Abstract
Occlusion of small side branch (SB) may result in significant adverse clinical events. We aim to characterize the predictors of small SB occlusion and incidence of periprocedural myocardial injury (PMI) in coronary bifurcation intervention.
Nine hundred twenty-five consecutive patients with 949 bifurcation lesions (SB ≤ 2.0 mm) treated with percutaneous coronary intervention (PCI) were studied. All clinical characteristics, coronary angiography findings, PCI procedural factors, and quantitative coronary angiographic analysis data were collected. SB occlusion after main vessel (MV) stenting was defined as no blood flow or any thrombolysis in myocardial infarction (TIMI) flow grade decrease in SB after MV stenting. Multivariate logistic regression analysis was performed to identify independent predictors of small SB occlusion. Creatine kinase-myocardial band activity was determined by using an immunoinhibition assay and confirmed by mass spectrometry. Incidence of PMI between no SB occlusion group and SB occlusion group was compared.
SB occlusion occurred in 86 (9.1%) of 949 bifurcation lesions. Of SB occlusion, total occlusion occurred in 64 (74.4%) lesions and a decrease in TIMI flow occurred in 22 (25.6%) lesions. True bifurcation lesion, irregular plaque, predilation in SB, preprocedural SB TIMI flow grade, preprocedural diameter stenosis of distal MV, preprocedural diameter stenosis of bifurcation core, bifurcation angle, diameter ratio between MV and SB, diameter stenosis of SB before MV stenting, and MV lesion length were independent risk factors of SB occlusion. We observed a significantly higher incidence of PMI in each cutoff level in patients with SB occlusion compared with those without SB occlusion.
True bifurcation lesion, irregular plaque, and 8 other predictors were independent predictors of SB occlusion. Patients with small SB occlusion had significant higher incidence of PMI.
INTRODUCTION
Percutaneous coronary intervention (PCI) of coronary bifurcation lesion can be technically challenging and result in high rates of periprocedural myocardial injury (PMI).1 Side branch (SB) occlusion after main vessel (MV) stenting (Figure 1) in coronary bifurcation intervention is one of the most important factors causing PMI.2 Occlusion of large SBs may result in significant adverse clinical events3,4; however, occlusion of small SBs was thought to be well tolerated and indifferent.5–7 Although small SB occlusion has already been recognized as a contributing factor toward periprocedural myocardial infarction (MI) and resultant clinical outcomes,8,9 the incidence, predictors, and PMI rate of small SBs occlusion in coronary bifurcation intervention have not been fully elucidated.
FIGURE 1.
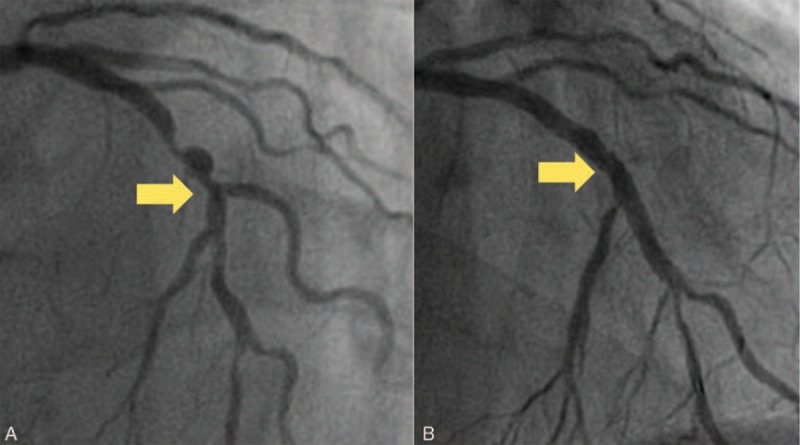
SB occlusion in coronary bifurcation intervention. (A) Bifurcation lesion located at left anterior descending artery and diagonal branch. (B) The diagonal branch occluded after left anterior descending artery stenting. SB = side branch.
The incidence of small SB occlusion did not draw enough attention of clinical interventionists. Among patients with bifurcation lesions undergoing PCI, there is a significant rate of small SB compromise, which may lead to PMI.10 Previous studies have reported that PMI was associated with statistically and clinically significant increase in the subsequent risk of death.11 Accordingly, this study was designed to characterize the predictors, PMI rate, and clinical outcome of small SB occlusion in coronary bifurcation intervention.
METHODS
Study Population
From January 2012 to July 2012, a cohort of 7007 consecutive patients underwent PCI at Fuwai Hospital in Beijing, China. For the present study, specific inclusion criteria were the following: patients with coronary bifurcation lesions (which was defined as a coronary artery narrowing occurring adjacent to or involving the origin of SB12) undergoing PCI; and the bifurcation lesion that consisted of a SB having baseline reference diameter ≤2.0 mm that is confirmed by the core laboratory and quantitative coronary angiography (QCA) analysis. Exclusion criterion was SB baseline reference diameter >2.0 mm. Among the 7007 patients with 9421 lesions, 7530 no bifurcation lesions and 942 coronary bifurcation lesions with SB baseline reference diameter >2.0 mm were excluded. Finally, 925 patients with 949 bifurcation lesions that met all the inclusion criteria and had no exclusion criteria were included in this study (Figure 2).
FIGURE 2.
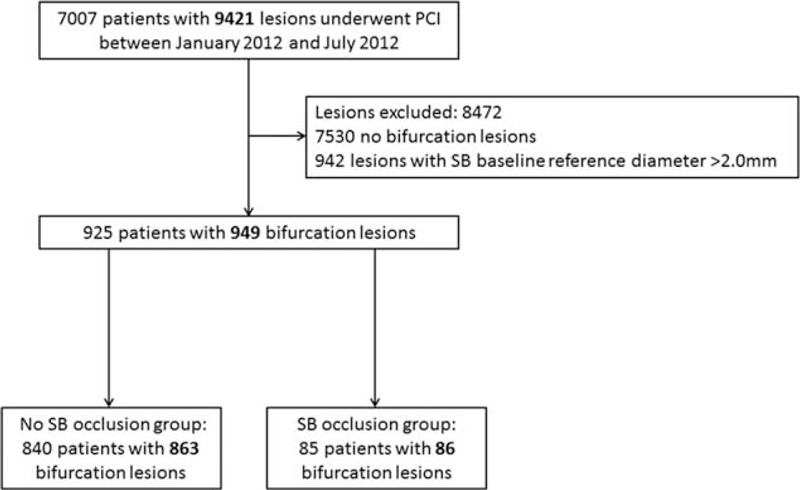
Flowchart of the study. PCI = percutaneous coronary intervention, SB = side branch.
The Ethics Committee of the Cardiovascular Institute and Fuwai Hospital approved this study. The study complies with the Declaration of Helsinki.
Procedure and Periprocedural Medications
Coronary angioplasty was performed in the conventional manner and coronary stents or other procedures/devices were used only when required. In all cases, the interventional strategy and instrumentation used were at the discretion of the interventional cardiologists. Decisions regarding the treatment strategy for bifurcation lesions were made by individual operators. The administration of periprocedural antiplatelet and antithrombotic medications was based on the operator's discretion and current guidelines. Administration of 300 mg clopidogrel and 300 mg aspirin as loading doses within the 24 hours before the procedure was mandatory. Lifelong aspirin (100 mg/d) was prescribed to all patients. At least 12 months of clopidogrel (75 mg/d) was recommended to all patients.
Data Collection and QCA
Clinical data were obtained through a review of the medical records. All baseline and procedural cineangiograms were reviewed and analyzed by an independent core laboratory. The synergy between PCI with taxus and cardiac surgery (SYNTAX) score13 and the residual SYNTAX score14,15 from all coronary angiograms were assessed by an independent angiographic core laboratory blinded to clinical outcomes. Procedural characteristics such as SB predilation and the presence of a jailed wire in the SB were also recorded.
The baseline reference diameter of SB was calculated by QCA. QCA is performed by using standard quantitative analyses and definitions.16 A main principle of our QCA approach was to ensure as little observer interference as possible. Angiograms obtained at baseline were analyzed with the use of a computer-based system dedicated to bifurcation analysis (Qangio XA, version7.3; Medis, Leiden, Netherlands). We obtained quantitative angiographic measurements of the 4 segments of the bifurcation lesion: the proximal MV segment, the distal MV segment, the SB segment, and the bifurcation core segment (Figure 3). Bifurcation core was defined as the central part of the bifurcation that begins where the common vessel starts to split into 2 branches and ends at the cardinal point,17 the area which is calculated by the Qangio XA software.
FIGURE 3.
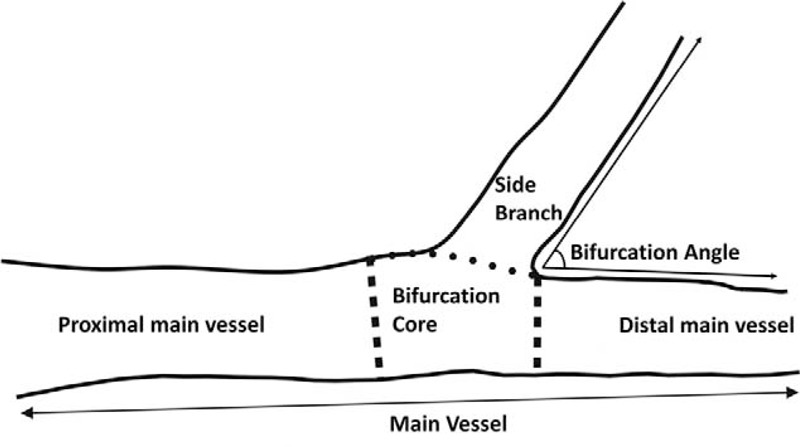
Schematic diagram of quantitative coronary angiographic analysis. Bifurcation lesions were analyzed as 4 segments: the proximal MV segment, the distal MV segment, the SB segment, and the bifurcation core segment. MV = main vessel, SB = side branch.
Blood samples were routinely obtained from patients before and after the procedure. Creatine kinase-myocardial band (CK-MB) activity was determined using an immunoinhibition assay and confirmed by mass spectrometry at the Fuwai Hospital Biochemistry Laboratory.
Follow-up data at 12 months were obtained during an outpatient clinic visit or by phone. Events ascertained at follow-up included all-cause mortality (cardiac or noncardiac), recurrence of the angina pectoris, rehospitalization, MI, any revascularization, and stent thrombosis. Events were defined according to the Academic Research Consortium definitions.18
Definitions
SB occlusion was defined as absence of flow in the SB post-PCI or any thrombolysis in myocardial infarction (TIMI) flow grade decrease in SB.
Recent studies have reported that measurement of CK-MB rather than troponin allows more accurate diagnosis of PMI; thus, we used CK-MB as a biomarker for PMI instead of troponin values.19,20 PMI was defined as a postprocedural CK-MB level higher than upper limit of normal (ULN); periprocedural MI was defined as an elevation of CK-MB ≥3 × ULN.18 The ULN for CK-MB at our institution is 24 U/L.
Statistical Methods
Continuous data were presented as mean ± standard deviation and compared using the Student t test. Categorical variables were summarized as counts and percentages and compared by χ2 test or Fisher exact test as appropriate. All P values were 2-tailed, and a P value of <0.05 was considered statistically significant. All analyses were performed with SAS 9.4 system (SAS Institute, Cary, NC). Any variable having a significant univariate association with SB occlusion (P ≤ 0.25) was selected as a candidate for the multivariable analysis. The multivariable model was then built by stepwise variable selection with same entry and exit criteria as in the univariable analysis. Thirty variables such as sex, acute MI, history of stroke, and jailed wire in SB were candidates for the multivariable model.
RESULTS
Patient, Lesion, and Procedural Characteristics
SB occlusion occurred in 86 (9.1%) of 949 bifurcation lesions. Of SB occlusion, total occlusion occurred in 64 (74.4%) of lesions and a decrease in TIMI flow occurred in 22 (25.6%) lesions. Blood flow in SB was restored spontaneously in 4 (4.7%) lesions and by SB intervention in 5 (5.8%) lesions of 86 occluded SB; 77 (89.5%) lesions occluded permanently.
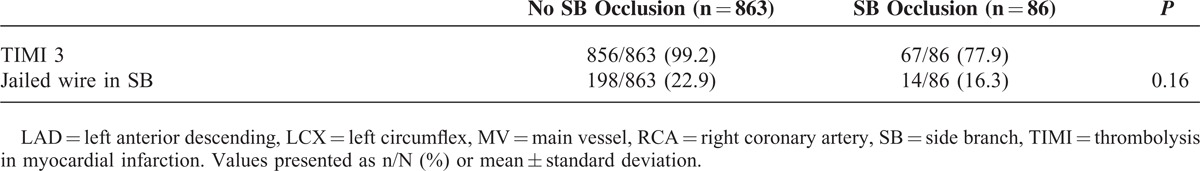
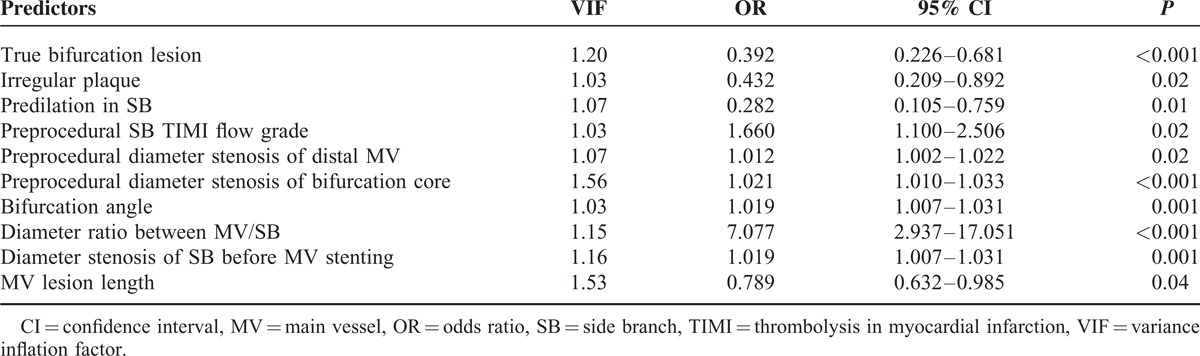
Patient characteristics are shown in Table 1. All the baseline characteristics were not significantly different between the 2 groups. There was no significant difference in SYNTAX score or residual SYNTAX score between the 2 groups. Lesion and procedural characteristics are presented in Table 2 . Among lesion characteristics, location of bifurcation, Medina classification, and distribution of plaque differed significantly between the 2 study groups. Among procedural characteristics, dissection before MV stenting and TIMI flow grade before MV stenting were significantly different between the 2 groups. Quantitative coronary angiographic data are presented in Table 3. There were significant differences between the 2 groups in reference diameter of all 4 parts. However, regarding the lesion length, only the lesion length of bifurcation core was significantly different between the 2 groups. Diameter ratio between MV and SB in SB occlusion group (1.7 ± 0.3) was significantly higher than no SB occlusion group (1.6 ± 0.3) (P < 0.001).
TABLE 1.
Patient Characteristics
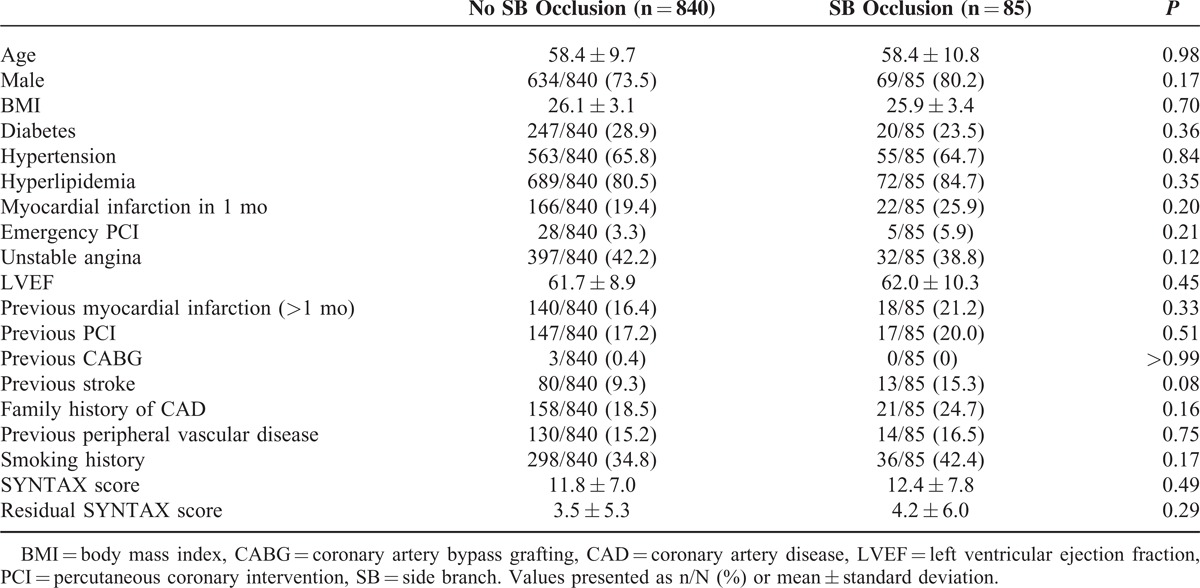
TABLE 2.
Lesion and Procedural Characteristics
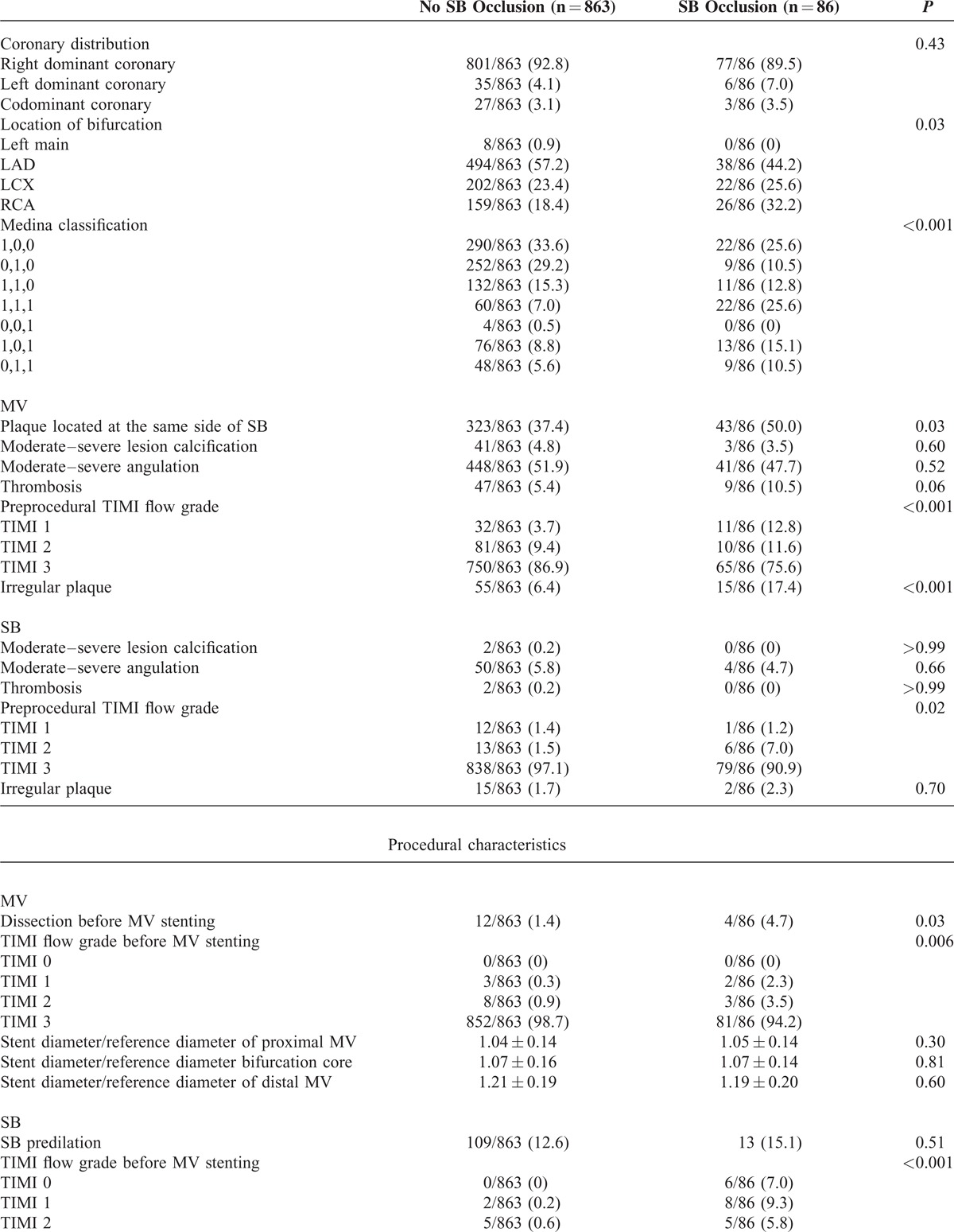
TABLE 2 (Continued).
Lesion and Procedural Characteristics
Predictors of SB Occlusion
After adjustment using a multiple logistic regression model, true bifurcation lesion, irregular plaque, predilation in SB, preprocedural SB TIMI flow grade, preprocedural diameter stenosis of distal MV, preprocedural diameter stenosis of bifurcation core, bifurcation angle, diameter ratio between MV and SB, diameter stenosis of SB before MV stenting, and MV lesion length remained significant and independent risk factors of SB branch occlusion (Table 4). The variance inflation factor (Table 4) showed absence of multicollinearity among these independent predictors.
TABLE 3.
Quantitative Coronary Angiographic Characteristics
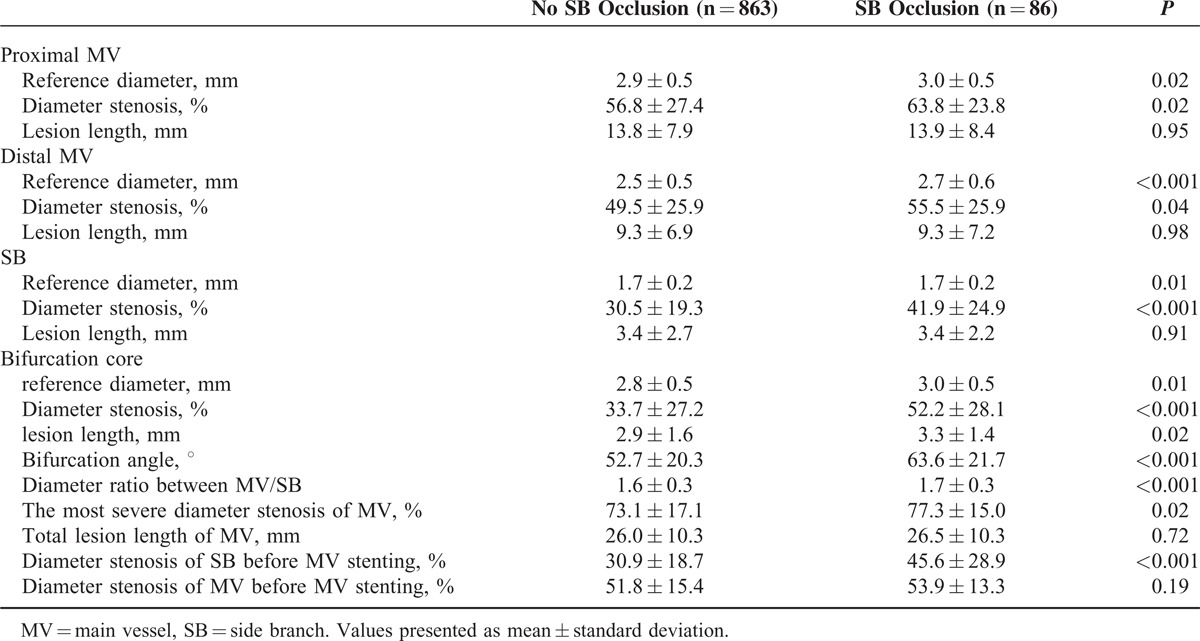
TABLE 4.
Independent Predictors of SB Occlusion
Incidence of PMI
Periprocedural cardiac enzymes were obtained from 97.74% (821/840) patients in the no SB occlusion group and from 97.65% (83/85) patients in the SB occlusion group. Compared with patients with no SB occlusion, patients in the SB occlusion group have significant higher elevations of postprocedural CK-MB. A significantly higher incidence of postprocedural CK-MB elevation was observed in patients with angiographic evidence of SB occlusion group compared with those in no SB occlusion group in each cutoff level (Figure 4).
FIGURE 4.
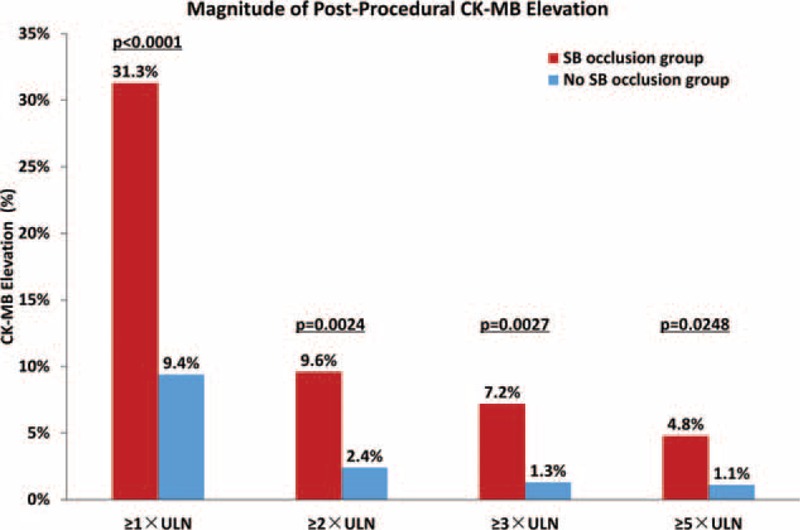
Magnitude of postprocedural CK-MB elevation. Comparisons between the patients with SB occlusion (red bars) and those without SB occlusion (blue bars). The incidence of PMI (CK-MB ≥1 × ULN) in SB occlusion group was 31.3%, which was significantly higher than the incidence of PMI in no SB occlusion group (9.4%) (P < 0.0001). Also, significantly higher incidence of postprocedural CK-MB elevation was observed in patients with SB occlusion group compared with those without SB occlusion in other cutoff level: CK-MB ≥2 × ULN (9.6% vs 2.4%, P = 0.0024), CK-MB ≥3 × ULN (7.2% vs 1.3%, P = 0.0027), and CK-MB ≥5 × ULN (4.8% vs 1.1%, P = 0.0248). SB = side branch, CK-MB = creatine kinase myocardial band, ULN = upper limit of the normal.
The frequency of PMI was greater in SB occlusion group (26/83, 31.3%) than no SB occlusion group (77/821, 9.4%) (P < 0.001). Periprocedural MI occurred more frequently in patients of SB occlusion group (6/83, 7.2%) than in those without SB occlusion (11/821, 1.3%) (P < 0.001). Among all 17 patients with periprocedural MI, 5 patients had prolonged ischemic symptoms >20 minutes, and 3 patients had both prolonged chest pain and new Q-wave MI (Q-wave MI developed in 2.9% [3/103] of PMI patients).
Clinical Outcomes
The follow-up duration was 12 months and the follow-up rate was 97.7% (904/925). No death, MI, or stent thrombosis occurred in the overall population. The rates of recurrence of the angina pectoris (0% vs 3.8%, P = 0.14), rehospitalization (1.2% vs 2.4%, P = 0.76), and any revascularization (2.4% vs 3.0%, P = 0.76) were similar between patients with and without SB occlusion.
DISCUSSION
The major findings of the present study are as follows: 9.1% of small SB occluded after MV stenting; irregular plaque, preprocedural diameter stenosis of bifurcation core, as well as other 8 factors were independent predictors of SB occlusion; patients with small SB occlusion had significant higher incidence of PMI; and there is no significant difference in clinical outcome during the 12-month follow-up.
Previous studies have reported that the incidence of SB occlusion was 8.4% to 19%.4–6 In our study, the rate of SB occlusion was 9.1%. This wide range of SB occlusion rate can be attributable to the difference of reference vessel diameter of SB in these studies. Smaller reference vessel diameter was an independent predictor of SB occlusion reported in the previous study.5 In our study, the mean reference vessel diameter of SB was 1.72 mm, which was smaller than the study of Hahn et al4 (SB occlusion rate: 8.4%) and larger than the studies by Kralev et al5 (SB occlusion rate: 12.5%) and Aliabadi et al6 (SB occlusion rate: 19%). The rate of SB occlusion increases as the reference vessel diameter of SB becomes smaller.
Identifying the predictors of SB occlusion could help interventional cardiologists to avoid abrupt closure of SB. In our study, several independent predictors have been disclosed by multivariable analyses. Among them, irregular plaque and true bifurcation lesion have been reported as independent predictors of SB occlusion.4 Previous studies have found that irregular plaque was linked to occlusive coronary artery thrombosis at sites of plaque fissure, rupture, or superficial erosion, which are largely involved in the pathogenesis of such acute events.21 Plaque surface morphology on coronary angiography can be a highly sensitive marker of plaque instability. The instability of irregular plaque may contribute to the SB occlusion. Preprocedural SB TIMI flow grade are index indicating the baseline coronary blood flow. Arteries with lower TIMI flow grade are easier to have SB occlusion. Diameter ratio between MV and SB was also an important predictor, which was concordant with the results of the previous study.22 Diameter ratio between MV and SB reflects the relative plaque volume of MV. Larger diameter ratio between MV and SB indicates relatively larger plaque burden to SB. Preprocedural diameter stenosis of distal MV, preprocedural diameter stenosis of bifurcation core, diameter stenosis of SB before MV stenting, and MV lesion length were also indexes reflecting the plaque volume and risk of SB occlusion. SB predilation was an effective way to decrease the stenosis of SB ostium and thus decrease the risk of SB occlusion.
The effect of bifurcation angle on the rate of SB occlusion during PCI is controversial. Previous studies have reported that smaller angle in coronary bifurcations predicted higher SB compromise, restenosis, and major adverse cardiac events (MACEs) rates based on small sample size.22 In addition, Yoshitaka Goto et al23 reported that bifurcation angle was not associated with SB compromise after MV stenting. On the other hand, Dzavik et al24 found that bifurcation angle >50° is an independent predictor of MACE after bifurcation crush stenting. In our study, a wide bifurcation angle predicted SB occlusion after MV stenting. Part of the explanation was that bifurcations with smaller bifurcation angle was easier for flow diversion into SB and too large bifurcation angle might increase the pressure drop and flow resistance,25 thus increasing the SB occlusion risk. Another potential explanation was that increasing bifurcation angle decreased wall shear stress and increases oscillatory shear index significantly around the carina,26 which might induce plaque proliferation at the bifurcation region.27,28 Higher plaque volume in bifurcation core may contribute to the higher SB occlusion risk.
Small SBs occlusion was thought to be well tolerated.6–8 In our study, both the rate of PMI and periprocedural MI were significantly higher in SB occlusion group than no SB occlusion group. CK-MB levels were significantly higher after stenting in patients with SB occlusion than in patients without SB occlusion. Previous studies have reported that even a small increase in CK-MB levels after PCI is associated with significantly higher risk of late mortality.11,29–31 However, the present study showed no significant differences in clinical outcome during the 12-month follow-up. The low residual SYNTAX score in both the groups (3.5 ± 5.3 in no SB occlusion group vs 4.2 ± 6.0 in SB occlusion group, P = .29) may explain the low incidence of MACEs. Greater sample sizes and a longer follow-up period are required to fully determine the effect of small SB occlusion on clinical outcome.
Prevention of SB occlusion may be useful for avoiding PMI. Identifying the predictors of small SB occlusion could help to prevent SB occlusion. For small SBs with high occlusion risk, jailed-balloon technique is recommended in consideration of that this technique was associated with lower rates of SB loss and a high procedural success rate.32,33 However, the mean reference of SB was 1.7 ± 0.2 mm in the present study and not all SBs were suitable for jailed-balloon technique. Thus, other approaches for preventing PMI were also needed. Previous studies have reported that a single high loading dose of atorvastatin or clopidogrel could reduce the incidence of PMI in elective PCI.34,35 Other novel approaches such as intravenous vitamin C infusion, trimetazidine intake before elective PCI, and lower inflation maximal pressure were also considered to be associated with less PMI.36–38
Compared with the previous studies,5–8 the strength of our study is that the present large-scale study has included all the clinical, angiographic, and procedural factors, as well as other innovative parameters such as diameter ratio between MV and SB, which is significantly predictive of SB occlusion. Another strength of our study is that the study was conducted in a consecutive cohort of bifurcation patients, which could reflect the real-world clinical practice. In addition, not only the baseline but also the procedural angiography is analyzed in the present study, risk factors in procedural cineangiograms such as diameter stenosis of SB before MV stenting were reported to be independent predictors of small SB occlusion for the first time. Last, but not least, the bifurcation core is the area most adjacent to SB and as such a smaller diameter stenosis could be a correlate of plaque shift during MV PCI. The present study performed QCA analysis with the use of a computer-based system dedicated to bifurcation analysis, thus bifurcation core is involved as a novel and important parameter in QCA analysis. Preprocedural diameter stenosis of bifurcation core is found to be an independent risk factor of small SB occlusion. We have brought this vital definition, bifurcation core, to the forefront.
Study Limitation
First, our study is limited by the retrospective single-center design and unknown confounding factors cannot be excluded. Second, selection of treatment strategies, stent types, and other instruments were at the discretion of operators. Our findings are subject to selection bias and compounded with unmeasured variables. Third, this study principally included patients with coronary bifurcation disease that is defined by European Bifurcation Club and excluded patients with bifurcation lesions with SB >2 mm in diameter. The incidence and predictors of SB occlusion would be expected to be different in larger SB. Last, because of the sample size, follow-up period, and low residual SYNTAX score, the incidence of MACE is low and further analysis of clinical outcomes is not available. Greater sample sizes and a longer follow-up period are required in future studies.
CONCLUSION
After MV stenting in coronary bifurcation intervention, 9.1% SB with reference vessel diameter ≤2 mm occluded. True bifurcation lesion, irregular plaque, predilation in SB, preprocedural SB TIMI flow grade, preprocedural diameter stenosis of distal MV, preprocedural diameter stenosis of bifurcation core, bifurcation angle, diameter ratio between MV and SB, diameter stenosis of SB before MV stenting, and MV lesion length are independent predictors of small SB occlusion. Patients with small SB occlusion had significant higher incidence of PMI.
Acknowledgments
The authors are grateful to the staff in the Department of Cardiology and Catheterization Laboratory at Fuwai Hospital. They also sincerely thank Wang Yang and Yan Ruohua for their expert statistical assistance.
Footnotes
Abbreviations: CI = confidence interval, CK-MB = creatine kinase-myocardial band, MACE = major adverse cardiac event, MI = myocardial infarction, MV = main vessel, OR = odds ratio, PCI = percutaneous coronary intervention, PMI = periprocedural myocardial injury, QCA = quantitative coronary angiography, SB = side branch, SYNTAX = synergy between PCI with taxus and cardiac surgery, TIMI = thrombolysis in myocardial infarction, ULN = upper limit of normal.
This research was supported by Beijing Municipal Science and Technology Commission (Grant number: Z141107002514096).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Cuculi F, Lim CC, Banning AP. Periprocedural myocardial injury during elective percutaneous coronary intervention: is it important and how can it be prevented? Heart 2010; 96:736–740. [DOI] [PubMed] [Google Scholar]
- 2.Park DW, Kim YH, Yun SC, et al. Frequency, causes, predictors, and clinical significance of peri-procedural myocardial infarction following percutaneous coronary intervention. Eur Heart J 2013; 34:1662–1669. [DOI] [PubMed] [Google Scholar]
- 3.Arora RR, Raymond RE, Dimas AP, et al. Side branch occlusion during coronary angioplasty: incidence, angiographic characteristics, and outcome. Cathet Cardiovasc Diagn 1989; 18:210–212. [DOI] [PubMed] [Google Scholar]
- 4.Hahn JY, Chun WJ, Kim JH, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol 2013; 62:1654–1659. [DOI] [PubMed] [Google Scholar]
- 5.Kralev S, Poerner TC, Basorth D, et al. Side branch occlusion after coronary stent implantation in patients presenting with ST-elevation myocardial infarction: clinical impact and angiographic predictors. Am Heart J 2006; 151:153–157. [DOI] [PubMed] [Google Scholar]
- 6.Aliabadi D, Tilli FV, Bowers TR, et al. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol 1997; 80:994–997. [DOI] [PubMed] [Google Scholar]
- 7.Fischman DL, Savage MP, Leon MB, et al. Fate of lesion-related side branches after coronary artery stenting. J Am Coll Cardiol 1993; 22:1641–1646. [DOI] [PubMed] [Google Scholar]
- 8.Muramatsu T, Onuma Y, Garcia-Garcia HM, et al. Incidence and short-term clinical outcomes of small side branch occlusion after implantation of an everolimus-eluting bioresorbable vascular scaffold: an interim report of 435 patients in the ABSORB-EXTEND single-arm trial in comparison with an everolimus-eluting metallic stent in the SPIRIT first and II trials. JACC Cardiovasc Interv 2013; 6:247–257. [DOI] [PubMed] [Google Scholar]
- 9.Saadeddin SM, Habbab MA, Sobki SH, et al. Minor myocardial injury after elective uncomplicated successful PTCA with or without stenting: detection by cardiac troponins. Catheter Cardiovasc Interv 2001; 53:188–192. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhry EC, Dauerman KP, Sarnoski CL, et al. Percutaneous coronary intervention for major bifurcation lesions using the simple approach: risk of myocardial infarction. J Thromb Thrombolysis 2007; 24:7–13. [DOI] [PubMed] [Google Scholar]
- 11.Ioannidis JP, Karvouni E, Katritsis DG. Mortality risk conferred by small elevations of creatine kinase-MB isoenzyme after percutaneous coronary intervention. J Am Coll Cardiol 2003; 42:1406–1411. [DOI] [PubMed] [Google Scholar]
- 12.Louvard Y, Medina A, Stankovic G. Definition and classification of bifurcation lesions and treatments. EuroIntervention 2010; 6 suppl J:J31–J35. [DOI] [PubMed] [Google Scholar]
- 13.Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 2005; 1:219–227. [PubMed] [Google Scholar]
- 14.Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation 2013; 128:141–151. [DOI] [PubMed] [Google Scholar]
- 15.Genereux P, Palmerini T, Caixeta A, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol 2012; 59:2165–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lansky AJ, Dangas G, Mehran R, et al. Quantitative angiographic methods for appropriate end-point analysis, edge-effect evaluation, and prediction of recurrent restenosis after coronary brachytherapy with gamma irradiation. J Am Coll Cardiol 2002; 39:274–280. [DOI] [PubMed] [Google Scholar]
- 17.Janssen JP, Rares A, Tuinenburg JC, et al. New approaches for the assessment of vessel sizes in quantitative (cardio-)vascular X-ray analysis. Int J Cardiovasc Imaging 2010; 26:259–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007; 115:2344–2351. [DOI] [PubMed] [Google Scholar]
- 19.Lim CC, van Gaal WJ, Testa L, et al. With the “universal definition,” measurement of creatine kinase-myocardial band rather than troponin allows more accurate diagnosis of periprocedural necrosis and infarction after coronary intervention. J Am Coll Cardiol 2011; 57:653–661. [DOI] [PubMed] [Google Scholar]
- 20.Thygesen K, Alpert JS, White HD. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol 2007; 50:2173–2195. [DOI] [PubMed] [Google Scholar]
- 21.Ambrose JA, Tannenbaum MA, Alexopoulos D, et al. Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol 1988; 12:56–62. [DOI] [PubMed] [Google Scholar]
- 22.Gil RJ, Vassilev D, Formuszewicz R, et al. The carina angle-new geometrical parameter associated with periprocedural side branch compromise and the long-term results in coronary bifurcation lesions with main vessel stenting only. J Interv Cardiol 2009; 22:E1–E10. [DOI] [PubMed] [Google Scholar]
- 23.Yoshitaka Goto Y, Kawasaki T, Koga N, et al. Plaque distribution patterns in left main trunk bifurcations: prediction of branch vessel compromise by multidetector row computed topography after percutaneous coronary intervention. EuroIntervention 2012; 8:708–716. [DOI] [PubMed] [Google Scholar]
- 24.Dzavik V, Kharbanda R, Ivanov J, et al. Predictors of long-term outcome after crush stenting of coronary bifurcation lesions: importance of the bifurcation angle. Am Heart J 2006; 152:762–769. [DOI] [PubMed] [Google Scholar]
- 25.Sayed Razavi M, Shirani E. Development of a general method for designing microvascular networks using distribution of wall shear stress. J Biomech 2013; 46:2303–2309. [DOI] [PubMed] [Google Scholar]
- 26.Huo Y, Finet G, Lefevre T, et al. Which diameter and angle rule provides optimal flow patterns in a coronary bifurcation? J Biomech 2012; 45:1273–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kimura BJ, Russo RJ, Bhargava V, et al. Atheroma morphology and distribution in proximal left anterior descending coronary artery: in vivo observations. J Am Coll Cardiol 1996; 27:825–831. [DOI] [PubMed] [Google Scholar]
- 28.Rodriguez-Granillo GA, Garcia-Garcia HM, Wentzel J, et al. Plaque composition and its relationship with acknowledged shear stress patterns in coronary arteries. J Am Coll Cardiol 2006; 47:884–885. [DOI] [PubMed] [Google Scholar]
- 29.Jang JS, Jin HY, Seo JS, et al. Prognostic value of creatine kinase-myocardial band isoenzyme elevation following percutaneous coronary intervention: a meta-analysis. Catheter Cardiovasc Interv 2013; 81:959–967. [DOI] [PubMed] [Google Scholar]
- 30.Kong TQ, Davidson CJ, Meyers SN, et al. Prognostic implication of creatine kinase elevation following elective coronary artery interventions. J Am Med Assoc 1997; 277:461–466. [PubMed] [Google Scholar]
- 31.Akkerhuis KM, Alexander JH, Tardiff BE, et al. Minor myocardial damage and prognosis: are spontaneous and percutaneous coronary intervention-related events different? Circulation 2002; 105:554–556. [DOI] [PubMed] [Google Scholar]
- 32.Singh J, Patel Y, Depta JP, et al. A modified provisional stenting approach to coronary bifurcation lesions: clinical application of the “jailed-balloon technique”. J Interv Cardiol 2012; 25:289–296. [DOI] [PubMed] [Google Scholar]
- 33.Depta JP, Patel Y, Patel JS, et al. Long-term clinical outcomes with the use of a modified provisional jailed-balloon stenting technique for the treatment of nonleft main coronary bifurcation lesions. Catheter Cardiovasc Interv 2013; 82:E637–E646. [DOI] [PubMed] [Google Scholar]
- 34.Patti G, Colonna G, Pasceri V, et al. Randomized trial of high loading dose of clopidogrel for reduction of periprocedural myocardial infarction in patients undergoing coronary intervention: results from the ARMYDA-2 (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) study. Circulation 2005; 111:2099–2106. [DOI] [PubMed] [Google Scholar]
- 35.Briguori C, Visconti G, Focaccio A, et al. Novel approaches for preventing or limiting events (Naples) II trial: impact of a single high loading dose of atorvastatin on periprocedural myocardial infarction. J Am Coll Cardiol 2009; 54:2157–2163. [DOI] [PubMed] [Google Scholar]
- 36.Wang ZJ, Hu WK, Liu YY, et al. The effect of intravenous vitamin C infusion on periprocedural myocardial injury for patients undergoing elective percutaneous coronary intervention. Can J Cardiol 2014; 30:96–101. [DOI] [PubMed] [Google Scholar]
- 37.Ferenc M, Gick M, Kienzle RP, et al. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J 2008; 29:2859–2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shehata M. Impact of trimetazidine on incidence of myocardial injury and contrast-induced nephropathy in diabetic patients with renal dysfunction undergoing elective percutaneous coronary intervention. Am J Cardiol 2014; 114:389–394. [DOI] [PubMed] [Google Scholar]


