represented at least 10% of women having an abortion in Georgia between 22 and less than 24 weeks from LMP: North Carolina and South Carolina. Georgia was the only state that represented at least 10% of women having an abortion in Georgia at 24 or more weeks from LMP.
FIGURE 2—
Proportion of women having an abortion in Georgia, by US state of residence, (a) at or after 24 weeks from last menstrual period in 2012 and (b) at 22 to < 24 weeks from last menstrual period in 2012–2013.
DISCUSSION
We found that almost 400 women in our sample had an abortion at or after 24 weeks from LMP in 2012. We also found that about 400 women in our sample had an abortion between 22 and less than 24 weeks from LMP in each of the 2 years, with fewer in 2013 than in 2012. Reflecting demographic characteristics of women who have abortions in Georgia,9 more than half of women having abortions after 20 weeks were Black. Although our data do not indicate that Black women are disproportionately affected compared with other abortion patients, they are the group of women most affected by these abortion regulations. Fewer Hispanic women and women with less than a high-school education had abortions at or after 20 weeks in Georgia in 2013 than in 2012; thus, they appear to be disproportionately affected by the ban that went into effect.
Only one third of women having an abortion at or after 24 weeks from LMP in the 4 Georgia facilities in 2012 were residents of Georgia, with women from throughout the South as well as the Midwest and Northeast also receiving this care. This is not surprising, as 87% of US counties lack an abortion provider and even fewer counties have a later provider.3,10 Georgia was the last state in the Southeast to provide abortion care at or after 24 weeks from LMP for reasons other than fetal anomalies and life endangerment, and no state in the Midwest provides this care.3 Because we found that a smaller proportion of later abortion patients were from the Midwest and Northeast in 2012 than 2013, we can see that Georgia’s ban affects not only Georgia women but also women throughout the South, as well as from the Midwest and Northeast.
It is also worth noting that the effects of the ban may extend to abortions at earlier gestations. There was also a decrease in abortions between 20 and 24 weeks from LMP between 2012 and 2013 even though no law restricted these services in that period (and even though the 22-week ban, if it took full effect, would not apply at 20 weeks from LMP). As many women resided outside Georgia, it may be that women at or after 20 weeks from LMP from out of state were no longer being referred to Georgia in 2013 out of misunderstanding of the part of the ban that went into effect or a misunderstanding about when the ban would apply if it did take full effect and thus that women would be beyond the gestational limit. The decrease in abortions between 20 and 24 weeks appears larger (2013 number was 86% of 2012 number) than the overall decrease in abortions in Georgia from 2012 to 2013 (2013 number was 95% of 2012 number; e-mail communication, Donna L. Moore, State Registrar and Director, State Office of Vital Records, Georgia Department of Public Health, October 30, 2014). Thus, it seems plausible that this reduction in the number of abortions between 20 and 24 weeks from 2012 to 2013 in Georgia was at least partially related to the 22-week ban.
Likewise, when one considers women who would be affected if courts allow Georgia to ban abortion starting at 22 weeks from LMP, a little less than half of women having an abortion in Georgia between 22 and 24 weeks from LMP were residents of Georgia. Women from throughout the South (especially North and South Carolina, neither of which has a provider who provides abortion care after 22 weeks3), and a small number from the Midwest also received this care. Thus, the 22-week ban would be expected to affect women throughout the South as well as some from the Midwest. If Georgia’s entire 22-week ban goes into effect, Florida will be the only state in the Southeast that provides abortion care for reasons other than fetal anomalies and maternal indications between 22 and 24 weeks from LMP.3
Whereas some women seek later abortion care because they discovered a fetal anomaly,11 others seek later abortion because they discovered pregnancies later in gestation, experienced financial and logistical barriers, or had difficulty deciding to terminate.12–14 Restricting later abortion care will likely mean that at least some women will be unable to obtain abortion care,15 which can result in these women having increased risk of intimate partner violence and adverse health outcomes.16,17 Later abortion costs more than abortion care earlier in pregnancy, and delays add additional costs.10,14 Even without additional delays because of new restrictions, direct costs of later abortion already present a substantial economic burden for women.14 Additional delays in timing of abortion as well as additional travel burden because of restricting care in already underserved regions is likely to exacerbate existing financial burdens associated with obtaining later abortion care.15
An essential public health service is assuring availability of personal health services.18 If one views later abortion as a personal health service, our findings strongly suggest that the public health role of assuring availability of abortion has not been met. Public health professionals should prioritize building capacity and ensuring access to this health service for women in the South and Midwest. They should also work with providers in states without state-based gestational limits to help them expand their later abortion services to help mitigate the loss of services in Georgia.
Limitations
This analysis has limitations worth noting. In particular, these analyses do not include data about women who would have received their abortion in Georgia in 2013 had the current restriction not been in place; nor do they include information about how (or if) this population of women were affected.
It is also likely that there were additional procedures provided at other facilities in Georgia that are not captured by this chart abstraction. However, the number of abortions reported to the Centers for Disease Control and Prevention after 21 weeks in Georgia in 2009 was 9952; in 2012 in our sample, this was 1030, which is more than the 2009 number. This suggests that we likely captured the vast majority of these procedures. Thus, there is no reason to believe that our main substantive finding regarding the regional significance of restricting Georgia’s later abortion services would be changed by including data from an additional facility.
Conclusions
Most women likely to be affected by Georgia’s entire 22-week ban and already affected by the part of the ban that went into effect in 2013 are already vulnerable populations. They are residents from states across the South, as well as the Midwest and Northeast. Later abortion care for a very limited type of fetal and maternal indications may still be available in some parts of the Southeast and Midwest. Outpatient abortion services at 24 or more weeks in the absence of maternal or fetal indications are no longer available in the Southeast or Midwest, and if Georgia’s entire 22-week ban goes into effect, Florida will have the only post-22-week outpatient abortion services in the absence of maternal or fetal indications in the Southeast. Georgia’s ban has regional implications and is perpetuating the already inequitable distribution of this health service. Examining this ban through a lens of essential public health services presents a challenge, obligating public health professionals to take steps to ensure access to this otherwise unavailable health service.
Acknowledgments
This study was funded by an anonymous foundation.
A presentation based on the work included in this article was presented at the American Public Health Association Annual Meeting; November 2–6, 2013; Boston, MA.
The authors thank Selena Phipps and Elise Belusa for research and project assistance associated with this study and the facilities in Georgia for their collaboration.
Human Participant Protection
This study was granted ethical approval by the University of California, San Francisco’s Committee on Human Research.
References
- 1.Guttmacher Institute. State policies in brief: state policies on later abortions. Available at: http://www.guttmacher.org/statecenter/spibs/spib_PLTA.pdf. Accessed June 27, 2014.
- 2.Pazol K, Creanga AA, Zane SB, Burley KD, Jamieson DJ. Abortion surveillance—United States, 2009. MMWR Surveill Summ. 2012;61(8):1–44. [PubMed] [Google Scholar]
- 3.Advancing New Standards in Reproductive Health. Later abortion. Available at: http://www.ansirh.org/research/late-abortion.php. Accessed June 27, 2014.
- 4. Ga Code Ann §§ 16-12-141, 31-9b-1, 31-9B-2, 31-9b-3 (2013).
- 5. Ga Code Ann § 16-12-141 (c) (2011).
- 6. Order Granting Plaintiffs’ Motion for Interlocutory Injunctive Relief, Lathrop v Deal, No. 2012-v-224423 (Ga Super Ct 2012).
- 7.Feminist Women’s Health Center. Surgical abortions. Available at: http://www.feministcenter.org/abortion-care/surgical-abortion. Accessed February 19, 2015.
- 8.US Census. Census regions and divisions of the United States. Available at: http://www2.census.gov/geo/docs/maps-data/maps/reg-div.txt. Accessed May 6, 2015.
- 9.Pazol K, Creanga AA, Burley KD, Hayes B, Jamieson DJ. Abortion surveillance—United States, 2010. MMWR Surveill Summ. 2013;62(8):1–44. [PubMed] [Google Scholar]
- 10.Jones RK, Finer LB. Who has second-trimester abortions in the United States? Contraception. 2012;85(6):544–551. doi: 10.1016/j.contraception.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Kerns JL, Swanson M, Pena S et al. Characteristics of women who undergo second-trimester abortion in the setting of a fetal anomaly. Contraception. 2012;85(1):63–68. doi: 10.1016/j.contraception.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Drey EA, Foster DG, Jackson RA, Lee SJ, Cardenas H, Darney PD. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol. 2006;107(1):128–135. doi: 10.1097/01.AOG.0000189095.32382.d0. [DOI] [PubMed] [Google Scholar]
- 13.Janiak E, Kawachi I, Goldberg A, Gottlieb B. Abortion barriers and perceptions of gestational age among women seeking abortion care in the latter half of the second trimester. Contraception. 2014;89(4):322–327. doi: 10.1016/j.contraception.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Roberts SCM, Gould H, Kimport K, Weitz TA, Foster DG. Out-of-pocket costs and insurance coverage for abortion in the United States. Womens Health Issues. 2014;24(2):e211–e218. doi: 10.1016/j.whi.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Upadhyay UD, Weitz TA, Jones RK, Barar RE, Foster DG. Denial of abortion because of provider gestational age limits in the United States. Am J Public Health. 2014;104(9):1687–1694. doi: 10.2105/AJPH.2013.301378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts SCM, Biggs MA, Chibber KS, Gould H, Rocca CH, Foster DG. Risk of violence from the man involved in the pregnancy after receiving or being denied an abortion. BMC Med. 2014;12:144. doi: 10.1186/s12916-014-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raymond EG, Grimes DA. The comparative safety of legal induced abortion and childbirth in the United States. Obstet Gynecol. 2012;119(2 pt 1):215–219. doi: 10.1097/AOG.0b013e31823fe923. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. The public health system and the 10 essential public health services. Available at: http://www.cdc.gov/nphpsp/essentialservices.html. Accessed June 27, 2014.