Abstract
During the early stages of an influenza pandemic, a pandemic vaccine likely will not be available. Therefore, interventions to mitigate pandemic influenza transmission in communities will be an important component of the response to a pandemic. Public-housing residents, single-parent families, and low-income populations may have difficulty complying with community-wide interventions.
To enable compliance with community interventions, stakeholders recommended the following: (1) community mobilization and partnerships, (2) culturally specific emergency communications planning, (3) culturally specific education and training programs, (4) evidence-based measurement and evaluation efforts, (5) strategic planning policies, (6) inclusion of community members as partners, and (7) policy and program changes to minimize morbidity and mortality.
LARGE CONCENTRATIONS OF public-housing residents, single-parent families, and poor families living in economically depressed neighborhoods continue to experience poor health status in the United States.1 Pre-existing social and health conditions will present major obstacles for stakeholders to effectively prepare for and respond to pandemic influenza in such communities.2
Few pandemic influenza plans, recommendations, and guidelines for preparedness and response have focused on the needs, barriers, concerns, and assets of public-housing residents, single-parent families, and poor populations.3–20 Data suggest that poverty, in addition to exposing individuals to more acute and chronic stressors, weakens an individual's ability to cope with new problems and difficulties.21
In this article we (1) highlight public health challenges that might differentially affect public-housing residents, single-parent families, and low-income populations; (2) provide specific recommendations for protecting these population groups; and (3) determine measures that public health communities should take to support these populations for the cascading second- and third-order consequences of recommended interventions, such as isolation and treatment, voluntary home quarantine, social distancing, and antiviral medications and vaccines.
POPULATION CHARACTERISTICS
On September 30, 2007, in the United States there were 3.4 million housing units that received operating funds from the US Department of Housing and Urban Development, and 6.8 million people living in those units.22 Nearly 1.5 million US residents reside in public housing (affordable housing for low-income people, subsidized by the federal government).23 Most public housing units usually are located in high-poverty neighborhoods with high unemployment rates.24 In 2006, there were 10.4 million households headed by a single female parent and 2.4 million headed by a male single parent in the United States.25 3.9 million of these single-parent households lived below the federal poverty level.26 The populations of public housing residents, single-parent families, and low-income households overlap (Figure 1).
FIGURE 1.
Overlapping populations of low-income households, single-parent families, and public-housing residents.
In 2000, US census data revealed that the southeastern United States has a high concentration of counties with high percentages of single-parent–headed households.27 Further, high percentages were observed in counties containing and surrounding major US cities. This observation was also noted in the percentages of persons living below the federal poverty level. In addition to high poverty in the southeast, high concentrations were also noted in Appalachia (Pennsylvania, West Virginia, Kentucky, Tennessee, and North Carolina)24 and in states along the southern border (Texas, New Mexico, and Arizona).24
CONCEPTUAL FRAMEWORK
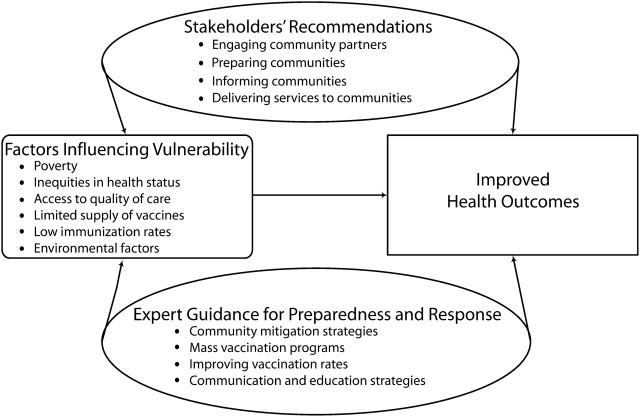
We developed a conceptual framework (Figure 2) to link the contributing and causal factors for preparing these selected populations in the event of an influenza pandemic. This framework was derived from a literature review of electronic databases and convening a meeting of stakeholders to obtain effective ways for stimulating community change.
FIGURE 2.
Preparing public-housing residents, single-parent families, and low-income households for pandemic influenza.
FACTORS INFLUENCING VULNERABILITY TO PANDEMIC INFLUENZA
Pandemic influenza could cause high levels of illness, death, social disruption and economic loss. Death rates from pandemic influenza may be determined by the number of people who become infected, the virulence of the virus, the underlying characteristics and vulnerability of affected people, and the availability and effectiveness of preventive measures.28 Public-housing residents, single-parent families, and low-income populations are likely to be more susceptible to complications from pandemic influenza because of some combination of the following factors: (1) insufficient funds to stockpile medications and supplies, (2) lack of adequate insurance that delays receipt of effective health care, (3) inability to obtain high-quality health care with publicly funded health insurance, (4) unstable employment and inefficient job benefits along with weak social support networks, and (5) lack of awareness of effective personal health interventions or inability to apply them because of competing everyday survival needs.3–20 These indicators of vulnerability are in turn influenced by underlying factors such as (1) poverty,29–31 (2) inequities in health status,32,33 (3) poor access and quality of care,34–39 (4) limited supply of pandemic vaccine,17,40 (5) low immunization rates,41,42 and (6) environmental factors.30,43 These social and personal factors are confounded by system, policy, and institutional factors that cannot be readily isolated or critically examined in a short essay focused on practical advice for lay persons.
Influence of Poverty on Pandemic Influenza
These populations are more susceptible to complications from pandemic influenza because of poverty. Women, especially single mothers, bear a disproportionate burden of poverty.29,30 Many low-income people are unable to meet their basic needs of adequate food, water, clothing, shelter, and health care.30
During an influenza pandemic, persons with low incomes may be reluctant to stay home from work because of fear of losing income, fear of being unemployed, and lack of flexibility in their jobs to work from home. These population groups may not receive compensated sick leave, may be employed in service-related industries in which telecommuting is not an option, or may work in industries with increased numbers of public contacts (e.g., fast-food service). These types of conditions may cause parents to keep their children in communal (unlicensed, unorganized, or informal) child care settings where risk exposures are relatively high.2
Inequities in Health Status
High prevalence of and excess morbidity from diabetes; chronic diseases of the lung, heart, and kidneys; and acute respiratory infections, including influenza, are among the manifestations of poor health status in these vulnerable populations.32 Poverty and near poverty play an increasingly important role in determining health status.33
Access and Quality of Care
The government's response to Hurricane Katrina showed gaps in the nation's ability to provide services for public-housing residents, single-parent families, and low-income populations.34 Public-housing residents are slightly more likely than other US citizens to be without health insurance or report financial barriers to medical care.35 According to the National Center for Health Statistics (NCHS), unmarried women aged 25–64 years are approximately 60% more likely than married women to lack health insurance coverage.36,37 Providing health care for the uninsured or underinsured during a pandemic may be a challenge for hospitals and physicians because more than 46 million persons living in the United States do not have health insurance38 and another 25 million are considered underinsured.39 In addition, low-income persons are more likely to obtain regular medical care in emergency rooms, health departments, and community health centers. These locations are becoming increasingly crowded. Patients waiting for care in these settings are likely to have greater exposure to influenza viruses and other pathogens.31
Limited Supply of Pandemic Vaccine
In the event of a pandemic influenza outbreak, a pandemic vaccine may not be available or may be in limited supply because the antigenic details of the evolved pandemic strain of the virus may not be known before the outbreak occurs. This factor may lead to an inability to prepare large numbers of doses of highly effective vaccine preceding an influenza pandemic outbreak.40 Vaccines will likely be administered in accordance with a prioritization scheme by which groups to be vaccinated first are already identified, including health care workers; homeland security workers, police, firefighters and other first responders; government leaders; and specific population subgroups (i.e., pregnant women, infants, and toddlers).17
Low Immunization Rates
Influenza is responsible for more than 36 000 deaths per year. Some experts believe there will be a relationship between the low rates of seasonal influenza vaccination among low-income populations and the distribution and acceptance of an influenza pandemic vaccine among these groups.41 Evidence exists of effective measures that have been used to improve rates of seasonal influenza immunization among low-income groups, but there is much to be done to improve those rates.42
In 2003, the proportion of persons aged 18–64 years and aged 65 years and older who reported receiving influenza vaccinations during the preceding 12 months fell short of the 2010 Healthy People objectives of 60% and 90%43, respectively. Characteristics associated with lower levels of vaccination coverage were race, age, and income below the federal poverty level. For persons aged 65 years and older, the vaccination rate for those below the poverty level among White, non-Hispanic, seniors was 59.5% ± 6.6, which was higher than that for Black, non-Hispanic, seniors (48.7% ± 9.7) and significantly higher than that for Hispanic seniors (38.5% ± 9.7).42
ENVIRONMENTAL FACTORS INFLUENCING PANDEMIC INFLUENZA
Public-housing residents are more likely than the community at large to be poor, and public housing is associated with poorer health. Substandard housing is a major public health issue associated with health conditions such as respiratory infections, asthma, lead poisoning, injuries, and mental health.44 Many residents of these populations face burdens of unsafe drinking water, absence of hot water for washing, ineffective waste disposal, housing infested by disease vectors (insects, mice, rats), inadequate food storage, overcrowding (from urbanization and landfill waste),30 and inadequate ventilation, which could cause serious implications during an influenza pandemic.44
The results of a metaregression performed using 4 nationally represented surveys determined that worsening housing instability and economic standing were associated with poorer health care access: being uninsured (5.4% per unit increase; 95% confidence interval [CI]=1.7%, 9.2%; P = .011), postponing needed care (3.3%; 95% CI=1.9%, 4.7%; P = .001), postponing medications (6.1%; 95% CI=1.5%, 10.6%; P = .035), and having higher hospitalization rates, which is one measure of use of acute health care (2.9%; 95% CI=1.2%, 4.6%; P = .008).45
SOLUTIONS FOR PANDEMIC INFLUENZA PREPAREDNESS AND RESPONSE
With limited vaccine and a tiered vaccine distribution plan, public health response activities for these targeted populations during a pandemic will rely on using nonpharmaceutical interventions and influenza antiviral medications, and these interventions will likely include both voluntary and imposed changes in social patterns. Community mitigation strategies include respiratory hygiene and cough etiquette, hand hygiene, isolation and treatment, voluntary home quarantine, school dismissal, and social distancing in the community and workplace.40 Both public health literature3–20 and stakeholders suggest that medical countermeasures and community mitigation strategies will be the most commonly used public health measures for protecting public-housing residents, single-parent families, and low-income populations in the event of an influenza pandemic.
Mass Vaccination Programs
Mass vaccination programs and vaccination intervention strategies mentioned in the literature may prove to be effective methods for improving vaccination rates among these populations in the event of an influenza pandemic. Federal, state, and local governments are proposing to use mass dispensing and vaccination clinics to swiftly distribute medication during an influenza pandemic. Many of the challenges of delivering medicines on a large scale during an emergency involve the receipt, breakdown, and distribution of the Strategic National Stockpile.46 Two key considerations in planning for mass vaccination clinics are (1) the capacity of each clinic, measured by the number of patients served per hour and (2) the time, measured in minutes, spent by patients in the clinic.47 Outreach and targeted communication efforts, as well as community partnerships, may be crucial in informing low-income communities about the location and distribution of pandemic vaccinations and medications.
Even though the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is not a mass vaccination program, strategies to promote immunization among clients in these programs have been effective in improving immunization coverage for low-income preschool children.48–50 Furthermore, WIC sites in the community could serve as mass vaccination clinics. WIC is the largest point of access to health-related services for low-income preschool children, a population known to have low immunization coverage.48
Improving Vaccination Rates
Several studies have identified interventions that were successful in improving vaccination rates among low-income populations. One study in east Harlem and the Bronx used intervention strategies that included disseminating information through mailings, education, and targeted advertising; presenting at meetings; and providing street-based and door-to-door vaccination during 2 influenza vaccine seasons. Results from the study show that communities and groups were more interested in receiving the influenza vaccine after the interventions occurred (OR=2.69; CI=2.17, 3.33; P =<0.01).51 Also, findings from the 2003 National Health Interview Survey indicated that among Hispanics, having Spanish-speaking health care providers and culturally specific, linguistically appropriate communication materials is associated with an increase in influenza vaccination coverage and a better response to communication materials about prevention messages and guidelines.42
Communicating Effectively With Targeted Populations
Prepandemic, pandemic, and postpandemic communications require special attention to ensure that public-housing residents, single-parent families, and low-income populations comply with community mitigation recommendations. Communicating effectively with the intended populations requires understanding the cultural context, social environment, and individual cognitions of these groups.52,53 Communication strategies should be designed to reflect the cultural backgrounds of these communities.37 Principles that can guide interactions and the development of messages for the targeted populations include the following: (1) build trust among individuals in the community, using gatekeepers, social networks, and lay communication leaders; (2) ensure that messages reach the intended recipient; (3) establish and deliver culturally competent and sensitive messages; (4) deliver personalized messages; and (5) use interpreters when needed. Because there are cultural differences among these groups, it is imperative that the various styles of communication among these targeted populations are understood. Social marketing and communication theories that help to explain and prepare these communities in the event of a pandemic influenza are described by Vaughn and Tinker54 in another paper in this issue.
STAKEHOLDER STRATEGIES AND RECOMMENDATIONS
At a meeting held at the Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, during May 1–2, 2008, “Pandemic Influenza Preparedness and Response in Selected Vulnerable Populations,” 26 stakeholders were invited to promote community participation, support, and capacity building for organizing recommendations to protect certain populations—public-housing residents, single-parent families and low-income populations, their families, service providers, and other stakeholders—from the adverse health impact of an influenza pandemic. These external partners represented federal, state, and local departments of Housing and Urban Development; state and local agencies; community-based organizations; faith-based organizations; college officials and instructors; and community members that serve low-income populations.
Preparing the Community for Pandemic Influenza
Participants provided an overview of their community's perceptions on health and crises situations; the importance of cultural values; patterns of using health services; and community mitigation risks. Even though the federal, state, and local governments have been engaged in extensive pandemic influenza preparedness efforts, many of the meeting participants were unaware of a possible pandemic influenza outbreak. Participants were concerned about how knowledgeable and aware public-housing residents, single-parent families, and low-income populations were regarding a potential pandemic influenza and their involvement in preparedness activities. During the meeting, participants suggested that a community risk assessment be conducted using participatory action research to (1) place community members in the lead role to conduct the assessment; (2) determine perceptions of needs, risks, and values in the communities; (3) determine strengths and weaknesses of the communities; and (4) obtain listings of resources in the community for developing effective strategies and recommendations for protecting these populations in the event of a pandemic influenza.
Participants concluded that communications and educational strategies are integral public health components for preparing these communities in the event of an influenza pandemic, acknowledging the distinctions in lifestyles, beliefs, behaviors, and cultures of these groups. The design (including practical, scientific, and ethical issues), planning, implementation, and evaluation of educational and communication strategies should include community organizations, community participants, and gatekeepers in the community to provide individual and community change.
Recommendations for Pandemic Influenza Preparedness and Response
External partners considered the existing data on the impact of influenza, effectiveness of different measures to lessen the burden of influenza, and barriers and strategies to implement measures to decrease the burden of influenza among communities. The following recommendations were suggested to help public-housing residents, single-parent families, and low-income populations comply with community-mitigation measures in the prepandemic and pandemic stages of an influenza pandemic (Table 1).
TABLE 1.
Suggestions for Effective Pandemic Influenza Containment and Community Mitigation Strategies for Public-Housing Residents, Single-Parent Families, and Low-Income Populations
| Recommendations | Needs | Barriers | Solutions |
| To prepare for recommendations about the use of vaccines (prepandemic, pandemic, and antivirals) | Community Mobilization | Lack of awareness, education, information | Engage and educate |
| Culturally and linguistically appropriate education information | Limited supply of vaccine and antivirals | Develop culturally specific communication methods | |
| Easy access to familiar and trusted distribution centers | Language barriers | Provide financial incentives | |
| Enough vaccine for the community | Transportation and financial needs | Establish partnerships | |
| Community involvement in an effective distribution plan | |||
| To prepare and respond to recommendations about hygiene | Personal items necessary for staying at home | Not engaging stakeholders early | Culturally competent communication methods |
| Resources and manpower to provide education about pandemic influenza | Lack of knowledge or understanding issues | Engage faith-based organizations, CBOs, and neighborhood planning units | |
| Effective communication methods | Limited resources | Identify community liaisons | |
| Early engagement of the community | Mixed or competing messages | ||
| To prepare and respond to recommendations about school closures | Clear policy on school closures | No alternatives for child care | Defined school policies |
| Health education and event preparedness | Increased financial burden | Voucher, waived fees for child care | |
| Trained staff | Lack of information | Community engagement | |
| Alternate daycare and after-school care solutions | Reluctance to accept services | Stockpile necessities using food banks, churches, community resources | |
| Lack of social support | Social and psychological support systems | ||
| To prepare and respond to recommendations about workplace policy during an influenza pandemic | Workplace pandemic plan | Fear of loss of jobs or profits | State and Federal mandates for assistance |
| Means to offset personnel loss and absences | Unclear expectations | Alternative compensation packages | |
| Employer and employee educational support | Lack of adequate communications | Government freeze on prices, wages, and so on | |
| Federal legislation on workplace closure and policies | Political influence | Flexibility (work from home) | |
| Education for employers and employees | Resistance to policies for fear of job loss | Community involvement in workplace plan | |
| To prepare and respond to recommendations about avoiding public gatherings | Social interaction | Difficulty enforcing isolation | Education and training |
| Purchase of goods and services | Varying definitions of public gatherings | Home-structured activities and programs | |
| Policies that are evidence based and explanatory | Economic challenges | Delivery of goods and services | |
| Education regarding the definition of public gatherings and need for postponement or cancellation of events | Inability to communicate with others | Culturally competent messages | |
| Stay-at-home alternatives | Inability to acquire personal needs | Mobile clinics and distribution centers | |
| To prepare and respond to recommendations about pandemic status, affected communities, risk, and recommended action | Right message, right time, right people | Misinformation | Keep it simple |
| Action-based planning | Apathy toward messages | Culturally sensitive and specific communications | |
| Education and buy-in | Messages not targeting the audience | Action-based educational messages | |
| Honesty and transparency | Messenger should know community | Use of existing mechanisms | |
| Messages too wordy | |||
| To identify signs and symptoms of pandemic influenza | Resources | Lack of community coordination | Education and training |
| Knowledge, training, education | Limited resources | Checklist for home | |
| Simplistic, culturally relevant messages | Lack of realistic expectations for identification and prevention | Available personal protective equipment | |
| Community involvement | Spiritual/religious restrictions/beliefs | Hotline case management | |
| Lack of trust and fear of being ostracized | Community resources |
Mobilization, partnerships, and networks.
Establish community mobilization, partnerships, and networks with faith-based organizations, community-based organizations, neighborhood planning units, and key informants to help educate the community; provide mobile clinics, distribution centers, culturally and linguistically appropriate education information; and deliver food, medication, goods, and services.
Risk-communications plans.
Establish a multifaceted, emergency risk-communications plan that is culturally specific and has relevant education messages.
Appropriate education and training programs.
Offer culturally specific and linguistically appropriate education and training programs for adults and children on signs and symptoms of pandemic influenza; how to prepare for school closures, respond to public gatherings, and use good hygiene; and offer resources to help meet the needs of these target populations that use WIC and other programs.
Evidence-based measurement and evaluation system.
Establish an evidence-based measurement and evaluation system guided by federal, state, and local governments to assess the progress, level of preparedness, and effectiveness of intervention strategies targeting low-income populations.
Planning policies.
Establish strategic planning policies, in partnership with faith-based organizations, community-based organizations, neighborhood planning units, and other partners for social distancing, containment, and the distribution of antiviral medications and vaccine.
Community partners.
Ensure community members are partners—sooner rather than later—in the strategic planning process.
Advocacy.
Advocate for policy and program changes at the federal, state, and local levels to minimize morbidity and mortality among low-income populations, such as policies for school closures, compensation packages, and state/federal mandates for assistance.
Stakeholder Suggestions
Stakeholders also suggested the following actions for public health practitioners, health care providers, and emergency managers to enhance the community's compliance with mitigation interventions:
Use mobile units to deliver health care services;
Provide transportation to health care facilities;
Distribute and ensure access to vaccine and antiviral medications;
Provide culturally and linguistically appropriate educational information, materials, and messages about pandemic influenza; and
Provide trained staff to handle inquiries and problems about school closings, workplace policies, public gatherings, alternatives for childcare, social support, and distribution plans for vaccine, antiviral, food, and other supplies.
These suggestions will enable governments, organizations, and associations to reach public-housing residents, single-parent families, and low-income populations with the appropriate information, adequate training, and awareness of disaster preparedness. Governments and community groups will benefit from sharing ideas on how best to collaborate to reach these groups and build trust among their communities.54 In addition, research is needed to prevent or minimize racial and ethnic disparities in vaccine distribution and acceptance, respond to mitigation strategies, and address factors that influence influenza-related diseases.2
CONCLUSIONS
Public health strategies for mitigating pandemic influenza among public-housing residents, single-parent families, and low-income populations are crucial for protecting these populations. Early diagnosis and timing of community mitigation strategies during a pandemic is critical for public safety, health, and treatment. Low-income populations often delay treatment and care because of issues with access and financial constraints, and being poor is one of the characteristics that has often been associated with lower influenza vaccination coverage. Planning and coordination efforts during an influenza pandemic require collaboration at all levels (federal, state, and local governments) and involves cooperation of leaders from the public and private sectors. National and homeland security, health care providers, community support groups, and planners of critical infrastructure should include the needs of vulnerable populations in planning activities for the potential worldwide threat of an influenza pandemic. Because of the uncertainty of the capacity of the federal, state, and local governments, there may be challenges in moving these recommendations forward to ascertain actions.
Acknowledgments
The authors acknowledge Karen Wooten for contributions to the paper, and Lander Stoddard (facilitator), Peter Rzeszotgarski (cofacilitator), Brandi Meriwether (scribe), and Angela Johnson (breakout session reporter) for work performed during the breakout session on public-housing residents, single-parent and low-income populations. We also acknowledge our external stakeholders for sharing their expertise during the external partners meeting on May 1–2, 2008, in Atlanta, GA: Lesley Green-Rennis, Rita Daye, Nina Agbayani Grewe, Mildred McClain, Jane Ka'ala Pang, Angela Johnson, Jemel Slughter, James Tomlin, Alida L. Ward, Cynthia Trawick, Bernie Hicks, Theresa Chappel, Margaret S. E. Counts-Spriggs, Wendy Cameron, Faye Boyd, Sue Davis, Beth Padgett, Lisa Petoney, Leslie Moye’, Nneka Mosley, and George Rust.
Human Participant Protection
No human participant protection was necessary for this article.
References
- 1.Krieger N, Chen JT, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95:312–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blumenshine P, Reingold A, Egerter S, Mockenhaupt R, Braveman P, Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg Infec Dis. 2008; 14(5):709–715. Available at: http://www.cdc.gov/eid. Accessed November 12, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Interim guidance on planning for the use of surgical masks and respirators in health care settings during an influenza pandemic. Available at: http://pandemicflu.gov/plan/healthcare/maskguidancehc.html. Accessed August 18, 2008.
- 4.Kansas Department of Health and Environment. Kansas Pandemic Influenza Preparedness and Response Plan. Topeka, KS: Center for Public Health Preparedness; 2007. [Google Scholar]
- 5.Association of State and Territorial Health Officials (ASTHO). At-risk populations and pandemic influenza: planning guidance for state, territorial, tribal, and local health departments. Available at: http://www.astho.org/index.php?template=at_risk_population_project.html. Accessed August 17, 2008.
- 6.Centers for Disease Control and Prevention. Interim guidance on environmental management of pandemic influenza virus. Available at: http://www.pandemicflu.gov/plan/healthcare/influenzaguidance.html. Accessed August 17, 2008.
- 7.Centers for Disease Control and Prevention. CDC Influenza pandemic operation plan (OPLAN). Available at: http://www.cdc.gov/flu/pandemic/cdcplan.htm. Accessed August 17, 2008.
- 8.Holmberg SD, Layton CM, Ghneim GS, Wagener DK. State plans for containment of pandemic influenza. Emerg Infect Dis. 2006;12(9):1414–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson AJ, Moore ZS, Edelson PJ, et al. Household responses to school closure resulting from outbreak of influenza B, North Carolina. Emerg Infect Dis. 2008;14(7):1024–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meltzer MI. Pandemic influenza, reopening schools, and returning to work. Emerg Infect Dis. 2008;14(3):509–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Occupational Safety and Health Administration. Guidance on preparing workplaces for an influenza pandemic—OSHA.3327-02N 2007. Available at: http://www.osha.gov/Publications/influenza_pandemic.html. Accessed August 21, 2008.
- 12.Osterholm MT. Preparing for the next pandemic. N Engl J Med. 2005;352(18):1839–1842. [DOI] [PubMed] [Google Scholar]
- 13.State and local governments. State and local government planning and response activities. Available at: http://www.pandemicflu.gov/plan/states/index.html. Accessed August 17, 2008.
- 14.US Department of Health and Human Services. HHS pandemic influenza plan. Available at: http://www.hhs.gov/pandemicflu/plan/part1.html. Accessed August 11, 2008.
- 15.US Government. Planning checklists. Available at: http://www.pandemicflu.gov/plan/checklists.html. Accessed August 17, 2008.
- 16.US Department of Health and Human Services. Community strategy for pandemic influenza mitigation. Available at: http://www.pandemicflu.gov/plan/community/commitigation.html. Accessed August 17, 2008.
- 17.US Department of Health and Human Services and US Department of Homeland Security. Guidance on allocating and targeting pandemic influenza vaccine. Available at: http://www.pandemicflu.gov/vaccine/allocationguidance.pdf. Accessed August 19, 2008.
- 18.World Health Organization. WHO global influenza preparedness plans: the role of WHO and recommendations for national measures before and during pandemics. Available at: http://www.who.int/csr/resources/publications/influenza/CDS_GIP_2006_5c.pdf. Accessed August 17, 2008.
- 19.World Health Organization. Pandemic Influenza Preparedness and Mitigation in Refugee and Displaced Populations: WHO Guidelines for Humanitarian Agencies. 2nd ed. Geneva, Switzerland: World Health Organization; 2008. Available at: http://www.who.int/diseasecontrol_emergencies/HSE_EPR_DCE_2008_3rweb.pdf. Accessed August 17, 2008. [Google Scholar]
- 20.Wu JT, Riley S, Fraser C, Leung GM. Reducing the impact of the next influenza pandemic using household-based public health interventions. PLoS Med. 2006;3(9):e361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Cleary PD. Social class and poverty. Am Sociol Rev. 1980;45(3):463–478. [PubMed] [Google Scholar]
- 22.US Department of Housing and Urban Development. Resident characteristics report. Available at: http://www.hud.gov. Accessed February 12, 2008.
- 23.Bennett GG, McNeill LH, Wolin KY, Duncan DT, Puleo E, Emmons KM. Safe to walk? Neighborhood safety and physical activity among public housing residents. PLoS Med. 2007;4(10):1599–1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leventhal T, Brooks-Gunn J. Moving to opportunity: an experience study of neighborhood effects on mental health. Am J Public Health. 2003;93:1576–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Census Bureau. Single-parent households showed little variation since 1994, Census Bureau reports. Available at: http://www.census.gov/Press-Release/www/releases/archives/families_households/009842.html. Accessed March 12, 2009.
- 26.Parents Without Partners. Facts about single parent families. Available at: http://www.parentswithoutpartners.org/Support1.htm. Accessed October 10, 2008.
- 27.US Census Bureau. American community survey, 2006. Available at: http://www.census.gov/acs. Accessed April 4, 2008.
- 28.World Health Organization. Epidemic and pandemic alert and response (EPR). Available at: http://www.wholint/csr/disease/influenza/pandemic10things/en/. Accessed August 17, 2008.
- 29.O'Neil MS, McMichael AJ, Schwarts J, Wartenberg D. Poverty, environment, and health: the role of environmental epidemiology and environmental epidemiologists. Epidemiology. 2007;18:664–668. [DOI] [PubMed] [Google Scholar]
- 30.International Council of Nurses. Fact Sheet: ICN on poverty and health: breaking the link. Available at: http://www.icn.ch/matters_poverty.htm. Accessed September 29, 2008.
- 31.Blumenshine P, Reingold A, Egerter S, Mockenhaupt R, Braveman P, Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Online Emerg Infec Dis. [Serial online]. May 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Australian Health Ministers’ Advisory Council. Preventing Chronic Disease: A Strategic Framework. Victoria, Australia: National Public Health Partnership; 2001. [Google Scholar]
- 33.Gould E, Smeeding T, Wolfe B. Trends in the health of the poor and near poor: have the poor and near poor been catching up to the non poor in the last 25 years? Paper presented at: Annual meeting of the Economics of Population Health: Inaugural Conference of the American Society of Health Economists; June 4, 2006; Madison, WI. [Google Scholar]
- 34.Krane NK, Kahn MJ, Market RJ, Whelton PK, Traber PG, Taylor IL. Surviving hurricane Katrina: reconstructing the educational enterprise of Tulane University School of Medicine. J Am Coll Health Assoc. 2007;82(8):757–762. [DOI] [PubMed] [Google Scholar]
- 35.Digenis-Bury EC, Brooks DR, Chen L, Ostrem M, Horsburgh CR. Use of a population-based survey to describe the health of Boston public housing residents. Am J Public Health. 2008;98(1):85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernstein AB, Cohen RA, Brett KM, Bush MA. Marital status is associated with health insurance coverage for working-age women at all income levels, 2007. NCHS Data Brief. 2009. [PubMed] [Google Scholar]
- 37.Documét PI, Green HH, Adams J, Weil LA, Stockdale J, Hyseni Y. Perspectives of African American, Amish, Appalachian and Latina women on breast and cervical cancer screening: implications for cultural competence. J Health Care Poor Underserved. 2008;19:56–74. [DOI] [PubMed] [Google Scholar]
- 38.Meltzer MI, Cox NJ, Fukuda K. The economic impact of pandemic influenza in the United States: priorities for intervention. Emerg Infect Dis. 1999;5:659–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.US Department of Health and Human Services. Overview of the uninsured in the United States: an analysis of the 2005 Current Population Survey. ASPE Issue Brief. Available at: http://aspe.hhs.gov/healthreports/05/uninsured-cps/index.htm. Accessed October 31, 2008.
- 40.Germann TC, Kadau K, Longini IM, Macken CA. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci USA. 2006;103(15):5935–5940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20(1):21–25. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Influenza vaccination levels among persons aged > 65 years and among persons aged 18–64 years with high-risk conditions–United States, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:1045–1049. [PubMed] [Google Scholar]
- 43.US Department of Health and Human Services. Healthy People 2010 (Conference Edition, in Two Volumes). Washington, DC: US Department of Health and Human Services; 2000. [Google Scholar]
- 44.Krieger J, Higgins D. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reid KW, Vittinghoff E, Kushel MB. Association between the level of housing instability, economic standing and health care access: a meta-regression. J Health Care Poor Underserved. 2008;19(4):1212–1228. [DOI] [PubMed] [Google Scholar]
- 46.Lien O, Maldin B, Franco C, Gronvall GK. Getting medicine to millions: new strategies for mass distribution. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2006;4(2):176–182. [DOI] [PubMed] [Google Scholar]
- 47.Aaby K, Herrmann JW, Jordan CS, Treadwell M, Wood K. Montgomery County's Public Health Service uses operations research to plan emergency mass dispensing and vaccination clinics. Interfaces. 2006;36(6):569–579. [Google Scholar]
- 48.Shefer AM, Fritchley J, Stevenson J, et al. Linking WIC and immunization services to improve preventive health care among low-income children. J Public Health Manag Pract. 2002;8(2):56–65. [DOI] [PubMed] [Google Scholar]
- 49.Hoekstra EJ, LeBaron CW, Megaloeconomou Y, et al. Impact of a large-scale immunization initiative in the Special Supplemental Nutritional Program for Women, Infants, and Children (WIC). JAMA. 1998;280(13):1143–1147. [DOI] [PubMed] [Google Scholar]
- 50.Lebaron CW, Birkhead GS, Parsons P, et al. Measles vaccination levels of children enrolled in WIC during the 1991 Measles Epidemic in New York City. Am J Public Health. 1996;86(11):1551–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Coady MH, Galea S, Blaney S, Ompad DC, Sisco S, Vlahov D; Project VIVA Intervention Group. Project VIVA: A multilevel community-based intervention to increase influenza vaccination rates among hard-to-reach populations in New York City. Am J Public Health. 2008;98:1314–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Regidor E, de la Fuente L, Gutierrez-Fisac JL, et al. The role of the public health official in communicating public health information. Am J Public Health. 2007;97(S1):S93–S97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eisenman DP, Cordasco KM, Asch S, Golden JF, Glik D. Disaster planning and risk communication with vulnerable communities: lessons from Hurricane Katrina. Am J Public Health. 2007;97(S1):S109–S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vaughn E, Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Public Health. 2009;99(Suppl 2):S324–S332. [DOI] [PMC free article] [PubMed] [Google Scholar]