Supplemental digital content is available in the text
Abstract
The optimal timing of percutaneous cholecystostomy for severe acute cholecystitis is unclear. The aim of this study was to investigate the timing of percutaneous cholecystostomy and its relationship to clinical outcomes in patients with inoperable acute severe cholecystitis.
From 2008 to 2010, 209 consecutive patients who were admitted to our hospital due to acute cholecystitis and were treated by percutaneous cholecystostomy were retrospectively reviewed. The time periods from symptom onset to when percutaneous cholecystostomy was performed and when patients were discharged were recorded.
In the 209 patients, the median time period between symptom onset and percutaneous cholecystostomy was 23 hours (range, 3–95 hours). The early intervention group (≤24 hours, n = 109) had a significantly lower procedure-related bleeding rate (0.0% vs 5.0%, P = 0.018) and shorter hospital stay (15.8 ± 12.9 vs 21.0 ± 17.5 days) as compared with the late intervention group (>24 hours, n = 100). Delayed percutaneous cholecystostomy was a significant independent factor for a longer hospital stay (odds ratio 3.03, P = 0.001).
In inoperable patients with acute severe cholecystitis, early percutaneous cholecystostomy reduced hospital stay and procedure-related bleeding without increasing the mortality rate.
INTRODUCTION
Currently, the gold standard treatment for acute cholecystitis is cholecystectomy. However, early cholecystectomy has a mortality rate of 5% to 30% in high-risk patients such as the elderly and critical illness.1 An alternative treatment for patients suffering from acute cholecystitis who are at high risk of surgery is percutaneous cholecystostomy, which is a minimally invasive procedure involving gallbladder drainage tube placement and decompression. Since the 1980s,2 several studies3–8 have reported the efficacy and safety of percutaneous cholecystostomy, and it has been shown that percutaneous cholecystostomy is a low-risk management strategy for high risk of surgery with acute cholecystitis. Percutaneous cholecystostomy has also been used as a bridging therapy allowing safer elective cholecystectomy after patients are recovering from acute illness.9,10 Some recent studies even suggested that temporary percutaneous cholecystostomy could be considered a first-line treatment for acute cholecystitis in high-risk patients without interval cholecystectomy.3,11,12 Although early percutaneous gallbladder drainage is safe and effective in critically ill patients in the acute phase of cholecystitis,13 to date, the optimal timing for percutaneous cholecystostomy remains unknown. Early percutaneous cholecystostomy in critically ill patients can cause severe complications such as massive bleeding as seen in sepsis-induced disseminated intravascular coagulation patients.14 However, delayed percutaneous cholecystostomy may result in progressive inflammation of the gallbladder leading to uncontrolled sepsis or shock. Hence, the aim of this study was to investigate the timing of percutaneous cholecystostomy and its relationship to clinical outcomes including procedure-related complications, hospital stay, and mortality rate in inoperable patients with acute severe cholecystitis.
MATERIALS AND METHODS
Patients
The Ethical Review Committee of Taipei Veterans General Hospital approved this study. Between July 2008 and July 2010, 209 patients who were consecutively admitted via the emergency room, diagnosed with acute cholecystitis, and underwent percutaneous cholecystostomy at our hospital were included in the study. The diagnosis of acute cholecystitis was based on clinical presentation, physical examination, laboratory data, and imaging studies including abdominal sonography and computed tomography.15 When acute cholecystitis was diagnosed, the patients received immediate medical treatment and evaluation of their surgical risk based on the American Society of Anesthesiologists (ASA) classification.16 Surgeons were consulted to explain the advantages and disadvantages of surgical treatment for the patients with acute cholecystitis; however, all of the patients refused early cholecystectomy because of the high surgical risk. These patients finally received percutaneous cholecystostomy when severe sepsis, septic shock, local gallbladder rupture, progressive intolerant pain, or persistent fever (no improvement in fever peak or frequency after 48-hour medical treatment) occurred.17
Percutaneous Cholecystostomy
Percutaneous cholecystostomy was performed by radiologists and was technically successful in all patients. After local anesthesia with lidocaine, an 8-Fr pigtail catheter (Bioteque Corporation, Taipei, Taiwan) was inserted into the gallbladder through transhepatic route under ultrasound guidance.
Data Collection
Medical records were reviewed for data collection, and the following data were recorded: patient characteristics including age, sex, underlying diseases, and ASA scores; clinical findings including time of symptom onset, vital signs in the emergency room and during admission, and indications of drainage; complete blood cell count and serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TB), alkaline phosphatase (Alk-P), γ-glutamyl-transferase (γ-GT), blood urea nitrogen (BUN), creatinine, and C-reactive protein (CRP), which were measured by Roche/Hitachi Modular Analytics Systems (Roche Diagnostics GmbH, Mannheim, Germany); abdominal computed tomography or sonography findings; procedure-related complications and mortality; and duration of hospital stay, in-hospital mortality, and causes of mortality.
Statistical Analysis
All statistical analyses were performed using SPSS version 17.0 for Windows (SPSS Inc, Chicago, IL). Continuous variables were presented as mean ± standard deviation (SD). Logistic regression was used to determine the effects of variables on in-hospital mortality and hospital stay. Only variables with P values proximal to 0.1 in univariate analysis were selected for multivariate analysis. The effects of categorical variables on outcomes were tested by the χ2 test. A 2-tailed P value <0.05 was considered to be significant.
RESULTS
Basic Patient Characteristics
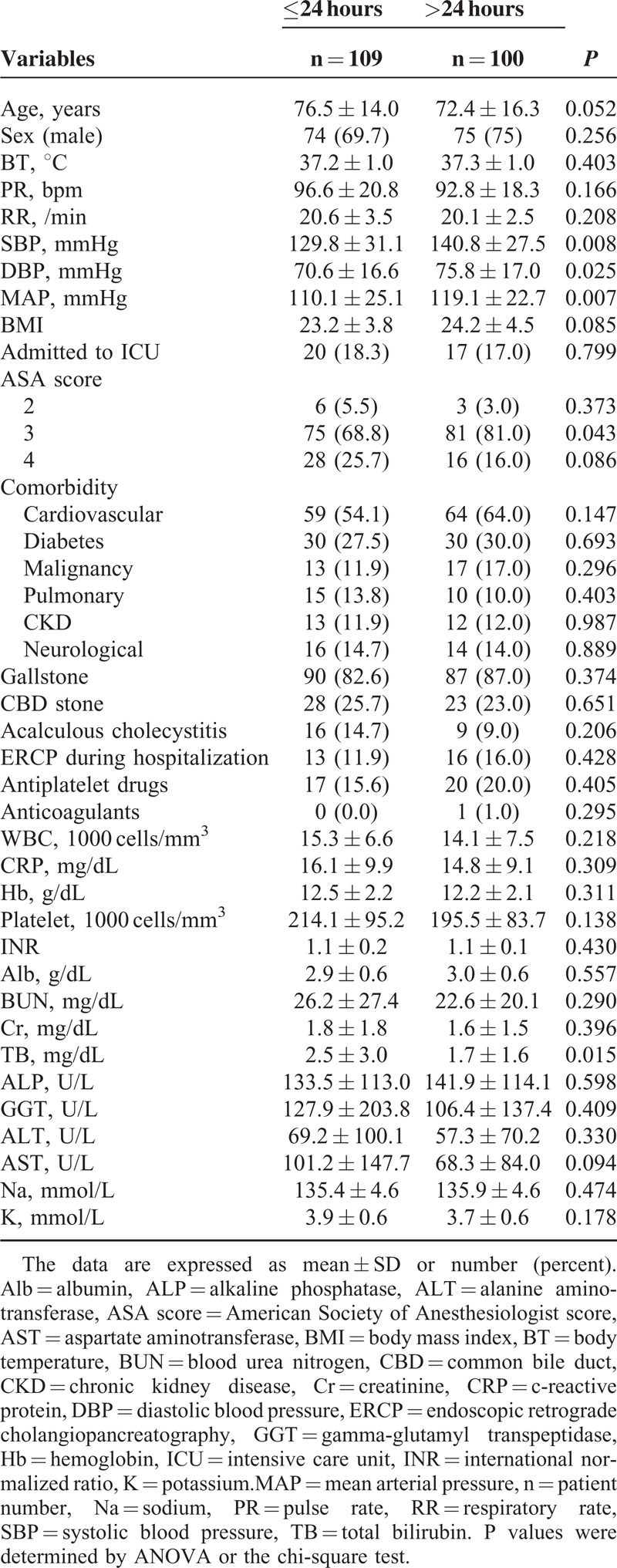
Among all 209 patients, the mean and median time periods between the onset of symptoms of acute cholecystitis and percutaneous cholecystostomy were 42.6 ± 49.4 hours (mean ± S.D) and 23 hours (range, 3–95 hours), respectively. The patients were divided into 2 groups according to the median time and clinical feasibility (the early group: ≤24 hours, n = 109; the late group: >24 hours, n = 100). The mean time periods from when symptoms occurred to cholecystostomy in the early and in the late groups were 10.3 ± 6.4 (median: 10, range: 3–24) hours and 77.9 ± 51.7 (median: 52, range: 25–95) hours, respectively. The basic characteristics of the patients are shown in Table 1. Most of the patients were male (71.3%). The mean age was 74.6 years, most patients were classified as ASA III or IV (95.7%), and 12.0% of the patients suffered from acalculous cholecystitis. The malignancy types in the 2 groups are shown in the supplemental table (see Table, Supplemental Digital Content 1, http://links.lww.com/MD/A324). The early group had lower levels of systolic blood pressure (129.8 ± 31.1 vs 140.8 ± 27.5 mmHg, P = 0.008), diastolic blood pressure (70.6 ± 16.6 vs 75.8 ± 17.0 mmHg, P = 0.025), mean arterial pressure (110.1 ± 25.1 vs 119.1 ± 22.7 mmHg, P = 0.007), fewer patients with an ASA score of III (68.8 vs 81%, P = 0.043), and higher serum total bilirubin levels (2.5 ± 3.0 vs 1.7 ± 1.6 mg/dL, P = 0.015) compared with the late group.
TABLE 1.
Characteristics of all Patients
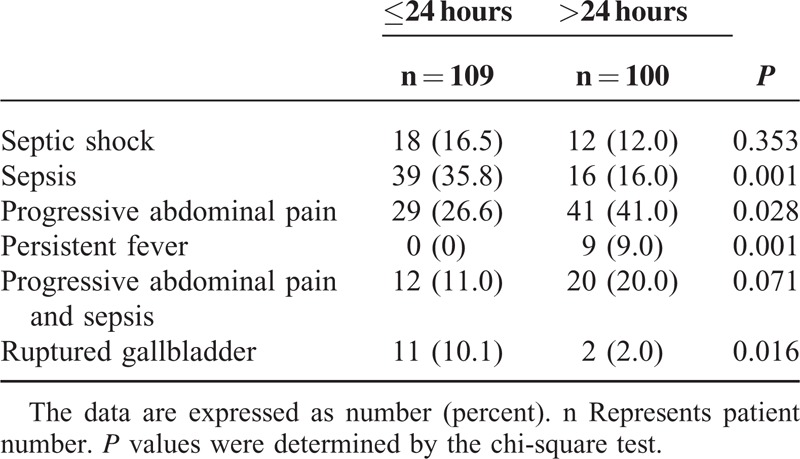
Indications and Complications of Percutaneous Cholecystostomy
More patients in the early group received percutaneous cholecystostomy due to sepsis (35.8% vs 16.0%, P = 0.001) and local gallbladder rupture (10.1% vs 2.0%, P = 0.016) than the late group (Table 2). In comparison, more patients in the late group received percutaneous cholecystostomy due to progressive intolerant abdominal pain (26.6 vs 41.0%, P = 0.028) and persistent fever (0.0 vs 9.0%, P = 0.001).
TABLE 2.
Indications of Percutaneous Transhepatic Cholecystostomy
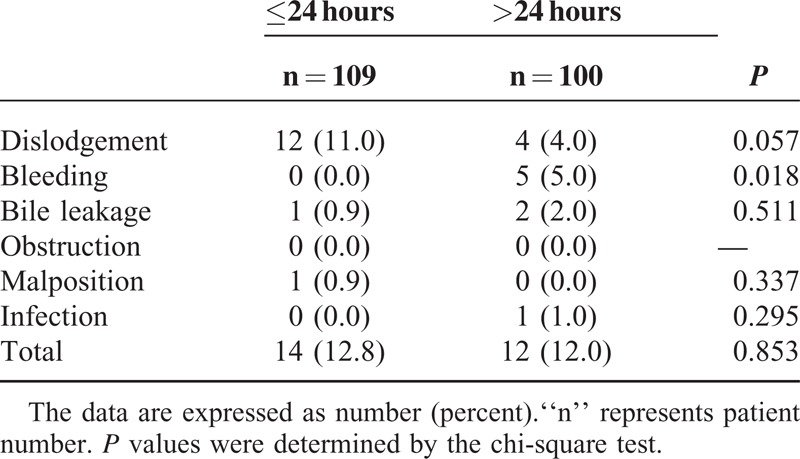
The early group had a lower (0.0% vs 5.0%, P = 0.018) procedure-related bleeding rate (Table 3). There were no significant differences in baseline levels of platelet counts, international normalized ratio, and in use of antiplatelet agents or anticoagulants. The 5 bleeding patients in the late group suffered from bloody drainage after the procedure. The bleeding was from gallbladder, not from the percutaneous puncture site. All the bleeding subsided after medical treatment. Additionally, there were no significant differences in the rate of catheter dislodgement, bile leakage, obstruction, malposition, catheter-related infection, and total complication rate. None of the patients died due to procedure-related complications.
TABLE 3.
Complications of Percutaneous Transhepatic Cholecystostomy
In-hospital Mortality Rate and Hospital Stay
Eight (7.3%) patients in the early group and 5 (5%) patients in the late group died in the hospital (P = 0.572) (Table 4). Of the 13 patients who died, 6 died due to cholecystitis-induced sepsis, 4 died due to hospital-acquired pneumonia, one died due to multiple organ failure, and one died due to terminal malignancy status (lymphoma) (Figure 1). All of these 13 patients declined emergency cholecystectomy, and all of the patients or members of their family signed “do not resuscitate” orders.
TABLE 4.
Duration of Hospital Stay and Mortality Rate During the Hospital Stay
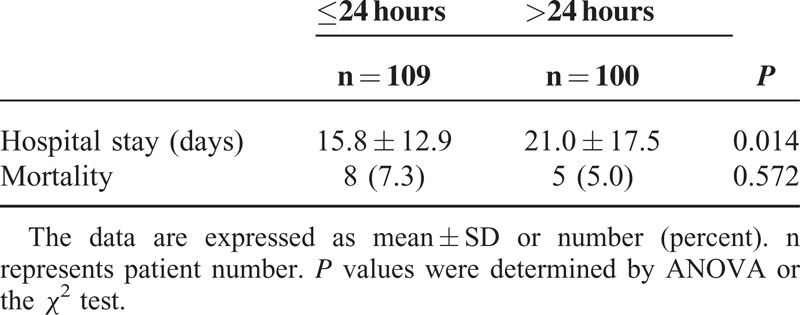
FIGURE 1.
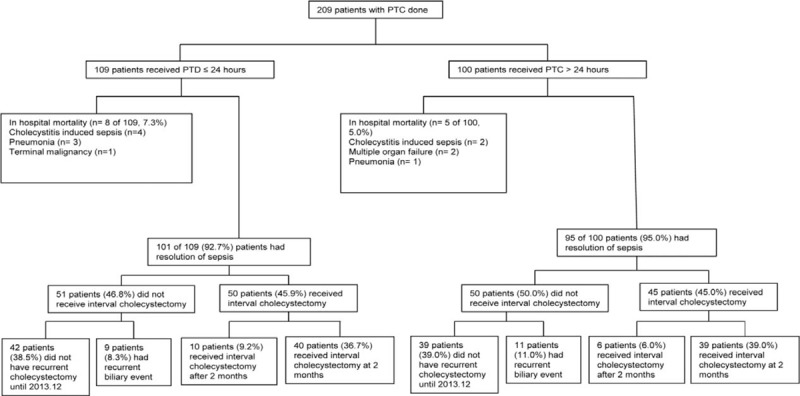
Outcomes of the patients with acute cholecystitis treated with percutaneous cholecystostomy (n = 209). PTC = percutaneous cholecystostomy.
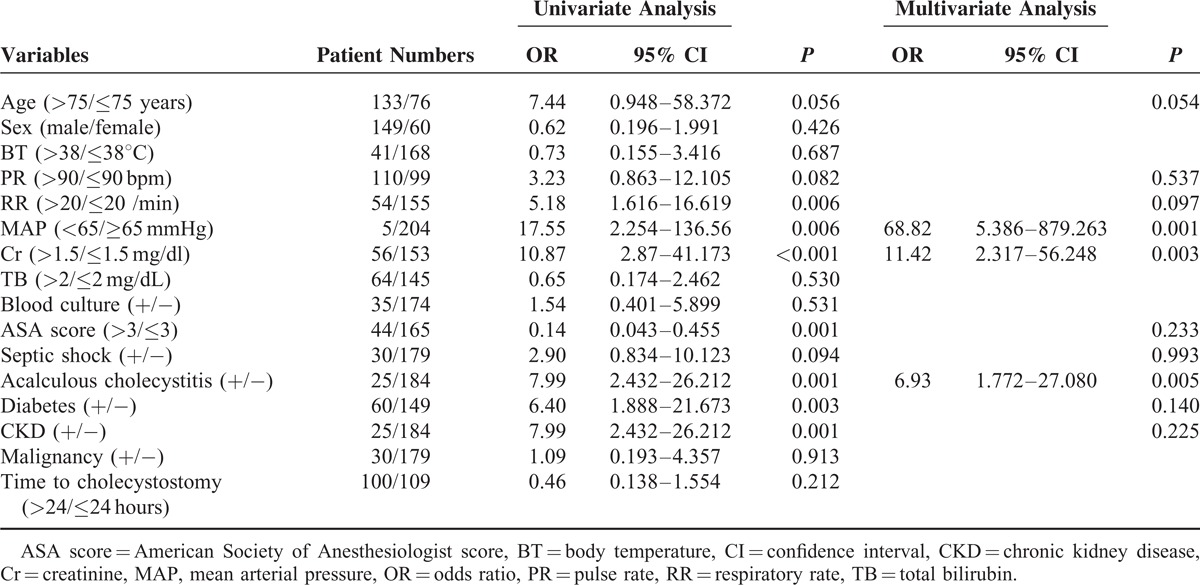
The risk factors possibly related to in-hospital mortality are shown in Table 5. According to univariate analysis (Table 5), a higher respiratory rate (>20 breaths/min), lower mean arterial pressure (<65 mmHg), higher serum creatinine level (>1.5 mg/dL), ASA score IV, acalculous cholecystitis, diabetes mellitus, and chronic kidney diseases were independent risk factors for in-hospital mortality. In multivariate analysis (Table 5), a lower mean arterial pressure (<65 mmHg), higher serum creatinine level (>1.5 mg/dL), and acalculous cholecystitis were independent risk factors for in-hospital mortality. Of these factors, a mean arterial pressure <65 mmHg was the strongest independent risk factor (odds ratio: 68.82, P = 0.001).
TABLE 5.
Univariate and Multivariate Analysis for Risk Factors Related to In-hospital Mortality
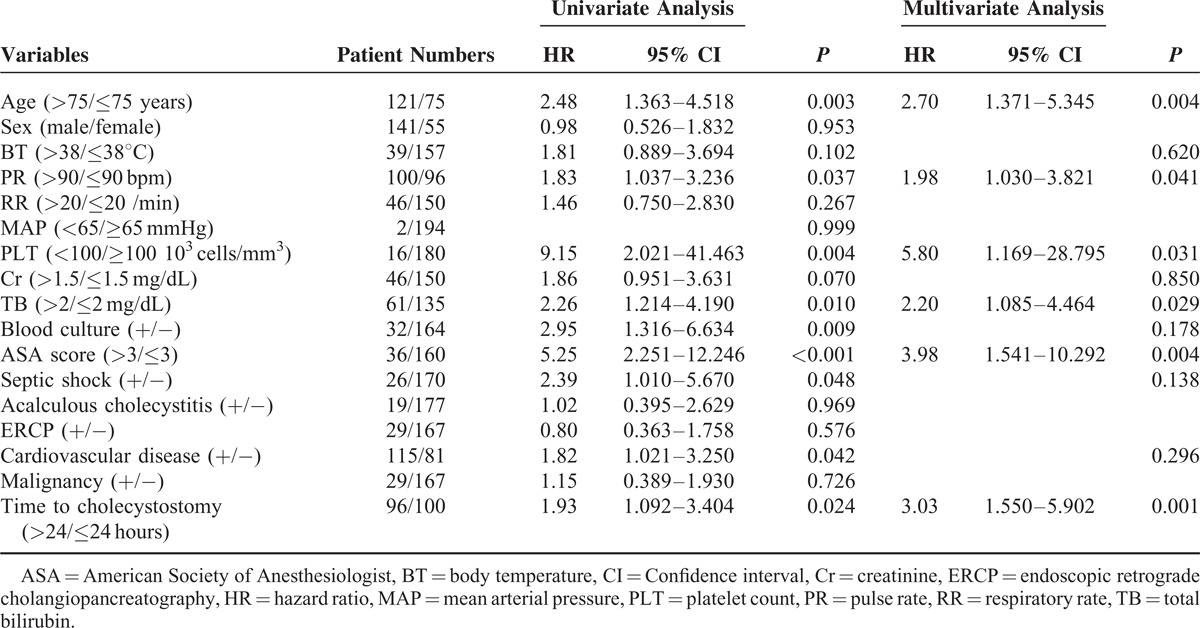
Importantly, the early group had a shorter duration of hospital stay (15.8 ± 12.9 vs 21.0 ± 17.5 days, P = 0.014) (Table 4). The duration of hospital stay remained significantly shorter after we excluded the deceased patients (16.0 ± 12.6 vs 20.1 ± 15.1 days, P = 0.038). However, the length of hospital stay after percutaneous cholecystostomy was not significantly different between the 2 groups (12.8 ± 1.2 vs 14.8 ± 1.9 days, P = 0.29). The shorter duration of hospital stay may have been due to the shorter duration from admission to performing cholecystostomy. In patients with malignancy and cholecystitis, the hospital stay between the 2 groups was not different (15.8 ± 9.5 vs 14.1 ± 6.7 days, P = 0.58) (Table S1). In univariate analysis (Table 6), older age (>75 year), higher pulse rate in the emergency room (>90 bpm), lower platelet count (<100 × 103 cells/mm3), higher serum total bilirubin level (>2.0 mg/dL), positive blood culture, ASA score IV, septic shock, cardiovascular disease, and delayed percutaneous cholecystostomy were the risk factors for a longer hospital stay (>14 days). In addition, the hospital stay in patients receiving endoscopic retrograde cholangiopancreatography or not is 21.52 ± 15.62 vs 17.77 ± 15.37 days (P = 0.226). Receiving endoscopic retrograde cholangiopancreatography is not a risk factor of a longer hospital stay in univariate analysis (P = 0.576) (Table 6). In multivariate analysis (Table 6), older age (>75 years), higher pulse rate in the emergency room (>90 bpm), lower platelet count (<100 × 103 cells/mm3), higher serum total bilirubin level (>2.0 mg/dL), ASA score IV, and delayed percutaneous cholecystostomy remained significant predictive factors of a longer hospital stay.
TABLE 6.
Univariate and Multivariate Analysis for Risk Factors of a Hospital Stay Longer Than 2 Weeks
DISCUSSION
Since the 1980s, percutaneous cholecystostomy has been proven to be effective in patients with acute cholecystitis who are at high risk of surgical morbidity and mortality.3,6,7,11–13 However, currently, no studies have mentioned the optimal timing for percutaneous cholecystostomy. The current study demonstrated that the timing of percutaneous cholecystostomy is important. Although relatively worse clinical conditions were noted in the early group, early percutaneous cholecystostomy reduced the length of hospital stay and procedure-related bleeding rate with a similar mortality rate to the late group. Therefore, our findings suggest that early percutaneous cholecystostomy may be more appropriate when patients have severe sepsis/septic shock, uncontrolled fever/pain, or local gallbladder rupture.
In patients with acute cholecystitis who are suitable for surgery, early laparoscopic cholecystectomy is advantageous.13,15,17 However, the optimal timing of early laparoscopic cholecystectomy is controversial.18 One recent prospective randomized trial showed that laparoscopic cholecystectomy within 24 hours of hospital admission was superior to a conservative approach with regard to morbidity and cost, although there was no significant difference in mortality.19 However, no study has mentioned the optimal timing for percutaneous cholecystostomy in patients with acute cholecystitis who are not suitable for surgery. Our results showed that in patients with acute cholecystitis who were at high surgical risk receiving percutaneous cholecystostomy, the early intervention group had a shorter hospital stay. Percutaneous cholecystostomy is a minimally invasive procedure and provides gallbladder decompression.20 As there was no difference in hospital stay post-cholecystostomy, earlier decompression of the gallbladder may reverse the process of inflammation earlier, subsequently contributing to a faster improvement and shorter hospital course.
In addition to a delayed intervention, multivariate analysis also found that an older age, higher pulse rate in the emergency room, lower platelet counts, higher serum total bilirubin levels, and ASA score IV were independent risk factors of a longer hospital stay. Tachycardia and lower platelet counts may be caused by acute cholecystitis-induced sepsis, and jaundice and higher ASA scores represent poor clinical conditions. Therefore, these factors may have resulted in the longer hospital stay.
Acute direct complications of percutaneous cholecystostomy include catheter dislodgement, hemorrhage, sepsis (exacerbation or de-novo), bile leakage, bowel perforation, pneumothorax, and vasovagal reactions. Sanjay et al21 analyzed the complication rate of ultrasound-guided percutaneous cholecystostomy in 242 patients with or without coagulopathy, and reported that the overall complication rate was about 10%. Winbladh et al22 found that catheter migration is the most common complication, with a rate of 8.6%. Our results are compatible with these previous studies, and our overall complication rate was about 13% with catheter dislodgement being the most common complication. Locking a pigtail drain, ensuring adequate fixation, and caution when patients are transferred back to the ward are simple steps, which may be able to reduce the risk of catheter dislodgement.10 In a previous study, it was reported that the percutaneous cholecystostomy-related bleeding rate was 1.9%.21 Similarly, the overall procedure-induced bleeding rate in our patients was 2.4%. Additionally, the post-cholecystostomy bleeding rate was higher in the late group of this study. The mean platelet counts, the levels of international normalized ratio before percutaneous cholecystostomy, and the use of antiplatelet agents or anticoagulants were not different between the 2 groups. The patients complicated with profound bleeding after percutaneous cholecystostomy had normal platelet counts and levels of international normalized ratio when the procedures were performed. A transhepatic approach has been reported to possibly lead to a higher rate of bleeding as compared with a transperitoneal route23; however, all of our patients received drainage by the same route (transhepatic route). Further studies are needed to elucidate whether persistent inflammation of the gallbladders in the late group caused difficulty in the approach or whether there were other reasons. Moreover, a systematic literature review concluded that the mortality rate directly resulting from percutaneous cholecystostomy was 0.4%.22 In our current study, none of the patients died directly due to the procedure-related complications. Taken together, these findings suggest that percutaneous cholecystostomy is a relatively safe intervention for critically ill patients.
Several studies have reported that the 30-day mortality rates in patients receiving percutaneous cholecystostomy ranged from 0% to 25%.13,22,24,25 In this study, the patients at high risk of surgery who received percutaneous cholecystostomy had an overall in-hospital mortality rate of approximately 6%. The early group had lower levels of mean arterial pressure and higher levels of serum total bilirubin. In other words, the early group had a worse clinical condition; however, the overall in-hospital mortality rate of the early group was not significantly higher than the late group. In multivariate analysis, a profound low mean arterial pressure (<65 mmHg) was a significant risk factor for mortality. This suggests that early intervention in selected patients may avoid progression to uncontrolled condition by blocking the inflammatory process.
Ha et al26 found that shock on admission was an independent risk factor for in-hospital mortality. In the current study, a profound low mean arterial pressure and higher serum creatinine levels were independent risk factors for in-hospital mortality. Furthermore, we found that acalculous cholecystitis was also an independent risk factor for in-hospital mortality. Clinically, acute acalculous cholecystitis often occurs in critically ill patients, and it is especially related to sepsis, shock, trauma, surgery, burns, total parenteral nutrition, and/or prolonged fasting. It has a high mortality (most studies, 30%; ranges between 10% and 90% with early or late diagnosis, respectively).27 Based on these findings, more attention should be paid to these patients.
There are several limitations in this study. First, in-patients with acute cholecystitis were excluded due to a lack of definitive timing between the symptom onset to percutaneous cholecystostomy, a very long hospital stay, and many comorbidities. In addition, the main patient group of our hospital is elderly male veterans, which may result in selection bias. Therefore, prospective studies are needed to confirm whether early intervention is more appropriate.
In conclusion, percutaneous cholecystostomy is an effective alternative treatment for acute cholecystitis for patients at a high risk for surgery. Early percutaneous cholecystostomy may reduce the length of hospital stay and procedure-related bleeding rate without increasing the overall mortality rate. Early percutaneous cholecystostomy is suggested when patients with acute cholecystitis who are not suitable for surgery respond poorly to medical therapy.
Acknowledgments
The authors gratefully acknowledge Dr. Yun-Cheng Hsieh for her excellent statistical assistance and declare no conflict of interest. This study is in part supported by grant V102B-017 from Taipei Veterans General Hospital, Taipei, Taiwan.
Footnotes
Abbreviations: Alb = albumin, Alk-p = alkaline phosphatase, ALT = alanine aminotransferase, ASA score = American Society of Anesthesiologists score, AST = aminotransferase, BMI = body mass index, BT = body temperature, BUN = blood urea nitrogen, CBD = common bile duct, CKD = chronic kidney disease, Cr = creatinine, CRP = C-reactive protein, DBP = diastolic blood pressure, γ-GT = gamma-glutamyl-transferase, Hb = hemoglobin, INR = international normalized ratio, K = potassium, MAP = mean arterial pressure, Na = sodium, PR = pulse rate, PTC = percutaneous cholecystostomy, RR = respiratory rate, SBP = systolic blood pressure, TB = total bilirubin.
The authors have no funding and conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Patterson EJ, McLoughlin RF, Mathieson JR, et al. An alternative approach to acute cholecystitis. Percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Surg Endosc 1996; 10:1185–1188. [DOI] [PubMed] [Google Scholar]
- 2.Shaver RW, Hawkins IF, Jr, Soong J. Percutaneous cholecystostomy. AJR Am J Roentgenol 1982; 138:1133–1136. [DOI] [PubMed] [Google Scholar]
- 3.Li M, Li N, Ji W, et al. Percutaneous cholecystostomy is a definitive treatment for acute cholecystitis in elderly high-risk patients. Am Surg 2013; 79:524–527. [DOI] [PubMed] [Google Scholar]
- 4.Silberfein EJ, Zhou W, Kougias P, et al. Percutaneous cholecystostomy for acute cholecystitis in high-risk patients: experience of a surgeon-initiated interventional program. Am J Surg 2007; 194:672–677. [DOI] [PubMed] [Google Scholar]
- 5.Carrafiello G, D’Ambrosio A, Mangini M, et al. Percutaneous cholecystostomy as the sole treatment in critically ill and elderly patients. La Radiol Med 2012; 117:772–779. [DOI] [PubMed] [Google Scholar]
- 6.Kapan M, Onder A, Tekbas G, et al. Percutaneous cholecystostomy in high-risk elderly patients with acute cholecystitis: a lifesaving option. Am J Hospice Palliat Care 2013; 30:167–171. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Sanjuan JC, Arruabarrena A, Sanchez-Moreno L, et al. Acute cholecystitis in high surgical risk patients: percutaneous cholecystostomy or emergency cholecystectomy? Am J Surg 2012; 204:54–59. [DOI] [PubMed] [Google Scholar]
- 8.McKay A, Abulfaraj M, Lipschitz J. Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg Endosc 2012; 26:1343–1351. [DOI] [PubMed] [Google Scholar]
- 9.Miura F, Takada T, Kawarada Y, et al. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreatic Surg 2007; 14:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Little MW, Briggs JH, Tapping CR, et al. Percutaneous cholecystostomy: the radiologist's role in treating acute cholecystitis. Clin Radiol 2013; 68:654–660. [DOI] [PubMed] [Google Scholar]
- 11.Chang YR, Ahn YJ, Jang JY, et al. Percutaneous cholecystostomy for acute cholecystitis in patients with high comorbidity and re-evaluation of treatment efficacy. Surgery 2014; 155:615–622. [DOI] [PubMed] [Google Scholar]
- 12.Zerem E, Omerovic S. Can percutaneous cholecystostomy be a definitive management for acute cholecystitis in high-risk patients? Surg Laparosc Endosc Percutan Tech 2014; 24:187–191. [DOI] [PubMed] [Google Scholar]
- 13.Atar E, Bachar GN, Berlin S, et al. Percutaneous cholecystostomy in critically ill patients with acute cholecystitis: complications and late outcome. Clin Radiol 2014; 69:e247–e252. [DOI] [PubMed] [Google Scholar]
- 14.Dewhurst C, Kane RA, Mhuircheartaigh JN, et al. Complication rate of ultrasound-guided percutaneous cholecystostomy in patients with coagulopathy. AJR Am J Roentgenol 2012; 199:W753–760. [DOI] [PubMed] [Google Scholar]
- 15.Strasberg SM. Clinical practice. Acute calculous cholecystitis. N Engl J Med 2008; 26: 358:2804–2811. [DOI] [PubMed] [Google Scholar]
- 16.Little JP. Consistency of ASA grading. Anaesthesia 1995; 50:658–659. [PubMed] [Google Scholar]
- 17.Skouras C, Jarral O, Deshpande R, et al. Is early laparoscopic cholecystectomy for acute cholecystitis preferable to delayed surgery?: Best evidence topic (BET). Int J Surg 2012; 10:250–258. [DOI] [PubMed] [Google Scholar]
- 18.Degrate L, Ciravegna AL, Luperto M, et al. Acute cholecystitis: the golden 72-h period is not a strict limit to perform early cholecystectomy. Results from 316 consecutive patients. Langenbecks Arch Surg 2013; 398:1129–1136. [DOI] [PubMed] [Google Scholar]
- 19.Gutt CN, Encke J, Koninger J, et al. Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg 2013; 258:385–393. [DOI] [PubMed] [Google Scholar]
- 20.Ginat D, Saad WE. Cholecystostomy and transcholecystic biliary access. Tech Vasc Interv Radiol 2008; 11:2–13. [DOI] [PubMed] [Google Scholar]
- 21.Sanjay P, Mittapalli D, Marioud A, et al. Clinical outcomes of a percutaneous cholecystostomy for acute cholecystitis: a multicentre analysis. HPB (Oxford) 2013; 15:511–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winbladh A, Gullstrand P, Svanvik J, et al. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB 2009; 11:183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nemcek AA, Jr, Bernstein JE, Vogelzang RL. Percutaneous cholecystostomy: does transhepatic puncture preclude a transperitoneal catheter route? J Vasc Interv Radiol 1991; 2:543–547. [DOI] [PubMed] [Google Scholar]
- 24.Chang L, Moonka R, Stelzner M. Percutaneous cholecystostomy for acute cholecystitis in veteran patients. Am J Surg 2000; 180:198–202. [DOI] [PubMed] [Google Scholar]
- 25.Avrahami R, Badani E, Watemberg S, et al. The role of percutaneous transhepatic cholecystostomy in the management of acute cholecystitis in high-risk patients. Int Surg 1995; 80:111–114. [PubMed] [Google Scholar]
- 26.Ha JP, Tsui KK, Tang CN, et al. Cholecystectomy or not after percutaneous cholecystostomy for acute calculous cholecystitis in high-risk patients. Hepatogastroenterology 2008; 55:1497–1502. [PubMed] [Google Scholar]
- 27.Huffman JL, Schenker S. Acute acalculous cholecystitis: a review. Clin Gastroenterol Hepatol 2010; 8:15–22. [DOI] [PubMed] [Google Scholar]


