Abstract
Objectives. We used Bronfenbrenner's ecological systems theory to identify factors that predicted never or sometimes using condoms in a multiethnic cohort of adolescent mothers.
Methods. We interviewed adolescent mothers within 48 hours of delivery and surveyed them 6 and 12 months after delivery (n = 636). We used multinomial logistic regression to identify individual-, dyad-, family-, and peer and community-level factors associated with never or sometimes using versus always using condoms during intercourse at 12 months postpartum.
Results. Pregnancy status, partner refusal to use condoms, intimate partner violence, and race/ethnicity predicted both never and sometimes using condoms. Condom use 6 months earlier and church attendance also predicted never using condoms, whereas maternal monitoring was an additional predictor for sometimes using condoms.
Conclusions. Overlapping yet distinct risk profiles predicted never or sometimes using versus always using condoms. Factors from multiple levels of influence affected the condom use behaviors of adolescent mothers indicating that multilevel interventions are needed to promote safer sexual practices among these young women.
US female adolescents between the ages of 15 and 19 years have the highest rates of sexually transmitted infections (STIs) when compared with other age and gender groups, and minority, pregnant, and parenting adolescents are at particularly high risk.1,2 In fact, depending on the population studied, 14% to 39% of adolescent mothers have an STI diagnosis within 6 to 10 months of delivery.3 These high rates of STIs are directly related to the significant proportions of adolescent mothers who report never or inconsistently using condoms (32%–63%).3 Given the frequent occurrence of STIs among young women and the negative and potentially severe sequelae of STIs, a greater understanding of the factors associated with condom use in this high-risk population is needed.
Studies of pregnant, never pregnant, and parenting adolescents have found that condom use is influenced by multiple factors, including hormonal contraceptive use,4–7 pregnancy status,4,8 self-esteem,9,10 drug and alcohol use,11–13 type of relationship with one's partner,5,6,10,14 living situation,11,15 intimate partner violence,16,17 and peers’ beliefs.11,18,19 Other factors that may be related to condom use include race/ethnicity,4,20,21 HIV/STI or condom-specific knowledge,4,8,11,20,22 sexual history,4,11,23,24 and religiosity,4,9,25–27 although the results of studies examining these factors have been equivocal. Few studies on adolescent mothers have simultaneously focused on more than one level of influence to include the dyad, family, and larger community.
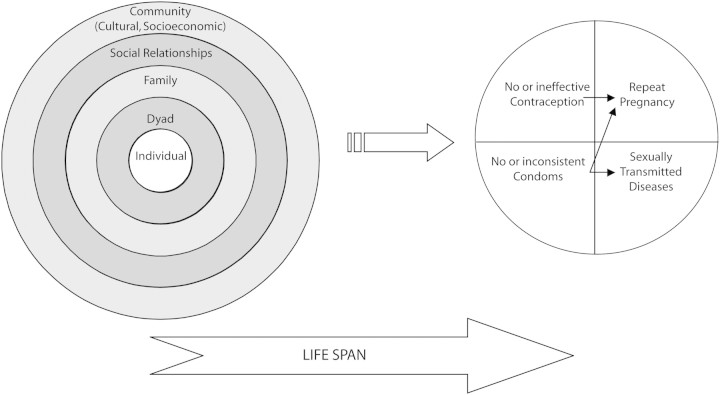
Bronfenbrenner's ecological systems theory (EST) has recently been used to better understand the sexual behavior of nonparenting and parenting adolescents.3,11,28,29 This theory asserts that the individual is nested within a set of interconnected domains (individual, dyad, family, social, and community) that both directly and indirectly influence the behavior of the individual.30–32 EST organizes risk factors by domain so that they can be targeted separately and in parallel, which allows program planners to identify strategies at each level of influence and develop more effective interventions. This is critical because recent evidence suggests that multilevel intervention approaches are essential to elicit behavioral changes.33 Figure 1, which is taken from a recent review by Meade and Ickovics,3 illustrates how the EST model applies to the sexual behaviors of adolescent mothers. Factors at the individual, dyad, and peer and community levels were found to predict rapid repeat pregnancy within 24 months after delivery in a previous study examining the same multiethnic cohort of adolescent mothers.29
FIGURE 1.
Ecological model of sexual risk.
Note. Reprinted from Meade and Ickovics.3
We sought to further apply EST to determine the multiple levels of influence (individual, dyad, family, social, and community) that predict never or sometimes using condoms at 12 months after delivery among a multiethnic cohort of adolescent mothers. Note that our study focused specifically on the effects of multiple levels of analysis on condom use and did not attempt to construct a model that addressed the extent to which these levels of analysis affected each other; nor did our study take into account the individual's history before delivery. We used an analytic approach to generate separate profiles of factors associated with never using condoms and sometimes using condoms as compared with always using condoms. We hypothesized that significant factors would be identified from each level of influence and that the profile of factors would differ for adolescent mothers who sometimes used condoms and adolescent mothers who never used condoms.
METHODS
Our study was part of a larger longitudinal investigation into drug use among adolescent mothers34 who delivered at the University of Texas Medical Branch at Galveston between December 8, 1993, and February 28, 1996. Details of participant recruitment are reported elsewhere.34 Participants in the larger study were interviewed in the postpartum unit within 48 hours of delivery and were mailed surveys to complete 3, 6, 12, 18, and 24 months later. This secondary analysis was undertaken to examine risk factors for inconsistent condom use at 12 months after delivery; we used data collected at the baseline (delivery) interview and at the 6- and 12-month surveys.
Sample and Data Collection
In all, 932 adolescents completed the baseline interview. A total of 636 participants completed both the 6- and 12-month surveys and were used in the analysis predicting condom use. Selected demographic characteristics of the original sample and of the analysis subsample are presented in Table 1; we observed no meaningful differences between these 2 groups. A comparison of the independent variables for mothers completing the 6-month survey only and mothers completing both surveys showed that those completing both surveys (and thus who were included in the analysis) had significantly lower self-esteem and were significantly more likely to exhibit moderate to severe depressive symptoms than were mothers completing the 6-month survey only.
TABLE 1.
Selected Demographic Characteristics, by Total Sample (N = 932), 6- and 12-Month Subsamples (n = 636), and Race/Ethnicity: Texas, 1993–1998
| Total Study Population, Mean (SD) or % | 6- and 12-Month Subsamples, Mean (SD) or % | White, Mean (SD) or % | African American, Mean (SD) or % | Mexican American, Mean (SD) or % | P | |
| Age, y | 16.8 (1.165) | 16.76 (1.17) | 16.95 (1.08) | 16.55 (1.267) | 16.78 (1.13) | .002 |
| Education, y | 9.56 (1.72) | 9.58 (1.73) | 10.06 (1.496) | 9.67 (1.47) | 9.07 (1.987) | < .001 |
| Gravidity > 1 | 27.2 | 26.3 | 28.3 | 23.6 | 27.0 | .531 |
| Parity > 1 | 16.6 | 15.9 | 13.6 | 17.5 | 16.4 | .554 |
| Race/ethnicity | … | |||||
| Mexican American | 37.6 | 35.5 | 0 | 0 | 100 | |
| African American | 32.3 | 33.3 | 0 | 100 | 0 | |
| White | 30.2 | 31.1 | 100 | 0 | 0 | |
| Spanish survey | 10 | 8.5 | 0 | 0 | 23.9 | < .001 |
| Living with parent(s) at delivery | 53.1 | 55.8 | 52.0 | 67.0 | 48.7 | < .001 |
| Living with partner at delivery | 40.6 | 39.3 | 53.0 | 9.4 | 55.3 | < .001 |
| School status at delivery | ||||||
| Enrolled in school or graduated | 26.4 | 26.1 | 37.9 | 14.7 | 26.0 | < .001 |
| Dropped out before conception | 24.0 | 21.3 | 22.2 | 9.0 | 32.3 | |
| Dropped out during pregnancy | 49.6 | 52.5 | 39.2 | 76.3 | 41.7 | |
| Own mother graduated high school or has GED | 75.0 | 75.4 | 51.4 | 74.7 | 28.3 | < .001 |
| Feels like has enough money to live | 87.5 | 88.5 | 92.9 | 89.2 | 84.1 | .017 |
| Planned pregnancy | 19.0 | 17.8 | 17.7 | 9.4 | 25.7 | < .001 |
Note. GED = general equivalency diploma. P values are for comparisons among racial/ethnic subgroups of White, African American, and Mexican American adolescent mothers. For Whites, n = 198; for African Americans, n = 212; for Mexican Americans, n = 226.
The initial interview was performed in English or Spanish in a private room. The 6- and 12-month follow-up data were collected via mail, phone, or in a University of Texas Medical Branch clinic for those who had medical appointments during the follow-up interval. Participants were compensated $10 for each completed survey. A total of 84% and 80% of the distributed surveys were returned at 6 and 12 months, respectively. Surveys were reviewed for missing data, and participants were contacted to help clarify responses.
Dependent Variable
Questions on sexual behaviors were limited to the time period since the last scheduled survey. Participants reporting sexual activity were asked, “In the last 6 months, how often do you use condoms when you have sexual intercourse?” Participants answered on a 5-point Likert scale, with the answers “sometimes,” “about half the time,” and “most times” consolidated into the “sometimes” category. “Always” and “never” remained as the other 2 categories to form a 3-category dependent variable. The reference category used in later analyses was “always” use condoms.
Independent Variables
Individual-, dyad-, family-, peer and community–, and social system–level factors elicited during either the baseline interview or the 6- or 12-month follow-up survey are described in Table 2. Also shown in the table are the number of items used to measure each factor and indexes of internal consistency (Cronbach α) for those variables measured as scale scores.
TABLE 2.
Description of Independent Variables, by Level of Influence in the Ecological Systems Theory Model: Adolescent Motherhood Project, 1993–2000
| Variable | Description of Variable | No. of Items (Cronbach α) |
| Individual | ||
| Age at deliverya | Age at time of delivery | 1 |
| Self-esteemb | 10-item Rosenberg scale, how she views herself | 10 (0.87) |
| Depressive symptomsb | BDI Short Form, exhibiting symptoms of depression | 13 (0.81) |
| Alcohol, marijuana, or other drugsb | Any alcohol or drug use in the past 3 mo | 22 |
| Dropped out of schoola | Not enrolled in school at the time she got pregnant | 4 |
| Enrolled in schoolb | Enrolled in school, college, GED classes, a homebound program, or a vocational program | 2 |
| High school aspirationsb | Has high school education or responded “will complete” high school or GED | 1 |
| Long-term birth controlb | Using Depo-Provera (Pfizer Inc, New York, NY), Norplant (The Population Council, New York, NY), or intrauterine device | 16 |
| Pregnancy | Currently pregnant or trying to get pregnant | 2 |
| Pregnancy desiresb | Never again wants another child versus wants more children | 1 |
| Concern over contracting an STI or HIVb | On a 5-point scale, greater concern being “always” and “a lot” worried about either STIs or HIV | 2 |
| Perceived susceptibility to STIs or HIVb | On a 5-point scale, high susceptibility being “completely likely” and “very likely” to get an STI or HIV | 2 |
| STI risk behaviorsb | Had sex with someone she didn't know very well, someone she knew was having sex with someone else, an intravenous drug user, anal sex, > 1 partner | 5 |
| Alcohol or drugs before sexb | Drank alcohol or got high before sex | 4 |
| Dyad | ||
| Age of current partnera | Current sexual partner aged ≥ 3 y older | 1 |
| Lives with male partnerb | Resides with male partner | 2 |
| Partner's future pregnancy desiresb | Partner does not ever want another child | 1 |
| Hit by male partnerb | Hit by boyfriend or husband during an argument or while he was drunk or high, or having been hit, slapped, kicked, or physically hurt enough by a current or ex-partner to cause bruising or bleeding | 5 |
| Sexually coercedab | Ever been forced to have sexual intercourse without consent or have been forced to touch a sexual partner | 4 |
| Prior condom useb | Always, sometimes, or never used condoms at 6 mo | 1 |
| Current refusal by partner to wear condomsc | Partner refused to wear a condom during sex | 1 |
| Family | ||
| Own mother has high school educationa | Mother has GED or completed high school | 2 |
| Family supportb (scale score) | On a 5-point scale, family helped them with money, transportation, child care, information, or emotional support | 5 (0.89) |
| Overall supportb (scale score) | On a 5-point scale, others helped them with money, transportation, child care, information, or emotional support | 5 (0.89) |
| Closeness with maternal guardiana (scale score) | Feelings that she could talk to her mother or maternal guardian, felt close to her, and enjoyed spending time with her | 3 (0.68) |
| Monitoring by maternal guardiana (scale score) | Perception that her parent or guardian wants to know who she spends time with, gives clear reasons for behavior-related rules, and strictly enforces set behavior-related rules | 3 (0.86) |
| Verbal abuseb | Someone close to the participant called her hurtful names | 1 |
| Religiositya | Attends weekly services | 1 |
| Peer and Community | ||
| Perceived condom use beliefs by friendsb | Most or all friends believe people should use condoms during sexual intercourse | 1 |
| Perceived use of condoms by friendsb | Most or all friends use condoms during sexual intercourse | 1 |
| Community violencea | Carried a weapon for protection, was afraid of being hurt by others, or had seen someone attacked with a weapon | 3 |
| Race/ethnicitya | Self-classified as Mexican American, White, or African American | 2 |
| Limited economic resourcesb | Felt she did not have enough money, food, clothing, and so on, to live | 1 |
Note. BDI = Beck Depression Inventory; GED = general equivalency diploma; STI = sexually transmitted infection.
Measured at the baseline interview after delivery.
Measured at 6 months after delivery, referring to current status (e.g., self-esteem, depressive symptoms) or within the past 3 months (e.g., verbal abuse, drug use).
Measured at 12 months after delivery.
Individual factors.
The 6-month survey elicited information on individual factors including self-esteem, depressive symptoms, substance abuse, current school enrollment and future academic plans, contraceptive use, future pregnancy plans, worries about and perceived susceptibility to STIs and AIDS, and recent sexual activities. The Rosenberg Self-Esteem Scale35 was used to evaluate self-esteem, and the Beck Depression Inventory, Short Form (BDI),36 was used to assess depressive symptoms. Total scores on the 10-item Rosenberg scale ranged from 0 to 40, with higher scores indicating higher self-esteem. Those with a score of 27 or lower (the lowest quartile) were described as having low self-esteem. The 13-item BDI had total scores of 0 to 39: a total score of 8 to 39 was coded as exhibiting moderate to severe depressive symptoms, whereas a score of 0 to 7 was coded as no to mild depressive symptoms.
High-risk sexual behaviors from the 6-month survey were divided into 2 variables: sexual intercourse after the use of alcohol or drugs and STI risk behaviors. STI risk behaviors included sexual intercourse with multiple partners, sexual intercourse with an intravenous drug user, sexual intercourse with someone not well known, anal sex, and sexual intercourse with someone who was having sexual intercourse with others. Reports of engaging in 1 or more of these activities were coded as “yes.”
Dyad factors.
Information on living arrangements and intimate partner violence was examined by using data from the 6-month survey as described previously.37 Sexual coercion was defined as having been forced to have sexual intercourse without consent or having been forced to touch a sexual partner. A history of sexual coercion reported at the baseline interview and 6-month surveys was used in this analysis. Refusal by a partner to wear a condom was evaluated at the 12-month survey with participant responses of “agree” or “strongly agree” coded as “yes.”
Family factors.
Perceived family support and overall support, in terms of emotional, financial, informational, transportation, and child support, were measured by using 5 items each on a 5-point scale as previously described.38 Scores ranged from 0 to 5; those with average scores in the lowest quartile were compared with those averaging higher family and overall support. Maternal closeness and parental monitoring were measured and coded as previously reported29 and are described in Table 2.
Participants were also asked whether a family member had slapped, kicked, or physically hurt them enough to cause bleeding or had physically hit or hurt them when in a fight or when high in the past 3 months. Verbal abuse was defined as someone close to the participant having called her hurtful names in the past 3 months. Both being hit by a family member and verbal abuse were analyzed with those reporting 1 or more incidents compared with those who reported no incidents.
Peer, community, and social system factors.
Participants were also asked at the 6-month survey to report the number of times in the past 3 months they had carried a weapon for protection, were afraid of being hurt by others, and had seen someone attacked with a weapon, to determine whether community violence was present or absent in the participant's life. As previously discussed, participants self-reported their race/ethnicity as White, Mexican American, or African American at the baseline interview. Economic resources were determined to be limited if the mother stated she felt she did not have enough money, food, or clothing to live.
Statistical Analysis
We used SPSS version 14.0 for Windows (SPSS Inc, Chicago, IL) to analyze all data. Demographic characteristics were examined by using descriptive statistics; racial/ethnic differences in demographic characteristics were assessed through χ2 analyses. Pearson r and Spearman ρ correlation analyses were used to evaluate collinearity among factors. Bivariate analyses implementing the χ2 test and the Student t test were used to identify the factors with the greatest potential of influencing the outcome. Factors with a P < .2 in the bivariate analyses, or those strongly related to condom use that were identified through the literature, were entered into a multinomial regression analysis to determine the predictors of condom use at 12 months after delivery. A multinomial logistic regression analytic approach was used in place of a traditional binary logistic regression to generate separate profiles of factors associated with never using condoms and sometimes using condoms as compared with always using condoms. After the core set of predictors was determined, all remaining variables were reentered and removed 1 at a time to verify the final model.
RESULTS
Comparisons of demographic variables among racial/ethnic subgroups showed several significant differences (Table 1). No racial/ethnic differences were found by parity of more than 1, gravidity of more than 1, or experience of a repeat pregnancy within 12 months of the index delivery.
The results of the bivariate analysis, which used the Student t test and χ2 test, indicated significant relations between condom use and several independent variables from each level of influence in the EST model. Individual factors significantly associated with never or sometimes using condoms included moderate to severe depressive symptoms (P = .002), dropped out of school before first pregnancy (P = .019), limited aspirations to complete high school (P = .036), being pregnant or trying to get pregnant (P = .001), limited worry about STIs/AIDS (P = .001), never or only sometimes using condoms at 6 months (P < .001), and sexual intercourse after use of alcohol or drugs (P = .015).
Three dyad factors were significantly associated with never or sometimes using condoms at 12 months: living with a male partner (P < .001), being hit by a male partner (P = .001), and partner refusing to wear a condom (P < .001). Family factors significantly associated with never or sometimes using condoms included mother with less than high school education (P = .003), higher maternal monitoring (P = .036), and low religiosity (P = .009).
Three peer and community factors were also significantly associated with always using condoms: perceived belief of friends that condoms should be worn during sexual intercourse (P = .001), perceived use of condoms during sexual intercourse by friends (P = .028), and African American race/ethnicity (P < .001). Nearly 50% of African Americans compared with 22% and 29% of Whites and Mexican Americans, respectively, reported always using condoms at 12 months.
Factors with P < .2 in the bivariate analyses, or those strongly related to condom use that were identified through the literature, were entered into a multinomial regression analysis to determine the predictors of condom use at 12 months after delivery. The results of the final model are presented in Table 3. African Americans were more likely to report always using condoms and therefore were used as the reference category for race. One individual factor, 3 dyad factors, 2 family factors, and 1 peer and community factor were found to be independently related to condom use at 12 months. Compared with mothers who always used condoms, mothers who never and sometimes used condoms were more likely to be White, be pregnant or trying to get pregnant, have a partner that refused to wear a condom, and have experienced intimate partner violence. Additional risk factors for never using condoms as opposed to always were never and sometimes using condoms at 6 months and not attending church regularly. Higher maternal monitoring was also found to be a significant predictor of sometimes using condoms compared with always using them.
TABLE 3.
Unstandardized Regression Parameter Estimates, Adjusted Odds Ratios (AORs), and 95% Confidence Intervals (CIs) From Multinomial Logistic Regression of Significant Predictors of Condom Use at 12 Months After Delivery: Texas, 1993–1998
| Sometimes Used vs. Always Used Condoms |
Never Used vs. Always Used Condoms |
|||
| b | AOR (95% CI) | b | AOR (95% CI) | |
| Individual | ||||
| Currently pregnant or trying to conceive | ||||
| Yes | 0.98 | 2.7* (1.1, 6.7) | 1.36 | 3.9** (1.6, 9.8) |
| No (Ref) | 0 | 1.0 | 0 | 1.0 |
| Dyad | ||||
| Partner refusal to wear condom | ||||
| Yes | 1.02 | 2.76* (1.2, 6.3) | 1.69 | 5.44*** (2.4, 12.2) |
| No (Ref) | 0 | 1.0 | 0 | 1.0 |
| Condom use at 6 mo | ||||
| Not sexually active | −0.063 | 0.53 (0.2, 1.2) | 0.38 | 1.45 (0.6, 3.6) |
| Never | 0.65 | 1.92 (0.9, 4.3) | 2.86 | 17.37*** (7.1, 42.3) |
| Sometimes | 0.68 | 1.97 (1.0, 3.9) | 1.57 | 4.81*** (2.1, 11.0) |
| Always (Ref) | 0 | 1.0 | 0 | 1.0 |
| Hit by male partner | ||||
| Yes | 1.34 | 3.82* (1.4, 10.6) | 1.15 | 3.17* (1.1, 8.9) |
| No (Ref) | 0 | 1.0 | 0 | 1.0 |
| Family | ||||
| Maternal monitoring | ||||
| High | 0.76 | 2.14* (1.2, 4.0) | 0.29 | 1.33 (0.7, 2.4) |
| Low (Ref) | 0 | 1.0 | 0 | 1.0 |
| Religiosity | ||||
| Little to no church attendance | 0.29 | 1.33 (0.7, 2.5) | 0.79 | 2.21* (1.1, 4.3) |
| Attend weekly (Ref) | 0 | 1.0 | 0 | 1.0 |
| Peer and community | ||||
| Race | ||||
| White | 1.27 | 3.59*** (1.8, 7.3) | 1.10 | 3.02** (1.5, 6.2) |
| Mexican American | 0.61 | 1.84 (1.0, 3.5) | 0.65 | 1.92* (1.0, 3.7) |
| African American (Ref) | 0 | 1.0 | 0 | 1.0 |
Note. N = 502. Negelkerke Pseudo R-Square = 0.361; P < .001; total classification = 60%.
* P < .05; **P < .01; ***P < .001.
Because of the many significant racial/ethnic differences in our sample, the multinomial logit was also run without race to verify that the model was not influenced by these differences. The living with her partner factor was added to the model with a significance level of P = 0.008 on the likelihood ratio test. No other differences between the 2 models were noted.
DISCUSSION
To our knowledge, no previous empirical study has used multisystem theory to examine condom use in adolescent mothers. Our results show that factors from each level of influence in the EST model independently predicted condom use within this population. In addition, we observed overlapping yet distinct profiles of risk predicting never and sometimes using condoms versus always using condoms. These findings are important because studies of both parenting and nonparenting adolescents have shown that adolescent sexual risk behaviors, including condom use behavior, are influenced by multiple domains and that interventions to promote condom use that target single domains have met with limited success.3,11,39
Condom use behavior (sometimes and never using) at 6 months was the strongest predictor of never using condoms at 12 months but was not a significant predictor for those who sometimes used condoms. In fact, young mothers who always used condoms at 6 months continued to do so at 12 months postpartum, whereas mothers who used condoms sometimes decreased their condom use to the point of never using them by 12 months postpartum. Longitudinal condom use research in the general adolescent population has established a strong correlation between past and future condom use.40–42 Similarly, Kershaw et al.43 found no significant changes in condom use when comparing consistent with inconsistent condom users from 6 to 12 months postpartum among a sample of adolescent mothers. However, our results indicate that this was not necessarily the case in the group of sometimes users. These findings confirm the need for continued interventions well into the postpartum period, especially for those previously reporting inconsistent condom use.
Only 1 individual characteristic, being pregnant or trying to get pregnant at 12 months after delivery, was found to be significantly associated with both sometimes and never using condoms. Earlier studies of pregnant and mothering adolescents4,8,44 also reported a strong relation between inconsistent condom use and pregnancy, with a meta-analysis showing that as high as 88% of currently pregnant adolescents do not use condoms.3 Koniak-Griffin et al.18 related the failure of pregnant adolescents to use condoms to their lack of concern over contraception and inability to perceive the risk of contracting HIV or STIs. Thus, clinicians providing prenatal care services must emphasize the benefits of protection during this critical period.
Both refusal of the partner to wear condoms and intimate partner violence predicted sometimes and never using condoms at 12 months. Fear of abuse as well as a perceived lack of power or control and male dominance can severely alter a woman's ability to demand or even suggest condom use to her partner, especially among young women who are immature or inexperienced.18,45,46 The perception by some that condom use implies a lack of trust or promiscuity,18,41 particularly with steady partners, not only validates but exacerbates this issue for those women whose partners refuse to negotiate or who are prone to invoke fear. In addition to inconsistent condom use,47 intimate partner violence has been associated with rapid repeat pregnancy (pregnancy onset within 12–24 months of a previous pregnancy outcome)29,48; concurrent or prior physical, sexual, and verbal abuse38,49; an increased risk of STIs50,51; frequent and severe abuse of illicit drugs by both mother and an abusive partner38; and an increased risk of behavioral problems in children exposed to maternal intimate partner violence.52 Thus, it is imperative that screening for intimate partner violence be done throughout pregnancy and the postpartum period to ensure the safety of the mother and child and to avoid complications associated with abuse.
Parental involvement has been found to directly influence children's risk behaviors, including sexual behavior and contraceptive use.11,53–55 In our study, high maternal monitoring positively predicted occasional condom use when compared with always using a condom. Previous studies on adolescent sexual risk behaviors54,56–58 have found an inverse relation between parental monitoring and high-risk sexual behaviors and outcomes, including consistency of condom use, frequency of sexual intercourse, number of sexual partners, and STI diagnosis. Although the associations among increased parental monitoring, less frequent sexual activity, and fewer sexual partners have been explained by a decreased opportunity to engage in sexual activities, they do not explain increased condom use consistency.59,60 In our sample, higher monitoring predicted sometimes using condoms, which follows the logic that more monitoring inherently creates less opportunity for sexual encounters. Consequently, adolescents may decide to take advantage of these rare opportunities despite the absence of a condom. Further investigation is needed to fully unravel the different roles parental monitoring takes in the sexual lives of adolescent parents.
Contradictory to previous adolescent pregnancy and parenting literature,4,8,20 our study showed that race/ethnicity is an important predictor in the adolescent mother's condom use behavior. Among those who were sexually active, Mexican Americans were least likely to report using condoms at every sexual encounter, whereas African Americans were most likely to report doing so. Cultural differences between these groups may provide some insight into these findings. For example, Mexican American mothers were more likely in this sample than African Americans to be living with their partner at delivery and to report that the index delivery was planned. Neither of these variables was significantly related to condom use at 12 months once race/ethnicity was included in the model. In addition, high rates of STIs among African Americans identified in the 1990s prompted the development of interventions targeting this population subgroup.61,62 Although we are not aware of any specific interventions in our area during the time of data collection, we cannot rule out the possibility that our African American sample received more STI and HIV prevention messages than the other groups in our sample.
Several limitations of this study are noteworthy. First, the study participants were confined to those living in southeast Texas and who delivered an infant in one of the only hospitals in the area at that time to accept Medicaid. Thus, our findings may not generalize to young mothers from other socioeconomic groups or regions of the country. Second, the absence of a nonparenting group of adolescents makes it difficult to directly compare our results with the general adolescent population. Note that research comparing pregnant and parenting adolescents with their nulliparous peers has found differences between their use of contraceptives21,44; feelings of susceptibility to STIs, HIV, and pregnancy43; STI rates63; and factors that may influence subsequent risk behavior, including depression and family support.64 Third, data on STI outcomes, either through self-report or biomarkers, were not available for this study. Fourth, data were collected from only adolescent mothers and thus represent their perceptions rather than an objective view of their ecological environment. Fifth, the 3 questions used to measure community violence likely underestimated the true incidence of community violence experienced by the participants in this study. Finally, because many of the predictors were assessed 6 months before the outcome, it is possible that changes in their current partner and life circumstances during the intervening 6-month period may have affected the results.
The key findings from this study were: (1) factors from multiple spheres of influence in the lives of young mothers predict the extent to which they use condoms, (2) overlapping yet distinct profiles of risk predict sometimes using versus never using condoms at 12 months after delivery, and (3) current nonuse of condoms is strongly predicted by past failure to use condoms consistently. By understanding all the factors affecting the sexual behaviors of adolescent mothers, and the differences between the profiles, service providers and policymakers can better address the problem areas contributing to the high rates of STIs among today's youths. Interventions to promote condom use in populations of young mothers must stress the risks to the mother and the fetus of contracting an STI during pregnancy and while trying to conceive. Given the strong influence of partners and the high rates of unplanned, repeat pregnancy among young mothers previously reported,29 programs must target male resistance to using condoms in an effort to prevent both STIs and unintended pregnancies. Moreover, service providers must recognize that young women experience violence at the hands of their intimate partners and may need intensive training to both prevent the violence and effectively negotiate condom use. Finally, interventions are needed for young mothers from all cultural backgrounds, because Whites and Mexican Americans were most at risk for inconsistent condom use.
Acknowledgments
This research was supported by the National Institutes of Health, Bethesda, MD (grants DA09636 and DA08404 to C. M. W.) and by the Hogg Foundation for Mental Health, Austin, TX (grant 3777).
These findings were presented at the 134th annual meeting of the American Public Health Association (Boston, MA, November 4–8, 2006).
We thank Elizabeth Conlisk for her guidance and help during the early stages of this project.
Note. The findings presented herein do not reflect the views of either the National Institutes of Health or the Hogg Foundation for Mental Health.
Human Participant Protection
This study was approved by the Baylor College of Medicine institutional review board for human subjects.
References
- 1.Centers for Disease Control and Prevention. Trends in Reportable Sexually Transmitted Diseases in the United States, 2004. Atlanta, GA: US Department of Health and Human Services; 2005. [Google Scholar]
- 2.Berman SM, Hein K. Adolescents and STDs. : Holmes KK, Sparling PF, Mardh P, et al., Sexually Transmitted Diseases. New York, NY: McGraw-Hill; 1999:129–142. [Google Scholar]
- 3.Meade CS, Ickovics JR. Systematic review of sexual risk among pregnant and mothering teens in the USA: pregnancy as an opportunity for integrated prevention of STD and repeat pregnancy. Soc Sci Med. 2005;60(4):661–678. [DOI] [PubMed] [Google Scholar]
- 4.Koniak-Griffin D, Lesser J, Uman G, Nyamathi A. Teen pregnancy, motherhood, and unprotected sexual activity. Res Nurs Health. 2003;26(1):4–19. [DOI] [PubMed] [Google Scholar]
- 5.Plichta SB, Weisman CS, Nathanson CA, Ensminger ME, Robinson JC. Partner-specific condom use among adolescent women clients of a family planning clinic. J Adolesc Health. 1992;13(6):506–511. [DOI] [PubMed] [Google Scholar]
- 6.Ott MA, Adler NE, Millstein SG, Tschann JM, Ellen JM. The trade-off between hormonal contraceptives and condoms among adolescents. Perspect Sex Reprod Health. 2002;34(1):6–14. [PubMed] [Google Scholar]
- 7.Roye CF. Condom use by Hispanic and African American adolescent girls who use hormonal contraception. J Adolesc Health. 1998;23(4):205–211. [DOI] [PubMed] [Google Scholar]
- 8.Koniak-Griffin D, Brecht ML. Linkages between sexual risk taking, substance use, and AIDS knowledge among pregnant adolescents and young mothers. Nurs Res. 1995;44(6):340–346. [PubMed] [Google Scholar]
- 9.Miller KS, Forehand R, Kotchick BA. Adolescent sexual behavior in two ethnic minority groups: a multisystem perspective. Adolescence. 2000;35(138):313–333. [PubMed] [Google Scholar]
- 10.Overby KJ, Kegeles SM. The impact of AIDS on an urban population of high-risk female minority adolescents: implications for intervention. J Adolesc Health. 1994;15(3):216–227. [DOI] [PubMed] [Google Scholar]
- 11.Kotchick BA, Shaffer A, Forehand R, Miller KS. Adolescent sexual risk behavior: a multi-system perspective. Clin Psychol Rev. 2001;21(4):493–519. [DOI] [PubMed] [Google Scholar]
- 12.Orr DP, Beiter M, Ingersoll G. Premature sexual activity as an indicator of psychosocial risk. Pediatrics. 1991;87(2):141–147. [PubMed] [Google Scholar]
- 13.Bagnall G, Plant M, Warwick W. Alcohol, drugs and AIDS-related risks: results from a prospective study. AIDS Care 1990;2(4):309–317. [DOI] [PubMed] [Google Scholar]
- 14.Crosby RA, DiClemente RJ, Wingood GM, Sionean C, Cobb BK, Harrington K. Correlates of unprotected vaginal sex among African American female adolescents: importance of relationship dynamics. Arch Pediatr Adolesc Med. 2000;154(9):893–899. [DOI] [PubMed] [Google Scholar]
- 15.Crosby RA, DiClemente RJ, Wingood GM, Rose E, Lang D. Correlates of continued risky sex among pregnant African American teens: implications for STD prevention. Sex Transm Dis. 2003;30(1):57–63. [DOI] [PubMed] [Google Scholar]
- 16.Roberts TA, Auinger P, Klein JD. Intimate partner abuse and the reproductive health of sexually active female adolescents. J Adolesc Health. 2005;36(5):380–385. [DOI] [PubMed] [Google Scholar]
- 17.Kreiter SR, Krowchuk DP, Woods CR, Sinal SH, Lawless MR, DuRant RH. Gender differences in risk behaviors among adolescents who experience date fighting. Pediatrics. 1999;104(6):1286–1292. [DOI] [PubMed] [Google Scholar]
- 18.Koniak-Griffin D, Nyamathi A, Vasquez R, Russo AA. Risk-taking behaviors and AIDS knowledge: experiences and beliefs of minority adolescent mothers. Health Educ Res. 1994;9(4):449–463. [DOI] [PubMed] [Google Scholar]
- 19.Gillmore MR, Lewis SM, Lohr MJ, Spencer MS, White RD. Repeat pregnancies among adolescent mothers. J Marriage Fam. 1997;59(3):536–550. [Google Scholar]
- 20.Brown LK, Lourie KJ, Flanagan P, High P. HIV-related attitudes and risk behavior of young adolescent mothers. AIDS Educ Prev. 1998;10(6):565–573. [PubMed] [Google Scholar]
- 21.Kershaw TS, Niccolai LM, Ickovics JR, Lewis JB, Meade CS, Ethier KA. Short and long-term impact of adolescent pregnancy on postpartum contraceptive use: implications for prevention of repeat pregnancy. J Adolesc Health. 2003;33(5):359–368. [DOI] [PubMed] [Google Scholar]
- 22.Breheny M, Stephens C. Barriers to effective contraception and strategies for overcoming them among adolescent mothers. Public Health Nurs. 2004;21(3):220–227. [DOI] [PubMed] [Google Scholar]
- 23.DiClemente RJ, Durbin M, Siegel D, Krasnovsky F, Lazarus N, Comacho T. Determinants of condom use among junior high school students in a minority, inner-city school district. Pediatrics. 1992;89(2):197–202. [PubMed] [Google Scholar]
- 24.Weisman CS, Plichta S, Nathanson CA, Ensminger M, Robinson JC. Consistency of condom use for disease prevention among adolescent users of oral contraceptives. Fam Plann Perspect. 1991;23(2):71–74. [PubMed] [Google Scholar]
- 25.Ku L, Sonenstein FL, Pleck JH. Young men's risk behaviors for HIV infection and sexually transmitted diseases, 1988 through 1991. Am J Public Health. 1993;83(11):1609–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jemmott LS, Jemmott JB. Increasing condom-use intentions among sexually active black adolescent women. Nurs Res. 1992;41(5):273–279. [PubMed] [Google Scholar]
- 27.Reitman D, St. Lawrence JS, Jefferson KW, Alleyne E, Brasfield TL, Shirley A. Predictors of African American adolescents' condom use and HIV risk behavior. AIDS Educ Prev. 1996;8(6):499–515. [PubMed] [Google Scholar]
- 28.Small SA, Luster T. Adolescent sexual activity: an ecological, risk-factor approach. J Marriage Fam. 1994;56(1):181–192. [Google Scholar]
- 29.Raneri LG, Wiemann CM. Social ecological predictors of repeat adolescent pregnancy. Perspect Sex Reprod Health. 2007;39(1):39–47. [DOI] [PubMed] [Google Scholar]
- 30.Bronfenbrenner U. The Ecology of Human Development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 31.Bronfenbrenner U. Ecological systems theory. : Vasta R, Annals of Child Development. Greenwich, CT: JAI Press; 1989;187–249. [Google Scholar]
- 32.Corcoran J. Ecological factors associated with adolescent sexual activity. Soc Work Health Care. 2000;30(4):93–111. [DOI] [PubMed] [Google Scholar]
- 33.Glanz K, Rimer BK, Lewis FM, Health Behavior and Health Education. 3rd ed. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 34.Wiemann CM, DuBois JC, Berenson AB. Ethnic differences in the decision to breastfeed among adolescent mothers. Pediatrics. 1998;101(6):e11. [DOI] [PubMed] [Google Scholar]
- 35.Rosenberg M. Society and the Adolescent Self-Image. Revised ed Middletown, CT: Wesleyan University Press; 1989. [Google Scholar]
- 36.Volk RJ, Pace TM, Parchman ML. Screening for depression in primary care patients: dimensionality of the short form of the Beck Depression Inventory. Psychol Assess. 1993;5(2):173–181. [Google Scholar]
- 37.Harrykissoon SD, Rickert VI, Wiemann CM. Prevalence and patterns of intimate partner violence among adolescent mothers during the postpartum period. Arch Pediatr Adolesc Med. 2002;156(4):325–330. [DOI] [PubMed] [Google Scholar]
- 38.Wiemann CM, Aguria CA, Berenson AB, Volk RJ, Rickert VI. Pregnant adolescents: experiences and behaviors associated with physical assault by an intimate partner. Matern Child Health J. 2000;4:93–101. [DOI] [PubMed] [Google Scholar]
- 39.DiClemente RJ, Salazar LF, Crosby RA, Rosenthal SL. Prevention and control of sexually transmitted infections among adolescents: the importance of a socio-ecological perspective–a commentary. Public Health. 2005;119(9):825–836. [DOI] [PubMed] [Google Scholar]
- 40.Fortenberry JD, Brizendine EJ, Katz BP, Orr DP. Post-treatment sexual and prevention behaviors of adolescents with sexually transmitted infections. Sex Transm Infect. 2002;78:365–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wingood GM, DiClemente RJ. Partner influences and gender-related factors associated with noncondom use among young adult African American women. Am J Community Psychol. 1998;26(1):29–51. [DOI] [PubMed] [Google Scholar]
- 42.Shafii T, Stovel K, Holmes K. Association between condom use at sexual debut and subsequent sexual trajectories: A longitudinal study using biomarkers. Am J Public Health. 2007;97(6):1090–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kershaw TS, Niccolai LM, Ethier KA, Lewis JB, Ickovics JR. Perceived susceptibility to pregnancy and sexually transmitted disease among pregnant and nonpregnant adolescents. J Community Psychol. 2003;31(4):419–434. [Google Scholar]
- 44.Crosby R, DiClemente RJ, Wingood GM, et al. Pregnant African-American teens are less likely than their nonpregnant peers to use condoms. Prev Med. 2002;34(5):524–528. [DOI] [PubMed] [Google Scholar]
- 45.Amaro H, Gornemann I. HIV/AIDS Related Knowledge, Attitudes, Beliefs, and Behaviors among Hispanics: Report of Findings and Recommendations. Boston, MA: Boston University School of Public Health and Northeast Hispanic AIDS Consortium; 1992. [Google Scholar]
- 46.Lesser J, Oakes R, Koniak-Griffin D. Vulnerable adolescent mothers' perceptions of maternal role and HIV risk. Health Care Women Int. 2003;24(6):513–528. [DOI] [PubMed] [Google Scholar]
- 47.Saul J, Moore J, Murphy ST, Miller LC. Relationship violence and women's reactions to male- and female-controlled HIV prevention methods. AIDS Behav. 2004;8(2):207–214. [DOI] [PubMed] [Google Scholar]
- 48.Jacoby M, Gorenflo D, Black E, Wunderlich C, Eyler AE. Rapid repeat pregnancy and experiences of interpersonal violence among low-income adolescents. Am J Prev Med. 1999;16(4):318–321. [DOI] [PubMed] [Google Scholar]
- 49.Malik S, Sorenson SB, Aneshensel CS. Community and dating violence among adolescents: perpetration and victimization. J Adolesc Health. 1997;21(5):291–302. [DOI] [PubMed] [Google Scholar]
- 50.Wenzel SL, Hambarsoomian K, D'Amico EJ, Ellison M, Tucker JS. Victimization and health among indigent young women in the transition to adulthood: a portrait of need. J Adolesc Health. 2006;38(5):536–543. [DOI] [PubMed] [Google Scholar]
- 51.Decker MR, Silverman JG, Raj A. Dating violence and sexually transmitted disease/HIV testing and diagnosis among adolescent females. Pediatrics. 2005;116(2):e272–e276. [DOI] [PubMed] [Google Scholar]
- 52.Kernic MA, Wolf ME, Holt VL, McKnight B, Huebner CE, Rivara FP. Behavioral problems among children whose mothers are abused by an intimate partner. Child Abuse Negl. 2003;27(11):1231–1246. [DOI] [PubMed] [Google Scholar]
- 53.Cleveland MJ, Gibbons FX, Gerrard M, Pomery EA, Brody GH. The impact of parenting on risk cognitions and risk behavior: a study of mediation and moderation in a panel of African American adolescents. Child Dev. 2005;76(4):900–916. [DOI] [PubMed] [Google Scholar]
- 54.Li X, Stanton B, Feigelman S. Impact of perceived parental monitoring on adolescent risk behavior over 4 years. J Adolesc Health. 2000;27(1):49–56. [DOI] [PubMed] [Google Scholar]
- 55.East PL. Racial and ethnic differences in girls’ sexual, marital, and birth expectations. J Marriage Fam. 1998;60(1):150–162. [PMC free article] [PubMed] [Google Scholar]
- 56.Metzler CW, Noell J, Biglan A, Ary D. The social context for risky sexual behavior among adolescents. J Behav Med. 1994;17(4):419–438. [DOI] [PubMed] [Google Scholar]
- 57.Kotchick BA, Dorsey S, Miller KS, Forehand R. Adolescent sexual risk-taking behavior in single-parent ethnic minority families. J Fam Psychol. 1999;13(1):93–102. [Google Scholar]
- 58.DiClemente RJ, Wingood GM, Crosby R, et al. Parental monitoring: association with adolescents’ risk behaviors. Pediatrics. 2001;107(6):1363–1368. [DOI] [PubMed] [Google Scholar]
- 59.Miller KS, Forehand R, Kotchick BA. Adolescent sexual behavior in two ethnic minority samples: the role of family variables. J Marriage Fam. 1999;60:85–98. [Google Scholar]
- 60.DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventative interventions for adolescents: sustaining effects using an ecological approach. J Pediatr Psychol. 2007;32(8):888–906. [DOI] [PubMed] [Google Scholar]
- 61.Jemmott JB, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: a randomized controlled trial. Arch Pediatr Adolesc Med. 2005;159:440–449. [DOI] [PubMed] [Google Scholar]
- 62.DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. JAMA. 2004;292:171–179. [DOI] [PubMed] [Google Scholar]
- 63.Ickovics JR, Niccolai LM, Lewis JB, Kershaw TS, Ethier KA. High postpartum rates of sexually transmitted infections among teens: pregnancy as a window of opportunity for prevention. Sex Transm Infect. 2003;79(6):469–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guijarro S, Naranjo J, Padilla M, Gutierez R, Lammers C, Blum RW. Family risk factors associated with adolescent pregnancy: study of a group of adolescent girls and their families in Ecuador. J Adolesc Health. 1999;25(2):166–172. [DOI] [PubMed] [Google Scholar]