Abstract
Simple bone cysts (SBCs) are benign bone tumors. However, the treatment of SBCs remains controversial because of their healing rate and the invasiveness of surgery. The purpose of the present study was to evaluate the treatment of SBCs using a cannulated hydroxyapatite (HA) pin.
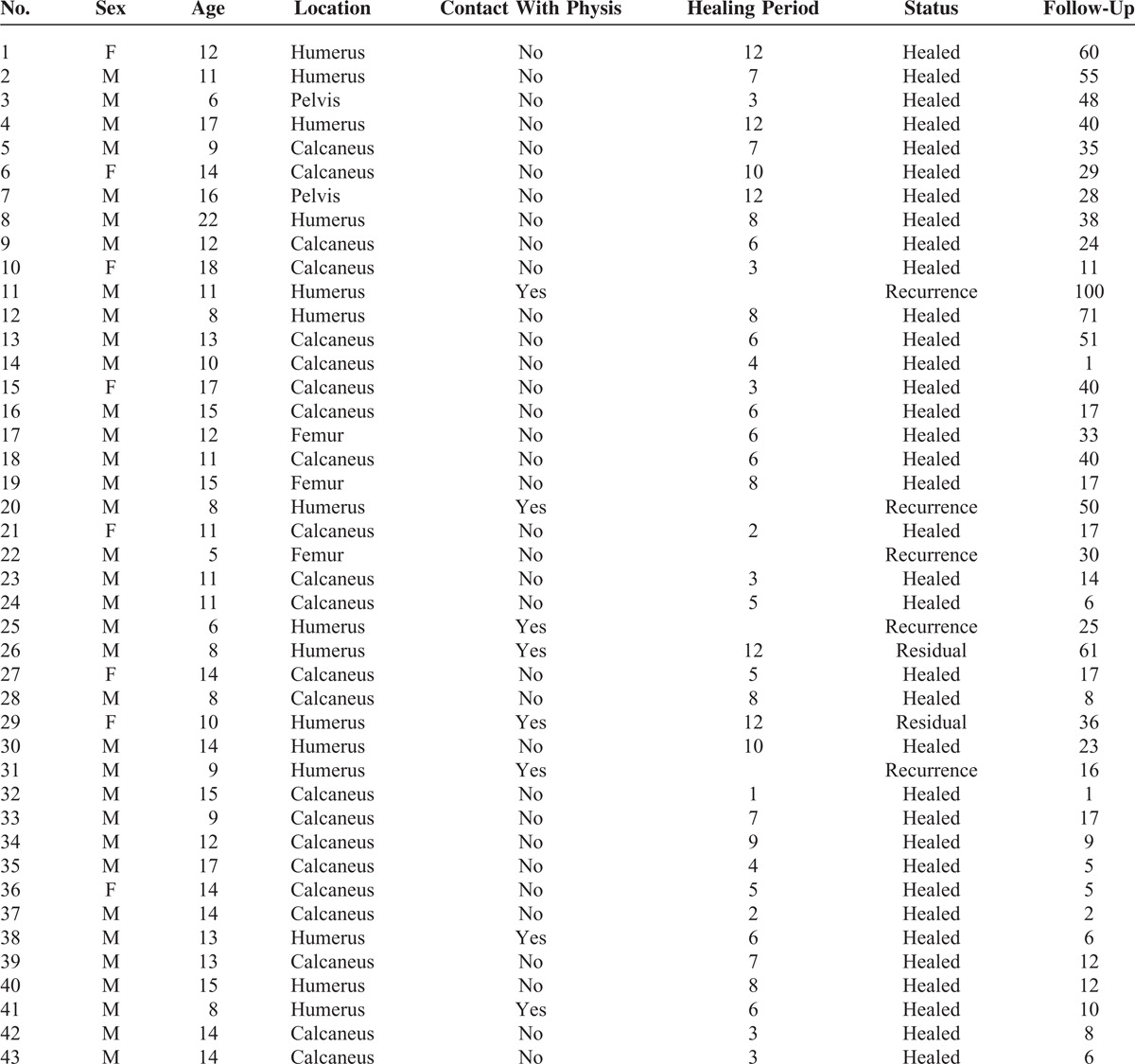
A total of 43 patients (35 males, 8 females; mean age 12.1 years; age range, 5–22 years) with SBCs were treated with continuous decompression by inserting ceramic HA pins between 1989 and 2014. The SBCs were located in the calcaneus in 23, the humerus in 15, the femur in 3, and the pelvis in 2 cases. In all patients, minimal fenestration of the cyst wall and curettage and multiple drilling in the cyst wall were performed, followed by insertion of the HA pin. The mean follow-up period was 26.6 months. Operating time, healing period, risk factors for recurrence, and the cure rate were evaluated.
Healing was achieved without intervention in 38 patients after a mean of 6.4 months. Two patients had persistent small residual cysts, which had no changes after 1 year at the latest follow-up. There were 5 patients with recurrences (humerus 4, femur 1), who were cured by curettage and artificial bone grafting. The final healing rate by cannulation only using an HA pin was 88.2%. On Fisher exact test, age, site of SBCs, and distance from the physis were found to be significantly associated with SBC recurrence (P < 0.05).
In the present study, cannulation using an HA pin for SBCs was found to be a useful technique, particularly for calcaneal cysts, because it is a minimally invasive procedure with a high cure rate. In patients <10 years, involvement of the humerus and contact with the growth plate were significant risk factors for SBC recurrence.
INTRODUCTION
Simple bone cysts (SBCs) are benign bone tumors that traditionally present in the first 2 decades of life. The cysts have a predilection to occur in males more frequently than in females (3:1). The most common site of SBCs is the humerus (59%), followed by the femur (25%) and the calcaneus (6%).1 Alternative therapeutic options for SBCs have included steroid injections, autologous bone marrow injection, open curettage and bone grafting, various methods of cyst decompression, the use of calcium phosphate and calcium sulfate, and cannulated screws.2–10 However, treatment of SBCs remains controversial because of the cure rate and the invasiveness of surgery. Although most SBCs resolve by the time the patient reaches skeletal maturity, it has been reported that patient age and the location of the cyst within the physis are predictors of successful treatment. The purpose of the present study was to evaluate the treatment of SBCs using a cannulated hydroxyapatite (HA) pin (Figure 1) that can decompress continuously and does not require further surgery for implant removal unlike cannulated screws.9
FIGURE 1.
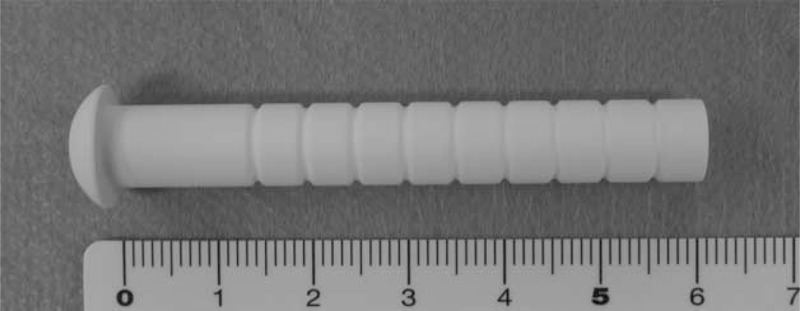
Cannulated hydroxyapatite pin (outside diameter 8 mm, inside diameter 3 mm).
PATIENTS AND METHODS
Between 1989 and 2014, HA pins (Kobayashi Medical, Tokyo, Japan) insertion was performed as the first operation on all cases of SBC that required surgery. Informed consent was obtained from the patients and their family members. Of the 43 patients that underwent HA pins insertion, 35 were males and 8 were females, with a mean age of 12.1 years (range, 5–22 years). The SBCs were located in the calcaneus in 23, the humerus in 15, the femur in 3, and the pelvis in 2 cases (Table 1). In all patients, minimal fenestration (diameter, 8 mm) was performed in the cyst wall, and then curettage was done. After that, multiple drill holes were made in the cyst wall with a K-wire to establish a connection to healthy bone marrow, followed by insertion of the HA pin. The mean follow-up period was 26.6 months. Healing period, recurrence and healing rates, and risk factors for recurrence were evaluated. A cyst was classified as healed when there was complete obliteration of the cavity. Fisher exact test was performed to examine the risk factors for SBC recurrence, such as sex, age, cyst sites, and distance from the physis. A P value of <0.05 was considered significant. Statistical analyses were performed using IBM SPSS Statistics software, version 19 (IBM SPSS, Armonk, NY).
TABLE 1.
Patient Characteristics and Treatment Outcomes
RESULTS
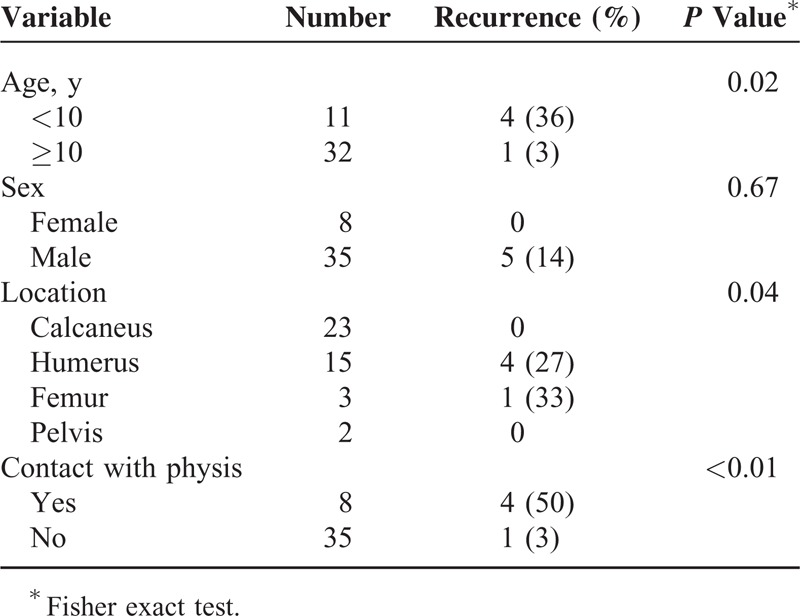
Healing was achieved without intervention in 38 patients after a mean of 6.4 months (range, 1–12) (Figures 2 and 3). Two patients had persistent small residual cysts, which had no changes after 1 year at the latest follow-up. There were 5 patients with recurrences (humerus 4, femur 1), which were cured by curettage and artificial bone grafting in expectation of adding mechanical strength (Figure 4). All patients with SBCs of the calcaneus were healed after a mean of 5.0 months (range, 1–10 months). The final healing rate by cannulation only using HA pins was 88.4%. On Fisher exact test, age <10 years, site involving the humerus, and contact with the growth plate were significantly associated with SBC recurrence (P < 0.05) (Table 2).
FIGURE 2.

Case 27. (A) SBC of the calcaneus of a 14-year-old girl. (B) Five months after surgery, the cyst has completely healed. SBC = simple bone cyst.
FIGURE 3.
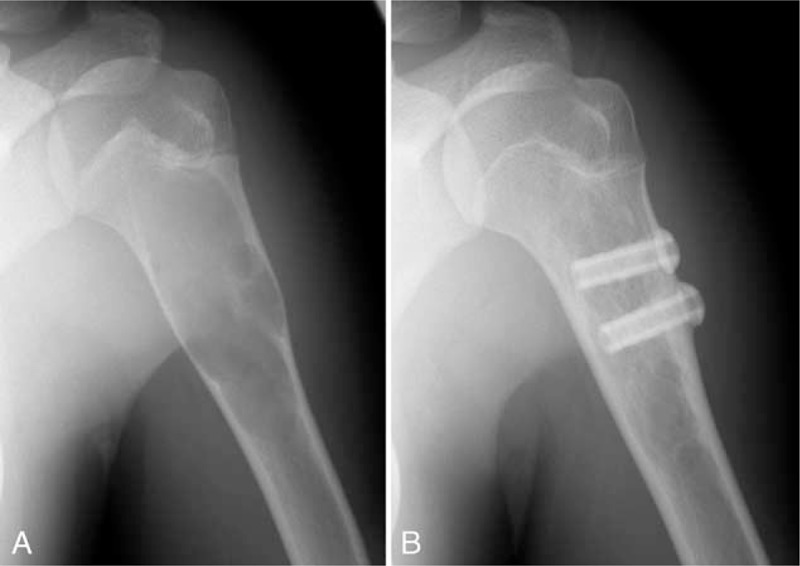
Case 40. (A) SBC of the humerus of a 15-year-old boy. (B) Eight months after surgery, the cyst has completely healed. SBC = simple bone cyst.
FIGURE 4.

Case 20. SBC of the humerus of an 8-year-old boy. (A) An HA pin has been inserted into the cyst cavity after curettage and drilling. (B) Nine months after initial surgery, the cyst has enlarged. (C) A reoperation was performed, with curettage and artificial bone grafting. (D) Recurrence of the cyst occurred in part of the proximal artificial bone 23 months after reoperation. (E) Sixteen months after the third operation, the cyst has completely healed. HA = hydroxyapatite, SBC = simple bone cyst.
TABLE 2.
Analysis of Recurrence Factors for Simple Bone Cyst
DISCUSSION
In the present study, cannulation using an HA pin was found to be a useful technique for SBCs, particularly calcaneal cysts, because it is a minimally invasive procedure with a high cure rate. Strategies for treatment of SBCs have evolved over a long time. Currently, management methods include observation,11 injections of steroid2,12 or bone marrow or demineralized bone matrix,3,13 decompression using a cannulated pin and screw,5,9,10 and combined surgical techniques. However, management of SBCs remains controversial because of their healing rate and the invasiveness of treatment. SBCs sometimes heal spontaneously subsequent to a pathological fracture. Spontaneous healing occurs in <10% of patients with an SBC as a result of traumatic decompression by a pathological fracture.14 Steroid injection was proposed by Scaglietti et al15 in 1979; they reported a high healing rate after steroid injection. However, subsequent studies reported a lower healing rate for steroid injection, only 41% to 63%.2,16 The injection of bone marrow alone or in combination with demineralized bone matrix has been proposed to have a good healing rate of 43% to 69%.17,18 On the other hand, Chang et al19 reported no advantage with the use of autologous bone marrow. The gold standard procedure has been considered for many years to be curettage with removal of the cyst membrane and bone grafting. However, the healing rate has ranged as low as 40%.4,20 Decompression of SBCs can be achieved using needles or implants, such as intramedullary nails, Kirchner wires, and cannulated screws or pins. Decompression using intramedullary nails provided healing rates of almost 70%, with recurrence rates of <10%.21,22 However, this technique requires a second surgery to remove the nails.
We have used cannulated HA pins that provide decompression continuously since 1989. They do not need to be removed and have osteoconductive properties that may stimulate healing. In the present study, the healing rate was 88.2%, which was satisfactory compared with the healing rate by the methods mentioned earlier. Cho et al,16 Rougraff et al,17 and Glanzmann and Campos22 reported that it took 9 to 16 months to achieve remodeling. In the present study, the mean healing period was only 6.1 months.
There are few reports about the risk factors for SBC recurrence. Age was reported to be a reliable predictor, with children >10 years of age having a higher rate of cyst healing than those <10 years.23,24 Nonetheless, in a more recent study, age and location were found not to affect the outcome.16 However, in the present study, age <10 years and location in the humerus were associated with a significantly higher recurrence rate. Alternatively, Haidar et al25 reported that a lesion located <2 cm from the growth plate may be a risk factor for recurrence. In the present study, a significantly higher recurrence rate was found for patients with a lesion contacting the physis. As the reason for this, we speculate that the proximal humerus in the young, due to its rapid growth, may have a likelihood of venous obstruction leading to the formation of cysts.
The limitation of the present study is the absence of a comparative group or a randomized comparison. Moreover, the number of patients enrolled was relatively small, and thus the statistical power of the study was weak. A large study would provide more information.
In conclusion, the present study suggests that cannulation using HA pins for SBCs is a useful technique, particularly for calcaneal cysts, because it is a minimally invasive procedure with a high cure rate. Age <10 years, site in the humerus, and contact with the growth plate were significant risk factors for SBC recurrence.
Footnotes
Abbreviations: HA = hydroxyapatite, SBC = simple bone cyst.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Kadhim M, Thacker M, Kadhim A, et al. Treatment of unicameral bone cyst: systematic review and meta analysis. J Child Orthop 2014; 8:171–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hashemi-Nejad A, Cole WG. Incomplete healing of simple bone cysts after steroid injections. J Bone Joint Surg Br 1997; 79:727–730. [DOI] [PubMed] [Google Scholar]
- 3.Yandow SM, Lundeen GA, Scott SM, et al. Autogenic bone marrow injections as a treatment for simple bone cyst. J Pediatr Orthop 1998; 18:616–620. [DOI] [PubMed] [Google Scholar]
- 4.Bensahel H, Jehanno P, Desgrippes Y, et al. Solitary bone cyst: controversies and treatment. J Pediatr Orthop B 1998; 7:257–261. [DOI] [PubMed] [Google Scholar]
- 5.Brecelj J, Suhodolcan L. Continuous decompression of unicameral bone cyst with cannulated screws: a comparative study. J Pediatr Orthop B 2007; 16:367–372. [DOI] [PubMed] [Google Scholar]
- 6.Masquijo JJ, Baroni E, Miscione H. Continuous decompression with intramedullary nailing for the treatment of unicameral bone cysts. J Child Orthop 2008; 2:279–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mainard D, Galois L. Treatment of a solitary calcaneal cyst with endoscopic curettage and percutaneous injection of calcium phosphate cement. J Foot Ankle Surg 2006; 45:436–440. [DOI] [PubMed] [Google Scholar]
- 8.Dormans JP, Sankar WN, Moroz L, et al. Percutaneous intramedullary decompression, curettage, and grafting with medical-grade calcium sulfate pellets for unicameral bone cysts in children: a new minimally invasive technique. J Pediatr Orthop 2005; 25:804–811. [DOI] [PubMed] [Google Scholar]
- 9.Tsuchiya H, Abdel-Wanis ME, Uehara K, et al. Cannulation of simple bone cysts. J Bone Joint Surg Br 2002; 84:245–248. [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Wanis ME, Tsuchiya H, Uehara K, et al. Minimal curettage, multiple drilling, and continuous decompression through a cannulated screw for treatment of calcaneal simple bone cysts in children. J Pediatr Orthop 2002; 22:540–543. [PubMed] [Google Scholar]
- 11.Pogoda P, Priemel M, Linhart W, et al. Clinical relevance of calcaneal bone cysts: a study of 50 cysts in 47 patients. Clin Orthop Relat Res 2004; 424:202–210. [DOI] [PubMed] [Google Scholar]
- 12.Sakamoto A, Matsuda S, Yoshida T, et al. Clinical outcome following surgical intervention for a solitary bone cyst: emphasis on treatment by curettage and steroid injection. J Orthop Sci 2010; 15:553–559. [DOI] [PubMed] [Google Scholar]
- 13.Cho HS, Seo SH, Park SH, et al. Minimal invasive surgery for unicameral bone cyst using demineralized bone matrix: a case series. BMC Musculoskelet Disord 2012; 13:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkins RM. Unicameral bone cysts. J Am Acad Orthop Surg 2000; 8:217–224. [DOI] [PubMed] [Google Scholar]
- 15.Scaglietti O, Marchetti PG, Bartolozzi P. The effects of methylprednisolone acetate in the treatment of bone cysts. Results of three years follow-up. J Bone Joint Surg Br 1979; 61:200–204. [DOI] [PubMed] [Google Scholar]
- 16.Cho HS, Oh JH, Kim HS, et al. Unicameral bone cysts. A comparison of injection of steroid and grafting with autologous bone marrow. J Bone Joint Surg Br 2007; 89:222–226. [DOI] [PubMed] [Google Scholar]
- 17.Rougraff BT, Kling TJ. Treatment of active unicameral bone cysts with percutaneous injection of demineralized bone matrix and autogenous bone marrow. J Bone Joint Surg Am 2002; 84:921–929. [DOI] [PubMed] [Google Scholar]
- 18.Di Bella C, Dozza B, Frisoni T, et al. Injection of demineralized bone matrix with bone marrow concentrate improves healing in unicameral bone cyst. Clin Orthop Relat Res 2010; 468:3047–3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang CH, Stanton RP, Glutting J. Unicameral bone cysts treated by injection of bone marrow or methyl prednisolone. J Bone Joint Surg Br 2002; 84:407–412. [DOI] [PubMed] [Google Scholar]
- 20.Sung AD, Anderson ME, Zurakowski D, et al. Unicameral bone cyst: a retrospective study of three surgical treatments. Clin Orthop Relat Res 2008; 466:2519–2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Sanctis N, Andreacchio A. Elastic stable intramedullary nailing is the best treatment of unicameral bone cysts of the long bones in children? Prospective long-term follow-up study. J Pediatr Orthop 2006; 26:520–525. [DOI] [PubMed] [Google Scholar]
- 22.Glanzmann MC, Campos L. Flexible intramedullary nailing for unicameral cysts in children's long bones. J Child Orthop 2007; 1:97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dormans JP, Pill SG. Fractures through bone cysts: unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas. Instr Course Lect 2002; 51:457–467. [PubMed] [Google Scholar]
- 24.Baig R, Eady JL. Unicameral (simple) bone cysts. South Med J 2006; 99:966–976. [DOI] [PubMed] [Google Scholar]
- 25.Haidar SG, Culliford DJ, Gent ED, et al. Distance from the growth plate and its relation to the outcome of unicameral bone cyst treatment. J Child Orthop 2011; 5:151–156. [DOI] [PMC free article] [PubMed] [Google Scholar]


