Abstract
Racial/ethnic minority populations experience worse health outcomes than do other groups during and after disasters.
Evidence for a differential impact from pandemic influenza includes both higher rates of underlying health conditions in minority populations, increasing their risk of influenza-related complications, and larger socioeconomic (e.g., access to health care), cultural, educational, and linguistic barriers to adoption of pandemic interventions.
Implementation of pandemic interventions could be optimized by (1) culturally competent preparedness and response that address specific needs of racial/ethnic minority populations, (2) improvements in public health and community health safety net systems, (3) social policies that minimize economic burdens and improve compliance with isolation and quarantine, and (4) relevant, practical, and culturally and linguistically tailored communications.
AN INFLUENZA PANDEMIC poses a major threat to the health of US and world populations.1 The national pandemic influenza strategy and implementation plans are designed to stop or slow pandemic virus transmission and mitigate the impact on the US population and critical infrastructure.2–4 Essential elements of the pandemic strategy and plans as outlined in this issue by Santibañez et al.4 need full community participation to achieve success. These elements include early detection of cases, rapid antiviral treatment and isolation of patients, antiviral prophylaxis and voluntary quarantine of patient contacts, and social distancing.
Racial/ethnic minority populations may have less capacity to implement these essential pandemic influenza interventions and to tolerate a pandemic because of broad disparities in underlying health status and social factors, such as socioeconomic disadvantages; cultural, educational, and linguistic barriers; and lack of access to and use of health care.5–7 An influenza pandemic could have a disproportionate effect on the health of more than 102 million members of racial/ethnic minorities in the United States.8 Furthermore, if the needs of these populations are not successfully addressed through engagement of their communities in planning, response, and deployment of adequate resources, the national strategy could fail for all, and the entire US population could fail to realize the benefit of timely pandemic prevention and control measures.
We reviewed epidemiological evidence related to the potential differential effect of an influenza pandemic on racial/ethnic minority populations, the potential economic impact of a pandemic on these populations, and implications and opportunities for influenza vaccination. We also report here on a meeting of stakeholders, convened by the Centers for Disease Control and Prevention (CDC) on May 1 and 2, 2008. Participants discussed barriers to recommended pandemic influenza interventions in racial/ethnic minority communities and suggested ways to fully implement them. Our focus is on African American; Asian, Native Hawaiian, and other Pacific Islander; and Latino populations. Protection of American Indian and Alaska Native populations from pandemic influenza is described in a separate article in this issue.9
POTENTIAL HEALTH DISPARITY DURING PANDEMIC INFLUENZA
During and after natural disasters, racial/ethnic minority populations have higher rates of injuries, poor health conditions, adverse health outcomes, and lack of access to health care.10–12 Therefore, pandemic influenza might disproportionately affect the health of racial/ethnic minority populations.5 To examine this proposition, we reviewed several types of available epidemiological evidence: health impact of previous influenza pandemics, annual age-adjusted pneumonia- and influenza-coded deaths, and risk factors for influenza complications, including disparities in annual influenza vaccination coverage. Pneumonia and influenza death rates provide direct evidence of health outcomes; indirect evidence comes from underlying health and health care disparities, which explain disparities in health outcomes. Together, these lines of evidence suggest that a pandemic would have a great impact on racial/ethnic minority populations.
Previous Influenza Pandemics
Racial/ethnic morbidity and mortality estimates for most of the 20th century are only available for African American and White populations.13 Reporting of mortality by other racial/ethnic categories did not begin until the late 1970s, after the last influenza pandemic.
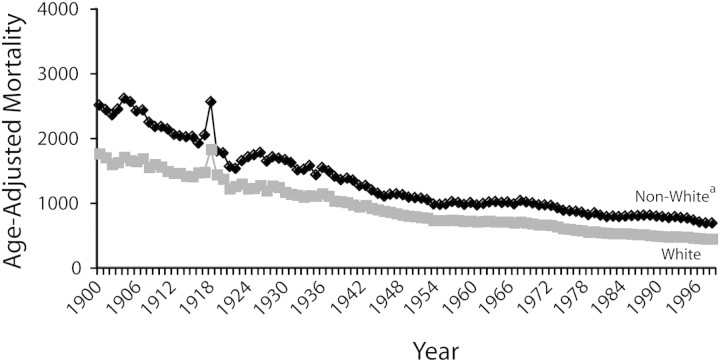
Of the 3 influenza pandemics in the 20th century, the highest age-adjusted, all-cause mortality in the United States occurred in 1918, the peak year of the 1918–1919 influenza pandemic.13 A mortality spike occurred among both White and non-White (African American) populations (Figure 1), although it was steeper among non-White populations, whose all-cause mortality rate was approximately 35% higher than that of Whites immediately before and during the pandemic.13
FIGURE 1.
Age-adjusted all-cause mortality: United States, 1900–1999.
Note. Age-adjusted to the 1940 standard population (per 100 000 population). aNon-White from 1900–1963, and Black or African American from 1964–1999.Source. Adapted from Levine RS et al., Figure 2-1A.13
Although the 1918 non-White–White gap in all-cause mortality cannot be linked exclusively to pandemic influenza because mortality gaps were reported in nonpandemic years, sustained gaps in influenza and pneumonia and in influenza mortalities were evident in subsequent years. For instance, between 1929 and 1931, influenza mortality per 100 000 persons was reported to be 71.3 among non-Whites and 30.3 among Whites.14 Similarly, in 1950 age-adjusted pneumonia and influenza mortality per 100 000 persons was reported as 76.7 among African Americans and 44.8 among Whites (Figure 2).15 Higher 1918 influenza mortality and case-fatality rates among non-White populations in cities and urban populations17,18 also revealed a 1918 non-White–White gap in influenza mortality. Today, a non-White–White gap may also occur because non-White populations are far more concentrated in cities: 27% lived in urban areas in 1910 and 90% do so now; 49% of Whites lived in urban areas in 1910 and 75% do so now.17 Crowding and high population density in cities are well-known risk factors for transmission of respiratory infectious diseases.19
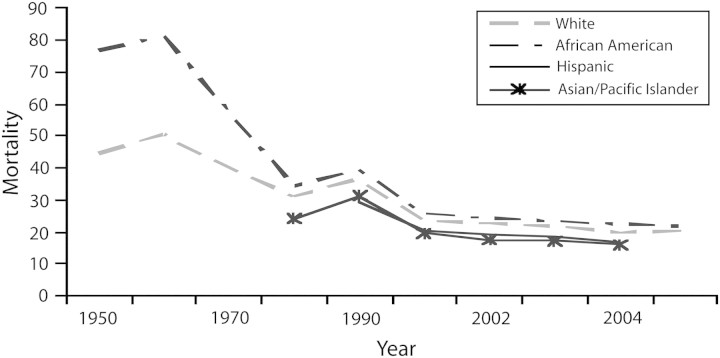
FIGURE 2.
Annual, age-adjusted overall pneumonia and influenza mortality by race/ethnicity: United States, 1950–2005.
Note. Mortality is per 100 000 population. Source. National Center for Health Statistics.15
Annual Pneumonia and Influenza Deaths
Pneumonia and influenza are major underlying causes of death in the United States; in 2004 they were together classified as the eighth leading cause.15 Estimates of annual influenza-related mortality are derived from regression models comprising pneumonia and influenza deaths, deaths from underlying respiratory and circulatory conditions, and types of circulating influenza viruses; influenza-related mortality constitutes a subset of these larger categories.20,21 Although the epidemiology of seasonal influenza may differ from that of a pandemic, and racial/ethnic–specific influenza-related mortality data are not currently available, the epidemiology of annual pneumonia and influenza deaths may nonetheless assist in identifying some high-risk populations during a pandemic.
To understand potential differences in influenza-related mortality, we examined, by race and ethnicity, annual, national age-adjusted mortalities in which influenza or pneumonia was coded as the underlying cause of death. Although pneumonia and influenza mortality from 1950 to 2005 declined among racial/ethnic minority populations for which data were available, and the higher mortality among African Americans than among Whites substantially narrowed, mortality among African Americans was still slightly higher (Figure 2).15,16 Pneumonia and influenza mortality per 100 000 persons was 77 among African Americans in 1950, decreased to 34 in 1980, and leveled off to approximately 23 from 2000 to 2005.15,16 By contrast, pneumonia and influenza mortality per 100 000 persons was 45 among Whites in 1950, decreased to 31 in 1980, and leveled off to approximately 22 from 2000 to 2005. Pneumonia and influenza mortality among Asian/Pacific Islanders was first recorded as 24 per 100 000 persons in 1980 and decreased to 16 in 2005. For Latinos, pneumonia and influenza mortality was not recorded until later: in 1990, rates were 30 per 100 000 persons, decreasing to 17 in 2005.
Among most age groups, African Americans had the highest age-specific pneumonia and influenza mortality. Although the overall pattern of age-specific pneumonia and influenza mortality was similar for African American, White, and other racial/ethnic populations (highest mortality occurred among persons aged ≥ 65 years), from 1999 to 2005, African American populations had the largest age-specific pneumonia and influenza mortality across all age groups up to 85 years.16 For example, among children younger than 5 years, the mortality among African Americans was 4.2 per 100 000; among Whites, 2.1; and among children classified as other, 2.3. Among adults aged 20 to 44 years, mortality was 2.6 per 100 000 among African Americans, 1.2 among Whites, and 0.7 among adults classified as other. Similarly, among persons aged 65 to 84 years, mortality per 100 000 persons was 91.8 among African Americans, 83.2 among Whites, and 60.8 among older persons classified as other. Further analysis is needed to determine whether this pattern of age-specific pneumonia and influenza mortality by race/ethnicity exists for both influenza-related pneumonia and influenza mortality and all influenza-related mortality.
Risk Factors for Influenza Complications
Underlying conditions.
Coronary disease and hypertension, cancer (if treatment or disease is immunosuppressive), asthma, diabetes, HIV/AIDS, and kidney disease are among the indications for annual influenza vaccination, because these conditions increase the risk of severe influenza illness and death (Table 1).15,28
TABLE 1.
Prevalence of Selected Diseases, English Proficiency, Literacy, Economic Characteristics, and Access to Health Care by Race/Ethnicity: United States
| Whites, % or % (No.) | African Americans, % or % (No.) | Latinos, % or % (No.) | Asian/Pacific Islanders, % or % (No.) | |
| Asthma | 10.9 | 12.0 | 8.2 | 8.6–18.0 |
| Coronary heart diseasea | 6.5 | 6.2 | 4.9 | 4.2–12.5b |
| Hypertensiona | 22.1 | 31.2 | 20.4 | 18.6–19.9b |
| Cancer (all sites)ac | ||||
| Men | 527.8 | 628.2 | 398.0 | 360.5 |
| Women | 407.7 | 396.7 | 298.0 | 291.7 |
| Diabetesa | 7.1 | 12.1 | 10.5 | 8.4h |
| HIV/AIDSd | 6.4 | 60.3 | 20.8 | 4.4 |
| Kidney diseasea | 1.5 | 2.0 | 1.5 | 1.2h |
| Limited literacye | 7 | 24 | 44 | 14 |
| Limited English proficiencyf | ||||
| Asian/Pacific Islander | 51 (3.6 million) | |||
| Indo-European | 34 (3.4 million) | |||
| Spanish | 49 (13.8 million) | |||
| Living in povertyg | ||||
| Age < 18 y | 26 | 61 | 61 | 28h |
| Age 18–64 y | 20 | 43 | 46 | 25h |
| Age ≥ 65 y | 33 | 58 | 55 | 33h |
| No health insurance | 11 | 21 | 34 | 16h |
| No usual source of care | ||||
| Adults aged 18–64 y | 18 | 19 | 34 | 19 |
| Children < 18 y | 5 | 6 | 11 | 8h |
| Influenza vaccination coverage | ||||
| Age 18–49 y | 17 | 15 | 11 | 20 |
| Age 50–64 y | 35 | 28 | 25 | 28 |
| Age ≥ 65 y | 67 | 47 | 45 | 61 |
Source. National Center for Health Statistics,15,22 Pleis and Lethbridge-Çejku,23 Centers for Disease Control and Prevention,24 National Center for Education Statistics,25 Shin and Bruno,26 and DeNavas-Walt et al.27
Age adjusted.
Range represents Asian populations with lowest disease prevalence (4.2% for coronary disease) and Native Hawaiians or other Pacific Islander populations with highest prevalence (12.5% for coronary disease).23
New cases (incidence) per 100 000 population, 2004.
Adolescents and adults combined, rate per 100 000 population.
Literacy defined as below basic prose literacy or not having more than the most simple and concrete literacy skills, 2003.
Limited English proficiency defined as reporting speaking English less than “very well” among families in which a language other than English was spoken at home.
Defined as a household income below 200% of the 2005 federal poverty level.
Data for Asians only.
Many of these conditions are more prevalent among racial/ethnic minority populations (Table 1). For example, prevalence among African Americans is 1.3 to 23 times as high as among Whites for certain underlying conditions associated with a severe influenza infection; Latinos have a prevalence of diabetes 1.5 times and of HIV/AIDS 3 times that of Whites.23,24 Although average prevalence estimates are not higher for some other racial/ethnic minority categories, certain subpopulations may have an elevated prevalence.23,29,30
Suboptimal influenza vaccination coverage.
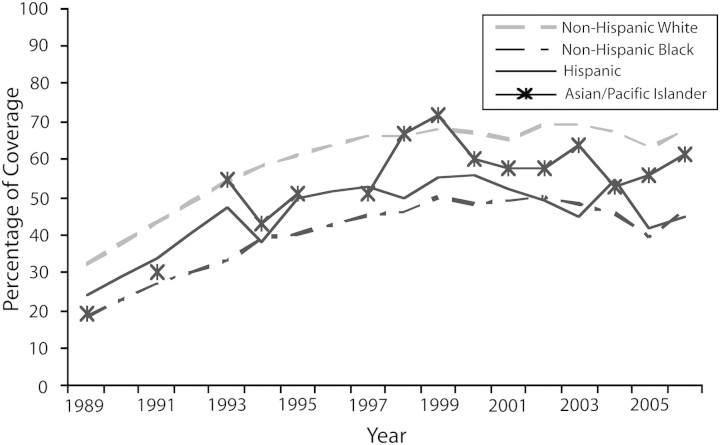
Annual influenza vaccination rates are suboptimal throughout the United States, but some minority populations have particularly low vaccination coverage (Table 1).22 Although gains in vaccination coverage were made in the early 1980s for persons 65 years and older (the age group at highest risk for seasonal influenza mortality and with the highest vaccination coverage), coverage rates leveled off by the late 1990s (Table 1; Figure 3).22 From 1989 to 2004, Latino and African American older persons consistently experienced 10% and 20% lower vaccination coverage, respectively, than did their White contemporaries. During the same period, vaccination coverage estimates for Asian/Pacific Islander older persons derived from relatively smaller samples were not significantly different from estimates for elderly Whites (Figure 3).
FIGURE 3.
Annual influenza vaccination coverage among persons aged 65 years and older by race/ethnicity: United States, 1989–2006.
Source. Centers for Disease Control and Prevention.22
If the racial/ethnic gap in annual influenza vaccination coverage among the elderly were closed by an influenza vaccination infrastructure that ensured access and use for all, 1880 annual influenza-related deaths among African American and Latino elderly persons might be prevented.31,32 Furthermore, if all populations met the Healthy People 201033 objective of 90% influenza vaccination coverage, a total of 11 840 annual influenza deaths might be prevented.31,32
Reasons for the substantial racial/ethnic disparity in influenza vaccination are not fully understood, but they likely involve many factors.34–36 One recent study observed similar rates of medical encounters during influenza vaccination weeks that were not vaccine-initiated for African American, Latino, and White patients, but markedly fewer vaccination-initiated only visits for African Americans.36 Another study found similar vaccine acceptance rates for African Americans and Whites who were systematically offered vaccine in the provider setting.37 These studies suggest that acceptance in the clinical setting may be similar but that these groups may differ in vaccination behaviors, possibly because of lack of access to vaccination-only visits.
Influenza complications.
More underlying health conditions are associated with higher complication rates from influenza. A recent population-based study of influenza hospitalizations found higher hospitalization rates among African American and Latino than among White children, although the differences were not statistically significant.38 In addition, secondary bacterial pneumonia, a major contributor to complications of influenza28 and pandemic influenza–related deaths,39,40 also occurs more often among racial/ethnic minority populations. Pneumococcal pneumonia is known to occur more often among racial/ethnic minorities and sometimes occurs in these populations without underlying health conditions.41–45 Explanations may include less access to and use of prevention and control interventions, indicated by lower pneumococcal vaccination coverage46 and differential access to health care,15 which may also affect antibiotic use. Influenza-associated pneumonia is also caused by staphylococcal infections, including methicillin-resistant Staphylococcus aureus pneumonia.47,48 Staphylococcal infections, including methicillin-resistant strains,49 are more common among some racial/ethnic minority populations,50 presumably because of higher rates of homelessness, incarceration, and residence in public housing.51,52
PANDEMIC VACCINATION COVERAGE
Influenza vaccination during a pandemic may differ from seasonal vaccination, in which most influenza vaccination takes place in a health care provider setting. Rather, it may initially require the use of public health–driven, large-scale vaccination clinics when demand for the vaccine is highest. However, an improved routine influenza vaccination infrastructure that ensures access to and uptake of vaccine for all could be built on to create a vaccination response system for pandemic influenza. In addition, vaccination may eventually shift to private-sector or routine health care administration. The timing of this shift may be a function of vaccine availability. Vaccination in large-scale vaccination clinics is different than usual clinical settings because it may require greater effort by individuals to seek it out. Thus, differences in vaccine-seeking behavior could exacerbate existing disparities, and any differences in vaccine acceptance would also worsen disparities. Outreach to populations known to have low influenza vaccination coverage during the interpandemic period will be crucial so that they understand the rationale for priority groups,53 know when they can be vaccinated, and know where to seek vaccination. Efforts to reach those who may not seek vaccination will likely be necessary.
The successful annual influenza campaigns and community engagement achieved by the Racial and Ethnic Adult Disparities Immunization Initiative (READII) and the Venue-Intensive Vaccines for Adults (VIVA) projects provide important lessons for efficient and effective planning for large-scale, mass vaccination during a pandemic, especially in their grassroots communication strategies. Routine communication approaches may be insufficient to ensure that racial/ethnic minority populations have equal access to information that will prompt effective action. For instance, to improve influenza and pneumococcal vaccination among African American and Latino older persons, READII sites in Chicago, Illinois; Milwaukee, Wisconsin; Hinds County (Jackson), Mississippi; Rochester, New York; and San Antonio, Texas, focused on developing local buy-in, engaging stakeholders and community partners, and using evidence-based, proven interventions with providers and communities.54 Each of the 5 READII sites developed community plans, convened focus groups of consumers and providers to develop effective messages for African American and Latino older persons, led community rollouts (health fairs, media events, and featured speakers), and evaluated activities. READII resulted in new partnerships among local public health agencies and communities that continued after the projects ended and possibly could be used to plan for pandemic interventions, including large-scale vaccination.
The VIVA project engaged economically disadvantaged New York City communities of East Harlem and the Bronx through a community-based participatory approach to increase interest in influenza vaccination during seasonal influenza periods; to provide free vaccine in clinics, street venues, and private homes; and to develop, implement, and assess rapid vaccination that could be used during an influenza pandemic among hard-to-reach racial/ethnic minority populations aged 19 years or older (including homebound older persons).55
To more accurately estimate the size of targeted populations for these interventions, enumeration was carried out at venues and by door-to-door sampling. A total of 2214 influenza vaccine doses were administered: 566 doses were given in a pilot study by 1 team (4 outreach workers and 1 clinician) in 4 neighborhoods over 8 weeks, and 1648 doses were given in a rapid vaccination study by 4 teams (each with 2 nurses and 4 outreach workers) in 4 other neighborhoods over 10 days. Both targeted and nontargeted persons were vaccinated: nearly half of persons opening the door received a vaccine, and nearly half of these were members of hard-to-reach populations. Vaccination provided on the street, in community-based organizations, and through door-to-door efforts was accepted by the population; the same methods might increase vaccination coverage among hard-to-reach populations during an influenza pandemic. In general, a major challenge for large-scale vaccination may be in identifying sufficient staff if volunteers are unavailable; this is also true if culturally competent staff from racial/ethnic minority communities are unavailable.
ECONOMIC CONSIDERATIONS
Negative economic effects may occur disproportionately among racial/ethnic minority populations during and after a pandemic. Many members of these populations live below or near the federal poverty level and have few financial resources, including economic assets to use during a protracted pandemic. Thus they are at risk because they cannot stockpile food and clean water or pay for utilities, transportation, and shelter if they cannot work while complying with home isolation or quarantine recommendations.6 Many members of minority populations, particularly African Americans, Latinos, and some Asians, are employed in the service industry,56 which is likely to be most affected by an economic downturn caused by a pandemic.
African American families are more likely to be headed by single parents, who are the sole source of income for the household and often hold low-paying jobs.57 This household structure places the entire family at greater economic jeopardy and limits their ability to carry out pandemic interventions.6 During Hurricane Katrina, such families sought shelter at home or in available shelters because they were unable to evacuate before the storm and could not afford to evacuate to a hotel and pay for a room.58 Furthermore, the higher risk of influenza-related mortality may leave more racial/ethnic minority children orphaned and dependent on social services for support during a pandemic. A well-described consequence of the HIV epidemic in many African countries is a high rate of children orphaned because their parents died of the disease.59
Understanding and addressing the unique historical contexts, cultures, and social networks, as well as the often low socioeconomic status, of many racial/ethnic minority populations is essential to preparing and responding to an influenza pandemic in these communities. Therefore, public health professionals, emergency managers, and other stakeholders need to include representatives from racial/ethnic minority communities to inform their planning and response and, where appropriate, to adapt strategies to the context of diverse minority communities.10 Racial/ethnic minority communities have many members who live below or near the federal poverty threshold; they may also have more crowded households, have limited English proficiency or limited literacy, be uninsured, have no usual source of care, and lack access to new health care information (Table 1).15,25–27,60 Mass health messages for the general population may need to be adapted to the language, culture, health literacy, and vaccine-seeking behavior of different populations and for their media channels and social networks.10,60
STAKEHOLDERS MEETING
The CDC convened a meeting of stakeholders on May 1 and 2, 2008, to (1) assess barriers likely to be encountered by racial/ethnic minority populations in implementing pandemic influenza interventions and (2) provide suggestions on how racial/ethnic minority populations and their families, communities, and service providers can fully undertake pandemic mitigation interventions. Invitations were sent to stakeholders named on lists provided by the CDC Office of Minority Health and Health Disparities and the Racial and Ethnic Minority Subgroup of the CDC Pandemic Influenza Working Group on Vulnerable Populations. Travel expenses were reimbursed for stakeholders who needed assistance. Attendees were leaders and individuals with experience in protecting the health of racial/ethnic minority populations and advancing the goal of eliminating racial/ethnic disparities in health. They were local and state directors of public health agencies and other public health officials; health care providers from academia, clinical practices, and national professional associations; emergency response professionals at state and local governmental levels; academic researchers; members of racial/ethnic minority populations; and directors and leaders of community- and faith-based organizations, national public health associations, professional and voluntary associations, and grassroots and advocacy organizations.
For racial/ethnic minority populations, stakeholders identified barriers to adopting pandemic influenza interventions: fewer financial resources; limited access to health care; diversity of beliefs; distrust of medical, research, or governmental institutions; limited community partnerships; lack of tailored and culturally and linguistically competent education and communications; and limited inclusion of racial/ethnic minority populations in planning for pandemic influenza (Table 2).
TABLE 2.
Barriers to and Suggestions for Fully Undertaking Pandemic Influenza Interventions Among Racial/Ethnic Minority Populations: Stakeholders Meeting, May 1–2, 2008
| Pandemic Mitigation Interventionsa | Barriers Identified by Stakeholders | Stakeholder Suggestions to Protect Racial/Ethnic Minority Populationsb |
| Use of antiviral medication and prepandemic and pandemic vaccines (pharmaceutical interventions) | Lack of inclusive preparedness and response plans and engagement of stakeholders | Include racial/ethnic minority populations, their service providers, and trusted community leaders in all aspects of preparedness planning and response plans for a pandemic. |
| Community characteristics (e.g., limited access to health care, economically distressed, chronic stress, diversity of beliefs, mistrust and distrust of government and health officials, limited knowledge, and language and cultural barriers) | Develop a strong public health system and community health system, including outreach activities to racial/ethnic minority populations. | |
| Limited initial supply and lack of a transparent system for allocation and distribution | Create a transparent system for ethical and equitable allocation and distribution of an adequate supply of pharmaceutical interventions for ensuring access (particularly among uninsured) and improving acceptance of interventions. | |
| Potential for real or perceived inequitable allocation because of limited priority groups for initial targeting of antiviral medications and prepandemic and pandemic vaccines | Provide culturally competent and low-literacy prepandemic educational and communication materials across diverse racial/ethnic minority populations with effective messages (e.g., visual ads with simple instructions) and multiple channels. Channels should include trusted sources of information (e.g., community members and organizations) ethnic media, comic books, radio, and television). | |
| Nonacceptance of antiviral medication and vaccines | ||
| Limited culturally and linguistically competent communication | ||
| Some erosion of public health infrastructure and safety net | Strengthen public health infrastructure through an adequate investment to support and sustain a coordinated response from the public health and community health systems using CBOs, FBOs, NGOs, service providers, and other stakeholders. | |
| Isolation of sick persons, quarantine of contacts, good hygiene practices, and use of PPDs | Limited individual and community financial resources to stockpile food and water and to prepare a family survival kit | Educate early about isolation, quarantine, hygiene, and use of PPDs, building on education and communication focusing on behavioral change and not merely on increasing knowledge (e.g., hand washing as a means of protecting self and family from deadly virus). |
| Lack of strong community partnerships | Establish social policies (at multiple levels) to address survival needs of vulnerable racial/ethnic minority populations. | |
| Self-interest of individual or family for survival: need either to go to work to keep job or to stay home with children | Develop partnerships with nontraditional public health partners who are stakeholders (e.g., businesses and American Red Cross). | |
| Undocumented immigrants with stigma, fear of deportation, and consequent fear of self-identification as pandemic influenza cases or contacts | Ensure adequate supply, distribution and use of PPDs through a clean stamps program for PPDs. | |
| Lack of information about PPDs and potential for inequitable supply and distribution | ||
| School closure, workplace policies, and avoidance of public gatherings | Lack of adequate community preparedness, response planning, and community engagement | Create or strengthen preparedness and response plans now for schools, workplaces, FBOs, and CBOs. |
| Challenges associated with school closure, including free lunches, educational needs, and supervision of students (e.g., parents with multiple jobs) | Establish key community partnerships with schools, businesses, CBOs, FBOs, programs such as Meals on Wheels, healthy volunteers, and students (from local universities and middle and high schools, outside of study time) to assist with food distribution and educational campaigns. | |
| Inadequate workplace policies, especially for small businesses (e.g., rules or policies to address worker return, limited worker benefits, job security, low wages, child care, and undocumented workers) | Use education and communication materials following previously mentioned stakeholder recommendations and building on existing systems to alert children, their families, teachers, employers, employees, CBOs, and FBOs. | |
| Unclear restrictions on public gatherings (e.g., need for education and planning with event planners such as FBOs, CBOs, and NGOs before the canceled event) and need to maintain community and family networking at social gatherings, mental health issues, and managing deaths and funerals (relying heavily on FBOs, but restructuring large gatherings alters FBOs’ potential to respond) | ||
| Ineffective education and communication | ||
| Mass communication of pandemic status, affected communities, risks and recommended actions | Lack of phone, no phone lines for persons with limited English proficiency, and lack of translation and interpretation services | Have open communication between community and leaders of city, county, and public health agencies that includes consistent engagement of all sectors, identification and translation of best practices into public health interventions with ample resources. |
| Community discomfort and distrust about reporting cases, differentiated and segregated areas, false sense of security, and changing demographics | Recognize everyone's expertise and unique roles in the community, including the development of a registry that lists the agencies, services, and vulnerable populations and their barriers and assets. |
Note. CBO=community-based organization; FBO=faith-based organization; NGO=nongovernmental organization; PPD=personal protective device.
Pandemic mitigation interventions are listed in order of discussion by stakeholders.
Suggestions from stakeholders are listed in order of response and may apply to more than 1 pandemic mitigation intervention. Suggestions are for racial/ethnic minority populations, their families, service providers, and other stakeholders.
The attendees also suggested how to enable racial/ethnic minority populations, their service providers, and other stakeholders to more effectively undertake pandemic mitigation interventions: encourage full participation of racial/ethnic minority populations, their service providers, and trusted community leaders in all aspects of preparedness and response planning in a coordinated way, especially when planning for surveillance of ill persons and their contacts, isolation and quarantine, assessment of community needs and assets, and social distancing. The stakeholders also identified ways to strengthen public health and community health systems for ensuring provision of safety net services, minimizing economic burdens through social policies that address income and job loss, and maximizing access to food, water, and shelter (Table 2).
Responsibilities for implementing these suggestions are outlined in the national strategy and implementation plan described by Santibañez et al. in this issue.4 Responsibility for preparedness and response rests primarily with local, state, tribal, territorial, and federal public health and emergency response agencies and with policymakers and decision makers at every level of government who are responsible for funding these activities.60 The private sector, individuals, families, and communities also have roles to play in keeping themselves, their families, and others in the community protected.
Inclusion of racial/ethnic minority communities in planning will help such communities realistically prepare for a pandemic. Participants suggested that careful and consistent inclusion of racial/ethnic minority populations, their providers, and their leaders in preparedness planning and response could allay distrust and ensure successful implementation of mitigation interventions in minority communities. Inclusion of these targeted populations in planning and response was considered important also because some members of these communities perceive that governments have available resources to meet their needs but are concerned about whether they will be allocated fairly.
CONCLUSIONS
Despite substantial gains since the 1918 pandemic in reducing mortality, improving health conditions that worsen the effects of influenza, increasing biological and epidemiological knowledge of the influenza virus, instituting international microbial and influenza surveillance systems, and developing antiviral medications that may reduce the severity of influenza if taken early and antibiotics that can treat secondary infections, during a pandemic racial/ethnic minority populations may still disproportionately suffer from severe influenza illness and death. Several factors will likely contribute: higher risk for exposure to pandemic influenza and for complications, disparities in susceptibility, less access to health care services and treatment, and a greater social risk with less ability to undertake pandemic interventions.
Available data suggest that an increased risk of adverse health outcomes is likely among minority populations during a pandemic: they experienced disproportionately poor health outcomes and greater barriers to care during both pandemic and annual pneumonia and influenza illnesses, including higher mortality, more complications, limited access to health care, lower annual influenza vaccination rates, and greater socioeconomic, cultural, educational, and linguistic obstacles to adoption of pandemic interventions. These health and social challenges place racial/ethnic populations at very high risk for poor health in a pandemic.
During the initial wave of a pandemic, the level of and adherence to pandemic mitigation interventions will largely determine the extent of influenza transmission, morbidity, and mortality until a pandemic vaccine is widely available for the general population. When such a vaccine appears and proves to be highly efficacious, it will play an important role in containing the pandemic virus for all communities, including racial/ethnic minority communities. Effective strategies for reaching racial/ethnic populations will be vital and may include the interventions used in successful large-scale annual vaccination programs and in the READII and VIVA projects.34,36,37,54,55
To minimize differential impact in an influenza pandemic, stakeholders suggested that racial/ethnic minority populations and communities must be included fully as partners in implementing all aspects of pandemic preparedness and response, especially in planning, identifying needs and local resources, designing local policies and procedures, and responding within their communities in a coordinated way. Participation of racial/ethnic minority populations should include input that addresses the socioeconomic, cultural, educational, and linguistic barriers faced by these populations, including intraracial differences. For partnerships to be successful, public health and emergency management agencies should engage racial/ethnic minority communities at the national, state, and local levels and allocate funding to support the planning process. Social safety net policies and procedures are needed to meet survival needs, including access to clean water, sufficient food, shelter, and utilities. Equitable allocation of scarce resources, including antiviral medications and vaccines, will also be paramount. Success in meeting the survival needs of some racial/ethnic minority populations may determine the extent to which community mitigation interventions are successful in stopping and slowing transmission of the pandemic virus in the United States.
Suggestions made by a diverse group of stakeholders for minimizing unnecessary transmission of pandemic influenza in the United States are essential for protecting racial/ethnic minority populations from adverse health consequences. A major step is community participatory planning, as described by Metzler et al. in an upcoming issue.61 This type of community mobilization is an essential public health service and should be ongoing to ensure that stakeholders can respond effectively during emergencies.62 Increasing awareness of community partners is under way in response to the new influenza A(H1N1) outbreak in the United States. Although not all possible stakeholders were engaged in the CDC meeting, suggestions from those who participated represent a full response to pandemic influenza and indicate that public health practitioners and community health systems should plan early. Many aspects of such planning can be applied to other public health emergencies.
Acknowledgments
Support for the expert meeting was provided by the Influenza Coordination Unit, Coordinating Center for Infectious Diseases, CDC.
We are especially grateful to the panel of experts on racial/ethnic minority populations at the CDC stakeholders’ meeting, “Pandemic Influenza Preparedness and Response in Selected Vulnerable Populations”: Virginia Caine, Marion County Health Department and Indiana University School of Medicine, IN; Patricia McManus, Black Health Coalition of Wisconsin, Inc, Milwaukee; Eduardo Cusicanqui, National Council of La Raza, Washington, DC; Albert W. Morris Jr, National Medical Association, Washington, DC; Marta Gill, Montgomery County Public Health Service, Department of Health and Human Services, Silver Spring, MD; Ho Luong Tran, Asian and Pacific Islander American Health Forum, San Francisco, CA; Perry Pong, Charles B. Wang Community Health Center, New York, NY; Christine Long, University of Rochester School of Medicine and Dentistry, NY; Georges Benjamin, American Public Health Association, Washington, DC; James Ransom, National Association of County and City Health Officials, Washington, DC; Caroline Barnhill, Association of State and Territorial Health Officials, Arlington, VA; Arthur Yancey II, Fulton County Department of Health and Wellness, Atlanta, GA; Crystal James, Interdenominational Theological Center, Atlanta, GA; Mark A. Colomb, My Brother's Keeper, Inc, Ridgeland, MS; Joanne Mauro, North Georgia Health District, Dalton; Jennifer Moorer, North Georgia Health District 1, Unit 2, Dalton; Miriam J. Burnett, Resource and Promotion of Health Alliance, Inc, Fayetteville, GA; Salah El Guindi, American Red Cross, Atlanta, GA; Edward Mihalek, Chicago Immunization Program, IL; Jalal Zuberi, Morehouse School of Medicine, Atlanta, GA; Venerable Bounnong Thomas Phommasone, Wat Lao Buddha Khanti of Atlanta, Snellville, GA; Charles Ishikawa, Cambridge Public Health Department, MA; Bill Pollard, Joyce Essien, and Michele L Pearson, CDC, Atlanta, GA; Fleda Jackson, Hoang Vu and Jejamaije E. Mujoro, Rollins School of Public Health, Atlanta, GA.
We are also grateful to Patricia Thompson-Reid, Pelagie Snesrud, and Frank Ceo for facilitating discussions of the expert panel during the meeting at the CDC; Pascale Wortley for reviewing literature on risk factors for lack of influenza vaccination and effective interventions to improve vaccination coverage; and Benedict Truman, Scott Santibañez, Toby Merlin, Carolyn Bridges, David Shay, and Walter Williams for providing editorial comments.
Note. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC. This article includes statements made by individuals at a meeting convened by the CDC for the purpose of obtaining their input. Such statements also do not necessarily represent the views of the CDC. No consensus opinions were solicited or obtained from individuals by the CDC.
Human Participant Protection
No protocol approval was necessary because no human volunteers were directly studied.
References
- 1.Cinti S. Pandemic influenza: are we ready? Disaster Manag Response. 2005;3:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. CDC influenza pandemic operation plan (OPLAN). Updated January 11, 2008. Available at: http://www.cdc.gov/flu/pandemic/cdcplan.htm. Accessed August 1, 2008.
- 3.US Department of Health and Human Services and Centers for Disease Control and Prevention. Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation in the United States—early, targeted, layered use of nonpharmaceutical interventions. Available at: http://www.pandemicflu.gov. Accessed July 16, 2008.
- 4.Santibañez S, Fiore AE, Merlin T, Redd S. A primer on strategies for prevention and control of seasonal and pandemic influenza. Am J Public Health. 2009;99(Suppl 2):S216–S224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumenshine P, Reingold A, Egerter S, Mockenhaupt R, Braverman P, Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg Infect Dis. 2008;14:709–715. Available at: http://www.cdc.gov/eid. Accessed May 31, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blendon RJ, Koonin LM, Benson JM, et al. Public response to community mitigation measures for pandemic influenza. Emerg Infect Dis. 2008;14:778–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bouye K, Truman BI, Hutchins S, et al. Pandemic influenza preparedness and response among public-housing residents, single-parent families, and low-income populations. Am J Public Health. 2009;99(Suppl 2):S287–S293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Census Bureau. Population estimates. Table 3: annual estimates of the population by sex, race, and Hispanic origin for the United States: April 1, 2007, to July 1, 2007. Available at: http://www.census.gov/popest/national/asrh/NC-EST2007/NC-EST2007-03.xls. Accessed October 2, 2008.
- 9.Groom AV, Jim C, LaRoque M, et al. Pandemic influenza preparedness and vulnerable populations in tribal communities. Am J Public Health. 2009;99(Suppl 2):S271–S278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrulis DP, Siddiqui NJ, Gantner JL. Preparing racially and ethnically diverse communities for public health emergencies. Health Aff (Millwood). 2007;26:1269–1279. [DOI] [PubMed] [Google Scholar]
- 11.Fothergill A, Maestas EG, Darlington JD. Race, ethnicity and disasters in the United States: a review of the literature. Disasters. 1999;23:156–173. [DOI] [PubMed] [Google Scholar]
- 12.Rivera JD, Miller DS. Continually neglected: situating natural disasters in the African American experience. J Black Stud. 2007;37:502–522. [Google Scholar]
- 13.Levine RS, Briggs NC, Husaini BA, Hennekens CH. Geographic studies of Black-White mortality. In: Satcher D, Pamies RJ, eds. Multicultural Medicine and Health Disparities. New York, NY: McGraw-Hill; 2005:33–104. [Google Scholar]
- 14.Byrd WM, Clayton LA. An American Health Dilemma: Race, Medicine, and Health Care in the United States, 1900–2000. New York, NY: Routledge; 2000:157. [Google Scholar]
- 15.National Center for Health Statistics. Health, United States, 2007. Available at: http://www.cdc.gov/nchs/data/hus/hus07.pdf. Accessed July 15, 2009.
- 16.Centers for Disease Control and Prevention. CDC wonder: mortality underlying cause, 1999–2005. Available at: http://wonder.cdc.gov/mortSQL.html. Accessed August 1, 2008.
- 17.Garrett TA. Pandemic economics: the 1918 influenza and its modern-day implications. Federal Reserve Bank St Louis Rev. 2008;90:75–93. [Google Scholar]
- 18.Frost WH. Statistics of influenza morbidity: with special reference to certain factors in case incidence and case fatality. Public Health Rep. 1920;35:584–597. [Google Scholar]
- 19.Osterholm MT, Hedberg CW. Epidemiology of infectious diseases. In: Mandell LE, Bennett MA, Dolin LI, eds. Principles and Practice of Infectious Diseases. 6th ed Philadelphia, PA: Elsevier; 2000:Chap 12. Available at: http://elib.cdc.gov:2149/das/book/body/111003822-2/0/1259/93.html&tocnode=51376013&fromURL=93.html#4-u1.0-B0-443-06643-4.X5001-6–section3_409. Accessed November 20, 2008. [Google Scholar]
- 20.Dushoff J, Plotkin JB, Vibroud C, Earn DJD, Simonsen L. Mortality due to influenza in the United States—an annualized regression approach using multiple-cause mortality data. Am J Epidemiol. 2006;163:181–187. [DOI] [PubMed] [Google Scholar]
- 21.Thompson WW, Shay DK, Weintraub E. Mortality associated with influenza and respiratory synctial virus in the United States. JAMA. 2003;289:179–186. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. Table: self-reported influenza vaccination coverage trends 1989–2006 among adults by age group, risk group, race/ethnicity, health-care worker status, and pregnancy status, United States, National Health Interview Survey (NHIS). Available at: http://www.cdc.gov/flu/professionals/vaccination/pdf/vaccinetrend.pdf. Accessed July 22, 2008.
- 23.Pleis JR, Lethbridge-Çejku M. Summary health statistics for U.S. adults: National Health Interview Survey, 2006. Vital Health Stat 10 2007 Dec(235):1–153. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_235.pdf. Accessed September 4, 2008. [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. HIV Surveillance Report, 2006. Vol 18. Atlanta, GA: US Department of Health and Human Services; 2008. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2006report/pdf/2006SurveillanceReport.pdf. Accessed January 27, 2009. [Google Scholar]
- 25.National Center for Education Statistics. National Assessment of Adult Literacy (NAAL): A First Look at the Literacy of America's Adults in the 21st Century. Washington, DC: US Department of Education, Institute of Education Sciences; 2006:Figure 8. NCES 2006-470. Available at: http://nces.ed.gov/NAAL/PDF/2006470.pdf. Accessed July 22, 2008. [Google Scholar]
- 26.Shin H, Bruno R. Language Use and English-Speaking Ability: 2000. Washington, DC: US Census Bureau; 2003:2, Figure 2. Available at: http://www.census.gov/prod/2003pubs/c2kbr-29.pdf. Accessed July 22, 2008. [Google Scholar]
- 27.DeNavas-Walt C, Proctor B, Smith J. Income, poverty and Health Insurance Coverage in the United States, 2006. Washington, DC: US Census Bureau; 2007. Available at: http://www.census.gov/prod/2007pubs/p60-233.pdf. Accessed July 22, 2008. [Google Scholar]
- 28.Fiore AE, Shay DK, Border K, et al. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2008. MMWR Recomm Rep. 2008;57(RR-7):1–60. [PubMed] [Google Scholar]
- 29.National Cancer Institute. Surveillance and epidemiology end results: SEER stat fact sheets. Available at: http://seer.cancer.gov/statfacts/html/livibd.html. Accessed August 13, 2009.
- 30.Miller BA, Chu KC, Hankey BF, Ries LAG. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19:227–256. 27, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fiscella K, Dressler R, Meldrum S, Holt K. Impact of influenza vaccination disparities on elderly mortality in the United States. Prev Med. 2007;45:83–87. [DOI] [PubMed] [Google Scholar]
- 32.Fiore AE, Wortley PM, Bridges CB. Missed opportunities for the prevention of influenza. Prev Med. 2007;45:88–89. [DOI] [PubMed] [Google Scholar]
- 33.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Department of Health and Human Services; 2000. Available at: http://web.health.gov/healthypeople/document/. Accessed August 10, 2009. [Google Scholar]
- 34.Williams WW, Hutchins SS, Orenstein WA, Rodewald L. Immunization and preventive care. In: Satcher D, Pamies RJ, eds. Multicultural Medicine and Health Disparities. New York, NY: McGraw-Hill; 2005:233–249. [Google Scholar]
- 35.Fiscella K. Commentary—anatomy of racial disparity in influenza vaccination. Health Serv Res. 2005;40:539–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40:517–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schwartz KL, Neale AV, Northrup J, et al. Racial similarities in response to standardized offer of influenza vaccination. J Gen Intern Med. 2006;21:346–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iwane MK, Edwards KM, Szilagyi PG, et al. Population-based surveillance for hospitalizations associated with respiratory syncytial virus, influenza virus, and parainfluenza viruses among young children. Pediatrics. 2004;113:1758–1764. [DOI] [PubMed] [Google Scholar]
- 39.Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198:962–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCullers JA. Planning for an influenza pandemic: thinking beyond the virus. J Infect Dis. 2008;198:945–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Keyserling HL. Prevention of pneumococcal disease in children. Available at: http://cme.medscape.com/viewprogram/1807_pnt. Accessed April 7, 2009.
- 42.Nuorti JP. Epidemiology of invasive pneumococcal disease in adults: implications for prevention (2000). Available at: http://ethesis.helsinki.fi/julkaisut/laa/kliin/vk/nuorti/. Accessed May 8, 2009.
- 43.Breiman RF, Spika JS, Navarro VJ, Darden PM, Darby CP. Pneumococcal bacteremia in Charleston County, South Carolina. A decade later. Arch Intern Med. 1990;150:1401–1405. [PubMed] [Google Scholar]
- 44.Bennett NM, Buffington J, LaForce FM. Pneumococcal bacteremia in Monroe County, New York. Am J Public Health. 1992;82:1513–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pastor P, Medley F, Murphy TV. Invasive pneumococcal disease in Dallas County, Texas: results from population-based surveillance in 1995. Clin Infect Dis. 1998;26:590–595. [DOI] [PubMed] [Google Scholar]
- 46.National Center for Health Statistics. Table: Self-reported pneumococcal vaccination coverage trends 1989–2006 among adults by age group, risk group, race/ethnicity, health-care worker status, and pregnancy status, United States, National Health Interview Survey (NHIS). Available at: http://www.cdc.gov/flu/professionals/vaccination/pdf/pneumococcal-vaccinetrend.pdf. Accessed September 4, 2008.
- 47.Hageman JC, Uyeki TM, Francis JS, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003–04 influenza season. Emerg Infect Dis. 2006;12:894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kallen AJ, Brunkard J, Moore Z, et al. Staphylococcus aureus community-acquired pneumonia during the 2006 to 2007 influenza season. Ann Emerg Med. 2009;53:358–365. [DOI] [PubMed] [Google Scholar]
- 49.Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. [DOI] [PubMed] [Google Scholar]
- 50.Tennessee Department of Health and Infections TaskForce. Methicillin-resistant Staphylococcus aureus (MRSA) infections. 2008. Available at: http://health.state.tn.us/Downloads/MRSAreport307.pdf. Accessed May 8, 2009.
- 51.Hota B, Ellenbogen C, Hayden MK, Aroutcheva A, Rice TW, Weinstein RA. Community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections at a public hospital: do public housing and incarceration amplify transmission? Arch Intern Med. 2007;167:1026–1033. [DOI] [PubMed] [Google Scholar]
- 52.Skiest DJ, Brown K, Cooper TW. Prospective comparison of methicillin-susceptible and methicillin-resistant community-associated Staphylococcus aureus infections in hospitalized patients. J Infect. 2007;54:427–434. [DOI] [PubMed] [Google Scholar]
- 53.US Department of Health and Human Services and US Department of Homeland Security. Guidance on allocating and targeting pandemic influenza vaccine. Available at: http://www.pandemicflu.gov/vaccine/allocationguidance.pdf. Accessed October 7, 2008.
- 54.Kicera TJ, Douglas M, Guerra FA. Best-practice models that work: the CDC's Racial and Ethnic Adult Disparities Immunization Initiative (READII) Programs. Ethn Dis. 2005;15(2 Suppl. 3):S3-S17–S3-S20. [PubMed] [Google Scholar]
- 55.Coady MH, Galea S, Blaney S, Ompad DC, Sisco S, Vlahov D. Project VIVA: a multilevel community-based intervention to increase influenza vaccination rates among hard-to-reach populations in New York City. Am J Public Health. 2008;98:1314–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.US Bureau of Labor Statistics. Household data averages, 2007. Available at: http://www.bls.gov/cps/cpsaat18.pdf. Accessed September 3, 2008.
- 57.US Census Bureau. American community survey, 2006. Available at: http://www.census.gov/acs. Accessed October 2, 2008.
- 58.Gabe T, Falk G, McCarty M, Mason VW. Hurricane Katrina: Social-Demographic Characteristics of Impacted Areas. CRS Report for Congress. November 4, 2005. Available at: http://www.gnocdc.org/reports/crsrept.pdf. Accessed September 23, 2008.
- 59.AVERT. AIDS orphans. Available at: http://www.avert.org/aidsorphans.htm. Accessed May 8, 2009.
- 60.ASTHO. At-risk populations and pandemic influenza: planning guidance for state, territorial, tribal, and local health departments. June 2008. Available at: http://www.astho.org/Search.aspxs=Pandemic%. Accessed August 10, 2009.
- 61.Metzler M, Jones CP, Pearson ML, Stevenson B, Lewis Y. Reducing vulnerability and achieving health equity in pandemic influenza preparedness and response through community-based participatory approaches. Am J Public Health. In press. [Google Scholar]
- 62.Centers for Disease Control and Prevention. Core Public Health Functions Steering Committee. 10 Essential services of public health. Available at: http://www.cdc.gov/od/ocphp/nphpsp/EssentialPHServices.htm. Accessed November 20, 2008.