Abstract
Multiple myeloma is characterized by the neoplastic proliferation of a single clone of plasma cells producing a monoclonal protein. However, the involvement of pancreas is a rare event. We herein report a rare case of pancreatic plasmacytoma, which was detected before the diagnosis of multiple myeloma.
An 83-year-old male was referred to our hospital for further evaluation of obstructive jaundice and a pancreatic mass. A contrast-enhanced computed tomography (CT) scan revealed solid masses with homogenous enhancement in the pancreatic head and retroperitoneum. The histological findings of the retroperitoneal mass obtained by CT-guided biopsy showed multiple sheets of atypical plasma cells, which were positively immunostained for CD79a, CD138, and the κ light chain. Serum immunoelectrophoresis detected M-component of immunoglobulin A-κ, and the histological findings of the bone marrow revealed an abnormally increased number of atypical plasma cells with irregular nuclei and cytoplasmic vacuolation. The patient was therefore diagnosed to have multiple myeloma involving the pancreas and retroperitoneum. Although chemotherapy was performed, the patient died 6 months after the diagnosis.
The pancreatic plasmacytoma was detected before the multiple myeloma in the present case. It is difficult to diagnose a pancreatic plasmacytoma without a history of multiple myeloma and related disease.
INTRODUCTION
Multiple myeloma is characterized by the neoplastic proliferation of a single clone of plasma cells producing a monoclonal protein. However, the involvement of pancreas is a rare event. We herein report a rare case of pancreatic plasmacytoma, which was detected before the diagnosis of multiple myeloma.
CASE REPORT
An 83-year-old male noticed dark urine and a yellowish tint to skin, and presented to a private clinic in December 2013. He had undergone distal gastrectomy with Billroth-II reconstruction due to a gastric ulcer 27 years earlier. As his doctor detected a mass of the pancreatic head by computed tomography (CT), he was referred to our hospital for further evaluation. A physical examination revealed icteric skin and sclerae without abdominal symptoms. Blood tests showed increases in the total bilirubin level (11.0 mg/dL; range 0.2–1.0 mg/dL), alkaline phosphatase (2513 U/L; range 96–284 U/L), γ-glutamyl transpeptidase (676 U/L; range 4–67 U/L), aspartate aminotransferase (284 U/L; range 6–40 U/L), alanine aminotransferase (337 IU/L; range 6–37 U/L), amylase (148 U/L; range 37–125 U/L), total protein (8.2 g/dL; range 6.0–8.0 g/dL), and the level of immunoglobulin A (IgA) (959.5 mg/dL; range 71.0–365.0 mg/dL). Hemoglobin level was slightly decreased (12.2 g/dL; range 13.5–17.0 g/dL), but serum albumin, serum calcium, and serum creatinine levels were within the normal limits. The levels of cancer antigen 19-9 (108 U/mL; range ≤37 U/mL), Dupan2 (308 U/mL; range ≤150 U/mL), and Span-1 (72 U/mL; range ≤30.0 U/mL) were elevated, whereas the carcinoembryonic antigen level was within the normal limits.
Multiphase CT detected a 5-cm solid mass with an unclear margin in the head of the pancreas with homogenous enhancement with intravenous contrast in the arterial phase, as well as in the delayed phase (Figure 1A). In addition, a 4.5-cm solid mass in the retroperitoneum involving the left ureter between the aorta and left kidney was also detected (Figure 1B). This mass also showed unclear margins and a homogenous enhancement by intravenous contrast in the arterial phase, which was similar to that in the head of the pancreas. An endoscopic retrograde cholangiopancreatography study with double balloon enteroscopy (EC-450-BI5; Fujifilm Co., Tokyo, Japan) revealed a smooth narrowing of the dorsal bile duct and an irregular stenosis of the pancreatic duct in the head of the pancreas. Subsequently, a biliary plastic stent was inserted into the common bile duct. Endoscopic biopsy could not be performed because it is difficult to insert biopsy foreceps into the common bile duct. Therefore, the histological findings of the specimens obtained from the retroperitoneal mass using CT-guided biopsy revealed multiple sheets of atypical plasma cells with irregular nuclei located eccentrically in the cytoplasm. The immunohistochemical profile of the tumor was positive for CD79a, CD138, and the κ light chain, which was consistent with plasmacytoma (Figure 2).
FIGURE 1.
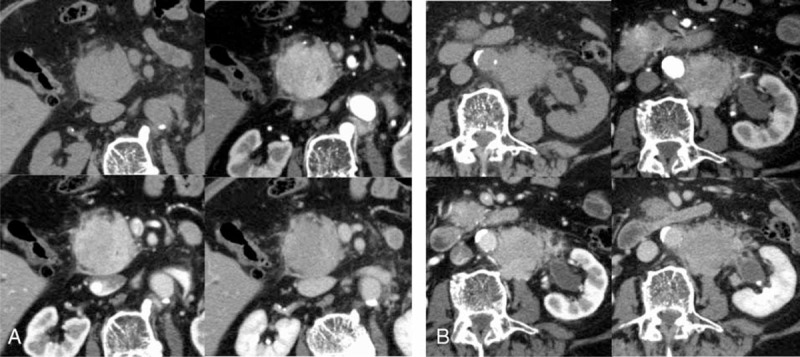
(A) Multiphasic contrast-enhanced abdominal CT demonstrating a solid mass of 5 cm in diameter with homogenous intravenous contrast enhancement in the arterial phase in the head of the pancreas. Upper left column: plain CT; upper right column: arterial phase; lower left column: portal venous phase; and lower right column: delayed phase. (B) Multiphasic abdominal CT of demonstrating a 4.5-cm solid mass in the retroperitoneum. Upper left column: plain CT; upper right column: arterial phase; lower left column: portal venous phase; and lower right column: delayed phase. CT = computed tomography.
FIGURE 2.
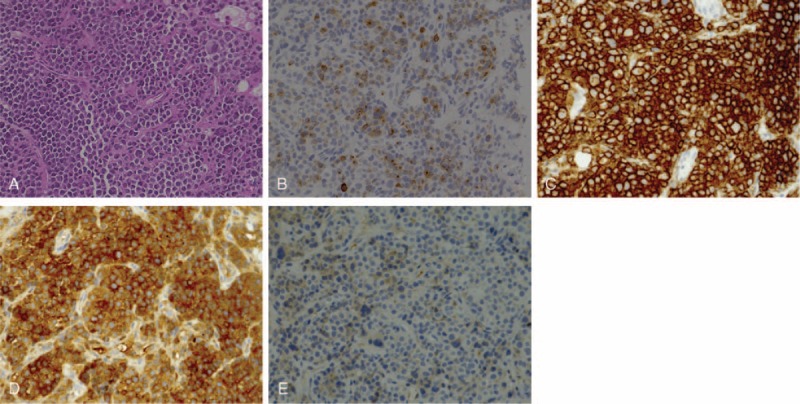
The pathological findings of a CT-guided biopsy of the retroperitoneal mass. (A) Hematoxylin-eosin staining. Multiple sheets of atypical plasma cells with irregular nuclei were located eccentrically in the cytoplasm. (B) CD79a. (C) CD138. (D) Immunoglobulin κ chain. (E) Immunoglobulin λ chain. The immunohistochemical profile of the tumor was positive for CD79a, CD138, and the κ light chain, which was consistent with plasmacytoma. CT = computed tomography.
Any bone destruction could not be detected by whole body examination of X-ray and CT. The histological findings of a bone marrow biopsy revealed 9.6% atypical plasma cells with irregular nuclei and cytoplasmic vacuolation. Serum protein electrophoresis showed a monoclonal spike of the fraction of γ globulin, which was confirmed to be IgA by immunoelectrophoresis. As there were no myeloma-defining events, the patient was diagnosed to have asymptomatic multiple myeloma with pancreatic plasmacytoma: clinical stage 1A in the Durie & Salmon staging system and clinical stage 1 in the International Staging System of myeloma.
Melphalan (6 mg days 1–4) and prednisolone (40 mg days 1–4); every 4 weeks were administrated as first-line chemotherapy after informed consent was obtained. Although the patient developed acute cholangitis, only endoscopic exchanging of a biliary stent could control and chemotherapy could be continued without other adverse events. However, after 3 courses, CT revealed the progression of pancreatic plasmacytoma, suggesting treatment failure. Thereafter, bortezomib (1.4 mg weekly) and dexamethasone (8 mg weekly) treatments were started, but his general condition immediately worsened, and the patient died 6 months after the diagnosis of pancreatic plasmacytoma.
Ethical approval was not required for this case report as it did not relate to patient's privacy or treatment. The informed consent for description of the case could not be obtained because the patient was dead.
DISCUSSION
We herein described a rare case of pancreatic plasmacytoma without symptoms of multiple myeloma. In the present case, histopathological examination to the pancreatic mass could not be performed. However, the characteristics of contrast-enhanced CT of pancreatic mass were similar to that of peritoneal mass; therefore, we diagnosed as pancreatic and peritoneal plasmacytoma. Notably, the pancreatic plasmacytoma was detected before the multiple myeloma in the present case. Most cases of pancreatic plasmacytoma had a history of multiple myeloma or related disease, suggesting that pancreatic involvement is a rare event at the time of diagnosis of myeloma. It is difficult to diagnose a pancreatic tumor without a history of such diseases due to the lack of typical features of pancreatic plasmacytoma on CT, magnetic resonance imaging (MRI), and other examinations.1 There were only 7 case reports, including our present case, that did not have a history of multiple myeloma or related disease (Table 1).2–7 The present patient was oldest. All of the 3 patients with plasmacytoma in the pancreatic head including our case complained jaundice, suggesting jaundice was the most common symptom of the patients with plasmacytoma in the head of the pancreas.
TABLE 1.
Case Reports of Pancreatic Plasmacytoma Without a History of Multiple Myeloma or Related Diseases
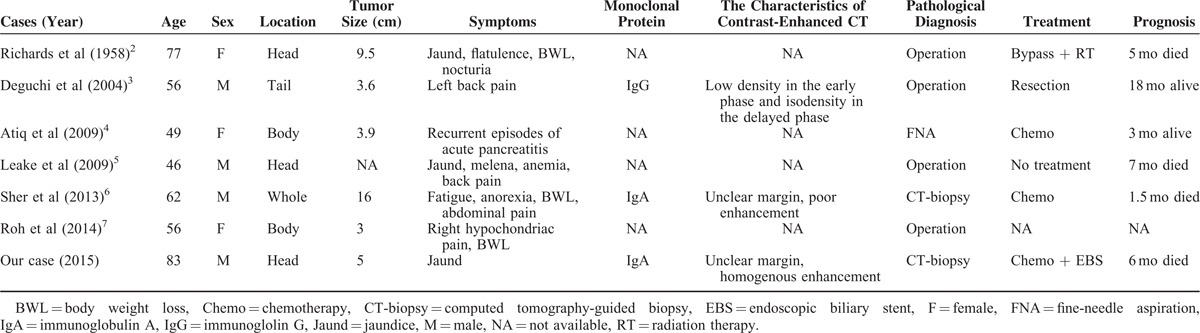
Contrast-enhanced CT was performed in only 3 cases. In the previous 2 cases, pancreatic plasmacytoma was revealed as solid mass with poor enhancement. However in the present case, multiphase contrast-enhanced CT revealed solid masses with homogenous enhancement in the arterial phase. Although Hammond et al1 reviewed the several case reports and proposed that the most typical finding of pancreatic plasmacytoma on CT might be the presence of a focal multilobulated mass with homogeneous contrast enhancement, the features of pancreatic plasmacytoma on multiphase contrast-enhancement CT have not been established. Further analysis with the accumulation of cases of pancreatic plasmacytoma will clarify the characteristic findings of pancreatic plasmacytoma on CT, MRI, and other examinations.
CONCLUSION
We have presented a rare case of pancreatic plasmacytoma, which was detected before the diagnosis of multiple myeloma. It is difficult to diagnose a pancreatic plasmacytoma without a history of multiple myeloma and related disease.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Hammond NA, Miller FH, Day K, et al. Imaging features of the less common pancreatic masses. Abdom Imaging 2013; 38:561–572. [DOI] [PubMed] [Google Scholar]
- 2.Richards WG, Katzmann FS, Coleman FC. Extramedullary plasmacytoma arising in the head of the pancreas; report of a case. Cancer 1958; 11:649–652. [DOI] [PubMed] [Google Scholar]
- 3.Deguchi Y, Nonaka A, Takeuchi E, et al. Primary pancreatic plasmacytoma. Am J Clin Oncol 2004; 27:247–249. [DOI] [PubMed] [Google Scholar]
- 4.Atiq M, Ali SA, Dang S, et al. Pancreatic plasmacytoma presenting as variceal hemorrhage: life threatening complication of a rare entity. JOP 2009; 10:187–188. [PubMed] [Google Scholar]
- 5.Leake PA, Coard KC, Plummer JM. Extramedullary plasmacytoma of the pancreas as an uncommon cause of obstructive jaundice: a case report. J Med Case Rep 2009; 3:8785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sher T, Bhat S, Jitawatanarat P, et al. Multiple myeloma mimicking metastatic pancreas cancer. J Clin Oncol 2013; 31:e297–e299. [DOI] [PubMed] [Google Scholar]
- 7.Roh YH, Hwang SY, Lee SM, et al. Extramedullary plasmacytoma of the pancreas diagnosed using endoscopic ultrasonography-guided fine needle aspiration. Clin Endos 2014; 47:115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]


